Abstract
Ischaemic stroke as the initial presentation of systemic malignancy is reported infrequently and is characterised by ischaemic lesions that exceed the vascular territory of a single vessel. There is also a high rate of early stroke recurrence. Several pathophysiological mechanisms are known to cause cerebrovascular complications in malignancies, as a direct effect of the tumour, paraneoplastic or even of the tumour treatment itself. Prognosis is reportedly poor, treatment is symptomatic and at best anecdotal. We present a case report and available literature.
Background
It is important to recognise ischaemic stroke as the initial presentation of systemic malignancy. It has been reported throughout medical literature in a small number of case reports and case series. It is an important differential diagnosis after cardiac emboli, vasculitis or giant cell arteritis have been ruled out. Ischaemic stroke may occur in malignancies as a direct effect of the tumour, coagulation disorder, infections or even due to the tumour treatment itself. The ischaemic lesions exceed the territory of a single vessel. Furthermore, early stroke recurrence is frequent which also contributes to the poor prognosis.
Case presentation
A 58-year-old woman was seen at the emergency department with a subacute change in behaviour. Her family reported her to have changed, over the course of several days: she appeared passive, repeated questions and wandered around seemingly aimless. Her medical history reported only migraine. She did not use any medication, drink alcohol, or smoke. Her family history revealed a twin sister, who died from breast cancer. General medical examination was normal except a blood pressure of 158/108 mm Hg, pulse frequency of 100/min, yet without signs of fever or skin rash. Neurological examination demonstrated disorientation and a disturbance in the reproduction of words, yet no other focal deficits.
Investigations
Laboratory examination revealed total bilirubin: 29 µmol/L (0–17), γ-glutamyl transpeptidase: 45 U/L (0–35), alanine transaminase (ALAT): 77 U/L (0–40), C reactive protein: 75 mg/L (0–10), leucocytes: 13.810E9/l (4.0–10.0).
CT scan of the brain showed bilateral hypodense lesions occipitally, suspect for subacute cerebral infarctions (figure 1).
Figure 1.
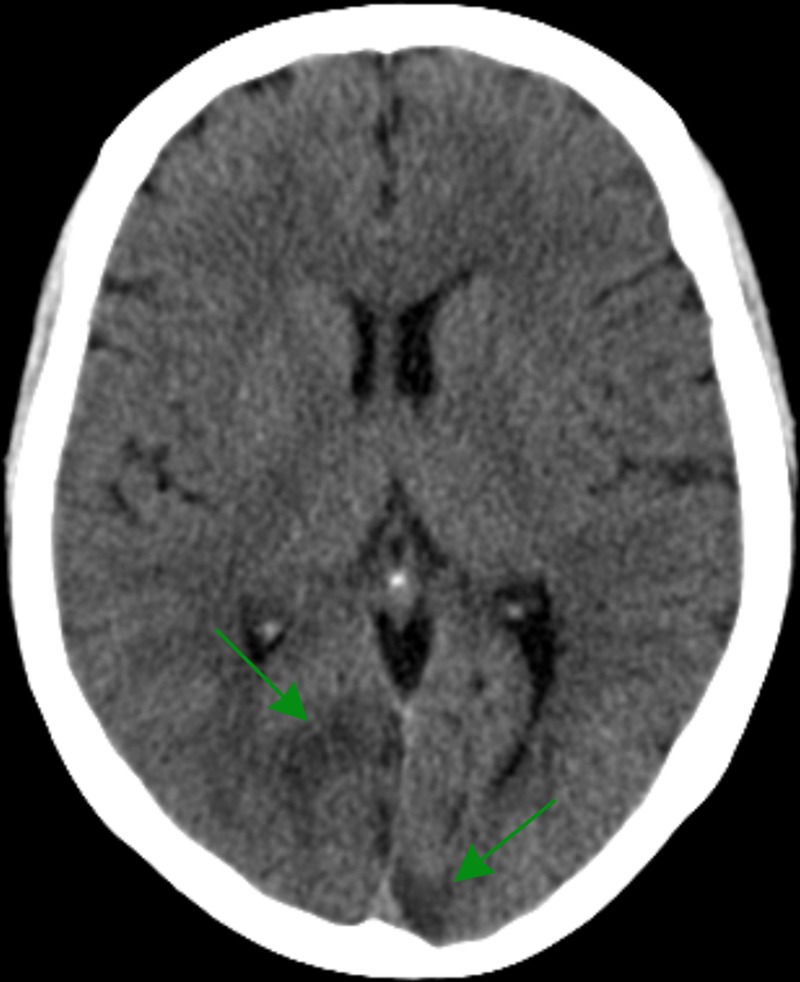
CT scan of the brain. The axial coupes reveal bilateral hypodense lesions occipitally, suspect for subacute cerebral infarctions.
ECG was normal.
MRI scan of the brain, 1 day later demonstrated multiple bilateral infarctions (most prominently in the posterior circulation, figure 2A–C).
Figure 2.
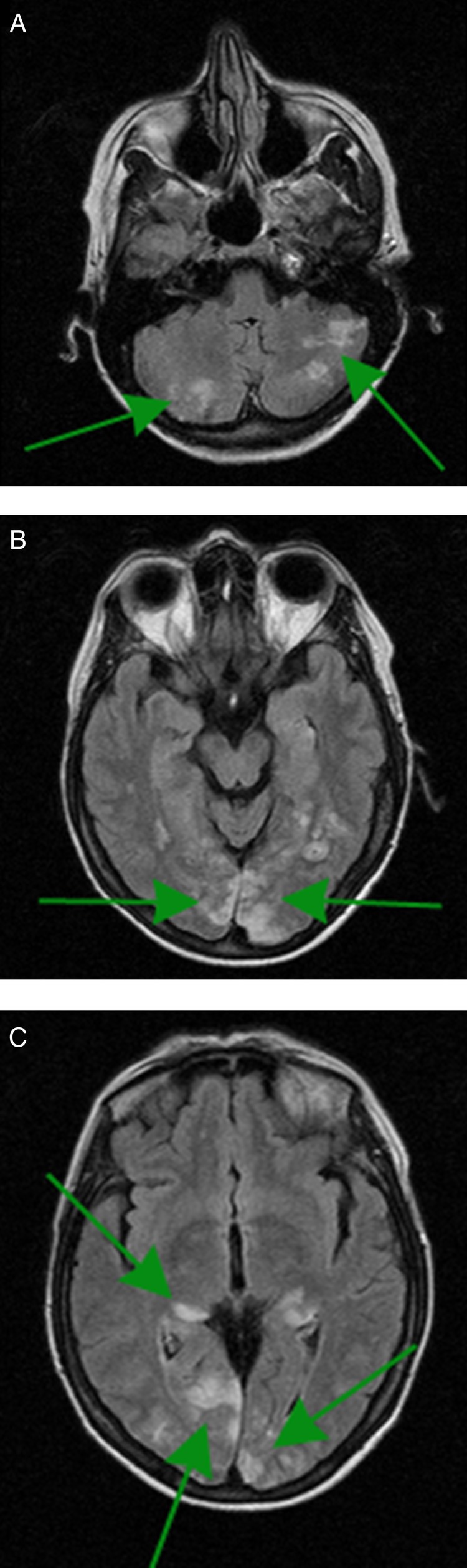
Brain MRI, axial coupes. The fluid-attenuated inversion recovery-weighted images reveal multiple bilateral ischaemic lesions in the cerebellum (A), occipital (B) and the posterior part of the right thalamus (C).
Differential diagnosis
Cardiac emboli.
Giant cell arteritis.
Vasculitis.
Malignancy with tumour emboli, a coagulation disorder, or opportunistic infection.
Treatment
As imaging had demonstrated very recent infarctions, treatment with oral anticoagulation was considered to be associated with a significantly increased risk of intracerebral haemorrhage. Therefore, she was instituted on aspirin, a boost dose of 240 mg followed by a daily dose of 80 mg.
Outcome and follow-up
After 2 days she suddenly developed a left sided visual inattention and ventricular fibrillation with takotsubo cardiomyopathy. The ventricular fibrillation ceased rapidly, without the need for cardiopulmonary resuscitation. Troponin levels increased to a maximum of 1.92 ng/mL (normal value <0.10) and ECG showed atrial fibrillation, which converted to sinus rhythm upon amiodaron and metoprolol. Clopidogrel was then added to the aspirin, as this was considered to carry a lower risk for intracerebral haemorrhage. CT angiography of the aorta ruled out a dissection, however did reveal splenic infarction and pleural fluid. Additional laboratory examination ruled out an auto-immune disorder and septic emboli. Transoesophageal echography showed an immobile cardiac apex with mild valve insufficiency, yet no signs of endocarditis or cardiac thrombus. This finding prompted the need for a more aggressive anticoagulant treatment. Therefore, aspirin and clopidogrel were then substituted with therapeutic fragmin. Both coronary angiography and CT angiography of the carotid and vertebral arteries as well as the circle of Willis demonstrated no abnormalities. As the patient was not known to have any prior cardiovascular risk factors and the angiography did not reveal any abnormalities, a malignancy was considered as a potential underlying cause. Therefore, a positron emission tomography (PET) scan was proposed, which demonstrated a pathological fluorodeoxyglucose uptake suggestive of a pelvic tumour. Hence, CT scan of the thorax and abdomen demonstrated a probable ovarian tumour, with signs of mesenterial lymphadenopathy, ascites and again pleural fluid. Finally, cytologic examination of the ascites and pleural fluid confirmed malignant cells, consistent with metastasised adenocarcinoma derived from the genital tract. Serum analysis showed an elevated Ca-125 level (2385, yet normalcarcinoembryonic antigen).
After initial improvement she further deteriorated, developing expressive aphasia, left sided haemianopsia, decreased motor control and hemi-inattention. An MRI of the brain demonstrated an increase of the ischaemic lesions (figure 3A–C). In spite of adding aspirin to the therapeutic fragmin, she failed to improve. Her condition rendered her unfit for chemotherapeutic treatment. Finally, she died 42 days after the initial hospitalisation.
Figure 3.
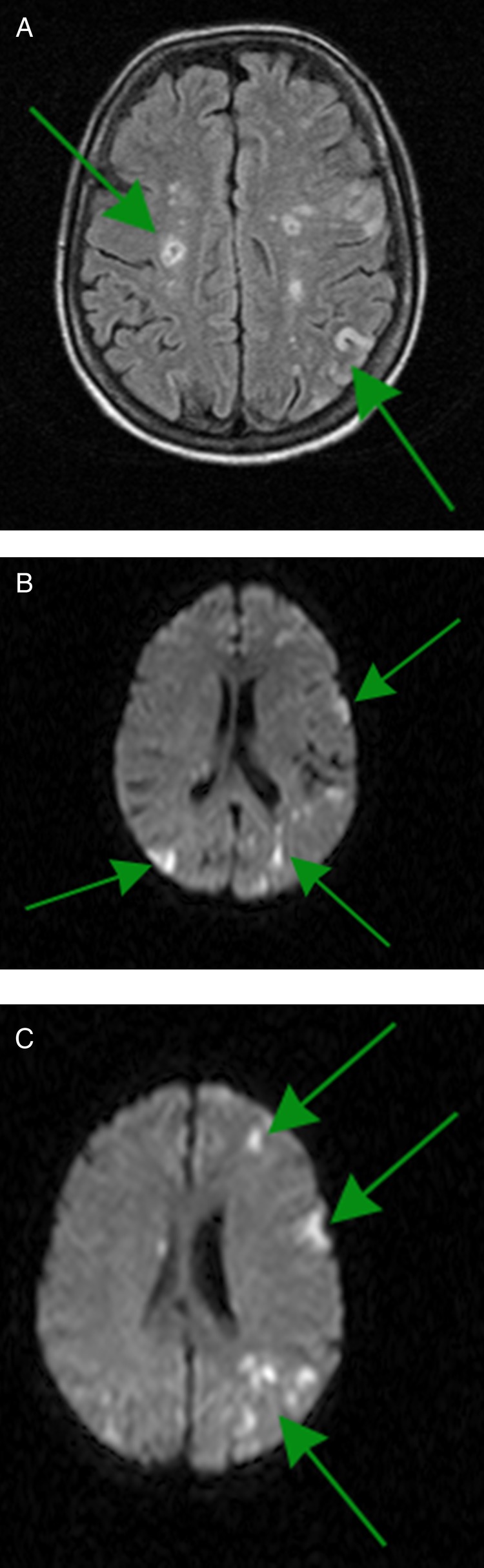
Brain MRI, axial coupes. The fluid-attenuated inversion recovery-weighted images reveal an increase of the bilateral infarctions, involving multiple vascular territories (A); this is also visible on diffusion weighted imaging (B and C), which showed new ischaemic lesions in comparison with initial MRI.
Discussion
At initial presentation, the patient demonstrated ischaemic lesions most prominently in the posterior circulation. Migraine is reported to be associated with increased risk for stroke in women, especially in the posterior circulation like our patient who had a history of migraine.1 However, when ischaemic lesions are distributed among multiple vascular territories, there should be a high suspicion for cardiac emboli, vasculitis or giant cell arteritis.2 At second instance, after deterioration, the patient demonstrated takotsubo cardiomyopathy with atrial fibrillation and an immobile cardiac apex as a potential source of emboli. However, it failed to explain the initial presentation of ischaemic stroke in our patient. Intracranial arterial stenosis, vasculitis and giant cell arteritis are known causes of multiple vascular lesions.2 We ruled out these causes, with extensive imaging and laboratory examinations. Further investigation with PET scan was suggestive for a pelvic tumour, which was confirmed by additional CT scan and ultimately, cytologic examination.
Cerebral ischaemia is one of the manifestations of malignancy associated thrombosis, which occurs frequently.3 4 There are several pathophysiological mechanisms (table 1).
Table 1.
| Stroke type | Specific causes among malignancies |
|---|---|
| Ischaemic | Non-bacterial endocarditis Coagulation disorder (paraneoplastic or due to liver metastasis) Tumour infiltration, compression blood vessel Tumour emboli Treatment-related (chemotherapy or radiotherapy) |
| Haemorrhagic | Coagulation disorder (paraneoplastic or due to liver metastasis) Tumour infiltration, compression blood vessel Treatment-related (chemotherapy) Mycotic aneurysm |
| Cerebral venous thrombosis | Coagulation disorder (paraneoplastic, chemotherapy)Opportunistic infections |
Non-bacterial endocarditis can cause infarction of multiple organs.4 5 Furthermore, clotting may be disrupted as a paraneoplastic phenomenon or due to metastasis in the liver, vessels can become occluded by local tumour infiltration or compression and tumour-emboli may give rise to distant infarctions.3–6 Finally, infarctions may be the result of cancer treatment: chemotherapy and radiotherapy are known causes of vessel damage, increase atherosclerosis and increase the vulnerability to superinfections (eg, Aspergillus and Candida species), which may give rise to emboli.3 4 These mechanisms can result in a wide spectrum of clinical cerebrovascular complications: transient ischaemic attack, ischaemic stroke, cerebral venous thrombosis, intracerebral and subarachnoid haemorrhage.3 4 Laboratory examinations in patients with stroke due to cancer may reveal elevated levels of fibrinogen and D-dimers.6–9 Therefore, it is recommended to determine coagulation parameters in selected cases of ischaemic stroke, in order to identify a malignancy as underlying cause.6–9 More importantly, as in the presented case, brain MRI typically shows ischaemic lesions that involve multiple vascular territories.8 Ischaemic stroke as the initial presentation of systemic malignancy, as in the presented case, is reported infrequently.9–12 This is likely to be underestimated, since extensive analysis to underlying causes of stroke is mainly limited to the younger patients. Borowski et al,11 Taccone et al12 and recently Tadokoro et al9 reported stroke as a first manifestation of ovarian cancer. Similar to our case, they found bihemispheric infarctions and the course was complicated by early stroke recurrence. In their series on 24 patients with stroke as a first manifestation of cancer, Taccone et al12 found a median survival of 58 days. They also found a strikingly high rate of recurrence, in spite of treatment, which obviously negatively influences outcome.12 Owing to the diversity of the underlying malignancies, there are no uniform guidelines to treat this group of patients. Treatment should primarily be aimed at the malignancy and anti-platelet/coagulative therapy tailored on a case-by-case basis. However, both the available literature and the presented case illustrate that this may still fail to prevent further recurrences.
Learning points.
Every patient who present with an ischaemic stroke, in which the lesions exceed the territory of a single vessel—in which cardiac emboli, vasculitis or giant cell arteritis have been ruled out—should be considered as possibly having a systemic malignancy.
The combination elevated levels of fibrinogen and D-dimers with multiterritorial ischaemic lesions may help to identify malignancy as underlying cause.
Early stroke recurrence is frequent in patients with malignancy, which also contributes to the poor prognosis.
Footnotes
Contributors: SHG was the primary physician and wrote the main part of the manuscript. AN was the consulting physician and critically revised the manuscript. JMPR was a second physician and critically revised the manuscript. GR was the attending supervisor and critically revised the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kruit MC, Launer LJ, Ferrari MD, et al. Infarcts in the posterior circulation territory in migraine. The population-based MRI CAMERA study. Brain 2005;128(Pt 9):2068–77 [DOI] [PubMed] [Google Scholar]
- 2.Rovira A, Grive E, Alvarez-Sabin J. Distribution territories and causative mechanisms of ischemic stroke. Eur Radiol 2005;15:416–26 [DOI] [PubMed] [Google Scholar]
- 3.Arboix A. Cerebrovascular disease in the cancer patient. Rev Neurol 2000;31:1250–2 [PubMed] [Google Scholar]
- 4.Rogers LR. Cerebrovascular complications in patients with cancer. Semin Neurol 2010;30:311–19 [DOI] [PubMed] [Google Scholar]
- 5.Alvarez-Perez FJ, Verde I, Uson-Martin M, et al. Frequency and mechanism of ischemic stroke associated with malignancy: a retrospective series. Eur Neurol 2012;68:209–13 [DOI] [PubMed] [Google Scholar]
- 6.Schwarzbach CJ, Schaefer A, Ebert A, et al. Stroke and cancer: the importance of cancer-associated hypercoagulation as a possible stroke etiology. Stroke 2012;43:3029–34 [DOI] [PubMed] [Google Scholar]
- 7.Isenegger J, Meier N, Lammle B, et al. D-dimers predict stroke subtype when assessed early. Cerebrovasc Dis 2010;29:82–6 [DOI] [PubMed] [Google Scholar]
- 8.Kim SJ, Park JH, Lee MJ, et al. Clues to occult cancer in patients with ischemic stroke. PloS One 2012;7:e44959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tadokoro Y, Sakaguchi M, Yagita Y, et al. Ischemic stroke in patients with solid gynecologic tract tumors and coagulopathy. Eur Neurol 2013;70:304–7 [DOI] [PubMed] [Google Scholar]
- 10.Ideguchi H, Ohno S, Ueda A, et al. Catastrophic antiphospholipid syndrome associated with malignancies (case report and review of the literature). Lupus 2007;16:59–64 [DOI] [PubMed] [Google Scholar]
- 11.Borowski A, Ghodsizad A, Gams E. Stroke as a first manifestation of ovarian cancer. J Neurooncol 2005;71:267–9 [DOI] [PubMed] [Google Scholar]
- 12.Taccone FS, Jeangette SM, Blecic SA. First-ever stroke as initial presentation of systemic cancer. J Stroke Cerebrovasc Dis 2008;17:169–74 [DOI] [PubMed] [Google Scholar]


