Abstract
Background: Readmissions after pancreatectomy, largely for the management of complications, may also occur as a result of failure to thrive or for diagnostic endeavours. Potential mechanisms to reduce readmission rates may be elucidated by assessing the adequacy of the initial disposition and the real necessity for readmission.
Methods: Using previously identified categories of readmission following pancreatectomy, details of reasons for and results of readmissions were scrutinized using a root cause analysis approach.
Results: Of 658 patients subjected to pancreatectomy between 2001 and 2010, 121 (18%) were readmitted within 30 days. The clinical course in 30% of readmitted patients was found to deviate from the pathway assumed on the initial admission. Patients were readmitted at a median of 9 days (range: 1–30 days) after initial discharge and had a median readmission length of stay of 7 days (mode = 4). Postoperative complications accounted for most readmissions (n = 77, 64%); 17 patients (14%) were readmitted for failure to thrive and 16 (13%) for diagnostics. Root cause analysis detailed subtextual reasons for readmission, including, for example, the initiation of new medications that could potentially have been ordered in an outpatient setting.
Conclusions: More than one quarter of readmissions after pancreatectomy occurred in the setting of failure to thrive or for diagnostic evaluation alone. Root cause analysis revealed potentially avoidable readmissions. The development of a system for stratifying patients at risk for readmission or the failure of the initial disposition, along with an alternative means of efficiently evaluating patients in an outpatient setting, could limit unnecessary readmissions and resource utilization.
Introduction
An increasing focus on value-based care, in the setting of changes in reimbursement, has resulted in an emphasis on hospital readmission rates as a source of increased costs and as a surrogate for quality.1 In the USA, postoperative readmission rates have not yet been specifically targeted at the federal level, but, at an institutional level, high readmission rates after surgery are increasingly viewed as an indicator of inferior quality. Readmission is clearly implicated as a driver of overall hospital costs; a recent US study on readmission after pancreatectomy identified an average cost increase of US$16 000 per readmission.2 Furthermore, readmission following surgical management of colon cancer has been linked to worse survival according to data sourced from the Surveillance, Epidemiology and End Results (SEER) Medicare database.3 In that setting, the authors concluded that readmission rates represent a measure of quality after colon cancer surgery.3 However, the interpretation of readmission rates following complex gastrointestinal (GI) surgery such as pancreatectomy may need to incorporate other factors. A recent editorial by Brown et al. considers whether higher readmission rates by surgeons reflect a failure of surgical care or whether, alternatively, they ought to be considered as representative of ‘rescue’ care (i.e. the provision of good quality care of a complication).4
Previous work has identified readmission rates following pancreatectomy in the range of 15–59%, including 19% in a recent paper by the present authors.2,5–9 Although little work has been published on the reduction of readmission rates after pancreatectomy, a multitude of initiatives underway across the USA are attempting to ease the transition from hospital to the outpatient setting in other, more common diagnoses.10,11 Postoperative readmissions following complex GI surgical procedures commonly occur as a result of complications. However, after pancreatectomy, recent work delineated other reasons for readmission. Although approximately two thirds of readmissions occurred as a result of postoperative complications, a quarter of readmissions occurred because of failure to thrive or to facilitate diagnostic endeavours.2 Although efforts to decrease the incidence of postoperative complications, notably of pancreatic fistula, continue, care providers may be able to identify potential mechanisms to reduce readmission rates by assessing the adequacy of the initial disposition and the real necessity for readmission.
This group's initial study of readmission after pancreatectomy2 was completed to identify the clinical nature and economic impact of such readmissions. The present study was designed to assess the adequacy of the initial disposition after pancreatectomy and to investigate the details of, reasons for and results of readmissions of patients after major pancreatic resection using a root cause analysis approach to identify potential targets for intervention. This study was undertaken with a longterm goal of effecting positive change on the transitions of care following pancreatectomy through interventions that serve to both reduce hospital costs and improve the quality of patient care and patient satisfaction.
Materials and methods
Using a prospectively collected database, all patients undergoing pancreatectomy over a 10-year period (2001–2010) were identified. All patients who required readmission were then identified by searching the electronic database. Patient charts, including physician, nursing, physical therapy and patient case management records, for all of these patients were reviewed in detail and a standardized datasheet was utilized to supplement previously recorded data. This included details of patient disposition, deviations from the standardized pathway, subjective cause(s) of readmission, therapeutic interventions resulting from readmission, length of stay (LoS) and type of secondary discharge. Once these data were available, the cases were evaluated utilizing the root cause analysis storytelling methodology and the failure modes and effect analysis tool (FMEA)12 to determine the root causes of the readmission, as well as whether the admission had been warranted or potentially avoidable, and where the failures occurred in the discharge and disposition planning system. Storytelling methodology entails definition of the problem, description of the event, details of who or what made or caused a mistake (where applicable), and details of what can be done to prevent this event from occurring again.12 In FMEA, a component of the system is identified and possible failures together with their respective effects are noted.12
Data were collected on a standardized datasheet and analysed using spss Version 20 for MAC (IBM Corp., Armonk, NY, USA). Descriptive statistics were tabulated. Qualitative and descriptive analysis was utilized to categorize the ‘failures’ or readmissions via the storytelling and FMEA methods, deconstructing the sequence of events leading to the initial discharge disposition, the readmission and the secondary discharge. The frequency of cause for readmission was categorized in the same manner as previously published,2 although several patients were re-categorized in this paper as per a more stringent review of the details surrounding the readmission (Table 1). In retrospect, each readmission was reviewed to determine whether it had been potentially avoidable and at which points interventions could have been made. The causes of failure (here, considered as readmission) were noted and categorized for each event.
Table 1.
Categories of readmission
| Root cause | Definition |
|---|---|
| General or operation-specific complication | Readmission directly related to complications of the initial operation such as abscess formation, wound infections, etc. |
| Failure to thrive | Readmission related to loss of functional status following the index operation, such as weight loss or inability to perform activities of daily life in the absence of evident postoperative complication |
| Previously existing medical comorbidity | Readmission for management of previously existing comorbidities, such as diabetes |
| Unrelated | Readmission for indications completely unrelated to the index operation |
| Diagnostic evaluation or unknown | Readmission for evaluation with no complication identified |
Results
Over the 10-year period between 2001 and 2010, 658 pancreatectomies were performed and 121 patients were readmitted for any reason, resulting in an all-cause readmission rate of 18%. The clinical course in 36 (30%) readmitted patients was found to deviate from the pathway assumed at their index admission. The median time to readmission was 9 days (range: 1–30 days) and the median LoS after readmission was 7 days (mode = 4; range: 1–45 days). The median LoS for readmission was 5 days in patients in the failure-to-thrive group and the diagnostics group, and 3 days in patients in the complication group (P = 0.051).
Of the readmitted patients, 58 (48%) had been discharged to home with services (medication administration, drain care, tube feeds or parenteral nutrition) and 14 (12%) patients had been discharged to rehabilitation. Forty-three (36%) patients had been discharged to home. Note that in six (5%) patients, the initial disposition was not known. After readmission, 26 (21%) patients required an escalation in their post-discharge care and 16 (13%) required the initiation of home services.
Postoperative complications represented the most common cause of readmission (n = 77, 64%), followed by failure to thrive (n = 17, 14%), diagnostic evaluation (n = 16, 13%), and previously existing comorbidities or unrelated medical factors (n = 11, 9%). Table 2 lists the causes of readmission identified according to whether readmission was potentially avoidable or probably unavoidable. Table 3 provides several examples of storytelling methodology as it applies to the root cause analysis. Figure 1 demonstrates the critical points along a patient's course at which decisions on disposition are made or at which failure might occur. A qualitative review of records regarding decision making on disposition revealed a paucity of detailed information on the patient's and his or her family's capacity to manage at home, other than the routine physical and occupational therapy evaluation of ambulation and stair-climbing ability. Of the 96 readmitted patients for whom sufficient data were available, 60 (63%) definitely required readmission, whether or not the situation leading to the subsequently necessary admission had been potentially avoidable (through successful efforts relating to the themes to be outlined). In 25 (26%) patients, readmission had been potentially avoidable. In 11 (11%) patients, the problems for which the patients were readmitted could have been considered for inpatient or outpatient management depending on resources. The combination of storytelling and FMEA resulted in the identification of themes associated with ‘failure of discharge’ (i.e. readmission) that can be utilized to develop appropriate interventions to prevent recurrence of the failure. In addition to the expected intraoperative or postoperative outcomes, these analyses revealed: insufficient oral intake or an under-appreciated insufficiency of nutrition (or nutrition that was changed after discharge); inaccurate assessment of the patient's or his or her family's capacity to manage after discharge in terms of resources and available help; errors in the assessment of the patient's ability to complete the activities of daily life, and under-appreciation of the patient's need for help in managing drains or medications. These can be grouped into: failure in the assessment of the patient's and his or her family's ability to meet needs at home (17 patients); failure to clarify expectations with patients, families and visiting nurses (21 patients), and failure to ensure adequate communication with subsequent or local care providers (15 patients). Seven readmissions occurred because no urgent outpatient evaluation was available and six occurred because the patients required nutritional support that could have been provided in an outpatient setting.
Table 2.
Events prompting readmission and failure analysis (not mutually exclusive)
| Probably necessary readmission | Potentially avoidable readmission |
|---|---|
| Initiation of antibiotic for infectious process | Diagnostic evaluation without acute process identified (sometimes in the setting of a transfer from a distant facility) |
| Initiation of insulin | Initiation of oral medication |
| Initiation of enteral or parenteral feeds | Inadequate support at home (self-care, meals, nutrition) |
| Intravenous hydration or resuscitation | Inadequate pain control |
| Percutaneous drain placement | Visiting nurse concern prompting emergency department evaluation as a result of lack of available urgent outpatient evaluation |
| Feeding tube placement (endoscopic) | Patient or family concern prompting emergency department evaluation as a result of lack of available urgent outpatient evaluation |
| Reoperation | Transfer from outside facility with re-interpretation of imaging results |
Table 3.
Examples of storytelling methodology in the evaluation of readmissions
| Example 1 |
|
| PROBABLY AN AVOIDABLE READMISSION | |
| Example 2 |
|
| Example 3 |
|
ED, emergency department
Figure 1.
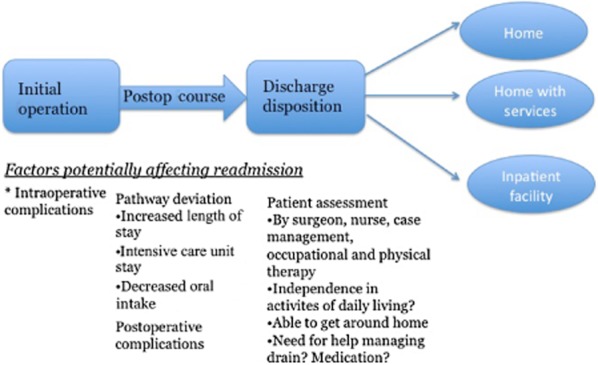
Flow diagram indicating the patient course and points at which problems might potentially occur or deviations from the usual course arise to prompt readmission
Discussion
Since 2009, the Center for Medicare and Medicaid Services has required hospitals to report 30-day hospital readmission rates for common medical conditions such as pneumonia, heart failure and myocardial infarction.13,14 This is the first step in a two-step policy option designed to encourage hospitals to reduce readmission rates. Medicare is considering complementing this with a change in payment rates so that hospitals with high risk-adjusted rates of readmission will receive a lower average per case payment.15 The Patient Protection and Affordable Care Act affords the Centers for Medicare and Medicaid Services the authority to penalize hospitals that show excessive readmission rates beginning in 2013 and strict policies in this regard are expected to be implemented.16 Initial efforts will focus on cases of heart failure, pneumonia and acute myocardial infarction, and will be extended to chronic obstructive pulmonary disease, coronary artery bypass grafts, percutaneous coronary interventions and vascular surgery procedures in 2015.16 Post-pancreatectomy readmission is not yet on the table for federal quality incentives. However, economic and regulatory pressures force physicians to continually re-evaluate their processes of care, including the transitions to postoperative outpatient follow-up, with the goals of improving quality and decreasing costs.
Although this study's sample includes patients represented as readmissions in an earlier study,2 the present study focuses specifically on the readmitted patients, refers to data points not previously investigated, and represents an outgrowth from the former paper2 and its initial findings. The present study confirms the finding that complications continue to underlie the majority of readmissions after pancreatectomy despite the fact that clinical care during the initial hospitalization of patients in this study follows a pathway that includes defined milestones that determine a patient's eligibility for discharge after his or her initial stay. Only when patients deviate from this pathway does their initial LoS differ from that of a typical post-pancreatectomy patient at this institution. Patients can deviate from the pathway for several reasons, such as the development of pneumonia or wound infection, as well as difficulty in identifying appropriate rehabilitation facilities or in approving home services. The clinical pathway calls for discharge at postoperative day 8; there is no push for earlier discharge. In fact, prior studies by the same group note a consistent median LoS of 7–8 days.2,17 A contemporary multicentre analysis reported an initial LoS of 9–10 days after pancreaticoduodenectomy18 and another noted a hospital stay of 7 days following distal pancreatectomy.19
However, nearly one third of readmissions occurred either in the setting of failure to thrive or in response to a need for diagnostic evaluation, without the identification of an acute process to justify hospital-level care. This group of patients stayed longer in hospital when readmitted than those with a complication. The reason for this difference is not well delineated in the current study, but may reflect the difficulty of developing an appropriate post-discharge care plan in patients who fail to thrive in particular, as specific needs must be assessed and resources identified to meet those needs. Particularly when the second discharge is associated with an escalation in need for services, case managers must work with the patient's insurance providers to identify the services covered and to secure their provision.
These data illustrate several points of failure in the current discharge planning system, including problems in communicating with other care providers and with the patient and his or her family, problems in establishing expectations, and problems in determining the patient's capacity to care for him-or herself. Furthermore, an important distinction among readmissions arises: some readmissions were potentially avoidable given the situation in which they occurred, and alternatives to readmission in such contexts may exist. In other cases, the situation prompting readmission was potentially avoidable, but once that situation had occurred, readmission became necessary. This distinction deserves consideration in the 63% of readmissions deemed necessary as these involved patients who had developed complications and were readmitted, and patients whose expectations, understanding and evaluation had been appropriate, as well as those in whom failures in setting expectations or in understanding, or failures of communication had led to the development of the problem for which the patient required readmission. Thus, the information becomes difficult to quantify well. It is difficult to make a retrospective definition of inadequate disposition, but factors identified in this study suggest that the current process may not be sufficient.
Discharge disposition
Nearly half of the patients in the readmitted group had initially been discharged home with services. This finding is consistent with a recent study of the changes over time in discharge disposition after pancreatectomy, which show that, nationally, over the last 22 years, the number of patients discharged to home has decreased, and, correspondingly, the numbers of patients discharged with home services or to inpatient facilities have increased.20 The present authors theorize that this may reflect the fact that sicker patients now qualify for pancreatectomy because mortality has declined. Readmission rates are significantly greater for those discharged home with services compared with those discharged home without services or to an inpatient facility.2 This may indicate that such patients are sicker or weaker at baseline, or perceived by providers to be at higher risk for a complication. By contrast, previous work on visiting nursing services has demonstrated that the visiting nurse, although able to assess the patient's status, has a limited ability to treat an identified problem.21 Therefore, concerns may prompt presentation for urgent evaluation and possible readmission.
As noted, the level of detail recorded and available for analysis regarding the determination of the initial disposition was fairly limited in comparison with the issues revealed at the time of readmission. A standard form is employed by case management staff, but this does not include detailed questions about the family resources available to the patient at home after discharge at the level identified as problematic upon readmission. This finding suggests that more detailed analysis of the patient's and family's resources for the provision of self-care at home may be helpful, in addition to measures already taken to assess these resources. In further support of this process, a study of health care providers reported that effective discharge planning was considered to include standardized discharge planning, as well as multidisciplinary efforts and communication amongst different care providers.22
Clarification of expectations and communication
Readmissions occurred because patients, families and visiting nurses were concerned about a problem when, in fact, the situation creating concern represented the patient's expected postoperative status. In addition, in several cases, patients were sent back to the hospital for admission by a concerned visiting nurse, facility provider or the patient or his or her family for reasons (e.g. poor oral intake, drain output) that had been present and accounted for at the time of index discharge. These cases reflect differences in expectations among patients, their families, visiting nurses and surgical staff, or failures in communication. Previous work on the effectiveness of case management found that a case management intervention targeting clearer patient discharge instructions was effective in limiting 30-day readmissions.10 Additional efforts might include establishing clearer postoperative expectations by educating visiting nurses and facility staff. Furthermore, a meta-analysis found pre-discharge interventions such as patient education, medication reconciliation, discharge planning and scheduling a follow-up appointment before discharge to be efficacious.11 Post-discharge interventions, including follow-up telephone calls, patient-activated hotlines, timely communication with ambulatory providers and home service providers, timely ambulatory provider follow-up and post-discharge home visits, and bridging interventions, including the provision of transition coaches, physician continuity across the inpatient and outpatient settings, and patient-centred discharge instruction, were also effective.11
System for re-evaluating patients with potential problems
Several readmissions occurred after an emergency department visit at night or at the weekend for what might potentially be evaluated in an outpatient setting. The increasing emphasis on the patient with ‘observation’ status may help in this area. However, other potentials for intervention include the initiation of an urgent drop-in clinic for postoperative patients, as well as increasing the frequency of postoperative calls to the patient and family to check on the patient's progress and address any concerns. These possibilities might be particularly useful in decreasing readmission in the group of patients in whom diagnostics are required, but in whom an acute process is not identified, and in those who demonstrate failure to thrive. For these latter patients, the earlier identification of patients at risk and patients who begin to fail at home could prompt outpatient evaluation by a physician and a nutritionist in order to address nutritional support.
Conclusions
This root cause analysis has again confirmed that postoperative complications remain the most common reason for readmission in this patient population and thus ongoing efforts to limit the occurrence of these complications is imperative. Readmission may be required for the optimal management of these patients, and physicians and hospital systems providing responsible care for these patients should not be penalized for doing so. Nonetheless, there are clearly several areas in which interventions may be able to reduce the rate of avoidable readmissions, such as through efforts to obtain a more detailed assessment of a patient's home support system, to clarify the patient's understanding of postoperative expectations, to develop alternative means of urgent evaluation (such as a drop-in clinic), and to develop effective strategies centred on ensuring nutritional support.
This study highlights the intricate glitches in the current system of care. Certainly, many patients who are readmitted require to be and medical care providers should not be penalized for caring for their patients well. However, there is room for improvements that could streamline patient care and improve quality. Innovative efforts to develop alternative means of evaluation and to achieve a better understanding of expectations in patients, their families and other providers are necessary.
Conflicts of interest
None declared.
References
- 1.Fischer C, Anema HA, Klazinga NS. The validity of indicators for assessing quality of care: a review of the European literature on hospital readmission rates. Eur J Public Health. 2012;22:484–491. doi: 10.1093/eurpub/ckr165. [DOI] [PubMed] [Google Scholar]
- 2.Kent TS, Sachs TE, Callery MP, Vollmer CM., Jr Readmission after major pancreatic resection. J Am Coll Surg. 2011;213:515–523. doi: 10.1016/j.jamcollsurg.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 3.Greenblatt DY, Weber SM, O'Connor ER, LoConte NK, Liou JI, Smith MA. Readmission after colectomy for cancer predicts one-year mortality. Ann Surg. 2010;251:659–669. doi: 10.1097/SLA.0b013e3181d3d27c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown RE, Qadan M, Martin RC, II, Polk HC., Jr The evolving importance of readmission data to the practising surgeon. J Am Coll Surg. 2010;211:558–560. doi: 10.1016/j.jamcollsurg.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 5.Reddy DM, Townsend CM, Kuo YF, Freeman JL, Goodwin JS, Riall TS. Readmission after pancreatectomy for pancreatic cancer in Medicare patients. J Gastrointest Surg. 2009;13:1963–1975. doi: 10.1007/s11605-009-1006-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Emick DM, Riall TS, Cameron JL, Winter JM, Lillemoe KD, Coleman J, et al. Hospital readmission after pancreaticoduodenectomy. J Gastrointest Surg. 2006;10:1243–1253. doi: 10.1016/j.gassur.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 7.Balcom JH, 4th, Rattner DW, Warshaw AL, Chang Y, Fernandez-del-Castillo C. Ten-year experience with 733 pancreatic resections: changing indications, older patients, and decreasing length of hospitalization. Arch Surg. 2001;136:391–398. doi: 10.1001/archsurg.136.4.391. [DOI] [PubMed] [Google Scholar]
- 8.Porter GA, Pisters PW, Mansyur C, Bisanz A, Reyna K, Stanford P, et al. Cost and utilization impact of a clinical pathway for patients undergoing pancreaticoduodenectomy. Ann Surg Oncol. 2000;7:484–489. doi: 10.1007/s10434-000-0484-0. [DOI] [PubMed] [Google Scholar]
- 9.Yermilov I, Bentrem D, Sekeris E, Jain S, Maggard MA, Ko CY, et al. Readmissions following pancreaticoduodenectomy for pancreas cancer: a population-based appraisal. Ann Surg Oncol. 2009;16:554–561. doi: 10.1245/s10434-008-0178-6. [DOI] [PubMed] [Google Scholar]
- 10.Schmeida M, Savrin RA. Pneumonia rehospitalization of the Medicare fee-for-service patient: a state-level analysis: exploring 30-day readmission factors. Prof Case Manag. 2012;17:126–131. doi: 10.1097/NCM.0b013e31823be14d. [DOI] [PubMed] [Google Scholar]
- 11.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 12.Gano DL, Gano DL. Apollo Root Cause Analysis – A New Way of Thinking. 3rd edn. Yakima, WA: Apollonian Publications; 2007. Comparison of common root cause analysis tools and methods; pp. 179–194. [Google Scholar]
- 13. Centers for Medicare and Medicaid Services. Fiscal year 2009 quality measure reporting for 2010 payment update. Available at http://www.cms.hhs.gov/apps/media/fact_sheets.asp (last accessed 12 August 2012)
- 14.Medicare Payment Advisory Committee. Report to the Congress: promoting greater efficiency in Medicare, ch. 5: payment policy for inpatient readmissions. Available at http://www.medpac.gov/chapters/jun07_ch05.pdf (last accessed 12 August 2012)
- 15.Foster DF, Harkness G. Healthcare reform: pending changes to reimbursement for 30-day readmissions. Available at http://thomsonreuters.com/content/healthcare/pdf/pending_changes_reimbursements (last accessed 12 August 2012)
- 16.Kent TS, Sachs TE, Callery MP, Vollmer CM., Jr The burden of infection for elective pancreatic resections. Surgery. 2013;153:86–94. doi: 10.1016/j.surg.2012.03.026. [DOI] [PubMed] [Google Scholar]
- 17.Ahmad SA, Edwards MJ, Sutton JM, Grewal SS, Hanseman DJ, Maithel SK, et al. Factors influencing readmission after pancreaticoduodenectomy: a multi-institutional study of 1302 patients. Ann Surg. 2012;256:529–537. doi: 10.1097/SLA.0b013e318265ef0b. [DOI] [PubMed] [Google Scholar]
- 18.Rosales-Velderrain A, Bowers SP, Goldberg RF, Clarke TM, Buchanan MA, Stauffer JA, et al. National trends in resection of the distal pancreas. World J Gastroenterol. 2012;18:4342–4349. doi: 10.3748/wjg.v18.i32.4342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah BC, Smith LM, Ullrich F, Are C. Discharge disposition after pancreatic resection for malignancy: analysis of national trends. HPB. 2012;14:201–208. doi: 10.1111/j.1477-2574.2011.00427.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hughes LC, Robinson LA, Cooley ME, Nuamah I, Grobe SJ, McKorkle R. Describing an episode of home nursing care for elderly post-surgical cancer patients. Nurs Res. 2002;51:110–118. doi: 10.1097/00006199-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Wong EL, Yam CH, Cheung AW, Leung MC, Chan FW, Yeoh EK. Barriers to effective discharge planning: a qualitative study investigating the perspectives of frontline healthcare professionals. BMC Health Serv Res. 2011;11:242. doi: 10.1186/1472-6963-11-242. [DOI] [PMC free article] [PubMed] [Google Scholar]


