Abstract
The prevalence of left ventricular diastolic dysfunction (LVDD) sharply increases in women after menopause and may lead to heart failure. While evidence suggests that estrogens protect the premenopausal heart from hypertension and ventricular remodeling, the specific mechanisms involved remain elusive. Moreover, whether there is a protective role of estrogens against cardiovascular disease, and specifically LVDD, continues to be controversial. Clinical and basic science have implicated activation of the renin-angiotensin-aldosterone system (RAAS), linked to the loss of ovarian estrogens, in the pathogenesis of postmenopausal diastolic dysfunction. As a consequence of increased tissue ANG II and low estrogen, a maladaptive nitric oxide synthase (NOS) system produces ROS that contribute to female sex-specific hypertensive heart disease. Recent insights from rodent models that mimic the cardiac phenotype of an estrogen-insufficient or -deficient woman (e.g., premature ovarian failure or postmenopausal), including the ovariectomized congenic mRen2.Lewis female rat, provide evidence showing that estrogen modulates the tissue RAAS and NOS system and related intracellular signaling pathways, in part via the membrane G protein-coupled receptor 30 (GPR30; also called G protein-coupled estrogen receptor 1). Complementing the cardiovascular research in this field, the echocardiographic correlates of LVDD as well as inherent limitations to its use in preclinical rodent studies will be briefly presented. Understanding the roles of estrogen and GPR30, their interactions with the local RAAS and NOS system, and the relationship of each of these to LVDD is necessary to identify new therapeutic targets and alternative treatments for diastolic heart failure that achieve the cardiovascular benefits of estrogen replacement without its side effects and contraindications.
Keywords: diastolic dysfunction, Doppler echocardiography, estrogen, G protein-coupled receptor 30, mRen2, sex differences
heart failure (HF) is a serious, potentially life-threatening condition that affects 5.3 million Americans and is one of the leading hospital discharge diagnoses (1, 72, 142). The prevalence of HF increases with age for both sexes, and, given the aging population, the number of patients with HF is expected to steadily increase. Approximately 2.5 million women in the United States have HF (85), and HF accounts for one-third of all disease-related mortality in American women (11). Nevertheless, HF in women remains a poorly understood syndrome and has not received the same level of public awareness as coronary heart disease (CHD). Although women with HF survive longer than men with HF, they remain symptomatic [e.g., have shortness of breath and difficulty exercising (30), have a lower quality of life (31, 35, 52), and have a significantly higher annual percent increase in hospitalization rates (30, 67, 103, 117, 135)] compared with men with HF. Understanding the sex-based differences in HF will have significant clinical implications, informing both risk factor screening and the development of effective interventions for this vulnerable yet expanding population.
Cardiac dysfunction, with or without systolic dysfunction, is associated with left ventricular (LV) diastolic dysfunction (LVDD). Diastolic dysfunction refers to mechanical and functional abnormalities present during relaxation and filling of the ventricle. It is a preclinical state in which the heart adapts to changes that cause abnormal relaxation or increased LV stiffness by increasing left atrial pressure so that the LV continues to be loaded with the appropriate volume for contraction. Patients with asymptomatic LVDD are included in American College of Cardiology/American Heart Association guidelines as having either stage A or B preclinical HF (66). With LVDD, any abnormal increase in diastolic filling pressure corresponds to a less distensible or less compliant ventricle during the filling phase of the cardiac cycle. Consequently, a “stiff” ventricle is less able to increase its stroke volume without a further elevation of left atrial pressure. Pressure reflected backward through the open mitral valve into the atrium and pulmonary veins can cause shortness of breath, elevation of pulmonary venous pressure, and decreased exercise capacity (5, 73). Thus, the distinction between diastolic HF or HF with preserved ejection fraction (HFPEF) and LVDD is merely the presence of congestive heart failure symptoms. One in six patients with asymptomatic LVDD will develop overt HF symptoms within 5 yr of diagnosis (4, 5).
LVDD, as the precursor to diastolic HF, is seen in both men and women, but it is more prevalent in postmenopausal women, suggesting a link between LVDD and estrogen deficiency. The marked increase in HF incidence in women after 55 yr of age also supports the idea that estrogen confers a protective effect that is lost after menopause (103, 114). However, negative results in clinical trials of hormone replacement therapy (HRT) have led to the speculation that the late initiation of estrogen replacement might not reverse cardiovascular damage or prevent further disease progression (60, 118). While recently completed and ongoing clinical trials continue to explore the “timing hypothesis” (see Ref. 48; http://clinicaltrials.gov/ct2/show/NCT00114517)–that estrogen replacement therapy may have different cardiovascular protective capacity depending on how soon it is given after menopause–reverse translational research is critically important to understand the mechanistic actions of estrogen that are relevant to the maintenance of cardiac diastolic function and structure.
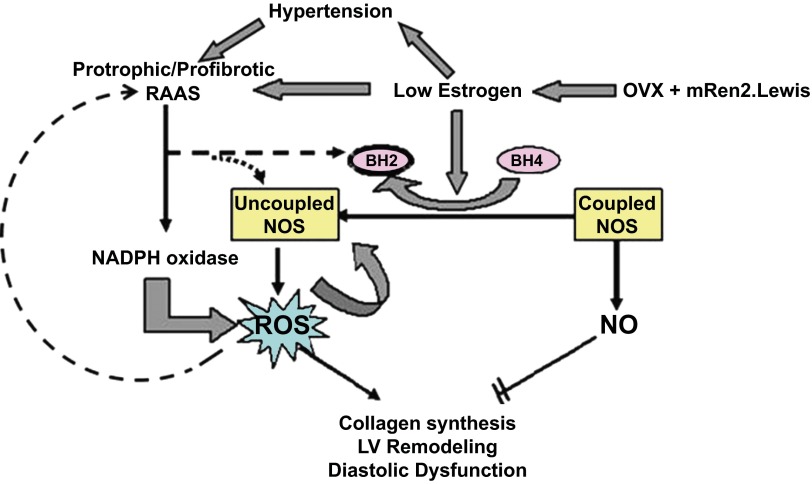
Overwhelming evidence from clinical and basic research has implicated an activated circulating and tissue renin-angiotensin-aldosterone system (RAAS) in the pathogenesis of diastolic dysfunction that occurs after the loss of ovarian estrogens (3, 162). Furthermore, chronic activation of the RAAS increases oxidative stress and reduces nitric oxide (NO) bioavailability in estrogen-sensitive tissues, leading to endothelial dysfunction (164), inflammation (74), and immune dysfunction (43). Each of these processes is associated with obesity, diabetes, renal disease, and hypertension, diseases characterized by reductions in myocardial relaxation and LV compliance. To investigate the relationships between estrogen loss, an activated RAAS, and/or a reduced or maladaptive local cardiac NO synthase (NOS) system in the pathogenesis of diastolic dysfunction, we have used the congenic mRen2.Lewis rat, a monogenetic hypertensive model that overexpresses the mouse renin gene. The female mRen2.Lewis rat is particularly well suited for mechanistic studies of diastolic dysfunction because early bilateral ovariectomy (OVX) in the mRen2.Lewis rat consistently exacerbates increases in systolic blood pressure, LV remodeling (including collagen deposition and myocyte hypertrophy), and diastolic functional impairment (14–16, 41, 63–65, 149, 150), key features emulating the cardiac phenotype of an estrogen-insufficient or -deficient woman (e.g., premature ovarian failure or postmenopausal). Using this model, we have shown that low-dose estrogen replacement (17β-estradiol) or activation of the novel membrane estrogen receptor (ER) G protein-coupled receptor 30 [GPR30; also called G protein-coupled estrogen receptor (GPER)1], with its specific agonist G-1, limits the adverse effects of ovarian hormone loss on blood pressure (81), diastolic function, and cardiac fibrosis, even in the absence of overt alterations in blood pressure (149), in part through deactivation of the circulating and tissue RAAS (150). Additionally, ovarian estrogen loss in this rat model increases renal and cardiac neuronal NOS (nNOS), which exacerbates the effects of salt on renal damage and proteinuria (159, 161), impairs myocardial relaxation, and increases perivascular fibrosis (63); these effects were reversed by treatment with a specific nNOS inhibitor, L-VNIO. Figure 1 shows the potential mechanisms by which estrogen-sensitive hypertension and/or an overactive RAAS modulate cardiac NOS, leading to the formation of ROS and subsequent diastolic dysfunction and LV remodeling.
Fig. 1.
Schema of the potential mechanisms for estrogen loss, hypertension, and/or an overactive renin-angiotensin-aldosterone system (RAAS) on the modulation of cardiac nitric oxide (NO) synthase (NOS) leading to the formation of ROS and subsequent left ventricular (LV) remodeling and diastolic dysfunction. OVX, ovariectomy; BH2, dihydrobiopterin; BH4, tetrahydrobiopterin.
In this review, we briefly discuss the physiological and pathophysiological determinants and Doppler echocardiographic correlates of LVDD relevant to preclinical models of sex-specific hypertensive heart disease and describe recent advances in our understanding of the roles of estrogen loss in the development of diastolic dysfunction and LV remodeling, focusing on the contributions of the cardiac RAAS and NOS system.
Physiological, Pathophysiological, and Echocardiographic Correlates of Diastolic Dysfunction
Hypertension is the primary risk factor for diastolic dysfunction and is the leading cause of diastolic HF in postmenopausal women (56, 122). In the general population, hypertension affects ∼15% of women and 20% of men; however, the prevalence of hypertension increases sharply after menopause, and more women than men become hypertensive as they age (49, 139). Moreover, steep increases in systolic blood pressure and pulse pressure occur after menopause, which have important implications for the maintenance of the diastolic and systolic reserve in the elderly (18, 71, 113). Hypertension in postmenopausal women also results in LV hypertrophy (LVH). LV hypertrophy is a major causative factor in reduced myocardial relaxation and diastolic compliance, which are key cardiac components of diastolic dysfunction. In addition to hypertension, obesity and obesity-related diseases, including insulin resistance and type II diabetes, are associated with the development of LVDD in women (2, 27, 109, 110). Obesity is also one of the strongest risk factors for HFPEF (39, 46, 102).
Recent experimental and clinical evidence also suggest an intriguing link between the kidney and heart that should be considered in the development of LVDD in postmenopausal women. Data from healthy community dwellers show that mild chronic renal insufficiency is a risk factor for diastolic dysfunction (24, 146). Also, patients with diastolic dysfunction who develop clinically significant HF are likely to have renal insufficiency, irrespective of their age, sex, and comorbid conditions (145, 146). Taken together with the risk excess for cardiovascular events that has been demonstrated among postmenopausal women with mild renal dysfunction (e.g., calculated glomerular filtration rate < 70 ml/min) (100, 108), any indication of chronic kidney disease should activate practitioners to screen for early changes in cardiac structure and diastolic function in this population. Although the precise mechanisms underlying the cardiorenal connection to female sex-specific LVDD are not known, findings from the uninephrectomized male rat model suggest that mild renal insufficiency may mediate early cardiac apoptosis and fibrosis (91).
Diastolic dysfunction is associated with abnormalities of active relaxation and passive stiffness of the LV. Active relaxation represents the speed of transition from the contracted state, or systole, to the relaxed state, or diastole, and is related to the reuptake of Ca2+ into the sarcoplasmic reticulum of the contracted myocyte. Passive stiffness is primarily linked to myocardial compliance and the effects of tissue fibrosis. With the advent of Doppler echocardiography, assessment of diastolic function has become increasingly more practical in both the clinical and reverse translational cardiovascular research arenas (112, 124). Several of the more commonly used Doppler echocardiographic parameters of diastolic dysfunction for basic research are shown in Table 1. However, it is important to understand the limitations of this noninvasive tool (92), which primarily reflect on the dynamic nature of the ever-changing diastolic function. For instance, Doppler transmitral velocity early deceleration time and tissue Doppler early diastolic mitral annular velocity (e′) are frequently used measures of myocardial relaxation. Early deceleration time changes with loading conditions, whereas e′ is relatively load independent. Similarly, the transmitral early-to-late filling ratio (E/A) fluctuates with ventricular pressures (5), and e′ is used to distinguish pseudonormal (E/A > 1) from normal filling patterns.
Table 1.
Classification of different stages of diastolic dysfunction relative to control animals with mitral flow and mitral annular velocity by conventional and tissue Doppler imaging and limitations with measures
| Mitral Flow and Tissue Doppler Imaging Parameters | Abbreviation, Units | Impaired Relaxation With Normal Filling Pressure | Impaired Relaxation With Elevated Filling Pressure | Pseudonormal | Restrictive Filling | Limitations |
|---|---|---|---|---|---|---|
| Early filling velocity | E, cm/s | ↓ | ↓ | Same as control | ↑↑ | Loading conditions (e.g., decreased preload induces a decrease in E; increased preload produces an increase E) |
| Ratio of early to late filling velocity | E/A | <1 | <1 | ≤1 | >2 | Loading conditions; heart rate (e.g., fused E and A waves with tachycardia); atrial function (e.g., no A wave with atrial fibrillation) |
| Deceleration time of early filing | DT, ms | ↑ | ↑ | Same as control | ↓ | Loading conditions (e.g., decreased preload produces an increase in DT; increased preload shortens DT) |
| Early mitral annular velocity | e′, cm/s | ↓ | ↓ | ↓ | ↓↓ | Represents regional function; myocardial tethering (e.g., fibrotic myocardium adjacent to normal tissue may show normal e′); septal e′ more load dependent than lateral e′; tachycardia in rodents induces increased e′ |
| Ratio of early diastolic filling velocity to early mitral annular velocity or filling pressure | E/e′ | Same as control | ↑ | Same or slightly increased | ↑↑ | Loading conditions |
↑, increase; ↓, decrease.
As with active relaxation analysis, accurate Doppler echocardiographic measures of intrinsic passive diastolic properties, such as stiffness, are difficult (92). Given that diastolic filling pressure reflects the load-dependent changes in chamber stiffness, the ratio of early transmitral inflow velocity to early mitral annular velocity (E/e′) is used as a biomarker of increased filling pressure (92). As the left atrial pressure increases, early filling (E) increases, reflecting the increased pressure gradient between the atrium and ventricle. Since mitral annular velocity (e′) is unaffected by loading conditions, E/e′ is considered a dynamic index of filling pressure. For instance, E/e′ might be normal at rest but abnormally elevated with exertion, clinically presenting as breathlessness and reduced exercise capacity due to the sudden increase in left atrial pressure (73). Likewise, rats with relatively high E/e′ at rest may exhibit shorter treadmill exercise tolerance times, suggesting a more severe diastolic dysfunction phenotype (42).
Animal Models of Postmenopausal LV Diastolic Function
The OVX rodent model is commonly used to study the role of estrogen in the maintenance of cardiac structure and function as it closely recapitulates the sex hormone milieu of surgical menopause and natural menopause in humans (87). However, despite its frequent use, there are some important limitations of this animal model that are worth mentioning. First, the abrupt loss of ovarian hormones does not model the hormonal transition of perimenopause to menopause (36, 87). Second, the removal of ovaries is performed at different life stages. For example, rodents may undergo OVX at 2–6 mo (regular estrous cycles), 11 mo (the beginning of acyclicity), or 18 mo (the beginning of constant estrous) to include specific age-related factors in the model (87, 132). Young and old rats respond differently to OVX and to exogenous hormone replacement, making it difficult to compare findings across studies (17). Even so, we can glean important insights into the mechanistic functions of ovarian hormones, and particularly estrogen, on the preservation of the female cardiac phenotype. Here we review a few commonly used models that have been helpful for the study of diastolic dysfunction in the context of estrogen loss.
OVX mRen2.Lewis rats.
The mRen2.Lewis strain, which expresses the mouse renin 2 (mRen2) gene, is a congenic model of ANG II-dependent hypertension that is generated by the successive backcross of the (mRen2)27 transgenic rat onto the Lewis background (14). This congenic strain exhibits marked sex differences in the extent of hypertension, with male rats exhibiting higher systolic blood pressures and a greater extent of oxidative stress than female rats of similar age or the background Lewis strain (14, 61, 106, 107). The characterization of this genetic model has further demonstrated that male mRen2.Lewis rats have higher circulating levels of ANG II, angiotensinogen, plasma renin, and serum angiotensin-converting enzyme (ACE) activity compared with female rats, which might explain the observed sex-related differences in cardiovascular pathology and disease progression (107).
In female mRen2.Lewis rats, the loss of estrogen by OVX (performed at 4–5 wk of age) exacerbates hypertension, increases Doppler-derived LV filling pressures, and decreases e′ or myocardial relaxation. These changes can be prevented by the treatment with 17β-estradiol or G-1, a selective agonist of GPR30 (14, 65, 149). Further characterization of this animal model found that estrogen loss by OVX-induced cardiomyocyte hypertrophy and cardiac fibrosis, important processes that contribute to diastolic dysfunction. Moreover, prolonged intake of a high-salt diet by mRen2.Lewis female rats resulted in reduced LV diastolic compliance and increased relative wall thickness, cardiomyocyte size, and midmyocardial interstitial and perivascular fibrosis, which were attenuated by treatment with G-1 (62). This model is also unique in that estrogen depletion by OVX markedly exacerbates the development and maintenance of hypertension that appears to be dependent on an activated RAAS (14–16, 150). Thus, the female mRen2.Lewis rat has helped us understand the mechanisms that drive diastolic dysfunction in postmenopausal women and has provided us with a potential animal model for evaluating preventive and therapeutic interventions for diastolic dysfunction.
Although estrogen loss is initiated at a set age in the OVX mRen2.Lewis rat (∼5 wk) that is far earlier than the age at which menopause begins in middle-aged women, mRen2.Lewis female congenics consistently exhibit accelerated increases in systolic blood pressure and LV hypertrophy after the depletion of ovarian hormones by bilateral OVX, characteristics that commonly occur in women after the transition to menopause. It remains unclear to what extent changes in diastolic function and the consequent risk of diastolic HF after menopause are consequences of hormonal changes versus advancing age. The mRen2.Lewis model allows us to examine the role of ovarian estrogens, independent of age-related cardiovascular changes, in the pathogenesis of diastolic heart disease. It is important to note that the mRen2.Lewis female rat is a renin-overexpressing animal model, which might not accurately emulate RAAS-related changes in women after menopause, as the Ren2 gene is expressed in cardiac myocytes.
Other models.
LVDD is related to reduced ventricular relaxation (primarily affecting early diastole) and increased myocardial and chamber stiffness (primarily affecting late diastole) (8, 70, 140, 167). Various rodent models have been developed to mimic the abnormalities in ventricular relaxation and/or LV compliance that occur after estrogen loss; these models may be useful for the study of female sex-specific diastolic dysfunction.
Rat pressure overload (PO) models are commonly used to understand the mechanisms that underlie the progression of diastolic dysfunction to HF (104). To this end, one of the earliest studies that shed light on the potential cardioprotective effects of estrogen in hypertensive heart disease was reported by Douglas et al. (28) using Wistar rats subjected to chronic PO induced by transverse aortic constriction (TAC). These investigators showed that at 6 wk after aortic banding in weanling rats, LV remodeling, ventricular function, and the extent of hypertrophy appeared similar in male and female rats. However, at 20 wk after TAC, only male rats showed an early transition to HF, with an onset of cavity dilatation, loss of concentric remodeling, elevated wall stress, and diastolic dysfunction. Correspondingly, in female rats subjected to 4 wk of suprarenal aortic constriction, estrogen loss by OVX increased myocardial fibrosis, elevated LV end-diastolic pressure, and decreased the transmitral Doppler early-to-late filling velocity ratio compared with ovary-intact rats subjected to the same afterload insult (98).
In addition to estrogen's role in the regulation of extracellular remodeling and presumably LV compliance, its beneficial effects on limiting diastolic dysfunction in the PO rat might also involve cardiac Ca2+ regulation. Weinberg et al. (153) showed that cardiac sarco(endo)plasmic reticulum Ca2+-ATPase (SERCA)2a gene expression was unchanged in hearts from estrogen-intact female Wistar rats subjected to TAC but was reduced in hearts from their male counterparts subjected to the same PO perturbation, revealing another possible explanation for the male sex-specific reduction in the functional reserve after TAC (153). For relaxation to occur, intracellular Ca2+ must decline, thereby causing the dissociation of Ca2+ from troponin C. The four mechanisms of Ca2+ removal from the cytosol include activation of SERCA, sarcolemmal Na+/Ca2+ exchanger, sarcolemmal Ca2+ ATPase, and mitochondrial Ca2+ uniport. A defect in any of these proteins could result in the impairment of myocardial relaxation. Alterations in phospholamban, a protein that regulates SERCA2 and the sarcolemmal Na+/Ca2+ exchanger, has also been implicated in diastolic dysfunction (70, 76). In addition, Ca2+ leak from the sarcoplasmic reticulum via ryanodine receptors may contribute to diastolic dysfunction (120). Taken together, estrogen's protective effects in the PO heart that might limit the progression of diastolic dysfunction include effects on interstitial remodeling and possibly intracellular Ca2+ through its regulation of SERCA2a and the Na+/Ca2+ exchanger (75).
In addition to surgically induced PO models, spontaneously hypertensive rats (SHRs) are commonly used to study LV remodeling and cardiac dysfunction secondary to essential hypertension (96). SHRs with OVX have been used to understand the relationship between estrogen and the development of cardiac fibrosis (90). Although diastolic function per se has not been evaluated in this model, estrogen loss accelerates cardiac fibrosis, a key contributor to myocardial and chamber stiffness (9, 151).
The inbred Brown Norway rat and the hybrid Brown Norway × Fischer 344 rat are considered to be ideal models for the study of normal cardiac aging because their cardiovascular phenotype is not confounded by concomitant obesity and renal dysfunction (84). Although there are no reports using these rats to study diastolic dysfunction as it relates to aging women, Knowlton and colleagues found that at 9 wk after OVX (performed at 18–22 mo) of female Brown Norway rats, extracellular matrix-related gene expression was significantly increased in the heart; this effect could be attenuated by 17β-estradiol treatment (105, 136). While functional and structural phenotypic changes with respect to estrogen status were not reported, their findings suggest that the aged OVX Brown Norway female rat might be a suitable model to study diastolic dysfunction. In fact, in a preliminary study of middle-aged Brown Norway × Fischer 344 female rats (18 mo of age), we observed subtle but significant increases in systolic blood pressure and reductions in tissue Doppler-derived measures of diastolic function 8 wk after OVX compared with age-matched, sham-operated female rats (unpublished observations). Additional work is underway to determine the potential of this normative aging model in the study of diastolic dysfunction as it relates to the postmenopausal woman.
To begin to understand the roles of estrogen in the pathogenesis of obesity- and/or insulin resistance-induced LVDD, two reverse translational animal models may be considered. Manrique et al. (89) recently showed that young female mice fed a Western diet high in fat and fructose corn syrup abrogated the protective effects of estrogen on whole body insulin sensitivity. Eight weeks of the Western diet also preferentially promoted the development of diastolic dysfunction in female mice as opposed to male mice, and this cardiac phenotype was associated with increased myocardial oxidative stress, increased collagen type 1 expression (a marker of stiffness), altered Ca2+ handling, and a pronounced decrease in Akt/endothelial NOS (eNOS) activation. Similarly, Murase et al. (99) showed that estrogen replacement exacerbated LVDD and cardiac fibrosis and further increased oxidative stress and inflammation in a new rat model of metabolic syndrome (OVX -Dahl salt-sensitive/obese rats). In contrast to the aforementioned models of hypertension- or PO-induced LVDD, these metabolic-related models of LVDD suggest that the cardioprotective effects of estrogen may be lost under conditions of diet-induced insulin resistance, obesity, and diabetes. The structural and functional cardiac implications of insulin resistance and the diabetic state, in the context of estrogen, have been extensively reviewed by Reichelt et al. (115).
Mechanisms of Estrogen's Protective Effects on Diastolic Function
Despite representing a disease continuum of great clinical importance and urgency, diastolic dysfunction in postmenopausal women is not well understood, and the mechanisms involved are not yet clear. Here, we review recent work from our group and others that has revealed potential mechanisms by which loss of estrogen induces diastolic dysfunction.
Estrogen, NOS, and diastolic dysfunction.
The molecular mechanisms associated with estrogenic modulation of hypertensive heart disease, and specifically LVDD, are complex, but reduced NO availability and altered NOS system component expression and activity have been implicated as potential contributors. Briefly, NO activity is the net result of a balance between its production by NOS and its inactivation by ROS (i.e., free radicals), such as superoxide (119). Under various pathological states, both NO and superoxide are increased by NOS with a net balance being a decrease in NO activity. This concept of “uncoupling” of NOS has been implicated as a major factor responsible for endothelial dysfunction, diastolic dysfunction, and LV remodeling (97, 131, 138, 141).
While all three NOS isoforms (eNOS, inducible NOS, and nNOS) have been identified in the heart, only nNOS and eNOS are considered to be constitutive isoforms whose activity in the formation of NO is dependent on Ca2+/calmodulin and other cofactors, including tetrahydrobiopterin (BH4), flavin mononucleotide, flavin adenine dinucleotide, and reduced nicotine adenine dinucleotide phosphate. Because BH4 is influenced by the estrogenic milieu (126), it may be involved in the cardiac phenotype of women after menopause. BH4 appears to act as an allosteric modulator of the NOS complex, contributing to the dimerization of NOS monomers (156, 157), which is necessary for the generation of NO (144, 147). Under conditions of suboptimal BH4 concentration or the oxidation of BH4 to dihydrobiopterin, both of which coincide with estrogen deficiency, the NOS complex is thought to uncouple, resulting in the preferential production of ROS rather than NO. GTP cyclohydrolase has been implicated in BH4 biosynthesis, and it is regulated by estrogen (95, 126, 128). Animal studies have shown decreased BH4 bioavailability in the aorta of female rats after OVX (78) and that 17β-estradiol therapy normalizes BH4 levels and suppresses ROS generation in aortic tissue. Moreover, in cultured endothelial cells, estrogens increase BH4 levels through upregulation of GTP cyclohydrolase mRNA and activity (95). Yamaleyeva et al. (159, 161) showed that the adverse effects of estrogen loss on kidney structure and function in the salt-sensitive, hypertensive mRen2.Lewis female rat, including increased renal nNOS expression, could be reversed by a specific nNOS inhibitor. Taken together, it seems plausible that estrogens may be involved in the maintenance of a “favorable” cardiac NOS complex and likely the preferential production of NO over superoxide.
To test this possibility, we studied the roles of NOS and BH4 in the maintenance of cardiac structure and diastolic function in the OVX mRen2.Lewis female rat (Table 2). Estrogen deprivation resulted in a relative deficiency in cardiac BH4, which was associated with an increase in cardiac superoxide production, a reduction in cardiac NO release (nitrate), and adverse LV remodeling and diastolic dysfunction. Importantly, chronic exogenous BH4 supplementation for 4 wk after the onset of hypertension (64, 149) reversed the unfavorable effects of estrogen loss on diastolic function, superoxide production, and cardiac collagen deposition (64). Moreover, chronic treatment with the specific nNOS inhibitor L-VNIO limited the adverse effects of a presumed uncoupled or maladaptive NOS on cardiac structure and diastolic function (63).
Table 2.
Summary of key cardiovascular end points in mRen2.Lewis rats after OVX and OVX + 4 wk of nNOS inhibition or BH4 supplementation
| Estrogen Loss (OVX) | Estrogen Loss and nNOS Inhibition | Estrogen Loss and BH4 Treatment | |
|---|---|---|---|
| Hypertension | ↑↑↑ | ↑↑ | ↑↑↑ |
| BH4:BH2 | ↓ | ↓ | ↑ biopterins |
| Cardiac ROS | ↑ | ↓ | ↓ |
| Cardiac NO | ↓ | ↓ | ↑ |
| Fibrosis | ↑ | ↓ | ↓ |
| Diastolic function | Moderately reduced | Preserved | Preserved |
While we can only speculate on the contribution of decreased NO and/or increased ROS toward OVX-elicited cardiac remodeling and diastolic derangement, we do know from data in the mRen2.Lewis parent strain, the (mRen2)27 rat, that blockade of mineralocorticoid receptors diminishes oxidative stress, which, in turn, attenuates collagen deposition in the heart associated with diastolic dysfunction in male rats (47). Similarly, cardiac oxidative stress due to ANG II stimulation from the activation of the RAAS in the (mRen2)27 rat induces structural and functional changes within the heart (47, 154). We do not yet know if these observations hold true in the mRen2.Lewis rat. Aside from the potential consequences of an activated RAAS, which is known to at least uncouple eNOS within the vasculature (123), it is possible that in our studies the diminished NO availability provoked further collagen deposition. NO has been shown to regulate matrix metalloproteinases (MMPs) in the heart (54, 86), which are responsible for the intricate balance of collagen turnover. NO appears to modulate this activity through activation of ERK and Akt pathways (7, 12, 26, 32). In contrast to the direct actions of NO, ROS has been implicated in collagen synthesis by mediating MMP induction or stimulation, decreasing tissue inhibitors of metalloproteinase levels, and stimulating collagen synthesis (147). Certainly, MMPs are increased in age-related diastolic dysfunction (20, 59). Since decreased NO and increased oxidative stress augment MMP release (23, 50, 143), these findings point to an additional mechanism that may account for the development of cardiac fibrosis in the OVX mRen2.Lewis model.
Estrogen and the RAAS in diastolic dysfunction.
Activation of the RAAS is associated with hypertension, cardiac hypertrophy, impaired cardiomyocyte relaxation, and cardiac fibrosis, which contribute to the impairment of diastolic function. Evidence suggests that the RAAS is involved in the sex-related differences and cardiac dissimilarities that occur during the pre- to postmenopausal transition. ACE activity is higher in men than in women among healthy young adults (164), whereas in postmenopausal women, plasma ACE activity is similar to that in men of the same age (25, 94, 125). Estrogen replacement has been shown to reduce ACE activity in postmenopausal women (111, 125). In hypertensive rats, ACE activity is higher in male rats than in female rats (107), and estrogen treatment decreases ACE activity in the plasma, kidney, and aorta of OVX female rats (10, 14). Mounting evidence indicates that estrogen also regulates other components of the RAAS, such as angiotensinogen, renin, tissue ANG II type 1 and 2 receptors (AT1Rs and AT2R, respectively), and aldosterone production (6, 57, 101, 116, 139). In the heart, activation of the ANG II-AT1R axis can affect diastolic function by altering the relaxation properties of cardiomyocytes (19) and by changing the composition of the extracellular matrix, specifically collagen content and type, which, in turn, reduces LV distensibility (166, 167).
In mRen2.Lewis female rats, the local and circulating RAAS are also regulated by estrogen, which has subsequent effects on blood pressure and diastolic function. OVX mRen2.Lewis rats treated with the AT1R blocker olmesartan exhibit a reduction in blood pressure similar to that seen with 17β-estradiol replacement (14). Estrogen replacement in the mRen2.Lewis rat also corrects the increase in circulating activities of renin and ACE as well as reduces plasma levels of ANG II and increased circulating ANG-(1–7) (14). Moreover, 17β-estradiol treatment attenuates OVX-associated increases in cardiac ANG II and diastolic dysfunction (150). The regulation of cardiac ANG II might be due to the inhibition of chymase expression by estrogen (Table 3). Chymase is an alternative pathway that generates ANG II in the heart. In the mRen2.Lewis rat, neither OVX nor OVX + 17β-estradiol altered cardiac expression or activity of ACE. Interestingly, in women with HF, pharmacological approaches aimed at the inhibition of ACE have met with minimal success (37, 38, 130, 155). Further studies are needed to determine whether the development of diastolic dysfunction after ovarian hormone loss involves the noncanonical pathway by which chymase (produced within cardiomyocytes or brought into these cells from activated mast cells) (79, 150) generates ANG II.
Table 3.
Chymase/ANG II/aldosterone and diastolic function in mRen2.Lewis rats after OVX and OVX + 4 wk of estrogen treatment
| Plasma ANG II, pg/ml | Cardiac ANG II Staining Intensity | Cardiac Chymase Protein/GAPDH | Plasma Aldosterone, pg/ml | e′, cm/s | E/e′ | |
|---|---|---|---|---|---|---|
| Sham-operated rats | 17.4 ± 2.1 | 129 ± 16 | 0.53 ± 0.09 | 23.4 ± 5.8 | 3.38 ± 0.16 | 19.2 ± 0.8 |
| OVX rats | ||||||
| Vehicle treatment | 31.2 ± 10.2 | 173 ± 9* | 1.14 ± 0.17* | 36.6 ± 7.5 | 2.87 ± 0.18 | 23.0 ± 1.1* |
| 17β-Estradiol treatment | 8.8 ± 1.4 | 141 ± 12 | 0.59 ± 0.13 | 12.1 ± 0.8† | 3.76 ± 0.19† | 17.0 ± 0.9† |
n = 7–10 rats/group.
P < 0.05 vs. sham-operated rats;
P < 0.05 vs. vehicle-treated OVX rats.
Several lines of evidence suggest that aldosterone excess might play a key role in diastolic dysfunction associated with ovarian estrogen deprivation. Aldosterone is mainly synthesized and released from the adrenal gland (158), and estrogen may regulate aldosterone synthesis and secretion via downregulation of AT1Rs in the adrenal gland (158). In OVX mRen2.Lewis rats, plasma aldosterone tended to be higher compared with sham-operated rats; aldosterone decreased significantly after estrogen treatment of OVX rats compared with vehicle-treated OVX rats (Table 3). Adverse effects of aldosterone on cardiac remodeling and diastolic dysfunction have been reported in both animal models and clinical studies (29, 47, 129). Compared with age-matched Sprague-Dawley rats, male (mRen2)27 rats at 8–9 wk of age display higher systolic blood pressure, plasma aldosterone levels, cardiac hypertrophy and fibrosis, and cardiac oxidative stress as well as impaired LV diastolic relaxation without changes in systolic function. Treatment with the specific aldosterone antagonist spironolactone for 3 wk improved diastolic dysfunction and reduced cardiac fibrosis and oxidative stress independent of changes in systolic blood pressure (47). These findings are consistent with data from recent randomized, controlled clinical trials of long-term aldosterone receptor blockade, which showed improved LV diastolic function in both male and female patients with diastolic HF who received spironolactone (29). These data suggest that aldosterone might play a role in postmenopausal diastolic dysfunction and that aldosterone antagonism may be a plausible treatment option. In contrast, recent data from the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist trial showed that HFPEF patients randomized to spironolactone treatment did not outperform placebo-treated patients on the primary composite outcome of cardiovascular death, heart failure hospitalization, or aborted cardiac arrest. Even so, spironolactone-treated patients had significantly fewer hospitalizations for HF than control patients, supporting its therapeutic potential in reducing the burden of disease (137).
Estrogen and natriuretic peptides in diastolic dysfunction.
The cardiac natriuretic peptides (NPs), including atrial NP, brain NP, and their related peptides, may also have an important role in the pathogenesis of LVDD after the menopausal transition. A positive relationship between female sex steroids and the production/secretion of NPs has been demonstrated in experimental (22, 58) and clinical (69, 77) studies. In addition to possessing diuretic, natriuretic, and vasodilatory properties, NPs have emerged as potent antifibrotic and antihypertrophic humoral factors in the heart, either by directly inhibiting the sympathetic RAAS or through the release or action of endothelin (22, 148). Findings from the Prospective Comparison of Angiotensin Receptor Neprilysin Inhibitor and Angiotensin Receptor Blocker on Management of Heart Failure with Preserved Ejection Fraction trial further underscore the therapeutic potential of augmenting the NP system via inhibition of neprilysin (the key enzyme responsible for NP breakdown) in combination with an angiotensin receptor blocker in the management of diastolic HF or HFPEF (133, 148). Therefore, it is plausible that a relative deficiency of NPs in the female heart after the loss of ovarian estrogens contributes to the cardiac fibrotic processes that underlie the postmenopausal diastolic dysfunction phenotype.
A Novel ER, GPR30, and Diastolic Function
Although preclinical studies have reported the presence of ERα and ERβ in cardiomyocytes and cardiofibroblasts (44), the role of estrogen in the maintenance of diastolic function remains poorly understood. An orphan GPER (GPR30) was discovered in triple-negative breast cancer cells that binds estrogen at high affinity and improves cardiac function and structure in an ER-independent manner; this discovery has revealed new insights into the cardioprotective effects of estrogen, beyond the genomic and nongenomic mechanisms of classic ERs (8, 13, 26, 32–34, 68, 152). GPR30-associated actions in the heart were first described in a myocardial ischemia-reperfusion injury animal model (26). RT-PCR and immunoblot analysis further confirmed the expression of GPR30 in both porcine and human coronary artery vascular smooth muscle cells (VSMCs). GPR30 activation by the selective agonist G-1 relaxes porcine aortic rings, rat mesenteric resistance vessels, and human coronary arteries in an endothelium-independent manner (81, 163). Moreover, a GPR30 activation-induced vasodilatory response was found to be abrogated in carotid arteries in GPR30 knockout mice compared with control mice as well as in the intact mRen2.Lewis rat maintained on a high-salt diet (45, 81). In the mesenteric vessels, both endothelial denudation and the NOS inhibitor N-nitro-l-arginine methyl ester achieve a similar extent of inhibition of estradiol- and G-1-induced vasorelaxation; however, there remains an endothelium-independent component that uses cAMP as a signaling molecule (83). Interestingly, the nonendothelial vasorelaxation response is reduced in the mesentery of older female Lewis rats and associated with reduced expression of GPR30 (82). In this regard, Yu et al. (163) demonstrated that GPR30 specifically activates the large-conductance Ca2+- and voltage-activated K+ channel in coronary artery VSMCs.
Consistent with in vitro and ex vivo findings, in vivo studies have demonstrated that GPR30 activation by G-1 reduces infarct size in the isolated perfused male mouse heart (7). The cardioprotective effects of GPR30 might be mediated by the ERK pathway, as the effects of G-1 are abolished by the ERK kinase inhibitor PD-98059. GPR30 has also been shown to be involved in systemic blood pressure regulation. Chronic G-1 treatment decreases blood pressure in OVX hypertensive mRen2.Lewis rats in a dose-dependent manner but does not influence blood pressure in intact female or male congenic rats (Table 4) (80, 81, 149). In intact female rats, we assume that endogenous estrogens are producing a maximal effect on blood pressure that cannot be enhanced by the additional agonist. The lack of an effect in male hypertensive mRen2.Lewis rats may result from a blunted vasodilatory response to G-1 in resistance arteries from these animals and decreased expression of vascular GPR30 (82). These results indicate that GPR30 activation by G-1 at doses of >100 μg·kg−1·day−1 exerts a tonic vasodilatory influence to lower blood pressure.
Table 4.
Dose-dependent systolic blood pressure effects of G-1 in OVX mRen2.Lewis rats
| Sham-Operated Rats |
OVX Rats |
||||||
|---|---|---|---|---|---|---|---|
| Vehicle | 400 μg·kg−1·day−1 G-1 | Vehicle | 50 μg·kg−1·day−1 G-1 | 100 μg·kg−1·day−1 G-1 | 400 μg·kg−1·day−1 G-1 | 800 μg·kg−1·day−1 G-1 | |
| No. of rats | 4 | 5 | 6 | 4 | 5 | 4 | 4 |
| Day 0 | 147 ± 3 | 140 ± 4 | 173 ± 6 | 169 ± 7 | 170 ± 7 | 182 ± 4 | 174 ± 2 |
| Day 14 | 134 ± 6 | 144 ± 4 | 167 ± 7* | 163 ± 4* | 161 ± 6* | 150 ± 7† | 148 ± 6† |
Values are in mmHg.
P < 0.05 vs. sham-vehicle-treated rats;
P < 0.05 vs. day 0
The activation of GPR30 with G-1 has also been found to preserve diastolic function and structure in OVX mRen2.Lewis female rats relative to vehicle-treated OVX littermates (149). Low doses of G-1 (50–100 μg·kg−1·day−1) limit the OVX-related increase in L V filling pressure, LV mass, wall thickness, cardiomyocyte size, and cardiac fibrosis. The mechanisms involved were further determined in in vitro studies focusing on the effects of GPR30 on cardiomyocyte hypertrophy and cardiac fibroblast proliferation. We found that G-1 treatment attenuates ANG II-induced hypertrophy in H9c2 cardiomyocytes and that the GPR30 antagonist G-15 inhibits the effects of both 17β-estradiol and G-1. Moreover, G-1 also inhibits the proliferation of cardiac fibroblasts derived from adult Sprague-Dawley rats. These studies revealed the importance of GPR30 in the maintenance of female sex-specific cardiac structure and function, which likely involve effects on both cardiomyocytes and cardiac fibroblasts. The RAAS also appears to modulate the protective effects of G-1 on diastolic function. Our preliminary data showed a significant increase in plasma ANG I and a trend toward increased plasma ANG II and, curiously, ANG-(1–12) in OVX mRen2.Lewis rats compared with sham control rats; G-1 treatment reversed these changes, suggesting that the regulation of RAAS by GPR30 may be involved in preserving diastolic function (Table 5).
Table 5.
Plasma angiotensins and diastolic function in OVX mRen2.Lewis rats treated with vehicle or G-1 for 2 wk
| Plasma ANG I, pg/ml | Plasma ANG II, pg/ml | Plasma ANG-(1–12), pg/ml | e′, cm/s | E/e′ | |
|---|---|---|---|---|---|
| Sham-operated rats | 66 ± 7 | 17 ± 3 | 143 ± 29 | 3.4 ± 0.2 | 19.0 ± 1.1 |
| OVX rats | |||||
| Vehicle treatment | 94 ± 8* | 25 ± 2 | 270 ± 59 | 2.6 ± 0.1* | 23.5 ± 1.1* |
| G-1 treatment | 53 ± 4† | 16 ± 3 | 145 ± 38 | 3.6 ± 0.2† | 15.6 ± 1.8† |
n = 7–10 rats/group.
P < 0.05 vs. sham-operated rats;
P < 0.05 vs. vehicle-treated OVX rats.
In high-salt diet-induced diastolic dysfunction in female mRen2.Lewis rats, activation of GPR30 by G-1 also increases LV lusitropy (e′) and improves the e′-to-a′ ratio, as determined by tissue Doppler, and is associated with attenuation of wall thickness, myocyte hypertrophy, and cardiac fibrosis (62). Studies using different animal models have concluded that the activation of GPR30 preserves diastolic function and heart structure. Further studies are needed to determine if the protective effects of GPR30 are mediated through similar mechanisms as estrogen, e.g., by regulating the cardiac RAAS and NOS system.
Clinical Perspective of HRT
Several large, randomized, controlled clinical trials of postmenopausal HRT have been undertaken since the 1990s and have examined a number of end points, including cardiovascular health. The Women's Health Initiative conducted the first randomized, placebo-controlled primary prevention trial of estrogen plus progestin in 16,608 postmenopausal women who were followed for an average of 5.2 yr to assess the incidence of CHD as well as the overall risks and benefits (40, 118). Women in the HRT arm received no cardiovascular benefit from treatment in terms of a reduced incidence of CHD, stroke, and pulmonary embolism. Another randomized control clinical trial, the Heart and Estrogen/Progestin Replacement Study, enrolled women who were generally older than 65 yr and had definitive evidence of CHD; this study also found that there was no significant decrease in the rates of primary CHD events or secondary cardiovascular events among women in the HRT group compared with the placebo group (40). However, further analysis of these carefully conducted trials showed that there was, on average, a 10-yr delay between the onset of menopause and the initiation of estrogen therapy. Interestingly, a more recent study showed a lower rate of CHD events and total mortality when HRT was initiated in younger women (<60 yr) in close proximity to the onset of menopause (<10 yr) and no effect or a possible adverse effect on these end points when HRT was initiated in older women (>60 yr) more than 20 yr after the onset of menopause (54). It was hypothesized that the vessels and myocardium of older postmenopausal women undergo significant age-related remodeling and development of pathology, including systolic hypertension, so that the “late” initiation of estrogen replacement (10 yr or more after the loss of ovarian hormone production) may not reverse cardiovascular damage or prevent further disease progression (74). The apparent timing-related benefit of HRT on CHD has been reported in a large meta-analysis of 23 randomized controlled clinical trials enrolling ∼39,000 women, which revealed a 32% reduction in CHD incidence in women starting HRT before 60 yr of age or <10 yr after menopause (121). This risk reduction was lost in women older than 60 yr of age or >10 yr after menopause (121). These results, along with animal studies in nonhuman primates, support the timing hypothesis, which posits that women respond differentially with respect to CHD based on the timing of HRT initiation relative to age and/or time since menopause (21).
Further underscoring the plasticity of the ovarian hormonal response in cardiovascular tissue with respect to age and possibly salt status, we showed that late OVX (15 wk of age) of mRen2.Lewis rats conveyed renal protective effects from a high-salt diet compared with age-matched, ovary-intact hypertensive littermates (160). The magnitude of the CHD reduction for women <60 yr of age or <10 yr since menopause when randomized to HRT was similar to that seen in observational studies of women who initiated HRT at the time of menopause (54, 55). The Kronos Early Estrogen Prevention Study was recently completed and found several favorable effects of HRT in newly menopausal women, including improved vasomotor symptoms, bone mineral density, and mood outcomes (88). Although none of these large trials examined the influence of HRT per se on diastolic function, its involvement is nearly certain; LVDD is associated with ischemia, and it precedes both diastolic and systolic HF. Clearly, further clinical and basic studies are needed to determine the basis for these clinical trial findings and the relationship among estrogen, preclinical LVDD, and overt heart disease, including the direct effects of estrogen on cardiomyocytes and fibrosis and the molecular mechanisms involved.
Summary
Basic research is essential for understanding the cellular and molecular mechanisms underlying diastolic dysfunction. Estrogen appears to be an important factor that protects against cardiac remodeling and diastolic dysfunction in women. The protective effects of estrogen involve the regulation of the cardiac RAAS and NOS system as well as the newly characterized estrogen receptor GPR30. The exact roles of estrogen and GPR30 on cardiomyocyte relaxation, cardiac fibroblasts, and collagen production as well as the related mechanisms leading to postmenopausal LVDD are the focus of current research.
GRANTS
This work was funded in whole or part by National Institutes of Health Grants AG-042758 (to L. Groban), AG-033727 (to L. Groban), HL-56793 (to M. C. Chappell), and HL-103974 (to S. H. Lindsey), Doctoral Research Grant of Shandong Province BS2010YY005, and National Natural Science Foundation of China Grant 81270175 (to Z. Zhao).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
AUTHOR CONTRIBUTIONS
Author contributions: Z.Z., H.W., M.C.C., and L.G. drafted manuscript; Z.Z., H.W., J.A.J., S.H.L., M.C.C., and L.G. approved final version of manuscript; H.W., J.A.J., S.H.L., M.C.C., and L.G. conception and design of research; H.W., J.A.J., S.H.L., and L.G. performed experiments; H.W., J.A.J., S.H.L., and L.G. analyzed data; H.W. and L.G. interpreted results of experiments; H.W. and S.H.L. prepared figures; H.W., S.H.L., M.C.C., and L.G. edited and revised manuscript.
REFERENCES
- 1.Ahmed A. Association of diastolic dysfunction and outcomes in ambulatory older adults with chronic heart failure. J Gerontol A Biol Sci Med Sci 60: 1339–1344, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aijaz B, Ammar KA, Lopez-Jimenez F, Redfield MM, Jacobsen SJ, Rodeheffer RJ. Abnormal cardiac structure and function in the metabolic syndrome: a population-based study. Mayo Clin Proc 83: 1350–1357, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ashraf MS, Vongpatanasin W. Estrogen and hypertension. Curr Hypertens Rep 8: 368–376, 2006 [DOI] [PubMed] [Google Scholar]
- 4.Aurigemma GP, Gottdiener JS, Shemanski L, Gardin J, Kitzman D. Predictive value of systolic and diastolic function for incident congestive heart failure in the elderly: the cardiovascular health study. J Am Coll Cardiol 37: 1042–1048, 2001 [DOI] [PubMed] [Google Scholar]
- 5.Aurigemma GP, Gaasch WH. Clinical practice. Diastolic heart failure. N Engl J Med 351: 1097–1105, 2004 [DOI] [PubMed] [Google Scholar]
- 6.Baiardi G, Macova M, Armando I, Ando H, Tyurmin D, Saavedra JM. Estrogen upregulates renal angiotensin II AT1 and AT2 receptors in the rat. Regul Pept 124: 7–17, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Bopassa JC, Eghbali M, Toro L, Stefani E. A novel estrogen receptor GPER inhibits mitochondria permeability transition pore opening and protects the heart against ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol 298: H16–H23, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borbély A, van der Velden J, Papp Z, Bronzwaer JG, Edes I, Stienen GJ, Paulus WJ. Cardiomyocyte stiffness in diastolic heart failure. Circulation 111: 774–781, 2005 [DOI] [PubMed] [Google Scholar]
- 9.Brilla CG, Janicki JS, Weber KT. Impaired diastolic function and coronary reserve in genetic hypertension. Role of interstitial fibrosis and medial thickening of intramyocardial coronary arteries. Circ Res 69: 107–115, 1991 [DOI] [PubMed] [Google Scholar]
- 10.Brosnihan KB, Li P, Ganten D, Ferrario CM. Estrogen protects transgenic hypertensive rats by shifting the vasoconstrictor-vasodilator balance of RAS. Am J Physiol Regul Integr Comp Physiol 273: R1908–R1915, 1997 [DOI] [PubMed] [Google Scholar]
- 11.Bybee KA, Stevens TL. Matters of the heart: cardiovascular disease in U.S. women. Mo Med 110: 65–70, 2013 [PMC free article] [PubMed] [Google Scholar]
- 12.Camper-Kirby D, Welch S, Walker A, Shiraishi I, Setchell KD, Schaefer E, Kajstura J, Anversa P, Sussman MA. Myocardial Akt activation and gender: increased nuclear activity in females versus males. Circ Res 88: 1020–1027, 2001 [DOI] [PubMed] [Google Scholar]
- 13.Carmeci C, Thompson DA, Ring HZ, Francke U, Weigel RJ. Identification of a gene (GPR30) with homology to the G-protein-coupled receptor superfamily associated with estrogen receptor expression in breast cancer. Genomics 45: 607–617, 1997 [DOI] [PubMed] [Google Scholar]
- 14.Chappell MC, Gallagher PE, Averill DB, Ferrario CM, Brosnihan KB. Estrogen or the AT1 antagonist olmesartan reverses the development of profound hypertension in the congenic mRen2.Lewis rat. Hypertension 42: 781–786, 2003 [DOI] [PubMed] [Google Scholar]
- 15.Chappell MC, Modrall JG, Diz DI, Ferrario CM. Novel aspects of the renal renin-angiotensin system: angiotensin-(1–7), ACE2 and blood pressure regulation. Contrib Nephrol 143: 77–89, 2004 [DOI] [PubMed] [Google Scholar]
- 16.Chappell MC. Emerging evidence for a functional angiotensin-converting enzyme 2-angiotensin-(1–7)-MAS receptor axis: more than regulation of blood pressure? Hypertension 50: 596–599, 2007 [DOI] [PubMed] [Google Scholar]
- 17.Chappell MC, Westwood BM, Yamaleyeva LM. Differential effects of sex steroids in young and aged female mRen2.Lewis rats: a model of estrogen and salt-sensitive hypertension. Gend Med 5, Suppl A: S65–S75, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen CH, Nakayama M, Nevo E, Fetics BJ, Maughan WL, Kass DA. Coupled systolic-ventricular and vascular stiffening with age: implications for pressure regulation and cardiac reserve in the elderly. J Am Coll Cardiol 32: 1221–1227, 1998 [DOI] [PubMed] [Google Scholar]
- 19.Cheng CP, Suzuki M, Ohte N, Ohno M, Wang ZM, Little WC. Altered ventricular and myocyte response to angiotensin II in pacing-induced heart failure. Circ Res 78: 880–892, 1996 [DOI] [PubMed] [Google Scholar]
- 20.Chiao YA, Ramirez TA, Zamilpa R, Okoronkwo SM, Dai Q, Zhang J, Jin YF, Lindsey ML. Matrix metalloproteinase-9 deletion attenuates myocardial fibrosis and diastolic dysfunction in ageing mice. Cardiovasc Res 96: 444–455, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clarkson TB, Meléndez GC, Appt SE. Timing hypothesis for postmenopausal hormone therapy: its origin, current status, and future. Menopause 20: 342–353, 2013 [DOI] [PubMed] [Google Scholar]
- 22.Clerico A, Fontana M, Vittorini S, Emdin M. The search for a pathophysiological link between gender, cardiac endocrine function, body mass regulation and cardiac mortality: proposal for a working hypothesis. Clin Chim Acta 405: 1–7, 2009 [DOI] [PubMed] [Google Scholar]
- 23.Consoli C, Gatta L, Iellamo F, Molinari F, Rosano GM, Marlier LN. Severity of left ventricular dysfunction in heart failure patients affects the degree of serum-induced cardiomyocyte apoptosis. Importance of inflammatory response and metabolism. Int J Cardiol 167: 2859–2866, 2013 [DOI] [PubMed] [Google Scholar]
- 24.Correa de Sa DD, Hodge DO, Slusser JP, Redfield MM, Simari RD, Burnett JC, Chen HH. Progression of preclinical diastolic dysfunction to the development of symptoms. Heart 96: 528–532, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Danser AH, Derkx FH, Schalekamp MA, Hense HW, Riegger GA, Schunkert H. Determinants of interindividual variation of renin and prorenin concentrations: evidence for a sexual dimorphism of (pro)renin levels in humans. J Hypertens 16: 853–862, 1998 [DOI] [PubMed] [Google Scholar]
- 26.Deschamps AM, Murphy E. Activation of a novel estrogen receptor, GPER, is cardioprotective in male and female rats. Am J Physiol Heart Circ Physiol 297: H1806–H1813, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Simone G, Devereux RB, Chinali M, Roman MJ, Barac A, Panza JA, Lee ET, Howard BV. Sex differences in obesity-related changes in left ventricular morphology: the Strong Heart Study. J Hypertens 29: 1431–1438, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Douglas PS, Katz SE, Weinberg EO, Chen MH, Bishop SP, Lorell BH. Hypertrophic remodeling: gender differences in the early response to left ventricular pressure overload. J Am Coll Cardiol 32: 1118–1125, 1998 [DOI] [PubMed] [Google Scholar]
- 29.Edelmann F, Wachter R, Pieske B. Aldosterone inhibition in patients with heart failure with preserved ejection fraction–reply. JAMA 310: 205–207, 2013 [DOI] [PubMed] [Google Scholar]
- 30.Fang J, Mensah GA, Croft JB, Keenan NL. Heart failure-related hospitalization in the U.S., 1979 to 2004. J Am Coll Cardiol 52: 428–434, 2008 [DOI] [PubMed] [Google Scholar]
- 31.Feldman DE, Ducharme A, Giannetti N, Frenette M, Michel C, Grondin F, Sheppard R, Lauriers JD, Behlouli H, Pilote L. Severity at entry to specialized heart failure clinics: discrepancies between health-related quality of life and function in men and women. Can J Cardiol 27: 382–387, 2011 [DOI] [PubMed] [Google Scholar]
- 32.Filice E, Recchia AG, Pellegrino D, Angelone T, Maggiolini M, Cerra MC. A new membrane G protein-coupled receptor (GPR30) is involved in the cardiac effects of 17β-estradiol in the male rat. J Physiol Pharmacol 60: 3–10, 2009 [PubMed] [Google Scholar]
- 33.Filardo EJ, Quinn JA, Bland KI, Frackelton AR., Jr Estrogen-induced activation of Erk-1 and Erk-2 requires the G protein-coupled receptor homolog, GPR30, and occurs via trans-activation of the epidermal growth factor receptor through release of HB-EGF. Mol Endocrinol 14: 1649–1660, 2000 [DOI] [PubMed] [Google Scholar]
- 34.Filardo EJ, Quinn JA, Frackelton AR, Bland KI. Estrogen activation via the G protein-coupled receptor, GPR30: stimulation of adenylyl cyclase and cAMP-mediated attenuation of the epidermal growth factor receptor-to-MAPK signaling axis. Mol Endocrinol 16: 70–84, 2002 [DOI] [PubMed] [Google Scholar]
- 35.Friedman MM. Gender differences in the health related quality of life of older adults with heart failure. Heart Lung 32: 320–327, 2003 [DOI] [PubMed] [Google Scholar]
- 36.Frye JB, Lukefahr AL, Wright LE, Marion SL, Hoyer PB, Funk JL. Modeling perimenopause in Sprague-Dawley rats by chemical manipulation of the transition to ovarian failure. Comp Med 62: 193–202, 2012 [PMC free article] [PubMed] [Google Scholar]
- 37.Garg R, Yusuf S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group on ACE Inhibitor Trials. JAMA 273: 1450–1456, 1995 [PubMed] [Google Scholar]
- 38.Ghali JK, Lindenfeld J. Sex differences in response to chronic heart failure therapies. Expert Rev Cardiovasc Ther 6: 555–565, 2008 [DOI] [PubMed] [Google Scholar]
- 39.Gottdiener JS, Arnold AM, Aurigemma GP, Polak JF, Tracy RP, Kitzman DW, Gardin JM, Rutledge JE, Boineau RC. Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol 35: 1628–1637, 2000 [DOI] [PubMed] [Google Scholar]
- 40.Grady D, Herrington D, Bittner V, Blumenthal R, Davidson M, Hlatky M, Hsia J, Hulley S, Herd A, Khan S, Newby LK, Waters D, Vittinghoff E, Wenger N; HERS Research Group Cardiovascular disease outcomes during 6.8 years of hormone therapy: Heart and Estrogen/Progestin Replacement Study follow-up (HERS II). JAMA 288: 49–57, 2002 [DOI] [PubMed] [Google Scholar]
- 41.Groban L, Yamaleyeva LM, Westwood BM, Houle TT, Lin M, Kitzman DW, Chappell MC. Progressive diastolic dysfunction in the female mRen(2).Lewis rat: influence of salt and ovarian hormones. J Gerontol A Biol Sci Med Sci 63: 3–11, 2008 [DOI] [PubMed] [Google Scholar]
- 42.Groban L, Wang H, Machado F, Trask AJ, Kritchevsky SB, Ferrario CM, Diz DI. Low glial angiotensinogen improves body habitus, diastolic function, and exercise tolerance in aging male rats. Cardiovasc Endocrinol 1: 49–58, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Groeschel M, Braam B. Connecting chronic and recurrent stress to vascular dysfunction: no relaxed role for the renin-angiotensin system. Am J Physiol Renal Physiol 300: F1–F10, 2011 [DOI] [PubMed] [Google Scholar]
- 44.Grohé C, Kahlert S, Löbbert K, Stimpel M, Karas RH, Vetter H, Neyses L. Cardiac myocytes and fibroblasts contain functional estrogen receptors. FEBS Lett 416: 107–112, 1997 [DOI] [PubMed] [Google Scholar]
- 45.Haas E, Bhattacharya I, Brailoiu E, Damjanović M, Brailoiu GC, Gao X, Mueller-Guerre L, Marjon NA, Gut A, Minotti R, Meyer MR, Amann K, Ammann E, Perez-Dominguez A, Genoni M, Clegg DJ, Dun NJ, Resta TC, Prossnitz ER, Barton M. Regulatory role of G protein-coupled estrogen receptor for vascular function and obesity. Circ Res 104: 288–291, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Haass M, Kitzman DW, Anand IS, Miller A, Zile MR, Massie BM, Carson PE. Body mass index and adverse cardiovascular outcomes in heart failure patients with preserved ejection fraction/clinical perspective. Circ Heart Fail 4: 324–331, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Habibi J, DeMarco VG, Ma L, Pulakat L, Rainey WE, Whaley-Connell AT, Sowers JR. Mineralocorticoid receptor blockade improves diastolic function independent of blood pressure reduction in a transgenic model of RAAS overexpression. Am J Physiol Heart Circ Physiol 300: H1484–H1491, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harman SM, Brinton EA, Cedars M, Lobo R, Manson JE, Merriam GR, Miller VM, Naftolin F, Santoro N. KEEPS: the Kronos Early Estrogen Prevention Study. Climacteric 8: 3–12, 2005 [DOI] [PubMed] [Google Scholar]
- 49.Hayes SN, Taler SJ. Hypertension in women: current understanding of gender differences. Mayo Clin Proc 73: 157–165, 1998 [DOI] [PubMed] [Google Scholar]
- 50.Henderson BC, Tyagi SC. Oxidative mechanism and homeostasis of proteinase/antiproteinase in congestive heart failure. J Mol Cell Cardiol 41: 959–962, 2006 [DOI] [PubMed] [Google Scholar]
- 51.Henderson BC, Tyagi N, Ovechkin A, Kartha GK, Moshal KS, Tyagi SC. Oxidative remodeling in pressure overload induced chronic heart failure. Eur J Heart Fail 9: 450–457, 2007 [DOI] [PubMed] [Google Scholar]
- 52.Heo S, Moser DK, Widener J. Gender differences in the effects of physical and emotional symptoms on health-related quality of life in patients with heart failure. Eur J Cardiovasc Nurs 6: 146–152, 2007 [DOI] [PubMed] [Google Scholar]
- 53.Hodis HN, Mack WJ. A “window of opportunity:” the reduction of coronary heart disease and total mortality with menopausal therapies is age- and time-dependent. Brain Res 1379: 244–252, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hodis HN, Collins P, Mack WJ, Schierbeck LL. The timing hypothesis for coronary heart disease prevention with hormone therapy: past, present and future in perspective. Climacteric 15: 217–228, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hodis HN, Mack WJ. The timing hypothesis and hormone replacement therapy: a paradigm shift in the primary prevention of coronary heart disease in women. Part 1: comparison of therapeutic efficacy. J Am Geriatr Soc 61: 1005–1010, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hogg K, Swedberg K, McMurray J. Heart failure with preserved left ventricular systolic function; epidemiology, clinical characteristics, and prognosis. J Am Coll Cardiol 43: 317–327, 2004 [DOI] [PubMed] [Google Scholar]
- 57.Holycross BJ, Summers BM, Dunn RB, McCune SA. Plasma renin activity in heart failure-prone SHHF/Mcc-facp rats. Am J Physiol Heart Circ Physiol 273: H228–H233, 1997 [DOI] [PubMed] [Google Scholar]
- 58.Hong M, Yan Q, Tao B, Boersma A, Han KK, Vantyghem MC, Racadot A, Lefebvre J. Estradiol, progesterone and testosterone exposures affect the atrial natriuretic peptide gene expression in vivo in rats. Biol Chem Hoppe Seyler 373: 213–218, 1992 [DOI] [PubMed] [Google Scholar]
- 59.Horn MA, Graham HK, Richards MA, Clarke JD, Greensmith DJ, Briston SJ, Hall MC, Dibb KM, Trafford AW. Age-related divergent remodeling of the cardiac extracellular matrix in heart failure: collagen accumulation in the young and loss in the aged. J Mol Cell Cardiol 53: 82–90, 2012 [DOI] [PubMed] [Google Scholar]
- 60.Hulley S, Grady D, Bush T, Furberg C, Herrington D, Riggs B, Vittinghoff E. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/Progestin Replacement Study (HERS) Research Group. JAMA 280: 605–613, 1998 [DOI] [PubMed] [Google Scholar]
- 61.Jessup JA, Gallagher PE, Averill DB, Brosnihan KB, Tallant EA, Chappell MC, Ferrario CM. Effect of angiotensin II blockade on a new congenic model of hypertension derived from transgenic Ren-2 rats. Am J Physiol Heart Circ Physiol 291: H2166–H2172, 2006 [DOI] [PubMed] [Google Scholar]
- 62.Jessup JA, Lindsey SH, Wang H, Chappell MC, Groban L. Attenuation of salt-induced cardiac remodeling and diastolic dysfunction by the GPER agonist G-1 in female mRen2.Lewis rats. PLOS ONE 5: e15433, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jessup JA, Zhang L, Chen AF, Presley TD, Kim-Shapiro DB, Chappell MC, Wang H, Groban L. Neuronal nitric oxide synthase inhibition improves diastolic function and reduces oxidative stress in ovariectomized mRen2.Lewis rats. Menopause 18: 698–708, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jessup JA, Zhang L, Presley TD, Kim-Shapiro DB, Wang H, Chen AF, Groban L. Tetrahydrobiopterin restores diastolic function and attenuates superoxide production in ovariectomized mRen2.Lewis rats. Endocrinology 152: 2428–2436, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jessup JA, Wang H, MacNamara LM, Presley TD, Kim-Shapiro DB, Zhang L, Chen AF, Groban L. Estrogen therapy, independent of timing, improves cardiac structure and function in oophorectomized mRen2.Lewis rats. Menopause 20: 860–868, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jessup M, Brozena S. Heart failure. N Engl J Med 348: 2007–2018, 2003 [DOI] [PubMed] [Google Scholar]
- 67.Jiménez-Navarro MF, Ramirez-Marrero MA, Anguita-Sánchez M, Castillo JC; BADAPIC Investigators Influence of gender on long-term prognosis of patients with chronic heart failure seen in heart failure clinics. Clin Cardiol 33: E13–E18, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kang S, Liu Y, Sun D, Zhou C, Liu A, Xu C, Hao Y, Li D, Yan C, Sun H. Chronic activation of the G protein-coupled receptor 30 with agonist G-1 attenuates heart failure. PLOS ONE 7: e48185, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Karjalainen AH, Ruskoaho H, Vuolteenaho O, Heikkinen JE, Bäckström AC, Savolainen MJ, Kesäniemi YA. Effects of estrogen replacement therapy on natriuretic peptides and blood pressure. Maturitas 47: 201–208, 2004 [DOI] [PubMed] [Google Scholar]
- 70.Kass DA, Bronzwaer JG, Paulus WJ. What mechanisms underlie diastolic dysfunction in heart failure? Circ Res 94: 1533–1542, 2004 [DOI] [PubMed] [Google Scholar]
- 71.Kawaguchi M, Hay I, Fetics B, Kass DA. Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: implications for systolic and diastolic reserve limitations. Circulation 107: 714–720, 2003 [DOI] [PubMed] [Google Scholar]
- 72.Kitzman DW. Diastolic heart failure in the elderly. Heart Fail Rev 7: 17–27, 2002 [DOI] [PubMed] [Google Scholar]
- 73.Kitzman DW, Groban L. Exercise intolerance. Cardiol Clin 29: 461–477, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Knowlton AA, Lee AR. Estrogen and the cardiovascular system. Pharmacol Ther 135: 54–70, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kravtsov GM, Kam KW, Liu J, Wu S, Wong TM. Altered Ca2+ handling by ryanodine receptor and Na+-Ca2+ exchange in the heart from ovariectomized rats: role of protein kinase A. Am J Physiol Cell Physiol 292: C1625–C1635, 2007 [DOI] [PubMed] [Google Scholar]
- 76.Lacombe VA, Viatchenko-Karpinski S, Terentyev D, Sridhar A, Emani S, Bonagura JD, Feldman DS, Györke S, Carnes CA. Mechanisms of impaired calcium handling underlying subclinical diastolic dysfunction in diabetes. Am J Physiol Regul Integr Comp Physiol 293: R1787–R1797, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lam CS, Cheng S, Choong K, Larson MG, Murabito JM, Newton-Cheh C, Bhasin S, McCabe EL, Miller KK, Redfield MM, Vasan RS, Coviello AD, Wang TJ. Influence of sex and hormone status on circulating natriuretic peptides. J Am Coll Cardiol 58: 618–626, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lam KK, Lee YM, Hsiao G, Chen SY, Yen MH. Estrogen therapy replenishes vascular tetrahydrobiopterin and reduces oxidative stress in ovariectomized rats. Menopause 13: 294–302, 2006 [DOI] [PubMed] [Google Scholar]
- 79.Levick SP, Meléndez GC, Plante E, McLarty JL, Brower GL, Janicki JS. Cardiac mast cells: the centrepiece in adverse myocardial remodelling. Cardiovasc Res 89: 12–19, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lindsey SH, Cohen JA, Brosnihan KB, Gallagher PE, Chappell MC. Chronic treatment with the G protein-coupled receptor 30 agonist G-1 decreases blood pressure in ovariectomized mRen2.Lewis rats. Endocrinology 150: 3753–3758, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lindsey SH, Carver KA, Prossnitz ER, Chappell MC. Vasodilation in response to the GPR30 agonist G-1 is not different from estradiol in the mRen2.Lewis female rat. J Cardiovasc Pharmacol 57: 598–603, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lindsey SH, da Silva AS, Silva MS, Chappell MC. Reduced vasorelaxation to estradiol and G-1 in aged female and adult male rats is associated with GPR30 downregulation. Am J Physiol Endocrinol Metab 305: E113–E118, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Linsdey SH, Liu L, Chappell MC. Vasodilation by GPER in mesenteric arteries involves both endothelial nitric oxide and smooth muscle cAMP signaling. Steroids; http://dx.doi.org/10.1016/j.steroids.2013.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lipman RD, Chrisp CE, Hazzard DG, Bronson RT. Pathologic characterization of brown Norway, brown Norway × Fischer 344, and Fischer 344 × brown Norway rats with relation to age. J Gerontol A Biol Sci Med Sci 51: B54-B59, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O'Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y; American Heart Association Statistics Committee, Stroke Statistics Subcommittee Heart disease and stroke statistics–2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 119: e21-e181, 2009 [DOI] [PubMed] [Google Scholar]
- 86.López-Rivera E, Lizarbe TR, Martínez-Moreno M, López-Novoa JM, Rodríguez-Barbero A, Rodrigo J, Fernández AP, Alvarez-Barrientos A, Lamas S, Zaragoza C. Matrix metalloproteinase 13 mediates nitric oxide activation of endothelial cell migration. Proc Natl Acad Sci USA 102: 3685–3690, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Maffucci JA, Gore AC. Age-related changes in hormones and their receptors in animal models of female reproductive senescence. In: Handbook of Models for Human Aging, edited by Conn MP. Burlington, MA: Elsevier, 2006, p. 533–552 [Google Scholar]
- 88.Manson JE. The Kronos Early Estrogen Prevention Study by Charlotte Barker. Women Health 9: 9–11, 2013 [DOI] [PubMed] [Google Scholar]
- 89.Manrique C, DeMarco VG, Aroor AR, Mugerfeld I, Garro M, Habibi J, Hayden MR, Sowers JR. Obesity and insulin resistance induce early development of diastolic dysfunction in young female mice fed a Western diet. Endocrinology 154: 3632–3642, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Marques CM, Nascimento FA, Mandarim-de-Lacerda CA, Aguila MB. Exercise training attenuates cardiovascular adverse remodeling in adult ovariectomized spontaneously hypertensive rats. Menopause 13: 87–95, 2006 [DOI] [PubMed] [Google Scholar]
- 91.Martin FL, McKie PM, Cataliotti A, Sangaralingham SJ, Korinek J, Huntley BK, Oehler EA, Harders GE, Ichiki T, Mangiafico S, Nath KA, Redfield MM, Chen HH, Burnett JC., Jr Experimental mild renal insufficiency mediates early cardiac apoptosis, fibrosis, and diastolic dysfunction: a kidney-heart connection. Am J Physiol Regul Integr Comp Physiol 302: R292–R299, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Maurer MS, Spevack D, Burkhoff D, Kronzon I. Diastolic dysfunction. Can it be diagnosed by Doppler echocardiography? J Am Coll Cardiol 44: 1543–1549, 2004 [DOI] [PubMed] [Google Scholar]
- 93.Mayer LP, Devine PJ, Dyer CA, Hoyer PB. The follicle-deplete mouse ovary produces androgen. Biol Reprod 71: 130–138, 2004 [DOI] [PubMed] [Google Scholar]
- 94.Miller JA, Anacta LA, Cattran DC. Impact of gender on the renal response to angiotensin II. Kidney Int 55: 278–285, 1999 [DOI] [PubMed] [Google Scholar]
- 95.Miyazaki-Akita A, Hayashi T, Ding QF, Shiraishi H, Nomura T, Hattori Y, Iguchi A. 17β-Estradiol antagonizes the down-regulation of endothelial nitric-oxide synthase and GTP cyclohydrolase I by high glucose: relevance to postmenopausal diabetic cardiovascular disease. J Pharmacol Exp Ther 320: 591–598, 2007 [DOI] [PubMed] [Google Scholar]
- 96.Mizutani S, Ishii M, Hattori A, Nomura S, Numaguchi Y, Tsujimoto M, Kobayshi H, Murohara T, Wright JW. New insights into the importance of aminopeptidase A in hypertension. Heart Fail Rev 13: 273–284, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Moens AL, Leyton-Mange JS, Niu X, Yang R, Cingolani O, Arkenbout EK, Champion HC, Bedja D, Gabrielson KL, Chen J, Xia Y, Hale AB, Channon KM, Halushka MK, Barker N, Wuyts FL, Kaminski PM, Wolin MS, Kass DA, Barouch LA. Adverse ventricular remodeling and exacerbated NOS uncoupling from pressure-overload in mice lacking the β3-adrenoreceptor. J Mol Cell Cardiol 47: 576–585, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mori T, Kai H, Kajimoto H, Koga M, Kudo H, Takayama N, Yasuoka S, Anegawa T, Kai M, Imaizumi T. Enhanced cardiac inflammation and fibrosis in ovariectomized hypertensive rats: a possible mechanism of diastolic dysfunction in postmenopausal women. Hypertens Res 34: 496–502, 2011 [DOI] [PubMed] [Google Scholar]
- 99.Murase T, Hattori T, Ohtake M, Nakashima C, Takatsu M, Murohara T, Nagata K. Effects of estrogen on cardiovascular injury in ovariectomized female DahlS.Z-Leprfa/Leprfa rats as a new animal model of metabolic syndrome. Hypertension 59: 694–704, 2012 [DOI] [PubMed] [Google Scholar]
- 100.Muntner P, He J, Hamm L, Loria C, Whelton PK. Renal insufficiency and subsequent death resulting from cardiovascular disease in the United States. J Am Soc Nephrol 13: 745–753, 2002 [DOI] [PubMed] [Google Scholar]
- 101.Nickenig G, Bäumer AT, Grohè C, Kahlert S, Strehlow K, Rosenkranz S, Stäblein A, Beckers F, Smits JF, Daemen MJ, Vetter H, Böhm M. Estrogen modulates AT1 receptor gene expression in vitro and in vivo. Circulation 97: 2197–2201, 1998 [DOI] [PubMed] [Google Scholar]
- 102.Nicklas BJ, Cesari M, Penninx BWJH, Kritchevsky SB, Ding J, Newman A, Kitzman DW, Kanaya AM, Pahor M, Harris TB. Abdominal obesity is an independent risk factor for chronic heart failure in older people. J Am Geriatr Soc 54: 413–420, 2006 [DOI] [PubMed] [Google Scholar]
- 103.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 355: 251–259, 2006 [DOI] [PubMed] [Google Scholar]
- 104.Patten RD, Hall-Porter MR. Small animal models of heart failure: development of novel therapies, past and present. Circ Heart Fail 2: 138–144, 2009 [DOI] [PubMed] [Google Scholar]
- 105.Pechenino AS, Lin L, Mbai FN, Lee AR, He XM, Stallone JN, Knowlton AA. Impact of aging vs. estrogen loss on cardiac gene expression: estrogen replacement and inflammation. Physiol Genomics 43: 1065–1073, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pendergrass KD, Averill DB, Ferrario CM, Diz DI, Chappell MC. Differential expression of nuclear AT1 receptors and angiotensin II within the kidney of the male congenic mRen2.Lewis rat. Am J Physiol Renal Physiol 290: F1497–F1506, 2006 [DOI] [PubMed] [Google Scholar]
- 107.Pendergrass KD, Pirro NT, Westwood BM, Ferrario CM, Brosnihan KB, Chappell MC. Sex differences in circulating and renal angiotensins of hypertensive mRen(2).Lewis but not normotensive Lewis rats. Am J Physiol Heart Circ Physiol 295: H10–H20, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Perticone F, Sciacqua A, Maio R, Perticone M, Laino I, Bruni R, Cello SD, Leone GG, Greco L, Andreozzi F, Sesti G. Renal function predicts cardiovascular outcomes in southern Italian postmenopausal women. Eur J Cardiovasc Prev Rehabil 16: 481–486, 2009 [DOI] [PubMed] [Google Scholar]
- 109.Peterson LR, Waggoner AD, Schechtman KB, Meyer T, Gropler RJ, Barzilai B, Dávila-Román VG. Alterations in left ventricular structure and function in young healthy obese women: assessment by echocardiography and tissue Doppler imaging. J Am Coll Cardiol 43: 1399–1404, 2004 [DOI] [PubMed] [Google Scholar]
- 110.Peterson LR, Saeed IM, McGill JB, Herrero P, Schechtman KB, Gunawardena R, Recklein CL, Coggan AR, Demoss AJ, Dence CS, Gropler RJ. Sex and type 2 diabetes: obesity-independent effects on left ventricular substrate metabolism and relaxation in humans. Obesity 20: 802–810, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Proudler AJ, Ahmed AI, Crook D, Fogelman I, Rymer JM, Stevenson JC. Hormone replacement therapy and serum angiotensin-converting-enzyme activity in postmenopausal women. Lancet 346: 89–90, 1995 [DOI] [PubMed] [Google Scholar]
- 112.Ram R, Mickelsen DM, Theodoropoulos C, Blaxall BC. New approaches in small animal echocardiography: imaging the sounds of silence. Am J Physiol Heart Circ Physiol 301: H1765–H1780, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Redfield MM, Jacobsen SJ, Borlaug BA, Rodeheffer RJ, Kass DA. Age- and gender-related ventricular-vascular stiffening: a community-based study. Circulation 112: 2254–2262, 2005 [DOI] [PubMed] [Google Scholar]
- 114.Regitz-Zagrosek V, Oertelt-Prigione S, Seeland U, Hetzer R. Sex and gender differences in myocardial hypertrophy and heart failure. Circ J 74: 1265–1273, 2010 [DOI] [PubMed] [Google Scholar]
- 115.Reichelt ME, Mellor KM, Bell JR, Chandramouli C, Headrick JP, Delbridge LM. Sex, sex steroids, and diabetic cardiomyopathy: making the case for experimental focus. Am J Physiol Heart Circ Physiol 305: H779–H792, 2013 [DOI] [PubMed] [Google Scholar]
- 116.Roesch DM, Tian Y, Zheng W, Shi M, Verbalis JG, Sandberg K. Estradiol attenuates angiotensin-induced aldosterone secretion in ovariectomized rats. Endocrinology 141: 4629–4636, 2000 [DOI] [PubMed] [Google Scholar]
- 117.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; American Heart Association Statistics Committee, Stroke Statistics Subcommittee Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation 125: e2-e220, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J; Writing Group for the Women's Health Initiative Investigators Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results. From the Women's Health Initiative randomized controlled trial. JAMA 288: 321–333, 2002 [DOI] [PubMed] [Google Scholar]
- 119.Rubanyi GM, Vanhoutte PM. Superoxide anions and hyperoxia inactivate endothelium-derived relaxing factor. Am J Physiol Heart Circ Physiol 250: H822–H827, 1986 [DOI] [PubMed] [Google Scholar]
- 120.Sacherer M, Sedei S, Wakula P, Wallner M, Vos MA, Kockskämper J, Stiegler P, Sereinigg M, von Lewinski D, Antoons G, Pieske BM, Heinzel FR; CONTICA Investigators JTV519(K201) reduces sarcoplasmic reticulum Ca2+ leak and improves diastolic function in vitro in murine and human non-failing myocardium. Br J Pharmacol 167: 493–504, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Salpeter SR, Walsh JM, Greyber E, Salpeter EE. Brief report: Coronary heart disease events associated with hormone therapy in younger and older women. A meta-analysis. J Gen Intern Med 21: 363–366, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Sanders D, Dudley M, Groban L. Diastolic dysfunction, cardiovascular aging, and the anesthesiologist. Anesthesiol Clin 27: 497–517, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Schulz E, Jansen T, Wenzel P, Daiber A, Münzel T. Nitric oxide, tetrahydrobiopterin, oxidative stress, and endothelial dysfunction in hypertension. Antioxid Redox Signal 10: 1115–1126, 2008 [DOI] [PubMed] [Google Scholar]
- 124.Schumacher A, Khojeini E, Larson D. ECHO parameters of diastolic dysfunction. Perfusion 23: 291–296, 2008 [DOI] [PubMed] [Google Scholar]
- 125.Schunkert H, Danser AH, Hense HW, Derkx FH, Kürzinger S, Riegger GA. Effects of estrogen replacement therapy on the renin-angiotensin system in postmenopausal women. Circulation 95: 39–45, 1997 [DOI] [PubMed] [Google Scholar]
- 126.Serova LI, Maharjan S, Huang A, Sun D, Kaley G, Sabban EL. Response of tyrosine hydroxylase and GTP cyclohydrolase I gene expression to estrogen in brain catecholaminergic regions varies with mode of administration. Brain Res 1015: 1–8, 2004 [DOI] [PubMed] [Google Scholar]
- 127.Serova LI, Maharjan S, Sabban EL. Estrogen modifies stress response of catecholamine biosynthetic enzyme genes and cardiovascular system in ovariectomized female rats. Neuroscience 132: 249–259, 2005 [DOI] [PubMed] [Google Scholar]
- 128.Serova LI, Filipenko M, Schilt N, Veerasirikul M, Sabban EL. Estrogen-triggered activation of GTP cyclohydrolase 1 gene expression: role of estrogen receptor subtypes and interaction with cyclic AMP. Neuroscience 140: 1253–1263, 2006 [DOI] [PubMed] [Google Scholar]
- 129.Shapiro Y, Boaz M, Matas Z, Fux A, Shargorodsky M. The association between the renin-angiotensin-aldosterone system and arterial stiffness in young healthy subjects. Clin Endocrinol (Oxf) 68: 510–512, 2008 [DOI] [PubMed] [Google Scholar]
- 130.Shekelle PG, Rich MW, Morton SC, Atkinson CS, Tu W, Maglione M, Rhodes S, Barrett M, Fonarow GC, Greenberg B, Heidenreich PA, Knabel T, Konstam MA, Steimle A, Warner Stevenson L. Efficacy of angiotensin-converting enzyme inhibitors and β-blockers in the management of left ventricular systolic dysfunction according to race, gender, and diabetic status: a meta-analysis of major clinical trials. J Am Coll Cardiol 41: 1529–1538, 2003 [DOI] [PubMed] [Google Scholar]
- 131.Silberman GA, Fan TH, Liu H, Jiao Z, Xiao HD, Lovelock JD, Boulden BM, Widder J, Fredd S, Bernstein KE, Wolska BM, Dikalov S, Harrison DG, Dudley SC., Jr Uncoupled cardiac nitric oxide synthase mediates diastolic dysfunction. Circulation 121: 519–528, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Smith CC, Vedder LC, Nelson AR, Bredemann TM, McMahon LL. Duration of estrogen deprivation, not chronological age, prevents estrogen's ability to enhance hippocampal synaptic physiology. Proc Natl Acad Sci USA 107: 19543–19548, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E, Shi V, Bransford T, Takeuchi M, Gong J, Lefkowitz M, Packer M, McMurray JJ; Prospective Comparison of ARNI with ARB on Management of Heart Failure with Preserved Ejection Fraction (PARAMOUNT) Investigators The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet 380: 1387–1395, 2012 [DOI] [PubMed] [Google Scholar]
- 134.Staessen J, Bulpitt CJ, Fagard R, Lijnen P, Amery A. The influence of menopause on blood pressure. J Hum Hypertens 3: 427–433, 1989 [PubMed] [Google Scholar]
- 135.Stein GY, Ben-Gal T, Kremer A, Bental T, Alon D, Korenfeld R, Yedidia I, Porter A, Abramson E, Sagie A, Fuchs S. Gender-related differences in hospitalized heart failure patients. Eur J Heart Fail 15: 734–741, 2013 [DOI] [PubMed] [Google Scholar]
- 136.Stice JP, Eiserich JP, Knowlton AA. Role of aging versus the loss of estrogens in the reduction in vascular function in female rats. Endocrinology 150: 212–219, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Stiles S. Aldo-Antagonist Falls Short but Impresses in Preserved-EF Heart Failure: TOPCAT. (online) http://www.medscape.com/viewarticle/814622 [12 December 2013]
- 138.Stroes E, Hijmering M, van Zandvoort M, Wever R, Rabelink TJ, van Faassen EE. Origin of superoxide production by endothelial nitric oxide synthase. FEBS Lett 438: 161–164, 1998 [DOI] [PubMed] [Google Scholar]
- 139.Sullivan JC. Sex and the renin-angiotensin system: inequality between the sexes in response to RAS stimulation and inhibition. Am J Physiol Regul Integr Comp Physiol 294: R1220–R1226, 2008 [DOI] [PubMed] [Google Scholar]
- 140.Sweitzer NK, Stevenson LW. Diastolic heart failure: miles to go before we sleep. Am J Med 109: 683–685, 2000 [DOI] [PubMed] [Google Scholar]
- 141.Takimoto E, Champion HC, Li M, Ren S, Rodriguez ER, Tavazzi B, Lazzarino G, Paolocci N, Gabrielson KL, Wang Y, Kass DA. Oxidant stress from nitric oxide synthase-3 uncoupling stimulates cardiac pathologic remodeling from chronic pressure load. J Clin Invest 115: 1221–1231, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Thomas MD, Fox KF, Coats AJ, Sutton GC. The epidemiological enigma of heart failure with preserved systolic function. Eur J Heart Fail 6: 125–136, 2004 [DOI] [PubMed] [Google Scholar]
- 143.Tyagi SC, Hayden MR. Role of nitric oxide in matrix remodeling in diabetes and heart failure. Heart Fail Rev 8: 23–28, 2003 [DOI] [PubMed] [Google Scholar]
- 144.Vásquez-Vivar J, Kalyanaraman B, Martásek P, Hogg N, Masters BS, Karoui H, Tordo P, Pritchard KA., Jr Superoxide generation by endothelial nitric oxide synthase: the influence of cofactors. Proc Natl Acad Sci USA 95: 9220–9225, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Victor BM, Barron JT. Diastolic heart failure versus diastolic dysfunction: difference in renal function. Clin Cardiol 33: 770–774, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Vogel MW, Slusser JP, Hodge DO, Chen HH. The natural history of preclinical diastolic dysfunction: a population-based study. Circ Heart Fail 5: 144–151, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Voloshenyuk TG, Gardner JD. Estrogen improves TIMP-MMP balance and collagen distribution in volume-overloaded hearts of ovariectomized females. Am J Physiol Regul Integr Comp Physiol 299: R683–R693, 2010 [DOI] [PubMed] [Google Scholar]
- 148.von Lueder TG, Sangaralingham SJ, Wang BH, Kompa AR, Atar D, Burnett JC, Jr, Krum H. Renin-angiotensin blockade combined with natriuretic peptide system augmentation: novel therapeutic concepts to combat heart failure. Circ Heart Fail 6: 594–605, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wang H, Jessup JA, Lin MS, Chagas C, Lindsey SH, Groban L. Activation of GPR30 attenuates diastolic dysfunction and left ventricle remodelling in oophorectomized mRen2.Lewis rats. Cardiovasc Res 94: 96–104, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wang H, Jessup JA, Zhao Z, Da Silva J, Lin M, MacNamara LM, Ahmad S, Chappell MC, Ferrario CM, Groban L. Characterization of the cardiac renin angiotensin system in oophorectomized and estrogen-replete mRen2.Lewis rats. PLOS ONE 8: e76992, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Weber KT. Fibrosis and hypertensive heart disease. Curr Opin Cardiol 15: 264–272, 2000 [DOI] [PubMed] [Google Scholar]
- 152.Weil BR, Manukyan MC, Herrmann JL, Wang Y, Abarbanell AM, Poynter JA, Meldrum DR. Signaling via GPR30 protects the myocardium from ischemia/reperfusion injury. Surgery 148: 436–443, 2010 [DOI] [PubMed] [Google Scholar]
- 153.Weinberg EO, Thienelt CD, Katz SE, Bartunek J, Tajima M, Rohrbach S, Douglas PS, Lorell BH. Gender differences in molecular remodeling in pressure overload hypertrophy. J Am Coll Cardiol 34: 264–273, 1999 [DOI] [PubMed] [Google Scholar]
- 154.Whaley-Connell A, Habibi J, Rehmer N, Ardhanari S, Hayden MR, Pulakat L, Krueger C, Ferrario CM, DeMarco VG, Sowers JR. Renin inhibition and AT1R blockade improve metabolic signaling, oxidant stress and myocardial tissue remodeling. Metabolism 62: 861–872, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Wing LM, Reid CM, Ryan P, Beilin LJ, Brown MA, Jennings GL, Johnston CI, McNeil JJ, Macdonald GJ, Marley JE, Morgan TO, West MJ; Second Australian National Blood Pressure Study Group A comparison of outcomes with angiotensin-converting-enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 348: 583–592, 2003 [DOI] [PubMed] [Google Scholar]
- 156.Witteveen CF, Giovanelli J, Kaufman S. Reduction of quinonoid dihydrobiopterin to tetrahydrobiopterin by nitric oxide synthase. J Biol Chem 271: 4143–4147, 1996 [DOI] [PubMed] [Google Scholar]
- 157.Witteveen CF, Giovanelli J, Kaufman S. Reactivity of tetrahydrobiopterin bound to nitric-oxide synthase. J Biol Chem 274: 29755–29762, 1999 [DOI] [PubMed] [Google Scholar]
- 158.Wu Z, Maric C, Roesch DM, Zheng W, Verbalis JG, Sandberg K. Estrogen regulates adrenal angiotensin AT1 receptors by modulating AT1 receptor translation. Endocrinology 144: 3251–3261, 2003 [DOI] [PubMed] [Google Scholar]
- 159.Yamaleyeva LM, Gallagher PE, Vinsant S, Chappell MC. Discoordinate regulation of renal nitric oxide synthase isoforms in ovariectomized mRen2.Lewis rats. Am J Physiol Regul Integr Comp Physiol 292: R819–R826, 2007 [DOI] [PubMed] [Google Scholar]
- 160.Yamaleyeva LM, Pendergrass KD, Pirro NT, Gallagher PE, Groban L, Chappell MG. Ovariectomy is protective against renal injury in the high-salt-fed older mRen2.Lewis rat. Am J Physiol Heart Circ Physiol 293: H2064–H2071, 2007 [DOI] [PubMed] [Google Scholar]
- 161.Yamaleyeva LM, Lindsey SH, Varagic J, Zhang LL, Gallagher PE, Chen AF, Chappell MC. Amelioration of renal injury and oxidative stress by the nNOS inhibitor L-VNIO in the salt-sensitive mRen2.Lewis congenic rat. J Cardiovasc Pharmacol 59: 529–538, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Yanes LL, Romero DG, Iliescu R, Zhang H, Davis D, Reckelhoff JF. Postmenopausal hypertension: role of the renin-angiotensin system. Hypertension 56: 359–363, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Yu X, Ma H, Barman SA, Liu AT, Sellers M, Stallone JN, Prossnitz ER, White RE, Han G. Activation of G protein-coupled estrogen receptor induces endothelium-independent relaxation of coronary artery smooth muscle. Am J Physiol Endocrinol Metab 301: E882–E888, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Yung LM, Wong WT, Tian XY, Leung FP, Yung LH, Chen ZY, Yao X, Lau CW, Huang Y. Inhibition of renin-angiotensin system reverses endothelial dysfunction and oxidative stress in estrogen deficient rats. PLOS ONE 6: e17437, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zapater P, Novalbos J, Gallego-Sandín S, Hernández FT, Abad-Santos F. Gender differences in angiotensin-converting enzyme (ACE) activity and inhibition by enalaprilat in healthy volunteers. J Cardiovasc Pharmacol 43: 737–744, 2004 [DOI] [PubMed] [Google Scholar]
- 166.Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure: part II: causal mechanisms and treatment. Circulation 105: 1503–1508, 2002 [DOI] [PubMed] [Google Scholar]
- 167.Zile MR, Baicu CF, Gaasch WH. Diastolic heart failure–abnormalities in active relaxation and passive stiffness of the left ventricle. N Engl J Med 350: 1953–1959, 2004 [DOI] [PubMed] [Google Scholar]