Abstract
Introduction
Epidemiological studies consistently show an initial survival advantage for PD patients compared to HD. It has recently been suggested that this is due to the fact that many HD patients are referred late, and start dialysis on an acute, in-patient basis. The present study was performed to investigate (1) whether, and if so, how, PD and HD prognosis had changed in recent years, (2) whether a potential survival advantage of PD versus HD is constant over dialysis duration, and (3) whether differences in prognosis could be explained by patient age, renal diagnosis of diabetic nephropathy, or mode of dialysis initiation.
Patients and Methods
12095 patients starting dialysis therapy between 1990 and 2010 in Denmark were studied. Prognosis was assessed according to initial dialysis modality on an intention-to-treat basis, censored for transplantation. Results were adjusted for age, sex, renal diagnosis, Charlson Comorbidity Index (CCI), and mode of dialysis initiation.
Results
Overall adjusted prognosis improved by 34% (HD 30%, PD 42%). PD prognosis relative to HD improved, and was 16% better at the end of the period. Final PD prognosis improved consistently from 1990–99 to 2000–10 in all subgroups. PD was associated with a significant initial survival advantage, both overall and for all subgroups For the latter cohort, overall PD prognosis was better than HD for the first 4 years, after which it was insignificantly worse. The initial survival advantage was also present in a subgroup analysis of patients with early & routine ESRD initiation.
Conclusions
Dialysis survival has increased during the past 20 years. PD survival since 2000 has been better than HD, overall and for all subgroups. The difference in survival is not explained by mode of dialysis initiation.
Introduction
The relative survival of end stage renal disease (ESRD) patients treated with peritoneal dialysis (PD) and hemodialysis (HD) has received much epidemiological interest in recent years [1]–[25]. Most studies [1], [2], [5], [8]–[11], [14], [15], [20], [22], [25] show a relative survival advantage for patients receiving PD lasting 1–2 years after dialysis initiation. Results in the long term differ, some showing identical survival [1], [20], [22], [25] and others [4], [6]–[10], [15], [19] showing poorer survival on PD.
This consensus has recently been challenged. The ANZA [19] study showed poorer survival for PD patients than a comparison group of center-HD and home-HD patients, Another paper by Quinn et al. [22] studied a subgroup of patients with early and routine referral to a nephrologist, i.e. the group that is most likely to have made an informed choice between the two therapies, and not have it forced upon them. In this group there was no survival difference between the two groups. The suspicion arises that the initial survival disadvantage of HD patients could be due to mode of ESRD initiation, with associated acute morbidity, that may be unrecorded in registry studies.
The Danish Nephrology Registry (DNR) is a prospective, national, incident registry of all patients receiving active ESRD therapy. It was established on 1.1.1990, and has a data completeness of >99% [26]. The present study was performed to answer the following questions:
Has there been any change in the relative survival of PD versus HD since 1990?
Is the (potential) survival advantage of PD versus HD constant over dialysis duration?
How is PD prognosis in subgroups of patients with diabetic nephropathy, patients older than 65 years, and patients with an early (>90 days before ESRD) and routine ESRD initiation.
Patients and Methods
Patients
All patients resident in Denmark, and thus possessing a national identity number, starting active treatment with dialysis for ESRD between 1.1.1990 and 31.12.2010 were included in the study. Patients receiving a preemptive transplant were not included. Data were extracted from the following databases:
The Danish Nephrology Registry (DNR) contains data from all patients starting active treatment in Denmark. A patient is regarded as having ESRD if (a) the nephrologist considers him/her to have ESRD on the day of first active treatment or later; (b) a renal transplant is performed; (c) there is some doubt regarding the reversibility of the uraemia (e.g. crescentic glomerulonephritis, acute tubulointerstitial nephropathy), but the patient has received at least 90 days of dialysis. Patients were included if (a) their first ESRD therapy was between 1.1.1990 and 31.12.2010; (b) their first ESRD therapy was PD or HD. The following data was extracted: patient age, sex, renal diagnosis, initial therapy (PD/HD), therapy at 90 days, and all changes of therapy. Renal diagnosis was classified as unknown, glomerulonephritis, chronic interstitial nephritis (including chronic pyelonephritis and post-renal uremia), polycystic kidneys, hypertensive nephropathy, Type 1 diabetic nephropathy, type 2 diabetic nephropathy, renal cancer, myeloma, amyloidosis, systemic glomerulonephritis, vasculitis, hæmolytic uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP) and other. This is a multicenter study covering all 15 dialysis centres in the country and their satellite units.
Discharge diagnoses for all admissions to public hospitals in Denmark between 1977–2010 were extracted from the National Patient Registry (LPR). A modified Charlson Comorbidity Index (CCI) [27] at ESRD was calculated, removing the contribution of the original categories based on diabetes and renal disease from the score calculation. Our CCI takes into account the presence of the following comorbid conditions: previous myocardial infarction (AMI), cardiac insufficiency, peripheral atherosclerosis, cerebrovascular disease, dementia, chronic lung disease, collagenosis, stomach ulcer, liver disease, hemiplegia, cancer, leukemia, lymphoma, liver failure, metastatic disease, AIDS [28]. Since hospital care is public in Denmark, the coverage of this database is essentially 100% [29], [30].
Details of patient referral were extracted from LPR. The date of first consultation at a specialist nephrology department was registered. Referrals were classified as early if the first consultation was >90 days before ESRD and late if it was <91 days. Therapy initiation was acute if the first ESRD therapy was as an in-patient and routine if it was as an out-patient. Patients were grouped as either Early & Routine (E&R), Late & Acute (L&A), and other. The LPR has registered referral dates and consultation dates for all in-patient and out-patient referrals and has been comprehensive since 1992. Data for the years 1990–1991 was incomplete.
Methods and statistical analysis
Since most modality changes are from PD to HD, and are associated with increased mortality after change, an “as treated” model is unsuitable for this subject. Patient survival was therefore assessed on an intention-to-treat basis - only the first dialysis course was evaluated - using Cox regression models with robust variance estimation as a safeguard against misspecification. All patients were followed until either death, renal transplant or lost-to-follow-up (LTF) (censoring date 1.1.2011). Model 1 included first dialysis modality (PD, HD), cohort (according to date of dialysis initiation: 1990–1994, 1995–1999, 2000–2004, 2005–2010) patient age at date of dialysis initiation (categorized into 0-, 60-, 70- and 80-), sex, renal diagnosis, CCI (categorized into 0, 1–2, > = 3) and type of ESRD initiation (early & routine, late & acute, other). For model 2, age was substituted by the binary age > = 65 years (yes/no), and renal diagnosis was substituted by binary DM diagnosis (yes/no), i.e. patients with and without diabetic nephropathy.
To explore the development of relative survival PD/HD Prior over cohorts, an interaction term for cohort and dialysis modality was subsequently added to model 2.
To study the effect of dialysis duration (since date of dialysis initiation) on the estimated relative survival PD versus HD, a piecewise Cox regression analysis was fitted independently for the following time periods: 0–6, 6–12, 12–18, 18–24, 24–36, 36–48 and >48 months, adjusted for covariates as in model 2 but stratified for cohort (1990–99, 2000–10). Additionally, the time-dependent hazard ratio for PD versus HD based on the scaled Schoenfeld residuals [31] was estimated. We used this method by Grambsch & Therneau (which originally was proposed to check for proportional hazards) to visualize the time-dependency of the hazard ratio. The curves are generated based on Schoenfeld residuals from the (multivariate/adjusted) Cox models separately for each cohort and subgroup. The curves employ a simple Lowess smoother with bandwidth .8.
Subgroup analyses for the last analysis were performed for 1. DM diagnosis (yes), 2. age > = 65 years, 3. patients older than 65 years and with diabetic nephropathy and 4. patients with an early & routine initiation.
A supplementary analysis was performed for those patients who were still on dialysis after 90 days, where the study period started 90 days after ESRD, and the patients were classified according to their dialysis modality on that date. Type of ESRD initiation was not considered in this analysis.
The proportional hazard assumption is violated for modality in the first model, but this is not a major problem. The first model estimates the average hazard ratio over time (since the estimated hazard ratio based on a Cox model is shown to be fairly close to the exact calculation of the average hazard ratio over time). Thus, the true underlying proportional hazard ratio is not measured, just the overall/average effect. The next step was to fit piecewise models, and the last was to show time-dependent hazard ratios. This last method was originally proposed as a model check (violation of proportional hazards) but can conveniently be applied to visualize time-dependency.
Since there was a tendency over cohorts for “increased superiority”, a cohort x modality effect analysis was performed to investigate whether there were any significant effects.
Reported p-values are based on Wald tests. All analyses were done using Stata (StataCorp 2011. Stata Statistical Software: Release 12. College Station TX: StataCorp LP).
Results
The patient characteristics are shown in Table 1. Patients treated with PD were generally younger, with a lower Comorbidity and a more planned ESRD initiation. Type 1 diabetic nephropathy was more prevalent in PD patients and Type 2 less. Average age increased significantly by 10.6 years for HD patients and 5.3 years for PD patients. Over cohorts, mean age ±SD increased from 55.0±15.8 in the cohort 1990–94 (HD: 55.3±16.5; PD: 54.4.±16.6) to 64.0±15.8 in the cohort 2005–10 (HD: 65.9±14.8; PD: 59.7±16.9). Mean CCI rose from 0.9±1.4 in 1990–94 to 1.6±1.8 in 2005–2010. This was not just due to increasing age. The CCI for patients aged 60–69-years rose from 1.3±1.5 to 1.8±1.9, 70–79 years from 1.2±1.6 to 2.1±1.9 and 80+ years from 0.7±1.2 to 2.1±1.7.
Table 1. Patient characteristics N (%) and hazard ratios (HR) together with 95%-confidence intervals (CI) for factors.
| Factor | Model 1: HR (CI) | Model 2: HR (CI) | |||
| Dialysis modality1 | HD | PD | All | ||
| 8273 (68) | 3822 (32) | 12095 (100) | .89 (.84–.93) | .87 (.83–.92)** | |
| Cohort | ** | ** | |||
| 1990–94 | 1099 (13) | 748 (20) | 1847 (15) | 1 (ref) | 1 (ref) |
| 1995–99 | 1877 (23) | 792 (21) | 2669 (22) | .85 (.79–.91)** | .86 (.80–.93)* |
| 2000–04 | 2482 (30) | 1022 (27) | 3504 (29) | .7 (.65–.75)** | .76 (.70–.81)** |
| 2005–10 | 2815 (34) | 1260 (33) | 4075 (34) | .59 (.54–.64)** | .66 (.61–.72)** |
| Age | ** | ||||
| 0–59 | 2961 (36) | 1962 (51) | 4923 (41) | 1 (ref) | |
| 60–69 | 2158 (26) | 975 (26) | 3133 (26) | 1.88 (1.76–2.01)** | |
| 70–79 | 2337 (28) | 697 (18) | 3034 (25) | 2.7 (2.52–2.89)** | |
| > = 80 | 817 (10) | 188 (5) | 1005 (8) | 3.62 (3.3–3.97)** | |
| Age> = 65 | 4335 (52) | 1344 (35) | 5679 (47) | 2.09 (1.99–2.20)** | |
| Female Sex | 3045 (37) | 1449 (38) | 4494 (37) | .98 (.94–1.03) | .99 (.94–1.04) |
| Renal Diagnosis | ** | ||||
| Unknown | 1931 (23) | 852 (22) | 2783 (23) | 1 (ref) | |
| Glomerulonephritis (GN) | 846 (10) | 590 (15) | 1436 (12) | .76 (.69–.84)** | |
| Chronic interstitial (CIN) | 996 (12) | 390 (10) | 1386 (12) | .92 (.85–1) | |
| Polycystic | 504 (6) | 356 (9) | 860 (7) | .73 (.66–.82)** | |
| Hypertensive | 961 (12) | 430 (11) | 1391 (11) | .99 (.91–1.07) | |
| Type 1 DM | 824 (10) | 632 (17) | 1456 (12) | 1.57 (1.44–1.71)** | |
| Type 2 DM | 998 (12) | 284 (7) | 1282 (11) | 1.41 (1.30–1.52)** | |
| Renal Cancer | 136 (2) | 19 (0.5) | 155 (1) | 1.13 (.90–1.42) | |
| Myeloma | 207 (3) | 32 (0.8) | 239 (2) | 2.08 (1.75–2.47)** | |
| Amyloidosis | 71 (0.9) | 41 (1) | 112 (0.9) | 2.11 (1.64–2.73)** | |
| Systemic GN | 97 (1) | 52 (1) | 149 (1) | .98 (.76–1.26) | |
| Vasculitis | 377 (5) | 70 (2) | 447 (4) | .83 (.72–.96)* | |
| HUS/TTP2 | 40 (0.5) | 15 (0.4) | 55 (0.5) | .49 (.29–.81)* | |
| Other | 285 (3) | 59 (2) | 344 (3) | .97 (.83–1.13) | |
| DM diagnosis | 1822 (22) | 916 (24) | 2738 (23) | 1.51 (1.43–1.6)** | |
| Comorbidity | ** | ** | |||
| 0 | 2837 (34) | 1941 (51) | 4778 (40) | 1 (ref) | 1 (ref) |
| 1–2 | 3623 (44) | 1423 (37) | 5046 (42) | 1.6 (1.51–1.69)** | 1.69 (1.6–1.79)** |
| >2 | 1813 (22) | 458 (12) | 2271 (19) | 2.3 (2.14–2.46)** | 2.52 (2.35–2.7)** |
| ESRD Initiation | ** | ** | |||
| Early & Routine | 2145 (26) | 1419 (37) | 3564 (29) | .91 (.86–.96)* | .89 (.84–.94)** |
| Late & Acute | 2138 (26) | 648 (17) | 2786 (23) | 1.1 (1.03–1.16)* | 1.12 (1.05–1.19)** |
| Other | 3990 (48) | 1755 (46) | 5745 (47) | 1 (ref) | 1 (ref) |
Corresponding significant p-values are presented as.
*: p<.05;
**:p<.001.
For definition of models see methods section.
:HD is the reference category;
: Hemolytic Uremic Syndrome/ThrombocoticThrombocytopenic Purpura.
Improvements in referral pattern were seen during the period of observation. L&A initiations fell from 37 to 16% and E&R rose from 10 to 43%.
The hazard ratios for the factors analyzed are shown in Table 1. All factors except for (female) sex had a highly significant influence on mortality in model 2. The unadjusted prognosis according to cohort and initial dialysis modality is shown in Table 2, and the adjusted in Table 3. Overall, there was a significant improvement in patient prognosis during the period of observation (HR for cohort, Table 1). Adjusted mortality fell overall by 34%. Estimated relative mortality of PD versus HD improved from .95 in 1990–94 to .8 in 2005–10 (Table 3, based on model 2 with an additional interaction term between cohort and dialysis modality).
Table 2. Prognosis according to cohort and modality.
| Within one year: | ||||||||||||||
| Cohort | Modality | N | Dead without change of modality (within 1 year) | LTF1 without change | Transplantation | Change of modality, later death | Change without subsequent death | Unchanged after 1 year | ||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |||
| 90-94 | HD | 1099 | 221 | 20.1 | 0 | 0 | 112 | 10.2 | 18 | 1.6 | 145 | 13.2 | 603 | 54.9 |
| 95-99 | 1877 | 446 | 23.8 | 2 | .1 | 92 | 4.9 | 19 | 1 | 172 | 9.2 | 1146 | 61.1 | |
| 00-04 | 2482 | 590 | 23.8 | 1 | 0 | 71 | 2.9 | 29 | 1.2 | 138 | 5.6 | 1653 | 66.6 | |
| 05-10 | 2815 | 557 | 19.8 | 348 | 12.4 | 63 | 2.2 | 22 | .8 | 160 | 5.7 | 1665 | 59.1 | |
| 90-94 | PD | 748 | 59 | 7.9 | 0 | 0 | 103 | 13.8 | 28 | 3.7 | 121 | 16.2 | 437 | 58.4 |
| 95-99 | 792 | 66 | 8.3 | 0 | 0 | 82 | 10.4 | 34 | 4.3 | 107 | 13.5 | 503 | 63.5 | |
| 00-04 | 1022 | 81 | 7.9 | 0 | 0 | 78 | 7.6 | 26 | 2.5 | 156 | 15.3 | 681 | 66.6 | |
| 05-10 | 1260 | 98 | 7.8 | 154 | 12.2 | 117 | 9.3 | 25 | 2 | 174 | 13.8 | 692 | 54.9 | |
| Within 5 years | ||||||||||||||
| 90-94 | HD | 1099 | 529 | 48.1 | 0 | 0 | 231 | 21 | 85 | 7.7 | 99 | 9 | 155 | 14.1 |
| 95-99 | 1877 | 1048 | 55.8 | 2 | .1 | 256 | 13.6 | 103 | 5.5 | 112 | 6 | 356 | 19 | |
| 00-04 | 2482 | 1512 | 60.9 | 1 | 0 | 221 | 8.9 | 94 | 3.8 | 101 | 4.1 | 553 | 22.3 | |
| 05-10 | 2815 | 1163 | 41.3 | 1157 | 41.1 | 165 | 5.9 | 70 | 2.5 | 136 | 4.8 | 124 | 4.4 | |
| 90-94 | PD | 748 | 231 | 30.9 | 0 | 0 | 194 | 25.9 | 137 | 18.3 | 134 | 17.9 | 52 | 7 |
| 95-99 | 792 | 206 | 26 | 0 | 0 | 174 | 22 | 175 | 22.1 | 154 | 19.4 | 83 | 10.5 | |
| 00-04 | 1022 | 285 | 27.9 | 0 | 0 | 231 | 22.6 | 161 | 15.8 | 219 | 21.4 | 126 | 12.3 | |
| 05-10 | 1260 | 244 | 19.4 | 394 | 31.3 | 226 | 17.9 | 114 | 9 | 256 | 20.3 | 26 | 2.1 | |
| Within 10 years | ||||||||||||||
| 90-94 | HD | 1099 | 625 | 56.9 | 0 | 0 | 247 | 22.5 | 107 | 9.7 | 79 | 7.2 | 41 | 3.7 |
| 95-99 | 1877 | 1259 | 67.1 | 2 | .1 | 296 | 15.8 | 142 | 7.6 | 79 | 4.2 | 99 | 5.3 | |
| 00-04 | 2482 | 1766 | 71.2 | 216 | 8.7 | 259 | 10.4 | 127 | 5.1 | 75 | 3 | 39 | 1.6 | |
| 05-10 | 2815 | 1177 | 41.8 | 1262 | 44.8 | 169 | 6 | 70 | 2.5 | 137 | 4.9 | |||
| 90-94 | PD | 748 | 254 | 34 | 0 | 0 | 196 | 26.2 | 193 | 25.8 | 99 | 13.2 | 6 | .8 |
| 95-99 | 792 | 238 | 30.1 | 0 | 0 | 184 | 23.2 | 249 | 31.4 | 112 | 14.1 | 9 | 1.1 | |
| 00-04 | 1022 | 331 | 32.4 | 37 | 3.6 | 238 | 23.3 | 240 | 23.5 | 173 | 16.9 | 3 | .3 | |
| 05-10 | 1260 | 246 | 19.5 | 415 | 32.9 | 227 | 18 | 116 | 9.2 | 256 | 20.3 | |||
: Lost to Follow-up.
Table 3. Cohort and mortality.
| Cohort | HD | PD | Relative Mortality PD/HD |
| 1990–94 | 1 (ref) | .95 (.85–1.06) | .95 (.85–1.06) |
| 1995–1999 | .88 (.8–.97) | .8 (.72–.89) | .9 (.82–1) |
| 2000–04 | .79 (.72–.86) | .66 (.59–.74) | .84 (.77–.92) |
| 2005–10 | .7 (.63–.77) | .56 (.49–.63) | .80 (.71–.89) |
Adjusted hazard ratio (CI) based on a Cox regression model with interaction term between dialysis modality and cohort. Overall hazard ratio for PD versus HD was .8 (.71–.89). Overall p-value for interaction term was 0.11 (not significant).
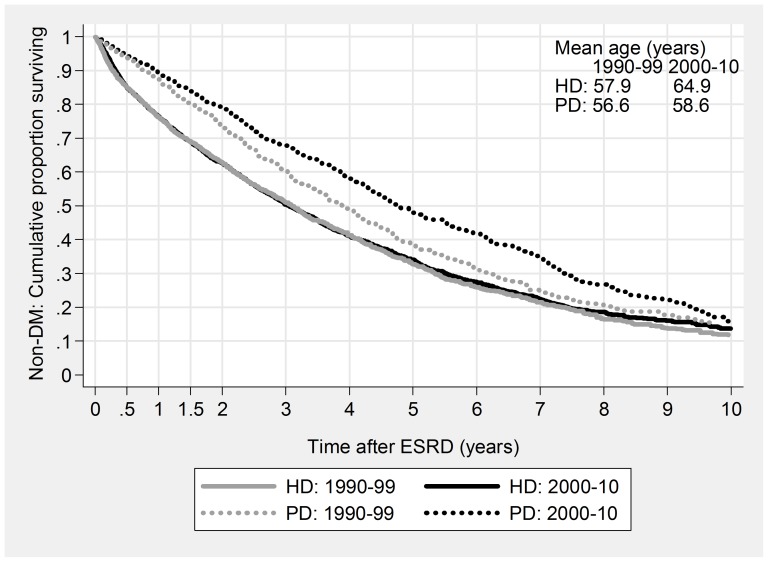
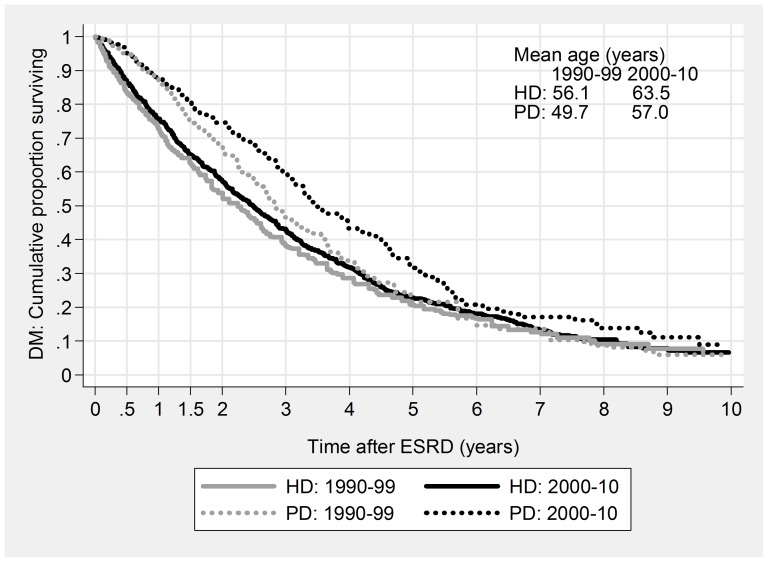
For HD patients improvement consisted of largely unchanged mortality despite rapidly increasing age and morbidity (Figs. 1 & 2), while for PD patients non-DM median survival increased by 10 months from 1990–99 to 2000–10, while DM survival increased by 8 months, despite a seven-year increase in average age. For some subgroups, the PD improvement was dramatic: 4-year mortality for young, non-DM patients fell from 47% to 23%, and two-year mortality for elderly diabetics from 74% to 39% (Table 4).
Figure 1. Patient Survival based on Kaplan-Meier curves, stratified for Modality and Cohort.
Non-DM.
Figure 2. Patient Survival based on Kaplan-Meier curves, stratified for Modality and Cohort.
DM.
Table 4. Patient mortality according to modality, age and diabetic status.
| Two-year Mortality (%) | Four-year Mortality (%) | |||||||||
| Modality | Diagnosis | Age (yrs) | 90-94 | 95-99 | 00-04 | 05-10 | 90-94 | 95-99 | 00-04 | 05-10 |
| PD | NonDM | <65 | 18 | 16 | 10 | 11 | 47 | 30 | 23 | 23 |
| > = 65 | 41 | 40 | 37 | 33 | 69 | 67 | 63 | 60 | ||
| DM | <65 | 34 | 22 | 19 | 21 | 71 | 53 | 48 | 46 | |
| > = 65 | 74 | 39 | 36 | 39 | 100 | 79 | 74 | 74 | ||
| HD | NonDM | <65 | 24 | 25 | 25 | 23 | 44 | 42 | 41 | 36 |
| > = 65 | 55 | 49 | 48 | 44 | 76 | 73 | 70 | 68 | ||
| DM | <65 | 43 | 42 | 31 | 31 | 64 | 64 | 56 | 57 | |
| > = 65 | 51 | 60 | 59 | 49 | 89 | 84 | 83 | 74 |
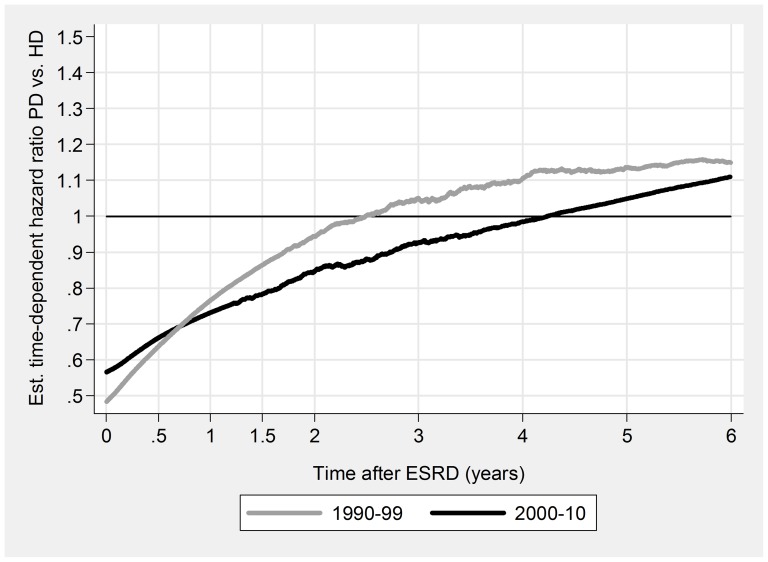
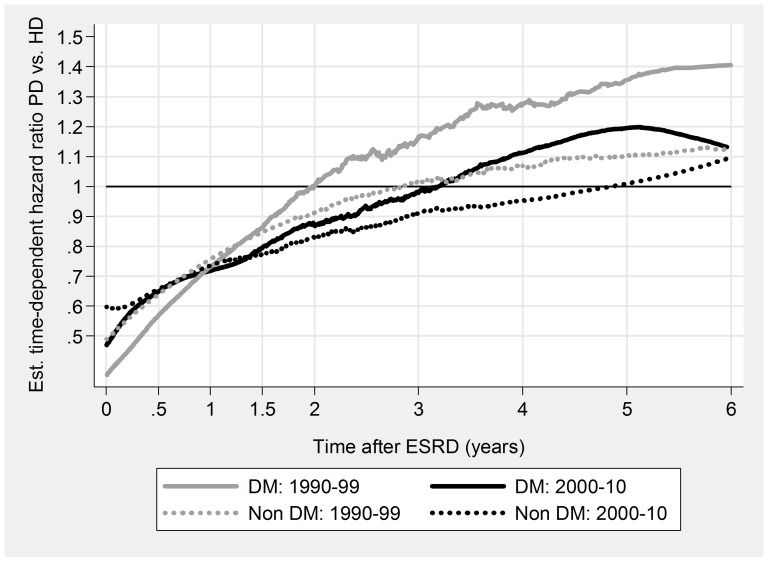
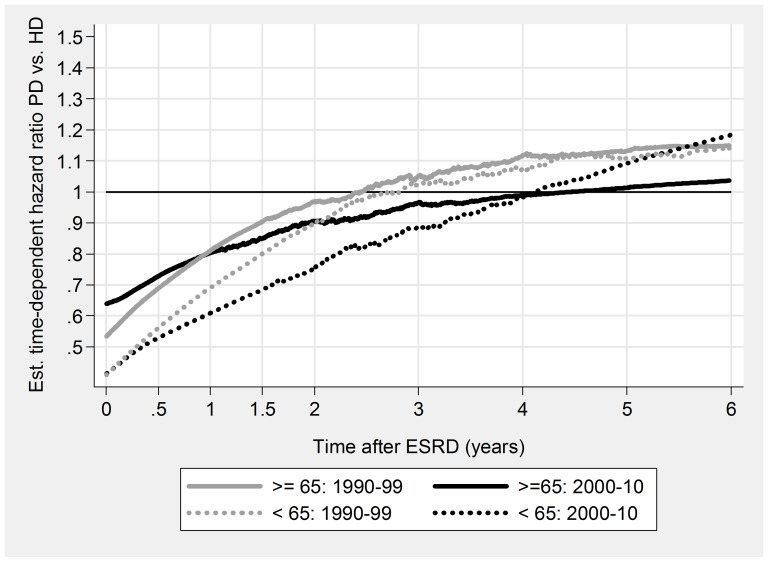
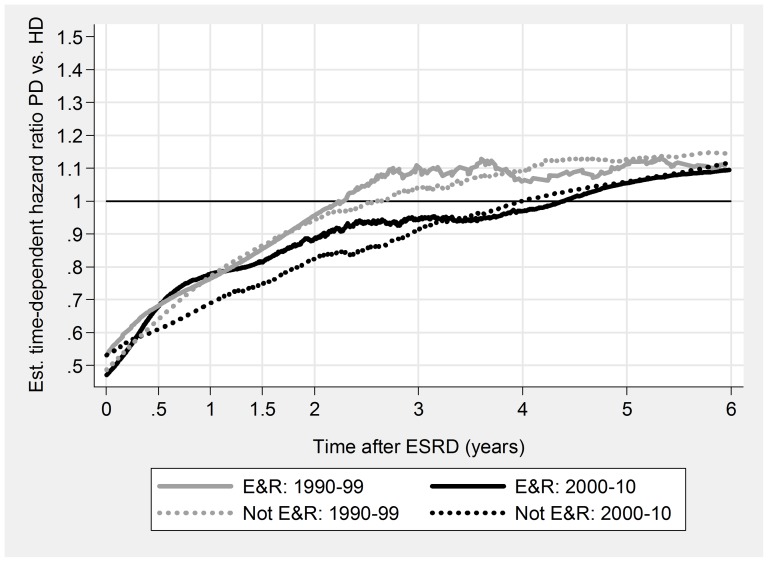
PD was associated with a significant initial survival advantage, both overall and for all subgroups (Table 5, Figs. 3, 4, 5, & 6). Late prognosis was generally poorer for PD patients, but less so for the later cohort. Relative PD prognosis improved for all subgroups from 1990–99 to 2000–10. The “crossover point” from better to poorer PD prognosis increased from about 30 months to 52 months, and for no subgroup was less than 24 months. PD results were mostly better for non-DM patients than DM, and younger (<65 years) than older. Improvements in referral pattern were seen during the period of observation. Relative PD prognosis was better for patients with E&R initiation in the later cohort for the initial 36 months. There were no significant differences in age or CCI index between the E&R group and other patients.
Table 5. Relationship between relative mortality PD/HD and dialysis duration.
| All | DM | > = 65 yrs | DM and > = 65 yrs | Early & Routine | ||||||
| Duration (months) | 1990–99 | 2000–10 | 1990–99 | 2000–10 | 1990–99 | 2000–10 | 1990–99 | 2000–10 | 1990–99 | 2000–10 |
| 0–6 | .45 (.36–.57)** | .54 (.44–.66)** | .34 (.2–.56)** | .48 (.32–.73)* | .51 (.38–.68)** | .60 (.48–.76)** | .19 (.07–.53)* | .33 (.17–.63)* | .52 (.25–1.1) | .50 (.35–.72)** |
| 6–12 | .79 (.63–1.00) | .69 (.56–.86)* | .78 (.49–1.25) | .76 (.52–1.11) | .84 (.61–1.15) | .78 (.60–1.01) | 1.36 (.65–2.86) | .81 (.49–1.32) | .64 (.32–1.28) | .87 (.61–1.24) |
| 12–18 | .96 (.75–1.22) | .79 (.64–.99)* | 1.01 (.66–1.55) | .73 (.49–1.08) | 0.97 (.7–1.36) | .83 (.64–1.09) | 1.25 (.59–2.65) | .66 (.37–1.16) | 1.15 (.62–2.14) | 1.12 (.8–1.57) |
| 18–24 | .97 (.74–1.26) | .84 (.65–1.08) | .65 (.39–1.07) | .81 (.51–1.29) | 1.06 (.74–1.52) | .97 (.71–1.33) | .84 (.33–2.15) | 1.04 (.54–2.01) | .73 (.39–1.38) | .66 (.43–1) |
| 24–36 | 1.17 (.97–1.42) | .88 (.74–1.06) | 1.43 (.98–2.08) | .9 (.65–1.24) | 1.2 (.92–1.56) | .93 (.74–1.16) | 1.65 (.87–3.13) | 1.03 (.62–1.69) | 1.22 (.78–1.89) | .81 (.6–1.1) |
| 36–48 | 1.1 (.87–1.38) | 1.03 (.83–1.28) | 1.28 (.8–2.04) | 1.32 (.91–1.9) | .94 (.67–1.32) | 1.08 (.83–1.41) | 1.01 (.36–2.84) | 1.32 (.78–2.24) | 1.18 (.65–2.14) | 1.28 (.9–1.81) |
| >48 | 1.15 (1–1.31)* | 1.12 (.96–1.32) | 1.52 (1.08–2.12)* | 1.11 (.81–1.53) | 1.17 (.96–1.43) | 1.04 (.83–1.31) | 3.09 (1.38–6.90)* | 1.62 (.93–2.83) | 1.05 (.76–1.47) | 1.05 (.8–1.38) |
| Overall | .94 (.87–1.01) | .83 (.77–.89)** | .97 (.84–1.12) | .85 (.75–.97)* | .94 (.85–1.04) | .86 (.78–.94)* | 1 (.77–1.29) | .85 (.71–1.01) | .97 (.81–1.17) | .88 (.78–.99)* |
Figure 3. Relationship of relative mortality risk PD/HD to dialysis duration.
1990–99 versus 2000–10.
Figure 4. Relationship of relative mortality risk PD/HD to dialysis duration.
DM versus Non-DM.
Figure 5. Relationship of relative mortality risk PD/HD to dialysis duration.
<65 years versus > = 65 years.
Figure 6. Relationship of relative mortality risk PD/HD to dialysis duration.
Early & routine versus not E&R referral pattern.
Results for the 90-day analysis were broadly similar and are therefore not shown.
Discussion
Substantial improvements in prognosis were seen for both HD and PD during the period of observation. This is in accordance with USRDS and DOPPS data [32], [33]. This is particularly remarkable, since the period has been characterized by an absence of major randomized controlled trials with a positive therapeutic result. Possible factors contributing to this general improvement include defined standards for adequate dialysis, increased attention to calcium, phosphate and PTH control, better anemia control, better preparation of dialysis initiation, and a tendency towards earlier dialysis initiation. Furthemore, advances in non-nephrological areas, such as reduced tobacco consumption, improved treatment of cardiovascular disease will also have contributed. It is possible that some of the improved prognosis is a statistical artifact, due to increased registration of comorbidity over time.
A trend to improvement in the relative prognosis of PD patients compared to HD patients were also seen, despite employing a conservative intention-to-treat analysis (ITT) strategy where the “true” group differences tend to be under- rather than overestimated. This is in accordance with previous studies [15], [19], [23], [25]. Substantial changes in the practice of PD occurred during the period. The observation of an increased mortality of patients with fast peritoneal transport [34] and the observation that automated PD (APD) seems to solve the problem [35]–[37] suggests that a major cause of PD mortality during the nineties was due to inadequate ultrafiltration secondary to rapid dissipation of the glucose osmotic gradient in fast transporters, with consequent overhydration, hypertension, pulmonary edema and death. Better fluid control using icodextrin and APD seems to have solved the problem of fast transport [36], [38]. Icodextrin became available in Denmark from 1999 and the use of APD rose rapidly from 3% in 1990 to 30% in 2000 and 66% in 2008 [39]. Biocompatible PD fluids became available in 2000, and have recently been demonstrated to preserve residual renal function (RRF), peritoneal membrane function and reduce the incidence of peritonitis and possibly other infections [40], [41]. The possible contribution of a reduction in peritonitis frequency in this study is unknown. Peritonitis frequency registration was first introduced in 2000, and has since showed a moderate improvement from 1/25 patient months to 1/31 [39]. HD-specific improvements have also occurred during the period. The introduction of biocompatible membranes and the use of “floating dry weight” (whereby fluid balance is controlled by fluid restriction rather than ultrafiltration in nonoliguric HD patients) may help to preserve RRF [42], [43]. The beneficial effects on mortality of high flux dialysis and hemodiafiltration remain however unproved [44], [45]. In conclusion, the improvement in PD prognosis has been greater than HD, and therefore cohorts from the nineties can no longer be used for comparing treatment results. Furthermore, randomized, controlled trials comparing HD and PD should offer patients the full range of PD products, including biocompatible fluids, icodextrin and APD.
As mentioned in the introduction, PD is characterized by a better initial prognosis, and an equal or worse late prognosis. One possible cause is better preservation of RRF in PD [46], perhaps due to intradialytic renal dehydration and ischemia during HD [47]. Preservation of RRF is a major determinant of dialysis survival [48]. One important exception to the general pattern is the ANZA study, which showed a poorer prognosis for PD patients, albeit with considerable improvement in the latest cohort [19]. Closer perusal of these results however [49] show that the good HD prognosis was mainly related to the high home HD prevalence in this population. If these patients are excluded from the analysis, the traditional pattern reappears, with an initial PD advantage disappearing after two years. The present study also showed a better initial prognosis, and an insignificantly worse late prognosis, again, despite a conservative ITT approach. The overall prognosis since 2000 was significantly better for PD for each of the four major subgroups.
Regardless of the overall result, most studies show a better relative effect of PD in younger [1]–[3], [5], [8], [9], [11], [12], [14]–[16], [19]–[21], [25], non-diabetic [1]–[3], [5]–[11], [14]–[16], [18], [20], [21], [23], [25] patients, and patients without comorbidity [8]–[12], [16], [19]–[21], [23], [24]. The present study also showed a relatively better prognosis for younger and non-diabetic patients, but for no subgroup was PD worse than HD. After 2000, there was no difference between relative diabetic and non-diabetic prognosis. It has been suggested [22] that the better initial prognosis is due to differences in dialysis planning, in that PD patients are more likely to have been referred earlier and started ESRD therapy as out-patients. The present study has the advantage that ESRD planning, which was found to have a major impact on prognosis, was included in the statistical analysis. In a separate analysis of patients with early, out-patient ESRD initiation, the initial PD advantage remained. Thus, differences in ESRD planning do not explain the initial PD survival advantage in this study. This conclusion is substantially different from the Quinn study [22]. It is possible that differences in patient population, protocol design and hospital practice may explain some of the differences.
All patients in the E&R group were out-patient at the time of initiation, and had been referred early to a nephrologist. This does not, of course exclude the possibility that they were acutely sick at the time of dialysis start, just that they did not need hospital admission. Furthermore, the vast majority of these patients will have been started using an AV fistula or graft, since a central catheter always requires hospital admission in Denmark. The initial PD advantage holds for all subgroups analysed, and may therefore be a universal phenomenon. Possible causes include early loss of residual function after HD initiation [47], [50] and the detrimental effects of myocardial stunning after HD initiation.
The practical consequences of this study remain controversial. Questions may be made as to the validity of the CCI and patient referral pattern. Discharge diagnosis registration may vary between centers and over time, particularly if quality measures or reimbursement rules are based on the CCI. This is not however the case in Denmark. The CCI measures only discharge diagnoses, and will thus underestimate the true comorbidity; this underestimation is not necessarily uniform between the groups studied. Despite these reservations, both CCI and referral patient were indeed very significant markers of death. As it is an epidemiological study, no causal conclusions can be drawn. The initial PD results may be due to better preservation of RRF, or to hitherto unidentified comorbid factors. The present consensus is that dialysis patients should continue to choose modality on the basis of personal preference. Patients, in particular younger, non-diabetic patients, should be informed of the possible advantage of PD. If survival is the primary motivating factor, this group of patients should however consider home HD as an alternative. It offers better phosphate, PTH, anemia and blood pressure control, fewer dietary restrictions, and removes the dangers of the long weekend [51]. Probably as a direct consequence, patient survival is greater than conventional PD and HD [49] and on a par with cadaver renal transplantation [52].
Funding Statement
There are no current funding sources for this study.
References
- 1. Fenton SS, Schaubel DE, Desmeules M, Morrison HI, Mao Y, et al. (1997) Hemodialysis versus peritoneal dialysis: a comparison of adjusted mortality rates. Am J Kidney Dis 30: 334–342 S0272638697001686 [pii]. [DOI] [PubMed] [Google Scholar]
- 2. Schaubel DE, Morrison HI, Fenton SS (1998) Comparing mortality rates on CAPD/CCPD and hemodialysis. The Canadian experience: fact or fiction? Perit Dial Int 18: 478–484. [PubMed] [Google Scholar]
- 3. Vonesh EF, Moran J (1999) Mortality in end-stage renal disease: a reassessment of differences between patients treated with hemodialysis and peritoneal dialysis. J Am Soc Nephrol 10: 354–365. [DOI] [PubMed] [Google Scholar]
- 4. Locatelli F, Marcelli D, Conte F, D'Amico M, Del VL, et al. (2001) Survival and development of cardiovascular disease by modality of treatment in patients with end-stage renal disease. J Am Soc Nephrol 12: 2411–2417. [DOI] [PubMed] [Google Scholar]
- 5. Heaf JG, Lokkegaard H, Madsen M (2002) Initial survival advantage of peritoneal dialysis relative to haemodialysis. Nephrol Dial Transplant 17: 112–117. [DOI] [PubMed] [Google Scholar]
- 6. Winkelmayer WC, Glynn RJ, Mittleman MA, Levin R, Pliskin JS, et al. (2002) Comparing mortality of elderly patients on hemodialysis versus peritoneal dialysis: a propensity score approach. J Am Soc Nephrol 13: 2353–2362. [DOI] [PubMed] [Google Scholar]
- 7. Collins AJ, Weinhandl E, Snyder JJ, Chen SC, Gilbertson D (2002) Comparison and survival of hemodialysis and peritoneal dialysis in the elderly. Semin Dial 15: 98–102 0032 [pii]. [DOI] [PubMed] [Google Scholar]
- 8. Termorshuizen F, Korevaar JC, Dekker FW, Van Manen JG, Boeschoten EW, et al. (2003) Hemodialysis and peritoneal dialysis: comparison of adjusted mortality rates according to the duration of dialysis: analysis of The Netherlands Cooperative Study on the Adequacy of Dialysis 2. J Am Soc Nephrol 14: 2851–2860. [DOI] [PubMed] [Google Scholar]
- 9. Ganesh SK, Hulbert-Shearon T, Port FK, Eagle K, Stack AG (2003) Mortality differences by dialysis modality among incident ESRD patients with and without coronary artery disease. J Am Soc Nephrol 14: 415–424. [DOI] [PubMed] [Google Scholar]
- 10. Stack AG, Molony DA, Rahman NS, Dosekun A, Murthy B (2003) Impact of dialysis modality on survival of new ESRD patients with congestive heart failure in the United States. Kidney Int 64: 1071–1079 kid165 [pii];10.1046/j.1523-1755.2003.00165.x [doi] [DOI] [PubMed] [Google Scholar]
- 11. Vonesh EF, Snyder JJ, Foley RN, Collins AJ (2004) The differential impact of risk factors on mortality in hemodialysis and peritoneal dialysis. Kidney Int 66: 2389–2401 KID66028 [pii];10.1111/j.1523-1755.2004.66028.x [doi] [DOI] [PubMed] [Google Scholar]
- 12. Jaar BG, Coresh J, Plantinga LC, Fink NE, Klag MJ, et al. (2005) Comparing the risk for death with peritoneal dialysis and hemodialysis in a national cohort of patients with chronic kidney disease. Ann Intern Med 143: 174–183 143/3/174 [pii]. [DOI] [PubMed] [Google Scholar]
- 13. Frimat L, Durand PY, Loos-Ayav C, Villar E, Panescu V, et al. (2006) Impact of first dialysis modality on outcome of patients contraindicated for kidney transplant. Perit Dial Int 26: 231–239. [PubMed] [Google Scholar]
- 14. Mircescu G, Garneata L, Florea L, Cepoi V, Capsa D, et al. (2006) The success story of peritoneal dialysis in Romania: analysis of differences in mortality by dialysis modality and influence of risk factors in a national cohort. Perit Dial Int 26: 266–275. [PubMed] [Google Scholar]
- 15. Liem YS, Wong JB, Hunink MG, de Charro FT, Winkelmayer WC (2007) Comparison of hemodialysis and peritoneal dialysis survival in The Netherlands. Kidney Int 71: 153–158 5002014 [pii];10.1038/sj.ki.5002014 [doi] [DOI] [PubMed] [Google Scholar]
- 16. Huang CC, Cheng KF, Wu HD (2008) Survival analysis: comparing peritoneal dialysis and hemodialysis in Taiwan. Perit Dial Int 28 Suppl 3: S15–S20 28/Supplement_3/S15 [pii]. [PubMed] [Google Scholar]
- 17. Sanabria M, Munoz J, Trillos C, Hernandez G, Latorre C, et al. (2008) Dialysis outcomes in Colombia (DOC) study: a comparison of patient survival on peritoneal dialysis vs hemodialysis in Colombia. Kidney Int Suppl: S165–S172 5002619 [pii];10.1038/sj.ki.5002619 [doi] [DOI] [PubMed] [Google Scholar]
- 18. Lee CC, Sun CY, Wu MS (2009) Long-term modality-related mortality analysis in incident dialysis patients. Perit Dial Int 29: 182–190 29/2/182 [pii]. [PubMed] [Google Scholar]
- 19. McDonald SP, Marshall MR, Johnson DW, Polkinghorne KR (2009) Relationship between dialysis modality and mortality. J Am Soc Nephrol 20: 155–163 ASN.2007111188 [pii];10.1681/ASN.2007111188 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Weinhandl ED, Foley RN, Gilbertson DT, Arneson TJ, Snyder J, et al. (2010) Propensity-matched mortality comparison of incident hemodialysis and peritoneal dialysis patients. J Am Soc Nephrol 21: 499–506 ASN.2009060635 [pii];10.1681/ASN.2009060635 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. van de Luijtgaarden MW, Noordzij M, Stel VS, Ravani P, Jarraya F, et al. (2011) Effects of comorbid and demographic factors on dialysis modality choice and related patient survival in Europe. Nephrol Dial Transplant 26: 2940–2947 gfq845 [pii];10.1093/ndt/gfq845 [doi] [DOI] [PubMed] [Google Scholar]
- 22. Quinn RR, Hux JE, Oliver MJ, Austin PC, Tonelli M, et al. (2011) Selection bias explains apparent differential mortality between dialysis modalities. J Am Soc Nephrol 22: 1534–1542 ASN.2010121232 [pii];10.1681/ASN.2010121232 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mehrotra R, Chiu YW, Kalantar-Zadeh K, Bargman J, Vonesh E (2011) Similar outcomes with hemodialysis and peritoneal dialysis in patients with end-stage renal disease. Arch Intern Med 171: 110–118 archinternmed.2010.352 [pii];10.1001/archinternmed.2010.352 [doi] [DOI] [PubMed] [Google Scholar]
- 24. Sens F, Schott-Pethelaz AM, Labeeuw M, Colin C, Villar E (2011) Survival advantage of hemodialysis relative to peritoneal dialysis in patients with end-stage renal disease and congestive heart failure. Kidney Int 80: 970–977 ki2011233 [pii];10.1038/ki.2011.233 [doi] [DOI] [PubMed] [Google Scholar]
- 25. Yeates K, Zhu N, Vonesh E, Trpeski L, Blake P, et al. (2012) Hemodialysis and peritoneal dialysis are associated with similar outcomes for end-stage renal disease treatment in Canada. Nephrol Dial Transplant 27: 3568–3575 gfr674 [pii];10.1093/ndt/gfr674 [doi] [DOI] [PubMed] [Google Scholar]
- 26.Wehberg S (2010) Datagrundlag og analysemetode. Danish Nephrology Registry Annual Report 2009. Available: www.nephrology.dk: 14–21. Accessed 2014 Feb 8.
- 27. Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40: 373–383. [DOI] [PubMed] [Google Scholar]
- 28. Lynge E, Sandegaard JL, Rebolj M (2011) The Danish National Patient Register. Scand J Public Health 39: 30–33 39/7_suppl/30 [pii];10.1177/1403494811401482 [doi] [DOI] [PubMed] [Google Scholar]
- 29. Pedersen CB, Gotzsche H, Moller JO, Mortensen PB (2006) The Danish Civil Registration System. A cohort of eight million persons. Dan Med Bull 53: 441–449 DMB3816 [pii]. [PubMed] [Google Scholar]
- 30. Andersen TF, Madsen M, Jorgensen J, Mellemkjoer L, Olsen JH (1999) The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 46: 263–268. [PubMed] [Google Scholar]
- 31. Grambsch PM, Therneau TM (2010) Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 81: 515–526. [Google Scholar]
- 32. Collins AJ, Foley RN, Chavers B, Gilbertson D, Herzog C, et al. (2012) 'United States Renal Data System 2011 Annual Data Report: Atlas of chronic kidney disease & end-stage renal disease in the United States. Am J Kidney Dis 59: A7, e1–A7,420 S0272-6386(11)01571-X [pii];10.1053/j.ajkd.2011.11.015 [doi] [DOI] [PubMed] [Google Scholar]
- 33. Port FK, Pisoni RL, Bommer J, Locatelli F, Jadoul M, et al. (2006) Improving outcomes for dialysis patients in the international Dialysis Outcomes and Practice Patterns Study. Clin J Am Soc Nephrol 1: 246–255 CJN.01050905 [pii];10.2215/CJN.01050905 [doi] [DOI] [PubMed] [Google Scholar]
- 34. Churchill DN, Thorpe KE, Nolph KD, Keshaviah PR, Oreopoulos DG, et al. (1998) Increased peritoneal membrane transport is associated with decreased patient and technique survival for continuous peritoneal dialysis patients. The Canada-USA (CANUSA) Peritoneal Dialysis Study Group. J Am Soc Nephrol 9: 1285–1292. [DOI] [PubMed] [Google Scholar]
- 35. Brimble KS, Walker M, Margetts PJ, Kundhal KK, Rabbat CG (2006) Meta-analysis: peritoneal membrane transport, mortality, and technique failure in peritoneal dialysis. J Am Soc Nephrol 17: 2591–2598 ASN.2006030194 [pii];10.1681/ASN.2006030194 [doi] [DOI] [PubMed] [Google Scholar]
- 36. Yang X, Fang W, Bargman JM, Oreopoulos DG (2008) High peritoneal permeability is not associated with higher mortality or technique failure in patients on automated peritoneal dialysis. Perit Dial Int 28: 92. [pii]. [PubMed] [Google Scholar]
- 37. Johnson DW, Hawley CM, McDonald SP, Brown FG, Rosman JB, et al. (2010) Superior survival of high transporters treated with automated versus continuous ambulatory peritoneal dialysis. Nephrol Dial Transplant 25: 1973–1979 gfp780 [pii];10.1093/ndt/gfp780 [doi] [DOI] [PubMed] [Google Scholar]
- 38. Davies SJ (2006) Mitigating peritoneal membrane characteristics in modern peritoneal dialysis therapy. Kidney Int Suppl: S76–S83 5001920 [pii];10.1038/sj.ki.5001920 [doi] [DOI] [PubMed] [Google Scholar]
- 39.Heaf JG (2011) Danish Nephrology Registry Annual Report. Available: www.nephrology.dk: 1–109. Accessed 2014 Feb 8
- 40. Johnson DW, Brown FG, Clarke M, Boudville N, Elias TJ, et al. (2012) Effects of biocompatible versus standard fluid on peritoneal dialysis outcomes. J Am Soc Nephrol 23: 1097–1107 ASN.2011121201 [pii];10.1681/ASN.2011121201 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Johnson DW, Brown FG, Clarke M, Boudville N, Elias TJ, et al. (2012) The effect of low glucose degradation product, neutral pH versus standard peritoneal dialysis solutions on peritoneal membrane function: the balANZ trial. Nephrol Dial Transplant 27: 4445–4453 gfs314 [pii];10.1093/ndt/gfs314 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lang SM, Bergner A, Topfer M, Schiffl H (2001) Preservation of residual renal function in dialysis patients: effects of dialysis-technique-related factors. Perit Dial Int 21: 52–57. [PubMed] [Google Scholar]
- 43. Vilar E, Wellsted D, Chandna SM, Greenwood RN, Farrington K (2009) Residual renal function improves outcome in incremental haemodialysis despite reduced dialysis dose. Nephrol Dial Transplant 24: 2502–2510 gfp071 [pii];10.1093/ndt/gfp071 [doi] [DOI] [PubMed] [Google Scholar]
- 44. Eknoyan G, Beck GJ, Cheung AK, Daugirdas JT, Greene T, et al. (2002) Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med 347: 2010–2019 10.1056/NEJMoa021583 [doi];347/25/2010 [pii] [DOI] [PubMed] [Google Scholar]
- 45. Grooteman MP, van den Dorpel MA, Bots ML, Penne EL, van der Weerd NC, et al. (2012) Effect of online hemodiafiltration on all-cause mortality and cardiovascular outcomes. J Am Soc Nephrol 23: 1087–1096 ASN.2011121140 [pii];10.1681/ASN.2011121140 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Moist LM, Port FK, Orzol SM, Young EW, Ostbye T, et al. (2000) Predictors of loss of residual renal function among new dialysis patients. J Am Soc Nephrol 11: 556–564. [DOI] [PubMed] [Google Scholar]
- 47. Jansen MA, Hart AA, Korevaar JC, Dekker FW, Boeschoten EW, et al. (2002) Predictors of the rate of decline of residual renal function in incident dialysis patients. Kidney Int 62: 1046–1053 kid505 [pii];10.1046/j.1523-1755.2002.00505.x [doi] [DOI] [PubMed] [Google Scholar]
- 48. Paniagua R, Amato D, Vonesh E, Correa-Rotter R, Ramos A, et al. (2002) Effects of increased peritoneal clearances on mortality rates in peritoneal dialysis: ADEMEX, a prospective, randomized, controlled trial. J Am Soc Nephrol 13: 1307–1320. [DOI] [PubMed] [Google Scholar]
- 49. Marshall MR, Hawley CM, Kerr PG, Polkinghorne KR, Marshall RJ, et al. (2011) Home hemodialysis and mortality risk in Australian and New Zealand populations. Am J Kidney Dis 58: 782–793 S0272-6386(11)00942-5 [pii];10.1053/j.ajkd.2011.04.027 [doi] [DOI] [PubMed] [Google Scholar]
- 50. Burton JO, Jefferies HJ, Selby NM, McIntyre CW (2009) Hemodialysis-induced cardiac injury: determinants and associated outcomes. Clin J Am Soc Nephrol 4: 914–920 CJN.03900808 [pii];10.2215/CJN.03900808 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Foley RN, Gilbertson DT, Murray T, Collins AJ (2011) Long interdialytic interval and mortality among patients receiving hemodialysis. N Engl J Med 365: 1099–1107 10.1056/NEJMoa1103313 [doi] [DOI] [PubMed] [Google Scholar]
- 52. Pauly RP, Gill JS, Rose CL, Asad RA, Chery A, et al. (2009) Survival among nocturnal home haemodialysis patients compared to kidney transplant recipients. Nephrol Dial Transplant 24: 2915–2919 gfp295 [pii];10.1093/ndt/gfp295 [doi] [DOI] [PubMed] [Google Scholar]