Abstract
Background
The relationship between psychiatric consultation and antipsychotic prescribing in nursing homes (NH) is unknown.
Objective
To identify the association between psychiatric consultant groups and NH-level antipsychotic prescribing after adjustment for resident case-mix and facility characteristics.
Research Design & Subjects
Nested cross-sectional study of 60 NHs in a cluster randomized trial. We linked facility leadership surveys to October 2009-September 2010 Minimum Data Set, Nursing Home Compare, U.S. Census and pharmacy dispensing data.
Measures
The main exposure is the psychiatric consultant group and the main outcome is NH-level prevalence of atypical antipsychotic use. We calculated annual means and interquartile ranges of NH-level antipsychotic use for each consultant group and arrayed consultant groups from lowest to highest prevalence. Generalized linear models were used to predict antipsychotic prescribing adjusting for resident case-mix and facility characteristics. Observed versus predicted antipsychotic prescribing levels were compared for each consultant group.
Results
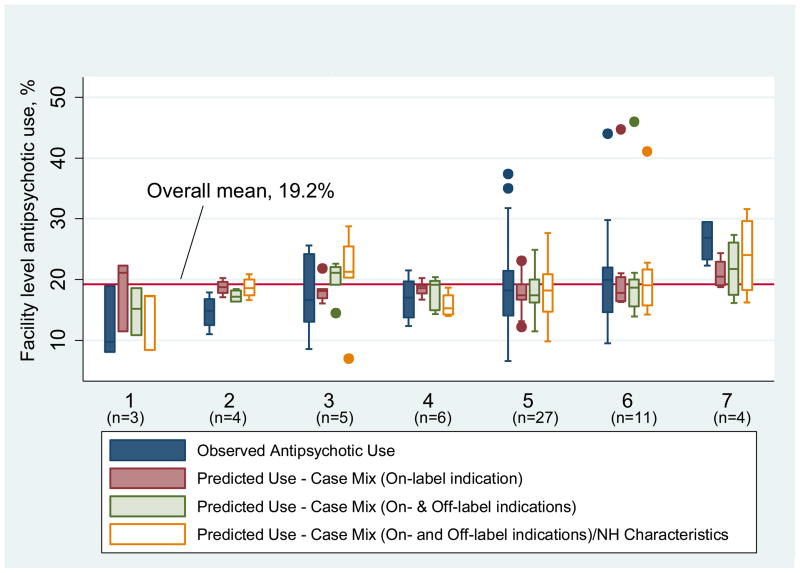
Seven (7) psychiatric consultant groups served a range of 3 to 27 study facilities. Overall mean facility-level antipsychotic prescribing was 19.2%. Mean prevalence of antipsychotic prescribing ranged from 12.2% (SD 5.8) in the lowest consultant group to 26.4% (SD 3.6) in the highest group. All facilities served by the highest-ranked consultant group had observed antipsychotic levels exceeding the overall study mean with half exceeding predictions for on-label indications, while most facilities served by the lowest-ranked consultant group had observed levels below the overall study and predicted means.
Conclusions
Preliminary evidence suggests that psychiatric consultant groups affect NH antipsychotic prescribing independent of resident case-mix and facility characteristics.
Keywords: antipsychotics, nursing homes, quality of care, case-mix, inappropriate drug use
BACKGROUND
Federal regulations require nursing homes (NHs) in the United States to have psychiatric services available to meet residents’ mental health and psychosocial needs.1 While dementia-related behaviors remain the predominant management challenge in most NHs,2 a large proportion of residents also have psychotic or mood disorders. NH staff are often ill-equipped to serve the complex needs of these residents and rely on expert mental health consultation.3
While geriatric psychiatrists are ideally suited to serve this population, with specialized training in the complexities of older adults with mental health and neurodegenerative disorders, there is a shortage of geriatric psychiatrists.4–6 Further, financial constraints limit the extent to which psychiatric and psychological consultants can provide behavior-based, non-pharmacologic, interventions.5,7,8 Taken together, financial and manpower constraints result in a persistent challenge for clinical and healthcare policy leaders.5
The psychiatric consultant has an important but little studied role in assisting NH physicians and nurses caring for residents with dementia. Prior studies have shown that specialty training can affect care delivery and outcomes in a variety of medical conditions.9–11 To date, there are no studies of the relationship between psychiatric consultations and antipsychotic prescribing in NHs. The objective of this study is to assess variation in antipsychotic prescribing across psychiatric consultant groups. We hypothesize that psychiatric consultant groups significantly affect the level of antipsychotic prescribing within the NHs they serve, even after accounting for differences in resident case-mix and facility characteristics.
METHODS
Study Design and Setting
We conducted a nested cross-sectional study of NHs participating in a cluster randomized controlled trial. The trial evaluated dissemination strategies for an educational intervention to improve evidence-based antipsychotic prescribing. [Clinical Trials Registration #NCT01347619]
Data Sources
Data for this study are derived from the baseline data for 68 NHs participating in the trial. Data sources include mailed surveys to facility leadership, facility-level aggregated Minimum Data Set (MDS) 2.0 data, Nursing Home Compare data,12 U.S. Census data and linked long-term care pharmacy dispensings.
Measurements
The main outcome measure is the facility-level prevalence of atypical antipsychotic use aggregated across psychiatric consultant groups. Facility-level atypical antipsychotic use was measured as the proportion of residents receiving at least 1 atypical antipsychotic prescription from among all short- and long-stay NH residents between the fourth quarter of 2009 to the third quarter of 2010.
Psychiatric consultant group
We identified psychiatric consultant groups from the baseline mailed survey to facility leadership conducted in the first quarter of 2011. Non-respondents were telephoned to ask to identify their psychiatric consultant group.
Case-mix measures
Case-mix measures known and hypothesized to affect antipsychotic prescribing13–15 were calculated at the facility level as a percentage of all residents with those characteristics in the MDS. These included age and sex (<65 years and male), on-label indications (schizophrenia and bipolar disorder), off-label indications (dementia, severe behaviors, and major depression) and risk of metabolic complications (diabetes mellitus). We used the MDS-based Behavioral Index score to identify residents with severe behaviors based on their frequency of verbal, physically abusive, socially inappropriate, and wandering behavior.16,17
Facility characteristics
We included facility characteristics known to affect NH-level antipsychotic use.13–15,18 Financial resource measures include profit status, ownership, % Medicaid payor and surrounding community socioeconomic status (census region % <150% of federal poverty level [FPL]).13,15,18 Personnel resources15,18 include nurse staffing time (Registered Nurse [RN] hours, Licensed Practical Nurse [LPN] hours, certified nursing assistant [CNA] hours, each per resident day) measured from Nursing Home Compare.12; NH quality18 was measured by the number of survey deficiencies on the facility’s most recent survey reported on Nursing Home Compare; and presence of a dementia unit was based on a published list from the Alzheimer’s Association.
Data analysis
The final analytic sample included 60 NHs after removing 8 NHs for which the psychiatric consultant group was unidentified (n=2) or provided services to 2 or fewer NHs in the parent study (n=6). The unit of analysis is the NH, with measurements representing mean NH-level antipsychotic use grouped by psychiatric consultant group. Generalized linear models with gamma distribution and log-link adjusted the relationship between psychiatric consultant group and antipsychotic use for confounders including: (model 1) on-label case-mix indicators; (model 2) on- and off-label case-mix indicators; and (model 3) on- and off-label case-mix indicators with NH characteristics. All models include adjustment for risk of metabolic complications (i.e. % residents with diabetes). These models were used to predict levels of antipsychotic prescribing adjusting for the model variables. We constructed box-and-whisker plots to demonstrate, across groupings of NHs within psychiatric consultant groups, observed versus predicted levels of antipsychotic prescribing. All analyses were conducted in STATA 10.1 SE (StataCorp, College Station, TX). The study was approved by the institutional review board of the University of Massachusetts Medical School.
RESULTS
Psychiatric Consultant Groups, Resident Case-Mix and Facility Characteristics
All 60 NHs included in our analytic sample reported having mental health services provided by one of 7 psychiatric consultant groups (range of 3 to 27 NHs per group). (Table 1) The NHs served by psychiatric consultant groups varied in case-mix from 1.6% to 5.3% of residents with schizophrenia, from 51.9% to 66.9% of residents with dementia, and from .4% to 2.4% residents with severe behaviors. The resources and quality of the NHs served by the psychiatric consultant groups also varied. (Table 1) Mean RN hours and LPN hours provided by the NHs served by different psychiatric consultant groups and varied by as much ~100% (i.e. ranging from 0.63 hours per resident day to 1.23 hours per resident day). Payor mix varied, with some psychiatric consultant groups serving NHs who had <45% Medicaid residents to other consultant groups whose NHs averaged nearly 70% Medicaid residents. Local NH census regions also varied in poverty level from 3.3% to 17.8% of the region <150% of FPL. The quality of the NHs served varied with the mean number of healthcare deficiencies ranging from 5.7 to 9.6. (Table 1)
Table 1.
Resident Case-Mix and Nursing Home Characteristics, by Psychiatric Consultant Group
| Psychiatric Consultant Group | |||||||
|---|---|---|---|---|---|---|---|
| Identification Number | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Number of Participating Nursing Homes | 3 | 4 | 5 | 6 | 27 | 11 | 4 |
| Characteristics of Nursing Homes Served | |||||||
| Resident Case-Mix | |||||||
| Mean % male & < 65 years old (SD) | 4.5 (4.6) | 3.1 (2.5) | 1.5 (0.8) | 2.6 (1.8) | 2.2 (2.6) | 3.3 (4.9) | 3.1 (2.6) |
| Mean % schizophrenia patients (SD) | 4.4 (4.4) | 3.7 (2.4) | 1.6 (1.1) | 1.6 (1.7) | 2.2 (2.3) | 5.3 (5.1) | 4.3 (4.2) |
| Mean % dementia (SD) | 51.9 (11.7) | 59.4 (11.2) | 66.9 (13.4) | 60.4 (11.8) | 62.5 (12.1) | 57.7 (10.5) | 61.7 (29.3) |
| Mean % Behavior Index - severe (SD) | 2.4 (4.1) | 1.7 (2.1) | .42 (.58) | 1.3 (1.3) | .9 (1.5) | 1.0 (1.2) | 1.2 (1.7) |
| Mean % diabetes mellitus (SD) | 28.5 (5.4) | 29.4 (4.9) | 30.9 (7.2) | 24.2 (9.6) | 28.5 (6.0) | 29.7 (4.9) | 25.8 (13.3) |
| Mean % body mass index > 30 (SD) | 20.4 (2.6) | 20.7 (6.4) | 22.5 (6.2) | 19.9 (5.1) | 24.0 (7.6) | 21.6 (3.7) | 21.4 (13.2) |
| Mean % major depression (SD) | 40.2 (9.1) | 51.6 (18.2) | 56.5 (9.0) | 49.4 (13.1) | 50.9 (11.9) | 55.0 (13.6) | 50.0 (20.9) |
| Mean % bipolar disorder (SD) | 8.1 (8.7) | 3.4 (1.7) | 2.4 (2.1) | 1.4 (0.9) | 3.7 (3.8) | 3.8 (3.0) | 0.9 (0.7) |
| Nursing Home Resources, Staffing and Quality | |||||||
| Mean % Medicaid (SD) | 65.3 (21.5) | 45.1 (15.8) | 64.9 (10.1) | 49.6 (26.1) | 55.6 (18.2) | 65.0 (11.7) | 74.4 (3.0) |
| For Profit | 0% | 100% | 60% | 100% | 96% | 73% | 75% |
| Mean % <150 federal poverty level (SD) | 3.3 (2.1) | 4.5 (2.1) | 17.8 (27.7) | 4.0 (3.6) | 6.7 (5.2) | 17.1 (18.3) | 9.0 (10.7) |
| Mean RN Hours (SD) | 1.23 (.62) | .64 (.16) | .87 (.72) | .75 (.17) | .77 (.26) | .81 (.20) | .63 (10.8) |
| Mean LPN Hours (SD) | .50 (.09) | .70 (.11) | .90 (.06) | .79 (.28) | .74 (.30) | .72 (.15) | .73 (.18) |
| Mean CNA Hours (SD) | 2.9 (.73) | 2.4 (.12) | 2.7 (.29) | 2.8 (.48) | 2.3 (.38) | 2.5 (.24) | 2.3 (.17) |
| Dementia Unit | 33% | 100% | 60% | 67% | 67% | 73% | 75% |
| Mean # Healthcare Deficiencies (SD) | 5.7 (4.1) | 7.0 (3.2) | 7.4 (4.5) | 7.7 (5.2) | 9.6 (4.8) | 5.7 (3.8) | 6.5 (2.7) |
Observed versus Predicted Antipsychotic Prescribing across Psychiatric Consultant Groups
Overall mean atypical antipsychotic prescribing for the 60 homes in this analysis was 19.2% (standard deviation (SD) 8.1, IQR 14.0%, 21.8%, median 18.2%). The statewide average was 21.6%. Across psychiatry consultant groups, prescribing of antipsychotics varied from a mean of 12.2% (SD 5.8) for psychiatric consultant group 1 to a high of 26.4% (SD 3.6) for group 7.
Figure 1 shows 4 box-and-whisker plots for each of 7 psychiatric consultant groups. Each box within consultant groups represents antipsychotic prescribing as follows: 1. observed; 2. case-mix (on-label) predicted; 3. case-mix (on- and off-label) predicted; 4. case-mix (on- and off-label) and facility characteristic predicted. Each plot shows antipsychotic prescribing of the median facility (central mark), the 25th and 75th percentile facilities (box edges), the adjacent facilities not considered outliers (whiskers), and outlier facilities. These estimates are shown compared to the overall study prescribing mean of 19.2%.
Figure 1.
Observed versus Predicted Antipsychotic Prescribing, by Psychiatric Consultant Group
Figure 1 shows that all of the NHs for psychiatric consultant groups 1 and 2 were under the study mean, and most (75%) of the facilities had lower observed prescribing levels than was predicted by on-label case-mix adjustment, and on- and off label case-mix adjustment; observed prescribing for most facilities in group 2 were also lower than predicted by full adjustment. In contrast, all of the participating NHs for psychiatric consultant group 7 were over the study mean prescribing level and half of the facilities for psychiatric consultant 7 had higher observed prescribing than predicted by on-label case-mix adjustment.
DISCUSSION
Access to quality mental health services within NHs is an ongoing concern for NH stakeholders, policy makers, and payors.5 In this study, we find that there is variation in facility-level antipsychotic prescribing by psychiatric consultant group, and that this relationship is not consistently explained by differences in the resident case-mix or facility characteristics. Most of the NHs served by the two lowest ranked psychiatric consultant groups in our study had observed antipsychotic use below predicted levels, while half of the NHs served by the highest ranked psychiatric consultant group had observed antipsychotic use above levels predicted for on-label indications. These findings provide preliminary evidence that characteristics of the psychiatric consultant groups can influence the overall quality of dementia care delivered within NHs.
The level at which antipsychotic prescribing in the NH is considered appropriate is yet unclear. The Center for Medicare and Medicaid Services’ (CMS) National Partnership to Improve Dementia Care called for a reduction in national NH antipsychotic use of 15% before 2013. The campaign resulted in a decrease in the national average from 23.9% to 21.7%, a 9% relative reduction. While CMS continues to encourage further reductions, it notes that “[T]here may be valid reasons why some providers have higher than average rates of antipsychotic use, based on their population”.19 Our analysis demonstrates that while this is generally true, some facilities have levels higher (and lower) levels than predicted by case-mix.
The literature suggests that different models for psychiatric consultation offer different levels of effectiveness.20 Psychiatric consultant models include a: 1) traditional consultation-liaison service model; 2) nurse-centered model; and 3) multi-disciplinary team model. Reported to be least effective is the traditional consultation-liaison service in which a clinician provides one-time, emergency, written consultation on an as-needed basis.20 Most desirable, but least available, is the multi-disciplinary team model integrating the psychiatric consultant into the fabric of the facility staff.21,22 In this model, the psychiatrist’s role is expanded beyond the provision of diagnostic and medication recommendations to include staff support, assistance dealing with staff and family conflicts, and assistance implementing non-pharmacologic behavioral management techniques.22
Our study has several limitations. First, we could not report actual antipsychotic use for on- and off-label indications; we could only report predicted levels based on facility-level adjustors because we lacked individual-level data linking resident characteristics to drug dispensings. Second, the measure of nurse staffing in our analysis, though drawn from NH Compare, is self-reported by each facility. Finally, we could not characterize each psychiatric consultant group in terms of specialty training or care model. We draw evidence of psychiatric practice variation from our facility leadership surveys and the websites for each psychiatric consultant group. For example, one NH leader reported that their psychiatric consultant group was comprised of a single physician paired with a single nurse practitioner who together provided care to over 30 facilities. In contrast, the psychiatric group with the most facilities in our study was a large mental health provider with over 250 employees serving NHs in several states. Websites also revealed that some psychiatric consultant groups promoted a model that focused on behavioral management and staff training, and that a few had specialty training in geriatric psychiatry. However, since we did not systematically measure psychiatric consultant group characteristics, we can only say that we found evidence of variation in psychiatric consult models.
Despite these limitations, this study provides the first preliminary evidence that there is variation in facility-level antipsychotic prescribing by psychiatric consultant groups, and that this variation is not well-explained by resident case-mix and facility characteristics. A strength of this study is the relatively large sample size and facility-level prescribing data linked with case-mix, resource, and quality data. We acknowledge that the number of facilities analyzed for some psychiatric consultant groups was small. Future studies need to replicate this analysis in a larger sample. Should this finding prove robust, there are important implications for policy and practice.
Current regulations specify that psychiatric services need to be available to NHs, but do not specify the model of care or type of required training. Clinicians and administrators agree that the traditional ‘as needed’ consultation model is inadequate to address many NH resident and staff needs.23 Innovative solutions should be pursued while we seek to validate our findings in larger, more regionally diverse settings. For example, teleconferencing technologies can connect NH staff with geriatric psychiatrists. And training and academic detailing activities can be expanded to target psychiatric consultant groups, and not just facility-based prescribers. In this way, efforts can continue to improve quality of mental health care for U.S. NH residents.
Acknowledgments
Funding Support: This project was supported by a grant from the Agency for Healthcare Quality and Research (R18 HS 019351). Dr. Briesacher was also supported by a Research Scientist Award (K01AG031836) from the National Institute on Aging.
Footnotes
Previous presentations: This research was accepted for presentation as a research abstract to the 29th International Conference on Pharmacoepidemiology & Therapeutic Risk Management, Montreal, Canada, August 25–28, 2013.
References
- 1.Health Care Financing Administration. Medicare and Medicaid: requirements for long-term care facilities, final regulations. Federal Register. 1991 Sep 26;56:48865–48921. [Google Scholar]
- 2.Fenton J, Raskin A, Gruber-Baldini AL, et al. Some predictors of psychiatric consultation in nursing home residents. Am J Geriatr Psychiatry. 2004;12:297–304. [PubMed] [Google Scholar]
- 3.Grabowski DC, Aschbrenner KA, Rome VF, et al. Quality of Mental Health Care for Nursing Home Residents: A Literature Review. Med Care Res Rev. 2010;67:627–656. doi: 10.1177/1077558710362538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abrams RC, Young RC. Crisis in Access to Care: Geriatric Psychiatry Services Unobtainable at Any Price. Pub Health Rep. 2006;121:646–649. doi: 10.1177/003335490612100603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Streim JE, Beckwith EW, Arapakos D, et al. Mental health services in nursing homes: Regulatory oversight, payment policy, and quality improvement in mental health care in nursing homes. Psych Serv. 2002;53:1414–1418. doi: 10.1176/appi.ps.53.11.1414. [DOI] [PubMed] [Google Scholar]
- 6.Juul D, Scheiber SC. Subspecialty certification in geriatric psychiatry. Am J Geriatr Psychiatry. 2003;11:351–355. [PubMed] [Google Scholar]
- 7.Gupta S, Goldstein MZ. Psychiatric consultation to nursing homes. Psych Serv. 1999;50:1547–1550. doi: 10.1176/ps.50.12.1547. [DOI] [PubMed] [Google Scholar]
- 8.Honn Qualls S, Segal Dl, Normal S, et al. Psychologists in practice with older adults. Current patterns, sources of training, and need for continuing education. Prof Psychol Res Pr. 2002;33:5435–5442. [Google Scholar]
- 9.Frances CD, Shlipak MG, Noguchi H, et al. Does physician specialty affect the survival of Health Serv Res. 2000;35:1093–1116. [PMC free article] [PubMed] [Google Scholar]
- 10.Smetana GW, Landon BE, Bindman AB, et al. A comparison of outcomes resulting from generalist versus specialist care for a single discrete medical condition: a systematic review and methodologic critique. Arch Int Med. 2007;167:10–20. doi: 10.1001/archinte.167.1.10. [DOI] [PubMed] [Google Scholar]
- 11.Donohoe MT. Comparing generalist and specialty care: discrepancies, deficiencies, and excesses. Arch Intern Med. 1998;158:1596–608. doi: 10.1001/archinte.158.15.1596. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Medicare and Medicaid Services. [Accessed on June 13, 2013];2013 http://www.medicare.gov/nursinghomecompare/
- 13.Hughes CM, Lapane KL, Mor V. Influence of Facility Characteristics on Use of Antipsychotic Medications in Nursing Homes. Med Care. 2000;38:1164–1173. doi: 10.1097/00005650-200012000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Chen Y, Briesacher B, Field T, et al. Unexplained variation across US nursing homes in antipsychotic prescribing rates. Arch Int Med. 2010;170:89–95. doi: 10.1001/archinternmed.2009.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castle NG, Hanlon JT, Handler SM. Results of a longitudinal analysis of national data to examine relationships between organizational and market characteristics and changes in antipsychotic prescribing in US nursing homes from 1996 through 2006. Am J Geriatr Pharmacotherapy. 2009;7:143–50. doi: 10.1016/j.amjopharm.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gambassi G, Lapane KL, Sgadari A, et al. Measuring health outcomes for older people using the SAGE database. Can J Aging. 2000;19:67–86. [Google Scholar]
- 17.Snowden M, Sato K, Roy-Byrne P. Assessment and treatment of nursing home residents with depression or behavioral symptoms associated with dementia: a review of the literature. J Am Geriatr Soc. 2003;51:1305–1317. doi: 10.1046/j.1532-5415.2003.51417.x. [DOI] [PubMed] [Google Scholar]
- 18.Mor V, Zinn J, Angelelli J, et al. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82:227–56. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonner A. Improving Dementia Care and Reducing Unnecessary Use of Antipsychotic Medications in Nursing Homes. Centers for Medicare and Medicaid Services presentation; [Accessed on: October 15, 2013]. Available at: http://doh.sd.gov/news/documents/cms_dementia_care.pdf. [Google Scholar]
- 20.Bartels SJ, Moak GS, Dums AR. Models of mental health services in nursing homes: A review of the literature. Psych Serv. 2002;53:1390–1396. doi: 10.1176/appi.ps.53.11.1390. [DOI] [PubMed] [Google Scholar]
- 21.American Geriatric Society and American Association for Geriatric Psychiatry. Consensus statement on improving the quality of mental health care in U.S. nursing homes: management of depression and behavioral symptoms associated with dementia. J Am Geriatr Soc. 2003;51:1287–1298. doi: 10.1046/j.1532-5415.2003.51415.x. [DOI] [PubMed] [Google Scholar]
- 22.Reichman WE, Coyne AC, Borson S, et al. Psychiatric consultation in the nursing home: A survey of six states. Am J Geritr Psychiatry. 1998;6:320–327. [PubMed] [Google Scholar]
- 23.Moak GS, Borson S, Jackson J. The AAGP long term care survey; Paper presented at the Long-Term Care Consensus Conference of the American Association for Geriatric Psychiatry; Washington, DC. 2000. [Google Scholar]