Abstract
Background:
Uterine rupture has continued to be a catastrophic feature of obstetric practice especially in the low-resource settings. This study determined the incidence, predisposing factors, treatment options and feto-maternal outcome of ruptured uterus.
Materials and Methods:
A 10-year retrolective study of all cases of uterine ruptures that were managed in Nnamdi Azikiwe University Teaching Hospital, Nnewi, Nigeria between 1st January, 2001 and 31st December, 2010 was undertaken. The proforma was initially used for data collection, which was transferred to a data sheet before entering them into the Epi-info software. Analysis was done using Epi info 2008 (version 3.5.1).
Results:
Out of 5,585 deliveries over the study period, 47 had uterine rupture, giving an incidence of 0.84% or 1 in 119 deliveries. All the patients were multiparous and majority (63.8%) was unbooked. Traumatic (iatrogenic) rupture predominated (72.1%). Uterine repair with (55.8%) or without (34.9%) bilateral tubal ligation was the commonest surgery performed. Case fatality rate was 16.3%, while the perinatal mortality rate was 88.4%. Average duration of hospitalization following uterine rupture was 10.3 days.
Conclusion:
Uterine rupture constituted a major obstetric emergency in the study hospital and its environs. The incidence, maternal and perinatal mortalities were high. The traumatic/iatrogenic ruptures constituted the majority of cases, hence, majority of the cases are preventable. There is therefore a dire need for education of our women on health-related issues, utilization of available health facilities, adequate supervision of labour and provision of facilities for emergency obstetric care.
Keywords: Fetomaternal outcome, perinatal mortality, risk factors, uterine rupture, unbooked
INTRODUCTION
Uterine rupture has continued to be a catastrophic feature of obstetrics practice in the low-resource settings in countries like Nigeria.1,2,3,4 It is life threatening to both the mother and the foetus.5,6,7,8 The lack of access to emergency obstetric care facilities and the low utilization of modern maternal services are the identified causes of higher incidence of uterine rupture in developing countries than in the developed countries.3,8,9
Most reports have identified not registering for antenatal care as a risk factor for uterine rupture.3,4,10,11 Maternal case fatality rates as high as 10.3% and 16.0% have been reported, while the foetal mortality rates are even much higher at 70%12 and 90%.13,14,15,16 However, mothers that escape mortality are left to suffer morbidities such as anaemia, wound and genital sepsis and burst abdomen.7,15 Others, in addition, lose their uterus and compromise their future fertility.15
Against this backdrop, this study aims to determine the incidence, predisposing risk factors, treatment options and maternal and foetal outcomes of patients with ruptured uterus in Nnamdi Azikiwe University Teaching Hospital, Nnewi, Nigeria. This study aims to assist in planning interventions that will reduce the incidence, morbidity and mortality associated with uterine rupture.
MATERIALS AND METHODS
This is a cross-sectional study with retrolective study of cases of uterine rupture in Nnamdi Azikiwe University Teaching hospital between 1st January, 2001 and 31st December, 2010. The names and hospital number of all the cases of uterine rupture in the hospital over a 10-year period were obtained from the labour ward and operating theatre registers.
A thorough scrutiny of the delivery records of the obstetric unit as well the records of the Medical Records Department and special care baby unit (SCBU) of the hospital was done to identify these patients by checking on their names, case file numbers and their diagnosis at the time of presentation in the labour ward and subsequent management of their babies on admission to SCBU. Their case files were subsequently retrieved and studied.
The labour ward register also provided information on the total number of deliveries. Of all the 5,585 deliveries during the study period, 47 cases of uterine rupture were recorded. Only 43 case files (91.5%) were retrieved from the medical records department of the hospital and were used subsequently for analysis. The information on the age, parity, number of living children, booking status, risk factors and the type/extent of rupture were extracted. The other information extracted included site of rupture, type of surgery performed, maternal and foetal outcome and the length of hospital admission. The rupture is described as traumatic if oxytocin infusion was used for induction or augumentation of labour. The study received the hospital's ethical committee approval.
The descriptive statistics was used in calculating percentages, means and standard deviation. Data analysis was done using Epi info 2008 (v 3.5.1; Epi Info, Centers for Disease Control and Prevention, Atlanta, GA).
RESULTS
During the study period, there were a total of 47 cases of uterine rupture out of 5,585 deliveries, giving an incidence of 1 in 119 deliveries or 0.84% or 8.4 per 1000 deliveries. Only 43 women were included in further analysis.
The mean age of the patients was 31.2 years ± 4.3, while the majority (34, 74.5%) were ≥30 years. However, none of the patients was aged ≤20 years and two of them were aged >35 years. The majority of the patients (14, 32.6%) were Para 1 and 2, while the remaining (6, 14.0%) were Para 3 and 4. Three of the patients were grand multiparous (parity ≥5) and none of the patients was nulliparous (parity = 0). Majority belonging to parity 1 and 2 had prior caesarean section scars.
Only 13 (30.2%) of the patients were registered for antenatal care (booked). The majority of the patients (30, 63.8%) did not register for their antenatal care (unbooked). Majority of the patients (13, 30.2%) had no living child, 11 (25.6%) and seven (16.3%) had two and one living children, respectively. Only three patients had more than four living children.
Table 1 shows the type of uterine rupture and the factors attributable to the rupture. All but two of the uterine ruptures occurred when the patients were in labour. Complete ruptures were seen in 38 patients (88.4%), while incomplete rupture occurred in only five patients (11.6%).
Table 1.
Aetiological factors attributable to uterine rupture
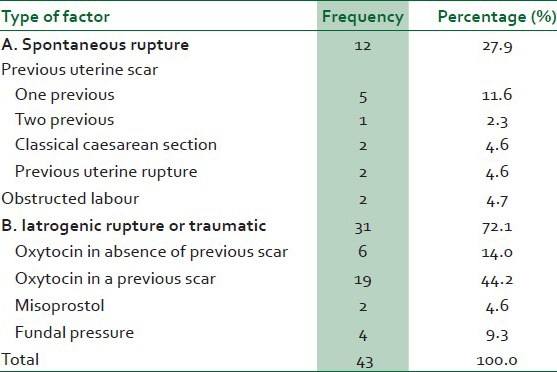
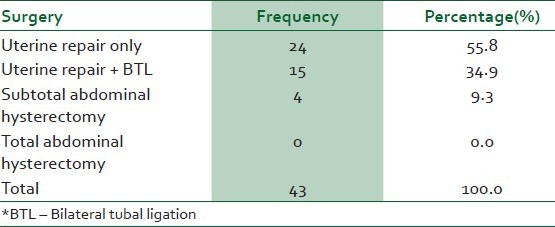
Table 2 shows the type of surgery performed at laparotomy for the patients who had uterine rupture. The majority (18, 41.9%) of the rupture occurred at the lateral uterine segment, followed by 15 (34.8%) and 10 (23.3%) at the anterior and posterior segments respectively. Some patients had more than one site of uterine segment involved in the rupture and up to seven (16.3%) patients had uterine rupture along the previous lower segment scar.
Table 2.
Types of surgery performed in patients with uterine rupture over a 10-year period
There were seven maternal deaths out of the 43 cases reviewed, giving a case fatality rate of 16.3%. All but one of the maternal deaths occurred in the unbooked patients; the booked patient involved had hyperstimulation from misoprostol, which was used for cervical ripening. There were 38 perinatal deaths given a perinatal mortality rate of 88.4% or 884 in 1000 deliveries. The average hospital stay was 10.3 days (8-15 days).
DISCUSSION
In the present study, the overall incidence of uterine rupture was 1 in 119 deliveries or 0.84%. This figure was higher than that in several reports from other parts of Nigeria, such as 0.33% in Ilorin,16 0.4% in Ife,17 0.5% in Lagos,5 0.53% in Enugu14 and 0.72% in Ibadan.15 The lowest incidence was found in the western world, with rates of 0.4 per 1000 being recorded.15
A number of factors may be responsible for the wide variation in the incidence of uterine rupture in Nigeria. These include the obstetric risk factors (previous caesarean section scar, not registering of antenatal care) operative in a given population, the capability of obstetric personnel, the facilities available for obstetric care of the patients and the utilization of the facilities by the resident population.6,15
Unfortunately, in Nigeria, most of the factors still operate and downturn of the economy has not helped matters. People wittingly or unwittingly have allowed spiritual churches to attend to them in labour at little or no cost.18,19,20 The trend of trial of vaginal birth after caesarean section (VBAC) and obstetric manoeuvres in breech presentation may be contributory. It is not surprising that the majority (>60%) of the patients with uterine rupture was unbooked and had not availed themselves of available obstetric services in the index pregnancy. This figure compares favourably with reports in various parts of Nigeria and Africa,5,6,8,11,17 supporting the notion that lack of antenatal care was associated with increased maternal and foetal morbidity in uterine rupture.3,4,10,11
The age and parity distributions were similar to several reports in various part of the country. Incidence of uterine rupture was highest in Para 1 and Para 2 groups and generally occurred between the Para 1 and Para 4 groups. This is similar to previous studies in Lagos,5 Ile-Ife,17 Enugu14 and Ibadan,15 all in Nigeria. The nulliparous uterus has been described as being ‘virtually immune to rupture’,21 especially before the onset of contractions. None of the patients in our study was nulliparous, which supports the above saying; however, other studies in other parts of Nigeria have found uterine rupture in nulliparous and grand multiparous women.14,15 Isolated case reports of uterine rupture in the primigravida have been described in association with connective tissue disease,22 chronic steroid use22 and cocaine misuse.23
In the majority of cases (72.1%), traumatic rupture contributed to these cases of uterine rupture. This resulted from the use of oxytocin infusion in both the scarred and unscarred uteri. Induction of labour either with oxytocin or prostaglandins is an independent risk factor for uterine rupture in women with scarred uterus.24,25,26,27 Application of fundal pressure in the second stage of labour was contributory. The incidence of iatrogenic rupture has been directly linked to the number of skilled personnel attending to the patients.14 Spontaneous rupture occurred in only 12 (27.9%) of the patients similar to report in Enugu,14 but different from reports from other subregions and countries where its contribution was higher than in iatrogenic uterine rupture.16,28
The overall incidence of caesarean section in the study centre in 2008 was 26.9%.29 This incidence appears to be increasing since then. This means that this will likely influence the epidemiology of uterine rupture in the future as some patients who had prior caesarean section may have uterine rupture based on extrapolation in the present study. Some of which might fail to present to hospitals in their subsequent pregnancy, only to present when they had already ruptured their uterus.
Complete uterine rupture in which the foetus was already extruded into the peritoneal cavity was observed in most cases (88.4%). In these cases, majority of the foetus were dead, reflecting the high perinatal mortality rate.
Majority (90.7%) of the patients had uterine repair [(with or without bilateral tubal ligation (BTL)]. Uterine repair alone was the commonest procedure probably because majority of the women were in their lower parity and had desire for more children. The findings of greater number of subtotal hysterectomy performed over total hysterectomy have been similarly reported in various regions in Nigeria.5,8,14,15,17 Two patients in this study had previous uterine rupture. They subsequently had repeat uterine rupture. Although most women with a previous uterine rupture with meticulous tertiary level antenatal care may have a favourable outcome in subsequent pregnancies, child birth after uterine rupture is not to be recommended routinely.30
The maternal mortality of 16.3% obtained in this study was high and compares with 17.0% in Ile-Ife,17 17.5% in Lagos5 and 17.9% in Ibadan, all in Nigeria. Some other regions recorded lower fatality rates, including 10% in Malawi,12 11% in Sokoto, Nigeria31 and 13 % in Enugu, Nigeria.14 Delay in arrival and receiving emergency obstetric care (EMOC) were the main reasons for the high case fatality in uterine rupture.8,31
The average hospital stay was 10.3 days. This was similar to a report from Ibadan,15 where 96% of the patients spent more than 7 days in the hospital. This is noteworthy because prolonged admission, especially without early ambulation, increases post-operative morbidity and adds to the economic loss to the patient.
LIMITATIONS
Limitations of the present analysis also need to be addressed. The main weakness is that the reasons why majority of the paturients were unbooked could not be explained by our study. Cultures and religious beliefs may appear to positively relate to higher rates of uterine rupture in our study. Furthermore, psychosocial factors such as ignorance and socioeconomic factors such as income and social class could have explained more variance in the uterine rupture, which we did not evaluate in the present study. Another limitation is the retrolective study design, where some data could have been missed.
CONCLUSION
Uterine rupture constitutes a major obstetric emergency in the study hospital and has potentially catastrophic implications for the mother and the baby. It is associated with high maternal and foetal mortality and morbidity. Iatrogenic rupture, especially in scarred uterus constituted the majority of the cases. Caesarean section rates are rising and hence a concomitant rise in incidence of uterine rupture is expected. There is a dire need for antenatal care and skilled attendants at delivery, and this should be emphasized through health education. Patients with scarred uterus must be adequately counselled on the need for hospital delivery in their subsequent pregnancy. Assessment of risk factors for uterine rupture is important both antenatally and in the intrapartum period. Careful selection of patients for trial of VBAC and adequate training of doctors and midwives to detect the early warning symptoms and signs of uterine rupture is advocated. Caution should be exercised with the use of oxytocics, especially during augmentation of poorly progressing multiparous women and those with prior caesarean section.
Finally, most of the cases of uterine rupture are preventable. Strategies should be aimed at improving the access to healthcare services and provision of resources to deal with obstetric emergencies. Timely diagnosis and institution of swift and appropriate interventions would help save the lives of mothers and their babies.
ACKNOWLEDGEMENT
We remain grateful to all the consultants, resident doctors and nurse mid-wives who managed the cases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ezegwui HU, Nwogu-Ikojo EE. Trends in uterine rupture in Enugu, Nigeria. J Obstet Gynaecol. 2005;25:260–2. doi: 10.1080/01443610500060768. [DOI] [PubMed] [Google Scholar]
- 2.Ekpo EE. Uterine rupture as seen in the university of Calabar Teaching Hospital, Nigeria: A five-year-Review. J Obstet Gynaecol. 2000;20:154–6. doi: 10.1080/01443610062922. [DOI] [PubMed] [Google Scholar]
- 3.Ebeigbe PN, Enabudoso E, Ande BA. Ruptured uterus in a nigerian community: A study of sociodemographic and obstetric risk factors. Acta Obstet Gynaecol Scand. 2005;84:1172–4. doi: 10.1111/j.0001-6349.2005.00778.x. [DOI] [PubMed] [Google Scholar]
- 4.Ezechi OC, Mabayoje P, Obiesie LO. Ruptured uterus in south western Nigeria: A reappraisal. Singapore Med J. 2004;45:113–6. [PubMed] [Google Scholar]
- 5.Ola RE, Olamijulo JA. Rupture of the uterus at the Lagos University Teaching Hospital, Lagos, Nigeria. West Afr J Med. 1998;17:188–93. [PubMed] [Google Scholar]
- 6.Konje JC, Odukoya OA, Ladipo OA. Ruptured uterus in Ibadan: A twelve-year-review. Int J Gynaecol Obstet. 1990;32:207–13. doi: 10.1016/0020-7292(90)90347-n. [DOI] [PubMed] [Google Scholar]
- 7.Johanson R. Ruptured uterus. In: Edmonds K, editor. Dewhursts Textbook of Obst. And Gynae. For postgraduates. 6th ed. Hoboken: Blackwell Scientific Pub; pp. 323–4. [Google Scholar]
- 8.Ekele BA, Audu LR, Muyibi S. Uterine rupture in Sokoto, Northern Nigeria – are we winning? Afr J Med Med Sci. 2000;29:191–3. [PubMed] [Google Scholar]
- 9.Ibekwe PC. Ruptured uterus in a primigravida: A case report. Trop J Obstet Gynaecol. 2002;19:47–8. [Google Scholar]
- 10.Onwuhafua P, Onwuhafua A, Omekara D, Ibrahim R. Ruptured uterus in Kaduna, Nigeria: A six-year-review. J Obstet Gynaecol. 1998;18:419–23. doi: 10.1080/01443619866688. [DOI] [PubMed] [Google Scholar]
- 11.Okonta PI, Igberase GO. A comparison of booked and unbooked patients with ruptured uterus in A referral hospital in the Niger Delta region of Nigeria. Nigeria J Med. 2007;16:129–32. doi: 10.4314/njm.v16i2.37295. [DOI] [PubMed] [Google Scholar]
- 12.Phillips JA. Ruptured uterus in mulanje CCAP Hospital, 1974-1982. Trop Doct. 1990;20:175–6. doi: 10.1177/004947559002000414. [DOI] [PubMed] [Google Scholar]
- 13.Diallo FB, Idi N, Vangeenderhuysen, Baraka D, Hadiza I, Garba M, et al. Uterine rupture at the Niamey Central Maternity Reference Center, Nigeria. Epidemiologic features and prevention strategies. Dakar Med. 1998;43:74–8. [PubMed] [Google Scholar]
- 14.Ibekwe PC. Ruptured uterus in Enugu, Nigeria. Port Harcourt Med J. 2008;2:136–9. [Google Scholar]
- 15.Ogunnowo T, Olayemi O, Aimakhu CO. Uterine rupture: UCH, Ibadan experience. West Afr J Med. 2003;22:236–9. doi: 10.4314/wajm.v22i3.27957. [DOI] [PubMed] [Google Scholar]
- 16.Aboyeji AP. Ruptured uterus in Ilorin. A 5 year Review. Niger Med Pract. 1997;33:5–8. [Google Scholar]
- 17.Faleyimu BL, Ogunniyi SO, Makinde OO. Rupture of the gravid uterus in ife, Nigeria. Trop Doct. 1990;20:188–9. doi: 10.1177/004947559002000425. [DOI] [PubMed] [Google Scholar]
- 18.Udoma EJ, John ME, Udosen GE, Udo AE. Obstetrics practices in spiritual churches in South Eastern Nigeria. Mary Slessor J Med. 2003;3:51–6. [Google Scholar]
- 19.Udoma EJ, Ekanem AD, John ME, Eshiet AI. The role of institutional factors in Maternal Mortality from obstructed labour. Global J Med Sci. 2003;2:13–7. [Google Scholar]
- 20.Udoma EJ, Ekanem AD, Abasittai AM, Bassey EA. Factors contributing touterine rupture in women having vaginal births after caesarean section. Trop J Obstet Gynaecol. 2005;22:177–9. [Google Scholar]
- 21.O"Driscoll K, Meagher D, Robson M. 4th ed. London: Mosby; 2004. Active Management of Labour: The Dublin Experience; pp. 223–62. [Google Scholar]
- 22.Gelbmann CM, Kollinger M, Gmeinwieser J, Leser HG, Holstege A, Scholmeric J. Spontaneous rupture of lever in a patient with Ehlers Danlos disease type IV. Dig Dis Sci. 1997;42:1724–30. doi: 10.1023/a:1018869617076. [DOI] [PubMed] [Google Scholar]
- 23.Gonsoulin W, Borge D, Moise KJ., Jr Rupture of unscarred uterus in primigravid woman in association with cocaine abuse. Am J Obstet Gynecol. 1990;163:526–7. doi: 10.1016/0002-9378(90)91189-j. [DOI] [PubMed] [Google Scholar]
- 24.Kwee A, Bots ML, Visser GH, Bruinse HW. Obstetric management and outcome of pregnancy in women with a history of caesarean section in the Netherlands. Eur J Obstet Gynecol Reprod Biol. 2007;132:171–6. doi: 10.1016/j.ejogrb.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 25.Locatelli A, Ghidini A, Ciriello E, Incerti M, Bonardi C, Regalia AL. Induction of labour: Comparison of a cohort with uterine scar from previous caesarean sectionvs a cohort with intact uterus. J Matern Fetal Neonatal Med. 2006;19:471–5. doi: 10.1080/14767050600746654. [DOI] [PubMed] [Google Scholar]
- 26.Kayani S, Alfirevic Z. Uterine rupture after induction of labour in women with previous caesarean section. BJOG. 2005;112:451–5. doi: 10.1111/j.1471-0528.2004.00336.x. [DOI] [PubMed] [Google Scholar]
- 27.Yogev Y, Ben-Haroush A, Lahav E, Horowitz E, Hod M, Kaplan B. Induction oflabour with prostaglandin E2 in women with previous caesarean section and unfavourable cervix. Eur J Obstet Gynecol Reprod Biol. 2004;116:173–6. doi: 10.1016/j.ejogrb.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 28.Padhye SM. Rupture of the pregnant uterus – a 20 year review. Kathmandu Univ Med J (KUMJ) 2005;3:234–8. [PubMed] [Google Scholar]
- 29.Eleje GU, Udigwe GO, Akabuike JC, Eke AC, Eke NO, Umeobika JC. The rate of Caesarean section in Nnewi, Nigeria: A 10-year Review. Afrimedic J. 2010;1:11–4. [Google Scholar]
- 30.Chibber R, El-Saleh E, Al Fadhli R, Al Jassar W, Al Harmi J. Uterine rupture and subsequent pregnancy outcome – how safe is it? A 25-year study. J Matern Fetal Neonatal Med. 2010;23:421–4. doi: 10.3109/14767050903440489. [DOI] [PubMed] [Google Scholar]
- 31.Ahmed Y, Shehu CE, Nwobodo EI, Ekele BA. Reducing maternal mortality from ruptured uterus – The Sokoto Initiative. Afr J Med Sci. 2004;33:135–8. [PubMed] [Google Scholar]


