Abstract
This study evaluated whether Tai Ji Quan: Moving for Better Balance (TJQMBB) could improve global cognitive function in older adults with cognitive impairment. Using a nonrandomized control group pretest-posttest design, participants aged ≥65 years who scored between 20 and 25 on the Mini-Mental State Examination (MMSE) were allocated into either a 14-week TJQMBB program (n=22) or a control group (n=24). The primary outcome was MMSE as a measure of global cognitive function with secondary outcomes of 50-foot speed walk, Timed Up&Go, and Activities-Specific Balance Confidence (ABC) scale. At 14 weeks, Tai Ji Quan participants showed significant improvement on MMSE (mean=2.26, p<0.001) compared to controls (mean=0.63, p=0.08). Similarly, Tai Ji Quan participants performed significantly better compared to the controls in both physical performance and balance efficacy measures (p<0.05). Improvement in cognition as measured by MMSE was related to improved physical performance and balance efficacy. These results provide preliminary evidence of the utility of the TJQMBB program to promote cognitive function in older adults in addition to physical benefits.
Keywords: cognitive ability, cognitive impairment, Tai Ji Quan
1. Introduction
It is estimated that as many as 20% of people age 65 and older have at least mild cognitive impairment (MCI) (Hanninen, Hallikainen, Tuomainen, Vanhanen, & Soininen, 2002; Lopez et al., 2003; Roberts et al., 2008), with an estimated annual conversion rate from MCI to dementia of 10% (Manly et al., 2008). Even for those without dementia, cognitive impairment can contribute to decreased quality of life, increased neuropsychiatric symptoms, and increased disability and healthcare costs (Alzheimer’s Association, 2012; Plassman et al., 2008).
Behavioral interventions, such as exercise, can provide cognitive benefits to older adults with cognitive impairment (Chang, Pan, Chen, Tsai, & Huang, 2012; Dresler et al., 2013; Erickson & Kramer, 2009; Etnier & Chang, 2009; Hahn & Andel, 2011) and are often recommended as a therapy for cognitive health (US Department of Health and Human Services, 2012). While conventional exercise modalities have been shown to improve cognition in older adults (Baker et al., 2010; Larson et al., 2006), there is emerging evidence to suggest that physical demands combined with mental challenges may have an additive effect on brain health and cognitive function (Curlik & Shors, 2013).
Tai Ji Quan, an alternative exercise regimen that incorporates both physical activity and cognitive requirements, is therefore posited to promote brain health (Chang, Nien, Tsai, & Etnier, 2010; Chang et al., 2011; Cheng et al., 2013). While findings from a limited number of existing studies (Burgener, Yang, Gilbert, & Marsh-Yant, 2008; Cheng et al., 2013; Lam et al., 2012; Mortimer et al., 2012) have provided the scientific basis and therapeutic impetus to further explore the cognitive benefits of Tai Ji Quan, few studies have considered exploiting the explicit integration of multi-tasking and combined mental and physical skill learning that would uniquely tax physical, sensory, and cognitive function simultaneously in this regard. This pilot study addresses this limitation by serving as a proof of concept for the utility of this integrated evidence-based Tai Ji Quan program that has been widely studied as a fall prevention intervention in older adults, a population at significant risk of developing cognitive impairment.
Specifically, this study explored the potential value of Tai Ji Quan: Moving for Better Balance (TJQMBB; Li et al., 2008; Li, in press; Li et al., 2013), to benefit cognitive function in older adults. The TJQMBB program has been proven to enhance physical performance, balance, well-being, and sleep quality and, most recently, to reduce symptoms of Parkinson’s disease (Li, in press). Although promising, its potential benefit to cognition has not been explored. Therefore, the primary aim of this study was to determine whether TJQMBB, with an enhanced training feature of integrating dynamic postural movements and concurrently challenging multiple dimensions of cognitive ability (Li et al., 2013), could improve global cognitive function in older adults with cognitive impairment.
Additionally, because cognitive impairment may also be associated with impaired physical performance (Aqqarwal, Wilson, Beck, Bienias, & Bennett, 2006) and Tai Ji Quan is specifically designed to stimulate both cognitive and physical capacities (Li, in press), it was also of interest to examine the concurrent relationships of these domains as a result of Tai Ji Quan exercise. Therefore, a secondary aim of the study was to examine whether change in global cognitive function was related to change in physical performance-based outcome and balance efficacy measures.
2. Methods
2.1. Study design and participants
A nonrandomized control group pretest-posttest design was used. Participants assigned to the intervention group (Tai Ji Quan) participated in a 60-minute group session twice weekly for 14 weeks. The study protocol was approved by an Institutional Review Board, and written informed consent was obtained from each participant.
Participants were recruited between April and August 2012 primarily through community-wide promotions, such as flyers, newsletters, and word of mouth at local senior and community activity centers in communities in Oregon, to participate in a community-based Tai Ji Quan dissemination project. Study eligibility criteria included (1) being ≥65 years of age, (2) being able to walk with or without an assistive device, (3) having Mini-Mental State Examination (MMSE) (Folstein, Folstein, & McHugh, 1975) scores between 20 and 30, and (4) having a medical clearance from a healthcare provider.
Individuals who responded to the study promotions were initially contacted via phone for screening for age and mobility criteria and subsequently invited to a research facility where a detailed, face-to-face intake process, including signing consent forms and completing the MMSE and other baseline measures, was conducted. Prior to signing the informed consent, participants were given sufficient time in a private room to ask questions regarding the study protocol and Tai Ji Quan exercise. Research assistants trained and monitored by the first author performed the study screening and outcome assessments.
For the purposes of this study, a subsample of 46 participants who had a score between 20 and 25 on the MMSE was selected as having cognitive impairment (Folstein, Folstein, McHugh, & Fanjiang, 2001; Mungas, 1991; O’Bryant et al., 2008; Spering et al., 2012; Vertesi et al., 2001). The decision to use this range of scores allows us to evaluate the relationship between Tai Ji Quan and cognitive function without a possible confounding effect of severe cognitive impairment. Of the total, those assigned to the control group (n=24) were individuals who could not participate in the intervention class due to logistical reasons such as time constraints and/or location and transportation issues but who were willing to participate in a follow-up assessment.
2.2. Primary outcome variable: Global cognitive function
All study outcome measures were taken twice: at baseline and again upon completion of the 14-week intervention. The primary study outcome was cognitive function as measured by the MMSE (Folstein et al., 1975). The MMSE consists of 11 questions concerning orientation, registration, attention and calculation, recall, and language and has a maximum score of 30. The 3-month test-retest reliability was 0.87.
2.3. Secondary outcome variables: Physical performance and balance efficacy
Two physical performance measures consisted of (a) 50-foot speed walk (Reuben & Siu, 1990) and (b) Timed Up&Go test (Podsiadlo & Richardson, 1991). The 50-foot walk measured the time, in seconds, taken to walk 50 feet. The Up&Go measured the time, in seconds, taken to rise from a chair, walk 10 feet (3 meters), return, and sit down. Test and retest reliability for the two measures was 0.59 (Timed Up&Go) and 0.67 (50 foot walk), respectively. Balance efficacy was measured using the Modified Activities-Specific Balance Confidence (ABC) scale (Powell & Myers, 2005), which measures confidence in one’s ability to avoid falling during activities of daily living. Participants were asked to rate their confidence in performing each activity without falling on a 1–5 scale; the average score across all 14 items was taken, with a minimum score of 1 indicating “not at all confident” and a maximum score of 5 indicating “completely confident” in performing the tasks without falling. The 3-month test-retest reliability for this measure was 0.87.
2.4. Other assessments
Participants completed a self-survey that collected their demographic, health status, and medical and chronic conditions information. The Physical Activity Scale for the Elderly (Washburn, Smith, Jette, & Janney, 1993) was used to assess occupational, household, and leisure time physical activities over a typical week.
2.5. Study conditions
Tai Ji Quan: The TJQMBB program (Li et al., 2008; Li, in press; Li et al., 2013) consisted of a set of movements designed specifically for older adults, with an emphasis on taxing motor performance, orientation, verbalization, visualization, and mental execution of simple-to-complex movements that have been shown to improve balance and mobility and reduce fear of falling and risk of falling. The 14-week training period was determined a priori based on studies that involve the use of MMSE (Burgener et al., 2008; Chang et al., 2011).
The training protocol began with a brief Tai Ji Quan-based warm-up activity followed by core training of movements contained in an 8-form routine and a set of therapeutic movements (Li et al., 2013). Unlike conventional Tai Ji Quan training which primarily involves participants learning forms by mimicking the instructor's movements, in the protocol used in this study, participants must follow the instructor's movement while simultaneously and deliberately responding to a variety of specific tasks designed to further tax cognitive function by adding attentional demands and memory interference. For example, in performing the form “Part the Wild Horse Mane,” participants had to recite the name of this form or an associated word/number, distinguish between a visual target movement and a conflicting auditory cue, and, when connected with other forms, change the sequence of forms when prompted by the instructor (requiring accurate recall and execution in a non-standard format). Practices were infused with multiple cognitive/motor tasks of these kinds through variations in configurations, teaching cues, and movement complexity.
To facilitate learning the Tai Ji Quan movements, ample practice opportunities were allocated during the first 6 weeks, with the emphasis on practicing single forms with multiple repetitions; the latter stage (the last 8 weeks) focused on practicing and repeating individual forms to strengthen integration of cognitive and physical tasks. Natural breathing was emphasized and integrated into the practice routine.
The program was delivered by qualified instructors, trained by the first author. Five intervention classes were conducted in local senior centers, with 10–15 participants in each class. The intervention teaching protocol, including program fidelity, was monitored by the first author per criteria described previously (Li et al., 2013).
Control: The control participants were asked to maintain their usual daily physical activities during the 14-week observational period.
2.6. Statistical analysis
Baseline demographic descriptors and primary and secondary outcome measures were compared between study groups (Tai Ji Quan vs. control), using analysis of variance for continuous variables, chi-square test for categorical variables, or tests for proportions. The primary efficacy analysis used a repeated analysis of variance (ANOVA) model to determine differences between groups over time. The independent variable was intervention (Tai Ji Quan or Control), dependent variables were the primary and secondary outcome measures, and covariates were baseline values of outcome variables and other demographic factors, including age, gender, education, living conditions, and health status. When these demographic covariates were included in the models, the results did not change. Relationships between changes in MMSE and the two physical performance and balance efficacy variables were evaluated using Pearson’s correlation coefficient. All P values were 2-sided, and analyses were performed using SPSS 17.0 for Windows.
3. Results
3.1. Sample characteristics
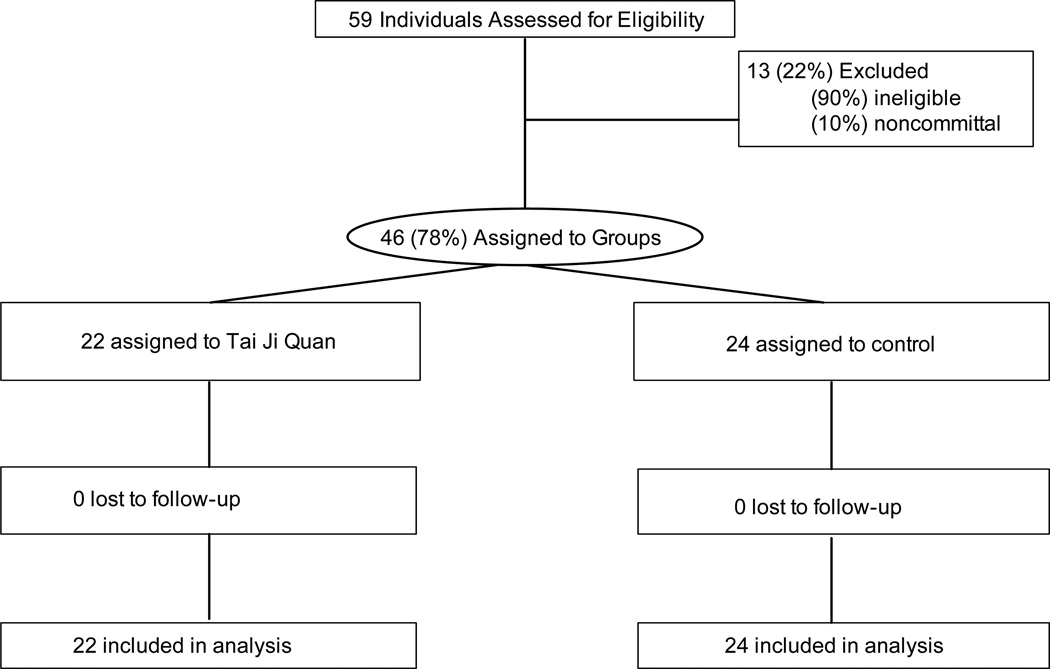
The study flow chart is presented in Figure 1. Baseline data on demographic, anthropometric, health status, medical conditions, and habitual physical activity characteristics of the study participants by study conditions are shown in Table 1. Analyses assessing the comparability of the two groups indicated that they were well matched with regard to baseline descriptors. Further analyses on the level of leisure physical activity between the two groups over the 14 weeks also indicated no significant differences (P = 0.28). There was also no significant change in the level of physical activity reported by participants in the control condition.
Figure 1.
Flow of Participants through the Nonrandomized Trial
Table 1.
Participant Characteristics by Nonrandomized Groups
| Tai Ji Quan = 22 | Control = 24 | P | |
|---|---|---|---|
| Female, no (%) | 15 (68%) | 17 (71%) | 0.44 |
| Age – mean (yr, standard deviation) | 75 (11) | 77 (10) | 0.54 |
| High school education or lower, no (%) | 12 (55%) | 9 (38%) | 0.67 |
| Household income below $35,000, no (%) | 21 (95%) | 19 (79%) | 0.86 |
| Common medical condition, mean (standard deviation) | 2.71 (1) | 2.54 (1) | 0.39 |
| Health status, mean (standard deviation) | 3.33 (0.73) | 3.37 (0.87) | 0.32 |
| Habitual physical activity, mean (standard deviation) | 113.87±62.19 | 112.25±61.35 | 0.21 |
Note: Common medical condition was measured on nine common medical conditions (e.g., diabetes, hypertension, depression). Health status was measured on a 5-point Likert scale with 1 = Poor and 5 = Excellent; higher scores indicated better health. Habitual physical activity was measured by the Physical Activity Scale for the Elderly (Washburn et al., 1993).
3.2. Attrition, Compliance, and Adverse Events
No participant dropped out of the study and all participants provided the outcome data. All Tai Ji Quan participants completed their 14-week training with a median class attendance of 22 sessions (range: 18–28 sessions). No adverse events or falls were observed during the course of intervention.
3.3. Global cognitive function
At the end of the 14-week intervention, Tai Ji Quan participants exhibited significant pre-to-post-intervention improvements in MMSE scores (t = 8.9, P < 0.001). No within-group pre-to-posttest change was observed for the control group. Consequently, there was a difference in the improvements from baseline between the groups. Compared to those in the control group, Tai Ji Quan subjects had significantly improved MMSE scores (F1,44 = 23.51, P < 0.001) (see Table 2). The effect size expressed in Cohen’s d, calculated as the difference between the Tai Ji Quan and control groups’ observed means at week 14 scaled by the pooled standard deviation, was 1.92.
Table 2.
Primary and Secondary Measures by Groups (Tai Ji Quan = 22; control = 24) at Pretest and Posttest
| PRE | POST | ||||
|---|---|---|---|---|---|
| Measures | Mean | SD | Mean | SD | P value |
| MMSE (range 0–30) | |||||
| Tai Ji Quan | 23.09 | 1.15 | 26.05 | 1.21 | <0.001 |
| Control | 23.17 | 1.20 | 23.79 | 1.14 | |
| 50-foot speed walk (sec) | |||||
| Tai Ji Quan | 15.29 | 4.27 | 13.51 | 3.65 | 0.02 |
| Control | 16.63 | 5.14 | 16.15 | 5.90 | |
| Timed Up&Go (sec) | |||||
| Tai Ji Quan | 11.36 | 5.57 | 9.67 | 5.29 | 0.01 |
| Control | 11.96 | 4.78 | 11.58 | 4.15 | |
| ABC (range: 1–5) | |||||
| Tai Ji Quan | 3.43 | 0.59 | 4.13 | 0.42 | <0.001 |
| Control | 3.45 | 0.56 | 3.55 | 0.53 | |
Note. MMSE = Mini-Mental State Examination. ABC = Activities-Specific Balance Confidence scale.
3.4. Physical performance and balance efficacy
Similarly, Tai Ji Quan participants exhibited significant pre-to-post-intervention improvements in the 50-foot speed walk (t = −8.20, P < 0.001, Cohen’s d = 0.53), Up& Go (t = −8.52, P < 0.001, Cohen’s d = 0.40), and ABC efficacy scores (t = 4.43, P <.0001, Cohen’s d = 1.21). No within-group pre-to-posttest change on the three secondary measures was observed for the control group. There was a difference in the improvements from baseline between groups. Compared to those in the control group, Tai Ji Quan participants had significantly improved 50-foot speed walk (F1,44 = 6.13, P = 0.02), Timed Up&Go (F1,44 = 6.82, P = 0.01), and ABC scores (F1,44 = 16.65, P < 0.001) scores (see Table 2).
3.5. Correlations between global cognitive function and secondary outcome variables
Changes in the MMSE scores were significantly correlated with the 50-foot speed walk (r = −0.44, P < 0.05), Timed Up&Go (r = −0.47, P < 0.05), and ABC scores (r=0.49, P<0.05), indicating that improvement in global cognitive function among Tai Ji Quan participants was associated with their improved physical performance (i.e., at a faster time) and belief in the ability to avoid a loss of balance during activities of daily living. The correlations between these relationships were not statistically significant for the control group (P = 0.26).
4. Discussion
After a 14-week intervention, the study showed that Tai Ji Quan participants improved significantly on the MMSE, a measure of global cognitive function. There were also concomitant improvements in physical performance measures of the 50-foot walk and Up&Go tests and a balance efficacy measure compared to those in the control group. In addition, as a pilot study the training protocol involving components of both physical and mental training was feasible in terms of implementation and was well tolerated, as evidenced by well-attended Tai Ji Quan sessions and an excellent program compliance.
The results from this study were in line with emerging research that shows physical activity, such as aerobic exercise (Baker et al., 2010) or general physical effort, including walking (Larson et al., 2006; Lautenschlager, Cox, Flicker et al., 2008; Maki, Ura, Yamaguchi et al., 2012), is associated with preservation of cognitive function. The results also support the findings of previous studies that indicate that Tai Ji Quan training may impact cognitive function in older adults in addition to enhancing physical attributes (Cheng et al., 2013; Lam et al., 2012; Mortimer et al., 2012; Taylor-Piliae et al., 2010). Specifically our finding of improvement in the global measure of MMSE is consistent with studies which have shown either short-term (Burgener et al., 2008) or dose-response (Chang et al., 2011) impact of Tai Ji Quan training on MMSE. However, the significant outcome from this study is that by deliberately targeting cognitive function through implementation of our multi-tasking approach, we observed a meaningful change in MMSE (as indicated by effect size) in only 14 weeks. This provides a preliminary indication that this specialized program can effect change more quickly than demonstrated byLam et al. (2012), thus providing the impetus for a larger-scale study to determine the trajectory of change in the longer term. Finally, unlikeLam et al. (2012), our study involved participants who did not have a cultural background related to Tai Chi (i.e., Americans rather than Chinese) and showed that the potential effects are not culture specific.
The precise mechanism(s) underlying the improvement in the global cognitive measure in this study is unclear. Potentially, given the deliberate multi-tasking nature of its movements, the Tai Ji Quan program is expected to engage significant spatial-temporal orientation, memory, and executive control resources as well as attention devoted to specific multi-segmental bodily movements and postural demands. The combined physical and mental challenges then tax the physiological and neurophysiological processes that drive positive adaptations in the brain. Future studies with neuroimaging may shed light on this explanation. Additionally, based on previous research (Curlik & Shors, 2013) that indicates that the combined effects of physical and mental training on cognition are greater than either independently because each affects different pathways, the integrated motor-cognitive training characteristics of this program may have driven the changes in cognitive function in the study population. Other possibilities include gains in physical function as a result of training leading to enhanced cognitive functioning. Currently these explanations are speculative and need further investigation.
With improved design and methodologies for defining cognitive impairment and using multiple domains of cognitive outcome measures, future studies should continue to focus on examining the potential of the program by incorporating incremental attention-demanding Tai Ji Quan-based motor tasks that tax the ability of older adults to perform exercises that involve quick recall of forms/movements, movement recognition, spatial orientation, movement switching/ordering, and movement retrieval. Implementation, however, should emphasize a slow progression and repetitive training approach in order to minimize negative learning and frustration that may arise among older adults due to the complex, multi-tasking training paradigm. These training features, when appropriately implemented, represent an improved approach that actively and concurrently engages cognitive and motor tasks that enhance cognitive functioning through dynamic Tai Ji Quan movements.
Given the preliminary nature of this study, several limitations should be noted. First, although the two groups were comparable on all baseline measures, participants were not randomized into the study conditions. Second, due to the use of a passive control condition, we are mindful of the potential influence of unequal between-group attention on our cognitive measure. It is possible that the participants in the active Tai Ji Quan group were benefiting from positive features that are inherent to group-based exercises (i.e., social interactions and attention from class instructors). Third, cognitive impairment was defined using the MMSE, a single general measure of cognitive function that has methodological limitations. However, for this initial work MMSE was chosen because it is the most widely used clinical short-screening measure for cognitive function due to its simplicity, ease of administration, and variety of cognitive domains assessed (orientation to space, short memory, registration, recall of immediate movement patterns, and ability to understand and follow instructions). A randomized controlled trial design using multiple cognitive outcomes that capture elicited change of Tai Ji Quan training in domains involving selective attention, working memory (e.g., semantic, procedural, episodic memories), and executive control (i.e., planning, organization, decision making, implementation) to enhance the clinical value of Tai Ji Quan on cognition should be conducted.
Bearing in mind the aforementioned limitations, the current study contributes to the paucity of research on the relationship between Tai Ji Quan and cognitive function in older adults with cognitive impairment. A notable strength of this study is the use of a program that has been extensively studied in terms of postural control and balance (Li et al., 2012; Li et al., 2013) and, as an evidence-based program for fall prevention among community-dwelling older adults, recommended for community implementation (CDC, 2010). Another strength of the study is that our training represents a new and substantive departure from the traditional generic application of Tai Ji Quan training to physical dysfunction by utilizing a unique multi-tasking protocol especially designed to counter the impact of neurodegenerative diseases, including balance, gait, and cognitive functioning. The findings of this study provide preliminary evidence suggesting the potential utility of our approach on improving cognition.
In conclusion, the results from this study have provided initial insight into the potential benefits of a specially tailored Tai Ji Quan training program in relation to cognitive function in older adults and are sufficiently provocative to warrant further investigation. A large-scale randomized trial with a clinical population of participants with cognitive impairment to determine whether the program would result in improved multidimensional clinical measures of cognitive function should be undertaken.
Acknowledgements
The work presented in this paper is supported by a research grant from the National Institute on Aging (AG034956).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement: No conflict of interest
Contributor Information
Fuzhong Li, Oregon Research Institute, Eugene, OR
Peter Harmer, Department of Exercise Science, Willamette University, Salem, OR.
Yu Liu, Laboratory of Exercise and Health Sciences, Shanghai University of Sport, Shanghai, China
Li-Shan Chou, Department of Human Physiology, University of Oregon, Eugene, OR 97403
References
- Alzheimer’s Disease Facts and Figures. Washington DC: Alzheimer’s Association; [Accessed August 2013]. Available at: http://www.alz.org. [Google Scholar]
- Aqqarwal NT, Wilson RS, Beck TL, Bienias JL, Bennett DA. Motor dysfunction in mild cognitive impairment and the risk of incident Alzheimer disease. Archives of Neurology. 2006;63(12):1763–1769. doi: 10.1001/archneur.63.12.1763. [DOI] [PubMed] [Google Scholar]
- Baker LD, Frank LL, Foster-Schubert K, Green PS, Wilkinson CW, McTiernan, et al. Effects of aerobic exercise on mild cognitive impairment: A controlled trial. Archives of Neurology. 2010;67(1):71–79. doi: 10.1001/archneurol.2009.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgener SC, Yang Y, Gilbert R, Marsh-Yant S. The effects of a multimodal intervention on outcomes of persons with early-stage dementia. American Journal of Alzheimer’s Disease and Other Dementia. 2008;23(4):382–394. doi: 10.1177/1533317508317527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Accessed November 15, 2013];A CDC compendium of effective fall interventions: What works for community-dwelling older adults. 2010 Available at: http://www.cdc.gov/HomeandRecreationalSafety/pdf/CDC_Falls_Compendium_lowres.pdf.
- Chang Y-K, Nien YH, Tsai CL, Etnier JL. Physical activity and cognition in older adults: The potential of Tai Chi Chuan. Journal of Aging and Physical Activity. 2010;18:451–472. doi: 10.1123/japa.18.4.451. [DOI] [PubMed] [Google Scholar]
- Chang Y-K, Pan CY, Chen FT, Tsai CL, Huang CC. Effect of resistance-exercise training on cognitive function in healthy older adults: A review. Journal of Aging and Physical Activity. 2012;20:497–517. doi: 10.1123/japa.20.4.497. [DOI] [PubMed] [Google Scholar]
- Chang J, Tsai P-F, Beck C, Hagen J, Cooley D, Anand K, Roberson P, Rosengren K, Beuscher L. The effects of Tai Chi on cognition in elders with cognitive impairment. Medsurg Nursing. 2011;20(2):63–70. [PMC free article] [PubMed] [Google Scholar]
- Cheng S-T, Chow P, Song Y-Q, Yu E, Chan A, Lee T, Lam J. Mental and physical activities delay cognitive decline in older persons with dementia. American Journal of Geriatric Psychiatry. 2013 doi: 10.1016/j.jagp.2013.01.060. e-pub ahead of print: [DOI] [PubMed] [Google Scholar]
- Curlik DM, Shors T. Training your brain: Do mental and physical (MAP) training enhance cognition through the process of neurogenesis in the hippocampus? Neuropharmacology. 2013;64:506–514. doi: 10.1016/j.neuropharm.2012.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dresler M, Sandberg A, Ohla K, Bublitz C, Trenado C, Mroczko-Wasowicz A, Kuhn S, Repantis D. Non-pharmacological cognitive enhancement. Neuropharmacology. 2013;64:529–543. doi: 10.1016/j.neuropharm.2012.07.002. [DOI] [PubMed] [Google Scholar]
- Erickson KI, Kramer AF. Aerobic exercise effects on cognitive and neural plasticity in older adults. British Journal of Sports Medicine. 2009;43(1):22–24. doi: 10.1136/bjsm.2008.052498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etnier JL, Chang YK. The effect of physical activity on executive function: A brief commentary on definitions, measurement issues, and the current state of the literature. Journal of Sport Exercise Psychology. 2009;31(4):469–483. doi: 10.1123/jsep.31.4.469. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-Mental State: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatrics Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR, Fanjiang G. Mini-Mental State Examination user’s guide. Odessa, FL: Psychological Assessment Resources; 2001. [Google Scholar]
- Hahn EA, Andel R. Nonpharmacological therapies for behavioral and cognitive symptoms of mild cognitive impairment. Journal of Aging Health. 2011;23(8):1223–1245. doi: 10.1177/0898264311422745. [DOI] [PubMed] [Google Scholar]
- Hanninen T, Hallikainen M, Tuomainen S, Vanhanen M, Soininen H. Prevalence of mild cognitive impairment: A population-based study in elderly subjects. Acta Neurologica Scandinavica. 2002;106:148–154. doi: 10.1034/j.1600-0404.2002.01225.x. [DOI] [PubMed] [Google Scholar]
- Lam LCW, Chau RCM, Wong BML, Fung AWT, Tam CWC, et al. A 1-year randomized controlled trial comparing mind body exercise (Tai Chi) with stretching and toning exercise on cognitive function in older Chinese adults at risk of cognitive decline. Journal of the American Medical Directors Association. 2012;13(6):568–573. doi: 10.1016/j.jamda.2012.03.008. [DOI] [PubMed] [Google Scholar]
- Larson EB, Wang L, Bowen JD, McCormick WC, Teri L, Crane P, et al. Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Annals of Internal Medicine. 2006;144(2):73–81. doi: 10.7326/0003-4819-144-2-200601170-00004. [DOI] [PubMed] [Google Scholar]
- Lautenschlager NT, Cox KL, Flicker L, et al. Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease: A randomized trial. Journal of American Medical Association. 2008;300:1027–1037. doi: 10.1001/jama.300.9.1027. [DOI] [PubMed] [Google Scholar]
- Maki Y, Ura C, Yamaguchi T, et al. Effects of intervention using a community-based walking program for prevention of mental decline: A randomized controlled trial. Journal of American Geriatrics Society. 2012;60:505–510. doi: 10.1111/j.1532-5415.2011.03838.x. [DOI] [PubMed] [Google Scholar]
- Li F. Transforming traditional Tai Ji Quan techniques into integrative movement therapy: Tai Ji Quan: Moving for Better Balance. Journal of Sport and Health Science. doi: 10.1016/j.jshs.2013.11.002. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Harmer P, Glasgow R, Mack KA, Sleet D, Fisher KJ, et al. Translation of an effective Tai Chi intervention into a community-based falls prevention program. American Journal of Public Health. 2008;98(7):1195–1198. doi: 10.2105/AJPH.2007.120402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Harmer P, Fitzgerald K, Eckstrom E, Stock R, Galver J, et al. Tai Chi and postural stability in patients with Parkinson’s disease. New England Journal of Medicine. 2012;366:511–519. doi: 10.1056/NEJMoa1107911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Harmer P, Fitzgerald K, Stevens J, Gladieux M, Chou L-S, et al. Implementing an evidence-based fall prevention program in an outpatient clinical setting. Journal of American Geriatrics Society. 2013 doi: 10.1111/jgs.12509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez OL, Jagust WJ, DeKosky ST, Becker JT, Fitzpatrick A, Dullberg C, et al. Prevalence and classification of mild cognitive impairment in the Cardiovascular Health Study Cognitive Study. Archives of Neurology. 2003;60:1385–1389. doi: 10.1001/archneur.60.10.1385. [DOI] [PubMed] [Google Scholar]
- Manly JJ, Tang MX, Schupf N, Stern Y, Vonsattel JP, Mayeux R. Frequency and course of mild cognitive impairment in a multiethnic community. Annals of Neurology. 2008;63:493–506. doi: 10.1002/ana.21326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortimer JA, Ding D, Borenstein AR, DeCarli C, Guo Q, Wu Y, et al. Changes in brain volume and cognition in a randomized trial of exercise and social interaction in a community-based sample of non-demented Chinese elders. Journal of Alzheimers Disorders. 2012;30:757–766. doi: 10.3233/JAD-2012-120079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mungas D. In-office mental status testing: A practical guide. Geriatrics. 1991;46(7):54–88. [PubMed] [Google Scholar]
- O’Bryant SE, Humphreys JD, Smith GE, Ivnik RJ, Graff-Radford NR, Petersen RC, Lucas JA. Detecting dementia with the Mini-Mental State Examination (MMSE) in highly educated individuals. Archives of Neurology. 2008;65(7):963–967. doi: 10.1001/archneur.65.7.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plassman BL, Langa KM, Fisher GG, et al. Prevalence of cognitive impairment without dementia in the United States. Annals of Internal Medicine. 2008;148:427–434. doi: 10.7326/0003-4819-148-6-200803180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsiadlo D, Richardson S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. Journal of American Geriatrics Society. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. Journal of Gerontology: Medical Science. 2005;50:M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- Reuben DB, Siu AL. An objective measure of physical function of elderly outpatients: The Physical Performance Test. Journal of American Geriatrics Society. 1990;38:1105–1112. doi: 10.1111/j.1532-5415.1990.tb01373.x. [DOI] [PubMed] [Google Scholar]
- Roberts RO, Geda YE, Knopman DS, Cha RH, Pankratz VS, Boeve BF, et al. The Mayo Clinic Study of Aging: Design and Sampling, participation, baseline measures and sample characteristics. Neuroepidemiology. 2008;30:58–69. doi: 10.1159/000115751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spering CC, Hobson V, Lucas JA, Menon CV, Hall JR, O’Bryant SE. Diagnostic accuracy of the MMSE in detecting probable and possible Alzheimer’s disease in ethnically diverse highly educated individuals: An analysis of the NACC database. Journal of Gerontology: Medical Sciences. 2012;67(8):890–896. doi: 10.1093/gerona/gls006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor-Piliae RE, Newell KA, Cherin R, Lee MJ, King AC, Haskell WL. Effects of Tai Chi and Western exercise on physical and cognitive functioning in healthy community-dwelling older adults. Journal of Aging and Physical Activity. 2010;18(3):261–279. doi: 10.1123/japa.18.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDepartment of Health and Human Services. National plan to address Alzheimer’s disease. Washington DC: U.S. Department of Health and Human Services; 2012. [Google Scholar]
- Vertesi A, Lever JA, Molloy DW, Sanderson B, Tuttle I, Pokoradi L, Principi E. Standardized Mini-Mental State Examination. Use and interpretation. Canadian Family Physician. 2001;47:2018–2023. [PMC free article] [PubMed] [Google Scholar]
- Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): Development and evaluation. Journal of Clinical Epidemiology. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]