Abstract
Background:
Neonatal tetanus is a vaccine preventable disease and is a leading cause of neonatal mortality in developing countries. The effectiveness of immunization and hygienic umbilical cord care practices in the prevention of the disease has been established.
Objective:
The objective of this study was to audit the scourge of neonatal tetanus in a tertiary health facility in a resource-limited setting.
Materials and Methods:
The study was a retrospective study. Case notes of neonates admitted with clinical diagnosis of tetanus into the Special Care Baby Unit (SCBU) between January 2009 and December 2010 were retrieved and evaluated to identify socio-demographic and clinical characteristics, mode of acquisition and severity of the disease, presence of co-morbidities, duration of hospital stay and outcome.
Results:
Most of the mothers had no tetanus immunization (66.7%) and the main social class of the children was class V (45.1%) and IV (41.2%), respectively. Only 29.4% of the mothers attended ante-natal care (ANC) while majority of the patients were delivered at home (94.1%). Half of the neonates presented with the severe form of the disease (51.0%). Sepsis is a prominent co-morbidity (59.2%). Morality was high with case fatality of 66.7%.
Conclusion:
This high prevalence of neonatal tetanus with high mortality is not only disappointing but unacceptable in the 21st century. Therefore, all efforts must be re-focused on current preventive strategies while pursuing new areas such as slow-release mono-dose tetanus vaccine and school health programme as well as advocacy on political will for the sustainability of immunization programmes of women of child-bearing age.
Keywords: Immunization, neonatal tetanus, prevention
INTRODUCTION
Neonatal tetanus is a preventable disease with high mortality and accounts for about 5-7% of neonatal death globally,1,2,3 mostly in developing countries. Management is mainly focused on relief of symptoms and the prevention of complications such as aspiration pneumonia. A meticulous nursing care is required to prevent occurrence of complications and death caused due to neonatal tetanus.
According to the World Health Organization (WHO)'s Global Immunization News of March, 2013, Nigeria is one of 30 remaining high-risk countries that have not achieved the Maternal and Neonatal Tetanus Elimination (MNTE) goal yet.4 Available data indicates that 18 states (out of 37) are at risk for maternal and neonatal tetanus.4 Many hospital based studies have identified neonatal tetanus as a problem of high magnitude in Nigeria.5,6,7,8 Maternal immunization and improved obstetric and neonatal care are the main strategies in Nigeria for improving protection against neonatal tetanus.4 Recently, the high-risk approach of conducting tetanus toxoid (TT) Supplementary Immunization Activities (SIAs) targeting women of reproductive age was conducted in three states of the federation and selected Local Government Areas (LGAs) in 5 other states including Borno. Health education to modify harmful cultural practices that directly encourage the risk of acquisition of tetanus is also useful.9,10 Nigeria plans to achieve elimination in a phased manner by focusing on two zones (South-east and South-west) in 2013-2014 followed by the remaining four zones. The bulk of African Countries, Nigeria inclusive, have a very young population with more women in reproductive age group.11 This further underscores the need for increase action towards maternal tetanus immunization of women of child-bearing age if the scourge is to be controlled.
There is a dearth of literature on neonatal tetanus from North-eastern Nigeria.
PATIENTS AND METHODS
A retrospective study of cases of neonatal tetanus in the University of Maiduguri Teaching Hospital (UMTH) over a 2-year period, from January 2009 to December 2010 was carried out.
The folders of all cases of neonatal tetanus admitted to the Special Care Baby Unit (SCBU), University of Maiduguri Teaching Hospital over the period under review were retrieved.
Information of the patients extracted included the sex, age, date of admission, date of discharge, total duration of hospital stay, place of delivery, cord care, probable portal of entry/site of injury, presenting complaints, period of onset, examination findings, diagnosis, associated morbidity/complications, management protocol, prognostic scores and outcome. Maternal information obtained included the maternal immunization status, level of education, occupation and the social class of the children determined. The data obtained were subjected to a statistical analysis, using the chi-squared statistical test, where appropriate. A P-value of <0.05 was considered significant. Tables were used for data presentation where necessary.
Permission to conduct the study was obtained from the Research and ethical committee of UMTH.
RESULTS
There were 71 cases of neonatal tetanus admitted into SCBU of the UMTH over the period under review, representing 4.9% of total admission into the unit. However, folders of 51 cases with complete records were analysed.
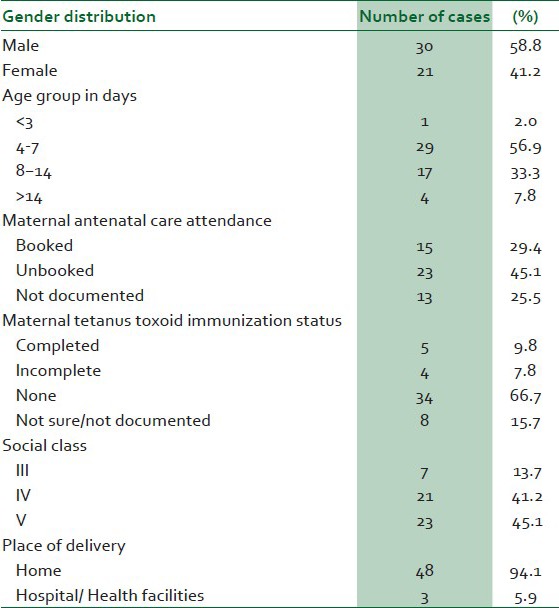
Table 1 summarizes the socio-demographic and clinical characteristics of patients with neonatal tetanus. Of the 51 neonates seen with neonatal tetanus, 30 (58.8%) were males and 21 (41.2%) were females, giving a male: female ratio of 1.4:1.0. Their ages ranged between 3 and 21 days, with a mean and SD of 8.72 ± 4.0 days. Majority of the mothers 34 (66.7%) had no tetanus immunization and most of the patients were from low social class, 23 (45.1%) and 21 (41.2%) in class V and IV, respectively. Most of the mothers 48 (94.1%) delivered at home assisted by traditional birth attendants/relatives in unhygienic settings and only 3 (5.9%) delivered in health facility compared to 15 (29.4%) who attended antenatal care (ANC).
Table 1.
Socio-demographic and clinical characteristics of patients with neonatal tetanus
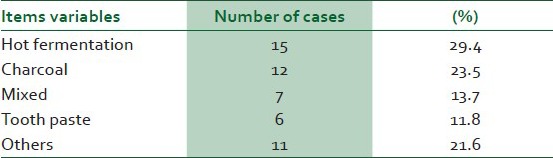
The instruments commonly used in cutting the cords were razor blades and pair of scissors in 28 (54.9%) and 4 (7.8%) cases, respectively. In 18 (35.3%) of the cases, the instruments used were unknown. Table 2 summarizes the items used for cord care.
Table 2.
Various items used for cord care
The probable portal of entry was the umbilical stump in 44 (86.3%) of cases, while 4 (7.8%) and 3 (5.9%) cases were from scarification marks and mixed portal of entry, respectively.
Sepsis was identified as co-morbidity in 26 (51%) of the patients.
Twenty-one (52.5%) of the neonates had onset period less than 48 hours, while 17 (42.5%) had onset period greater than 48 hours. Eleven (21.6%) of the patients had no documented onset period.
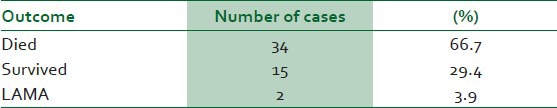
Table 3 summarizes the severity of the disease in the patients managed, while Tables 4 and 5 show the duration of hospitalization and the outcome of the patients, respectively.
Table 3.
Severity of neonatal tetanus
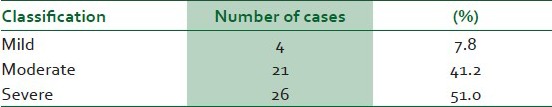
Table 4.
Duration of hospital stay of patients with neonatal tetanus
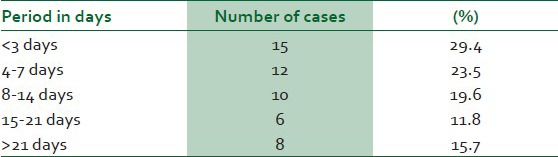
Table 5.
Outcome of patients with neonatal tetanus
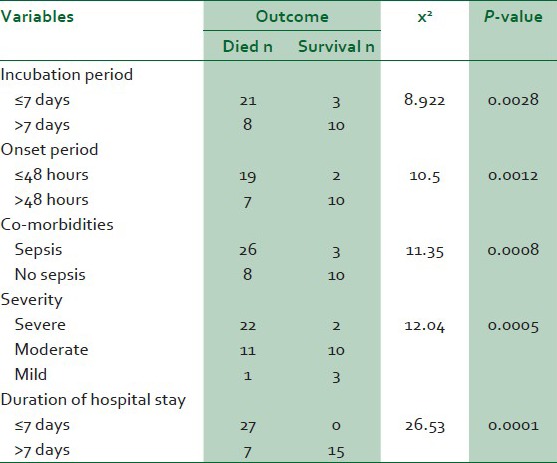
Clinical variables such as incubation period, onset period, co-morbidities, severity of the disease and duration of hospital stay all had statistically significant effect on the patients’ outcome [Table 6].
Table 6.
Relationship between variables and outcome of patients with neonatal tetanus
DISCUSSION
This study reviews neonatal tetanus in a tertiary health facility in Maiduguri. Neonatal tetanus is still a significant cause of neonatal morbidity and mortality, accounting for 4.9% of all admissions into the SCBU over the period under review with fatality rate of 66.7%.
It has been reported that neonatal tetanus accounts for 5-7% of worldwide neonatal mortality.1,2,3 This is despite over two decades of commitments by the public health community globally to the elimination of tetanus (defined as fewer than one case of neonatal tetanus per livebirths in all districts) by 199512 as well as the renamed initiative of maternal and neonatal tetanus elimination by 2005, a decade ago.13 The high prevalence and mortality reported in this study is unacceptable in the 21st century. This could be due to the declining immunization coverage observed in this study with only 9.8% of mothers having had full immunization. In addition, harmful traditional practices towards cord care such as hot fomentation, application of charcoal, etc., would have also contributed. Other studies have reported similar effects of these factors on neonatal tetanus.9,10,14
The preponderance of male neonates with neonatal tetanus in this study is in accord with previous studies.5,6,15,16 The reason for this finding is not clear, however, it could be partly explained by the preference given to the male child in the society that makes parents to seek for medical attention promptly. Majority of mothers of the neonates with neonatal tetanus were not immunized against tetanus, a trend consistent with findings of other studies.5,15,17 The high proportion of unimmunized and incompletely immunized mothers (74.5%) could be attributed to the low ANC attendance (29.4%) among these women. In addition, the higher proportion of booked mothers when compared to those with complete or incomplete immunization (17.6%) suggest that missed opportunity of tetanus vaccination among pregnant women attending ANC would have contributed to the observed high rate of unimmunization. This finding is consistent with previous studies.18,19
The parents of most of the patients with neonatal tetanus are of low socio-economic status as reported by other workers20,21,22 which is a documented factor associated with increased risk of neonatal tetanus.
A high number of neonates with neonatal tetanus in this study were delivered at home, and the main portal of entry for the organism was the umbilical cord as a result of unhygienic umbilical cord care practices. This finding is similar to previous findings7,8,9,20,23 There were no cases of circumcision or ear piercing recorded as probable portal of entry.
The prognosis of neonatal tetanus is strongly influenced by both the incubation and onset periods. Short incubation and onset periods correlates with increased disease severity and higher mortality.24,25,26,27,28
This study confirms that co-morbidities such as sepsis identified in these patients worsen the severity of the illness as previously reported,29,30,31 that about half of the neonates with neonatal tetanus also have sepsis and contribute significantly to neonatal mortality.
The overall case-fatality of 66.7% in the present study falls within the range of 3.9-79.4% reported in Nigeria.16,20 The varied rates were attributed to difference in incubation and onset periods, associated co-morbidities as well as improvement in management.32
In conclusion, despite various programmes and concerted efforts towards elimination of neonatal tetanus, with readily available effective vaccine, the high prevalence and mortality reported across the country is disappointing. Therefore, there is need to explore research and development trend at improving access points of vaccination such as slow-release mono-dose tetanus vaccine. This will undoubtedly improve compliance and lessen need of repeated injection.33 In addition; revamping the school health programme in primary and secondary schools all over the country and incorporating mandatory TT vaccination will provide a good operational opportunity. Hence, all efforts must be re-focused on strengthening the current strategies while developing new ones as well as advocacy on political will for the sustainability of immunization programmes in Nigeria.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Brye J, Boschi-Pinto C, Shibuya K, Black RE. WHO estimates of the causes of death in children. Lancet. 2005;365:1147–52. doi: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed] [Google Scholar]
- 2.Lawn JE, Cousens S, Darmstadt GL, Paul V, Martines J. Why are 4 million newborn babies dying every year? Lancet. 2004;364:2020. doi: 10.1016/S0140-6736(04)17511-9. [DOI] [PubMed] [Google Scholar]
- 3.Vandelaer JH, Birmingham M, Gasse FL, Kurain M, Shaw C, Garnier S. Tetanus in developing countries: An update on the Maternal and Neonatal Tetanus Elimination Initiative. Vaccine. 2003;21:3442–5. doi: 10.1016/s0264-410x(03)00347-5. [DOI] [PubMed] [Google Scholar]
- 4.Adovohekpe P, Onimisi A, Ekpemauzor C. WHO. Global Immunization News March; 2013. Planning meeting on maternal and neonatal tetanus elimination in Nigeria. [Google Scholar]
- 5.Osinusi K, Dawodu AH, Sodeinde O, Adeyokunnu AA. Neonatal tetanus in Ibadan. Niger J Paediatr. 1986;13:121–5. [Google Scholar]
- 6.Oruamabo RS, Mbuagbaw LT. Neonatal tetanus in Port Harcourt. Niger J Paediatr. 1986;13:115–20. [PubMed] [Google Scholar]
- 7.Hassan B, Popoola A, Olokoba A, Salawu FK. A survey of Neonatal tetanus at a district hospital in North-east Nigeria. Trop Doct. 2011;41:18–20. doi: 10.1258/td.2010.100310. [DOI] [PubMed] [Google Scholar]
- 8.Owa JA, Makinde OO. Hospital survey of Neonatal tetanus at Obafemi Awolowo University Teaching Hospital Complex, Ile-Ife. Niger Med Pract. 1995;30:56–9. [Google Scholar]
- 9.Ambe JP, Bello M, Yahya SJ, Omotara BA. Umbilical cord care practices in Konduga local government area of Borno State, North-eastern Nigeria. The Internet J Trop Med. 2009:5. [Google Scholar]
- 10.Abhulimhen-Ihoha BI, Ofili A, Ibadin MO. Cord care practices among mothers attending immunization clinic at the University of Benin Teaching Hospital, Benin City. Niger J Paediatr. 2011;38:104–8. [Google Scholar]
- 11.Cincotta R. The future of sub-Saharan Africa's tentative fertility decline. [Last accessed on 2012 Mar 7]. Available from: http://www.newsecuritybeatorg/2010/08/future-of-sub-sharan-africas-tentative_25.html .
- 12.Anonymous. Expanded programme on immunization. The global elimination of neonatal tetanus: Progress to date. Wkly Epidemiol Red. 1993;68:277–82. [PubMed] [Google Scholar]
- 13.Geneva: World Health Assembly; 1989. WHO. WHA. 42.32 Expanded Programme on Immunization. World Health Assembly Resolutions and Decisions. [Google Scholar]
- 14.Abdulkarim AA, Ibrahim RM, Fawi AO, Adebayo OA, Johnson A’WBR. Vaccines and immunization: The past, present and future in Nigeria. Niger J Paediatr. 2011;38:186–94. [Google Scholar]
- 15.Ibadin MO, Omoigberale AI. Neonatal tetanus in Benin City, Nigeria: A decade after commencement of Expanded programme on immunization (EPI) Niger Med J. 1996;5:55–7. [Google Scholar]
- 16.Okoromah CN, Lesi FEA, Egri-Okwaji MTC, Iroha EO. Clinical and management factors related to outcome in Neonatal tetanus. Niger Postgrad Med J. 2003;10:92–5. [PubMed] [Google Scholar]
- 17.Taiwo O, Senbanjo T, Adamolekun B. Maternal immunization status in Neonatal tetanus. Niger J Paediatr. 1992;19:6–8. [Google Scholar]
- 18.Adiega A, Omilabu SA, Audu RA, Sanni F, Lakehinde GP, Balogun O, Olagbaju O. Tetanus toxoid immunization coverage among mothers of children below one year of age in difficult-to-reach area of Lagos metropolis. Afr J Clin Exper Microbiol. 2005;6:233–7. [Google Scholar]
- 19.Maral I, Bayka Z, Aksakal FN, Kayikcioglu F, Burmin MA. Tetanus immunization in pregnant women: Evaluation of maternal tetanus vaccination status and factors affecting rate of vaccination coverage. Public Health. 2001;115:359–64. doi: 10.1038/sj/ph/1900780. [DOI] [PubMed] [Google Scholar]
- 20.Asekun-Olarinmoye EO, Lawoyin TO, Onadeko MO. Risk factors for neonatal tetanus in Ibadan, Nigeria. Eur J Pediatr. 2003;162:526–7. doi: 10.1007/s00431-003-1225-8. [DOI] [PubMed] [Google Scholar]
- 21.Asekun-Olarinmoye EO, Lawoyin TO, Onadeko MO. Risk factors associated with neonatal tetanus in Ibadan, Nigeria - a revisit. Afr J Med Sci. 2003;32:275–8. [PubMed] [Google Scholar]
- 22.Oruamabo RS. Neonatal tetanus in Nigeria: Does it still pose a major threat to neonatal survival? Arch Dis Child. 2007;92:9–10. doi: 10.1136/adc.2006.102087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nte AR, Mayuku A, Oruamobo RS. Neonatal and post neonatal tetanus: The time to act is now. Niger J Paediatr. 2002;29:85. [Google Scholar]
- 24.Roper MH, Vandelaer JH, Gasse FL. Maternal and neonatal tetanus. Lancet. 2007;370:1947–59. doi: 10.1016/S0140-6736(07)61261-6. [DOI] [PubMed] [Google Scholar]
- 25.Osinusi K, Njinyam MN. A new prognostic scoring system in neonatal tetanus. Afr J Med Sci. 1997;26:123–5. [PubMed] [Google Scholar]
- 26.Thwaites CL, Yen LM, Glover C, Tuan PQ, Nga NT, Parry J, et al. Predicting the clinical outcome of tetanus: The tetanus severity score. Trop Med Int Health. 2006;11:279–87. doi: 10.1111/j.1365-3156.2006.01562.x. [DOI] [PubMed] [Google Scholar]
- 27.Davies-Adetugbo AA, Torimiro SE, Ako-Nai KA. Prognostic factors in neonatal tetanus. Trop Med Int Health. 1998;3:9–13. doi: 10.1046/j.1365-3156.1998.00162.x. [DOI] [PubMed] [Google Scholar]
- 28.Eregie CO. Epidemiological factors associated with neonatal tetanus mortality; observation from a cluster survey in Nigeria. East Afr Med J. 1993;70:434–7. [PubMed] [Google Scholar]
- 29.Oyelami OA, Owa JA, Olusanya IO. Septicaemia associated with neonatal tetanus. Cent Afr J Med. 1995;41:171–3. [PubMed] [Google Scholar]
- 30.Antia-Obong OE, Ekanem EE, Udo JJ, Utsalo SJ. Septicaemia among neonates with tetanus. J Trop Pediatr. 1992;38:173–5. doi: 10.1093/tropej/38.4.173. [DOI] [PubMed] [Google Scholar]
- 31.Egri-Okwaji MTC, Iroha EO, Kesah CN, Odugbemi TO. Bacteria causing septicaemia in neonates with tetanus. West Afr J Med. 1998;17:138–9. [PubMed] [Google Scholar]
- 32.Airede A’KI, Okuonghae HO. Neonatal tetanus: Incidence and improved outcome with diazepam. Dev Med Child Neurol. 1992;34:448–53. doi: 10.1111/j.1469-8749.1992.tb11458.x. [DOI] [PubMed] [Google Scholar]
- 33.Dineshkumar B, Dhanaraj SA, Santhi K, Vijayan P, Raghu C. Single dose vaccine delivery system of tetanus toxoid formulation based on chitosan microspheres. Int J Adv Pharm Sci. 2010;1:42–9. [Google Scholar]


