Abstract
The purpose of this study was to explore trajectories of recovery in patients with lower extremity joint replacements receiving post-acute rehabilitation. A retrospective cohort design was used to examine data from the Uniform Data System for Medical Rehabilitation for 7,434 patients with total knee replacement and 4,765 patients with total hip replacement who received rehabilitation from 2008–2010. Functional Independence Measure (FIM)™ instrument ratings were obtained at admission, discharge, and 80–180 days after discharge.
Random coefficient regression analyses using linear mixed models were used to estimate mean ratings for items within the four motor subscales (self-care, sphincter control, transfers, and locomotion) and the cognitive domain of the FIM instrument. Mean improvements at discharge for motor items ranged from 1.16 (95% confidence interval [CI]: 1.14, 1.19) to 2.69 (95% CI: 2.66, 2.71) points for sphincter control and locomotion, respectively. At follow-up mean motor improvements ranged from 2.17 (95% CI: 2.15, 2.20) to 4.06 (95% CI: 4.03, 4.06) points for sphincter control and locomotion, respectively. FIM cognition yielded smaller improvements: discharge = 0.47 (95% CI: 0.46, 0.48); follow-up = 0.83 (95% CI: 0.0.81, 0.0.84). Persons who were younger, female, non-Hispanic white, unmarried, with fewer comorbid conditions, and who received a total knee replacement demonstrated slightly higher functional motor ratings. Overall, patients with unilateral knee or hip replacement experienced substantial improvement in motor functioning both during and up to six months following inpatient rehabilitation.
Keywords: Joint Replacement, Orthopedics, Longitudinal Outcomes, Functional Performance
INTRODUCTION
Lower extremity joint replacement, including total hip replacement and total knee replacement, is the third most common impairment category among Medicare beneficiaries admitted to inpatient rehabilitation facilities (IRFs) in the United States.1 With the expanding number of older adults in the U.S. population, there will be an increased number of older persons with total hip and knee replacement receiving various forms of post-acute rehabilitation services in the coming decade.2
Patients with joint replacement receiving inpatient rehabilitation usually show substantial improvements in functional performance from admission to discharge.3–10 Unlike acute injuries or trauma, such as stroke or hip fracture, joint replacement is typically an elective procedure, where the patients expect to achieve better physical functioning following surgery and rehabilitation. Relatively few studies, however, have compared longer-term functional outcomes between total hip and total knee replacement patients following inpatient rehabilitation.11,12 Understanding patient characteristics and clinical factors associated with favorable and unfavorable outcome patterns is important as the setting for providing post-acute services changes with the introduction of accountable care organizations and bundled payment systems.13
The purpose of this study was to model the trajectories of functional outcomes in a national sample of patients admitted to rehabilitation facilities in the United States with primary diagnoses of unilateral hip or knee replacement. Functional assessments were obtained at admission, discharge, and 80–180 days following discharge. We hypothesized that, after controlling for covariates, patients with total hip and knee replacements would demonstrate improved functional outcomes at discharge and at three to six-month follow-up, and that improvement in functional outcomes would be similar for the two impairment groups.
MATERIAL AND METHODS
Data Source
This study was a secondary analysis of data submitted by rehabilitation facilities across the United States to the Uniform Data System for Medical Rehabilitation (UDSMR®). The UDSMR is the largest non-federal data registry in the U.S. containing both patient and facility level information submitted by individual facilities for reimbursement purposes.14 A subset of UDSMR facilities also collect follow-up data on patients via telephone interview at 80–180 days post discharge. For this study, we used data from patients in the UDSMR database with complete information related to functional status at admission, discharge and follow-up.
Study Sample
We included records for patients who received rehabilitation services between 2008 and 2010. Our cohort was limited to cases with a primary impairment of unilateral hip replacement (rehabilitation impairment category 08.51) or unilateral knee replacement (rehabilitation impairment category 08.61). These criteria resulted in an eligible study sample of 13,033 patient records. We excluded patients if this was not their initial rehabilitation stay (n=299); time since surgery was greater than 45 days (n=136); rehabilitation length of stay was greater than 45 days (n=1); or admission to IRFs was from non-acute settings (n=119). Also excluded were patients who died during their inpatient rehabilitation stay (n=46); were less than 18 years old (n=3); had experienced rehabilitation program interruption (n=46); or were not living in community settings prior to admission to IRFs (n=54). Records with missing information related to the living status of patients at discharge (living with someone vs. alone, n=130) were also excluded. These criteria resulted in a final study sample of 12,199 records, representing approximately 93% of the eligible records.
Independent Variable
Each patient’s joint replacement status was categorized as total knee replacement (TKR) or total hip replacement (THR) and indicated as admission, discharge or follow-up. Persons with total hip replacement served as the reference category for all analyses.
Dependent Variables
The dependent variables included the mean ratings for the self-care, sphincter control, transfer, and locomotion sub-scales of the motor domain of the Functional Independence Measure (FIM instrument). Self-care contains six items, transfer has three items, the sphincter control and locomotion sub-scales each contain two items. The FIM cognition domain includes five items. Performance on each item in the FIM instrument is rated on a scale of 1–7. Table 1 shows the level of functional independence that defines the numerical rating in terms of lassistance required. To facilitate interpretation and discussion functional recovery over time using the FIM instrument, Table 1 also shows how we defined three broad categories of independence (high, medium, and low) representing clinically meaningful transitions. Assessments of functional status were conducted at admission, discharge, and 80–180 days following discharge. Admission and discharge data collection occurred in the facilities and were done by staff credentialed by the UDSMR. The follow-up ratings were obtained through telephone interviews by trained clinical staff. The validity and reliability of the FIM instrument, including data collection by phone interview, are well established.15–17
Table 1.
Functional Performance Criteria* for Rating Individual FIM Instrument items.
| Rating | Performance Criteria | Category |
|---|---|---|
| 7 | Complete independence (timely, safely) | High |
| 6 | Modified independence (device) | |
| 5 | Supervision (subject = 100%) | Medium |
| 4 | Minimal assistance (subject ≥ 75% | |
| 3 | Moderate assistance (subject ≥ 50%) | Low |
| 2 | Maximal assistance (subject ≥ 25%) | |
| 1 | Total assistance (subject < 25%) | |
Adapted from the Inpatient Rehabilitation Facility-Patient Assessment Instrument (IRF-PAI) available on Centers for Medicare and Medicaid Services website: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS/IRFPAI.html
Dashed lines indicate thresholds we used in creating broader categories (low, mid, high) of functional independence to facilitate interpretation and discussion of clinically meaningful transitions.
Covariates
Sociodemographic variables included age in years (categorized as < 65, 65–75, 75–85, and > 85); gender; race/ethnicity (white or nonwhite); marital status (married versus not married); length of stay was the total number of days spent in the medical rehabilitation unit or hospital. Length of follow-up was the number of days between discharge and the next reassessment of functional independence. Number of comorbid conditions (comorbid sum) was calculated as the total number of comorbidities reported for each patient (range: 0–10).
Data Analysis
Sociodemographic and clinical characteristics at admission and mean ratings for individual items within each of four functional subscales of the FIM motor subscales and FIM cognition domain over time were stratified by joint replacement status and examined through descriptive statistics. Comparisons across joint replacement status and patient characteristics were evaluated using chi-square tests and t-tests for categorical and continuous variables, respectively. Repeated-measures analysis of variance and post-hoc tests were applied to mean item ratings for all five functional measures.
To account for the repeated assessments within each patient and variation among patients, random coefficient regression analyses (linear mixed models) were used to estimate mean ratings for individual items within the four motor subscales (self-care, sphincter control, transfers, and locomotion) and for the cognitive domain. Because the correlation of mean ratings between admission and discharge was higher than between admission and follow-up, AR (1) (autoregressive process with order 1) was specified as the covariance structure within patients. A model including a time-level variable was constructed to reflect the changes in mean ratings over time. Basic sociodemographic factors, including age, race/ethnicity, gender, and marital status were added to the model. Number of comorbid conditions was included as a clinical status variable.
All analyses were conducted using SAS for Windows, version 9.2 (SAS Institute, Inc., Cary, NC).
RESULTS
The final sample included records for 12,199 patients representing approximately 93% of the eligible cases described above in Study Sample. The sample of patients in the UDSMR dataset with follow-up information was similar to the total UDSMR sample of patients with lower extremity joint replacement. Demographic and clinical information for the sample with follow-up data included the following; mean age of 71.3 (sd 11.4) years, 31.7% male, 82.5% white; 49.6% married; and 35% lived alone. The mean number of comorbidities was 7.6 (sd 2.6) and the mean length of stay was 8.7 (sd 3.8). For persons with lower extremity joint replacements without follow-up information the mean age was 70.5 (sd 11.4) years; 30.9% were male; 79.0% white; 48.7% married; and 33.6% lived alone. The mean number of comorbidities was 7.5 (sd 2.6) and the mean length of stay was 9.4 (sd 3.9).
Sociodemographic, clinic characteristics and mean ratings for individual items within the FIM motor subscales and FIM cognition domain over time are presented in Table 2 according to the joint level (total hip or total knee). Approximately 60% of patients had total knee replacement. In unadjusted analyses, patients with total knee replacement were significantly (p < .0001) more likely to be younger, nonwhite, and female and to experience shorter lengths of stay in rehabilitation than patients with total hip replacement. With one exception, patients with total knee replacement demonstrated higher functional independence on the four FIM motor subscales at all three assessments: there were no significant differences between patients with total knee and total hip replacement in locomotion ratings at admission. There was a statistically significant time effect (p < 0.001) observed across the four FIM motor subscales.
Table 2.
Patient Characteristics and Functional Ratings over time Stratified by Joint Replacement Status (categorical variable as %, continuous variables as M, sd).
| Joint Replacement |
||||
|---|---|---|---|---|
| Total | Knee | Hip | P value | |
| N | 12,199 | 7,434 | 4,765 | |
| Age in years | 71.3 (11.4) | 71.3 (10.6) | 71.3 (12.4) | < .001 |
| < 65 | 25.2% | 24.8% | 25.7% | |
| 65 – 75 | 31.2% | 33.0% | 28.4% | |
| 75 – 85 | 34.7% | 34.2% | 35.6% | |
| > 85 | 8.9% | 8.0% | 10.3% | |
| Male | 31.7% | 29.2% | 35.7% | < .001 |
| White | 82.5% | 80.5% | 85.6% | < .001 |
| Married | 49.6% | 50.1% | 48.9% | .187 |
| Living status | .273 | |||
| Alone | 35.0% | 34.7% | 35.6% | |
| With others | 65.0% | 65.3% | 64.4% | |
| Comorbid sum | 7.6 (2.6) | 7.7 (2.6) | 7.5 (2.7) | .006 |
| Length of stay, days | 8.7 (3.8) | 8.4 (3.7) | 9.1 (4.0) | < .001 |
| Length of follow-up, days | 107.4 (25.6) | 107.2 (25.3) | 107.7 (26.1) | .338 |
| FIM motor mean item scores+ | ||||
| Self-care + | < .001 | |||
| Admission | 4.1 (0.8) | 4.2 (0.8) | 4.0 (0.8) | < .001 |
| Discharge | 5.8 (0.7) | 5.8 (0.7) | 5.7 (0.7) | < .001 |
| Follow-up * | 6.7 (0.6) | 6.7 (0.5) | 6.6 (0.6) | < .001 |
| Sphincter control+ | < .001 | |||
| Admission | 4.5 (1.5) | 4.6 (1.5) | 4.5 (1.5) | < .001 |
| Discharge | 5.7 (1.1) | 5.7 (1.1) | 5.6 (1.1) | < .001 |
| Follow-up * | 6.7 (0.6) | 6.7 (0.6) | 6.7 (0.7) | .009 |
| Transfer+ | < .001 | |||
| Admission | 2.95 (0.9) | 2.99 (0.9) | 2.89 (0.9) | < .001 |
| Discharge | 5.07 (1.0) | 5.12 (0.9) | 4.98 (1.0) | < .001 |
| Follow-up * | 6.39 (0.7) | 6.42 (0.7) | 6.33 (0.7) | < .001 |
| Locomotion+ | < .001 | |||
| Admission | 1.6 (0.76) | 1.6 (0.75) | 1.6 (0.8) | .552 |
| Discharge | 4.2 (1.36) | 4.3 (1.33) | 4.1 (1.4) | < .001 |
| Follow-up * | 5.6 (1.31) | 5.7 (1.28) | 5.5 (1.4) | < .001 |
| FIM cognition mean item scores + | .102 | |||
| Admission | 5.9 (1.0) | 6.0 (1.0) | 5.9 (1.0) | .034 |
| Discharge | 6.4 (0.7) | 6.4 (0.7) | 6.4 (0.7) | .256 |
| Follow-up * | 6.8 (0.5) | 6.8 (0.4) | 6.8 (0.5) | .859 |
Note:
the corresponding statistics are computed based on N = 10,680
Values are mean ratings from individual items within each subscale
Table 3 presents the estimated regression coefficients (b) and 95% confidence intervals for the joint level (knee vs. hip) and all covariates related to mean ratings on each FIM motor subscale and on the FIM cognition domain. Given the reference categories for the categorical variables and that the sum of comorbid conditions variable was grand-mean centered, the intercepts represent the estimated admission-FIM item ratings for a patient with total hip replacement who is < 65 years old, white, female, unmarried and has nearly 8 comorbid conditions. Locomotion scores were substantially lower than all other subscale scores at admission. Joint level had small but statistically significant effects across all 4 FIM motor scales with higher values for persons with knee replacement. Joint level was not significantly associated with mean ratings on FIM cognition items. The time effect (admission, discharge, and follow-up) produced the largest coefficients in all five functional outcomes. Both the rate and magnitude of improvements in functional independence were greatest from admission to discharge. The models also show that patients with joint replacement, on average, continued to gain functional independence over the three plus months following discharge.
Table 3.
Results of Random Coefficient Regression Analyses on Modeling Mean Ratings for Individual Items within FIM Subscales.
| FIM motor | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Self-care | Sphincter control | Transfer | Locomotion | FIM cognition | ||||||
| b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | b | 95% CI | |
| Intercept | 4.13 | 4.11, 4.16 | 4.70 | 4.66, 4.74 | 3.02 | 2.99, 3.05 | 1.51 | 1.47, 1.55 | 6.10 | 6.07, 6.13 |
| Knee | 0.13 | 0.11, 0.15 | 0.08 | 0.05, 0.11 | 0.11 | 0.09, 0.13 | 0.13 | 0.10, 0.16 | 0.02 | −0.01, 0.04 |
| Time (ref: Admission) | ref | ref | ref | ref | ref | |||||
| Discharge | 1.69 | 1.68, 1.70 | 1.16 | 1.14, 1.19 | 2.11 | 2.10, 2.13 | 2.69 | 2.66, 2.71 | 0.47 | 0.46, 0.48 |
| Follow-up | 2.59 | 2.58, 2.61 | 2.17 | 2.15, 2.20 | 3.43 | 3.41, 3.45 | 4.06 | 4.03, 4.09 | 0.83 | 0.81, 0.84 |
| Age (ref: < 65) | ref | ref | ref | ref | ref | |||||
| 65–75 | −0.02 | −0.04, 0.01 | −0.07 | −0.11, −0.03 | −0.03 | −0.06, −0.00 | 0.03 | −0.01, 0.07 | −0.07 | −0.10, −0.04 |
| 75–85 | −0.15 | −0.18, −0.13 | −0.25 | −0.29, −0.21 | −0.18 | −0.21, −0.15 | −0.14 | −0.18, −0.10 | −0.24 | −0.27, −0.21 |
| > 85 | −0.32 | −0.36, −0.28 | −0.42 | −0.48, −0.37 | −0.32 | −0.36, −0.28 | −0.30 | −0.35, −0.24 | −0.43 | −0.48, −0.39 |
| Minority | −0.06 | −0.09, −0.04 | −0.18 | −0.22, −0.14 | −0.07 | −0.10, −0.04 | −0.08 | −0.12, −0.04 | −0.03 | −0.06, −0.00 |
| Male | −0.02 | −0.04, −0.00 | −0.13 | −0.16, −0.09 | −0.00 | −0.03, 0.02 | 0.13 | 0.10, 0.16 | −0.08 | −0.11, −0.06 |
| Married | −0.03 | −0.05, −0.01 | −0.01 | −0.04, 0.02 | −0.03 | −0.05, −0.00 | 0.004 | −0.02, 0.03 | 0.01 | −0.01, 0.04 |
| Comorbid sum | −0.01 | −0.02, −0.01 | −0.03 | −0.04, −0.03 | −0.02 | −0.02, −0.01 | −0.06 | −0.07, −0.06 | −0.03 | −0.04, −0.03 |
Note: Reference categories for dichotomous variables are as follows: knee (hip), minority (white), male (female), married (unmarried). Bolded values indicate parameter estimates are statistically significant at the significance level.
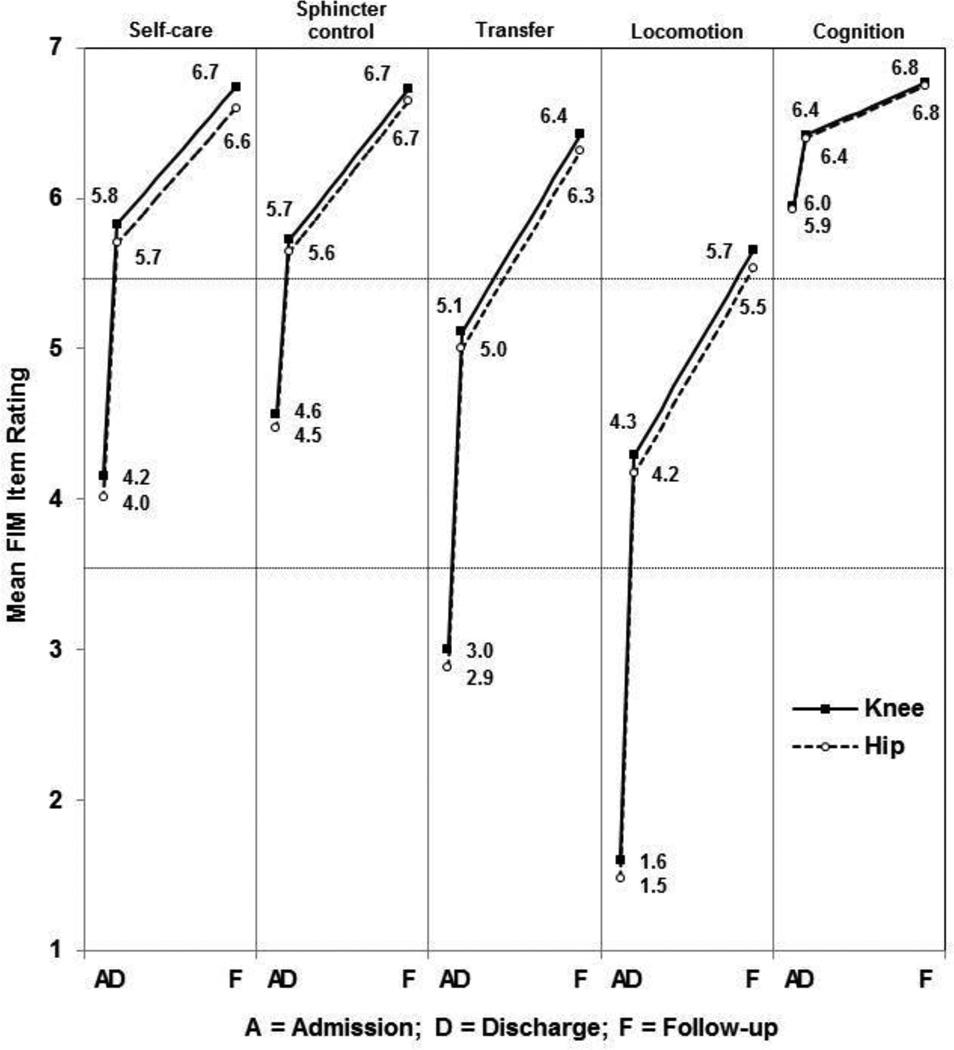
A profile plot (Figure 1) was computed to display the trends in adjusted mean ratings over time for each subscale of the FIM motor domain and FIM cognition domain. The figure shows the progression of functional independence from low to medium to high for the mean item ratings of the four motor scales. The mean item ratings for the cognitive domain show relatively little change from admission to follow-up.
Figure 1.
Mean plot of the adjusted mean ratings for individual items within the FIM instrument by joint replacement status during and after rehabilitation services according to the adjusted models shown in Table 2. Ratings for individual items, 1 (total assistance), 2 (maximal assistance), and 3 (moderate assistance), are indexed as low independence; 4 (minimal assistance) and 5 (supervision) are indexed as medium independence; 6 (modified independence) and 7 (complete independence) are indexed as high independence.
DISCUSSION
Our goal was to examine differences between functional outcomes in persons with total knee and total hip replacements over the course of rehabilitation including admission, discharge and follow-up. Persons in both impairment groups experienced substantial improvements from admission to discharge. Although attenuated, significant functional status gains were also observed from discharge to follow-up. The ratings for the four FIM motor subscales and FIM cognition showed statistically significant (p < 0.05) increases from admission to discharge and from discharge to follow-up, with the motor scores demonstrating clinically meaningful improvements. The adjusted models (Table 3) suggest that patients who were younger, female, non-Hispanic white, unmarried, with fewer comorbid conditions, and who received a total knee replacement versus hip replacement demonstrated slightly higher functional ratings.
Assessing mean item ratings for each motor subscale in the framework of the FIM rating criteria allowed us to document temporal trends in domain-specific transitions to higher levels of independence: low → moderate → high. A unique contribution of our study is the identification of clinically meaningful improvements in the parallel trajectories in motor functioning experienced by both the patients receiving total knee and total hip replacements (Figure 1). Mean ratings for self-care and sphincter-control were in the middle of the moderate independence range at admission and improved to the lower limit of high independence by discharge. Continued improvement yielded group mean values near the upper limit of high independence at follow-up. Mean ratings for transfer and locomotion began in the low independence range at admission, progressed to moderate independence by discharge, and ultimately reached high independence at follow-up (Figure 1).
Three related studies by DeJong and colleagues using data from six inpatient rehabilitation facilities provide context for the functional recovery patterns we observed in our sample. The rates and magnitudes of functional gains experienced during inpatient rehabilitation are consequences of both the relatively large potential for improvement immediately following surgery and the intensity of rehabilitation services the patients received during their stays. Both patients with knee and hip joint replacement averaged 2.7 hours of physical therapy or occupational therapy per day throughout their inpatient rehabilitation stays, with a majority of time spent on exercise and gait activities.19 The continued gains observed at follow-up remind us that discharge from inpatient rehabilitation does not mark the end of care or recovery for patients with joint replacements; 93% of patients with knee replacement and 87% of patients with hip replacements receive outpatient rehabilitation, home rehabilitation, or both following discharge.20 In the United States, the pattern of post-acute care for patients with lower extremity joint replacement is changing. These patients are receiving less treatment at inpatients in rehabilitation facilities and more often are referred to skilled nursing facilities, home health agencies or outpatient therapy. The impacts of these changes in service delivery on long-term functional outcomes are unknown. This is an important area for future research given the clinical and financial implications of bundled payments on service delivery patterns.13
As noted in the Introduction, joint replacement is typically an elective procedure. Following the procedure, patients expect to achieve better physical functioning. It is important to consider the high levels of independence observed at follow-up in our study from the perspective of patient expectations. DeJong et al.12 reported that 80% and 84% of patients with knee and hip replacement, respectively, felt their physical health was “somewhat” to “much better” 7.5 months after discharge from inpatient rehabilitation compared with before their replacement procedures.
The functional recovery experienced by patients with joint replacement exceeds the prognosis for patients with traumatic orthopedic conditions such as hip fracture, where up to 18–33% of patients die within 1 year and as many as 75% of patients who were independent prior to their injury are unable to walk independently or return to their pre-injury living setting 1 year later.21
Limitations
Our investigation has limitations. We did not have information on pre-surgical functional status so we cannot comment on recovery of function relative to pre-hospitalization levels of independence. We also did not have information on the type or intensity of outpatient therapy a person received following discharge from inpatient rehabilitation. Follow-up functional status was obtained by self-report and may be subject to recall or reporting bias. The validity and reliability of self-reported FIM ratings collected by trained telephone interviewers have been examined by independent investigators and found to be adequate.16,17 Our study also has several strengths. Recent reports from the American Joint Replacement Registry indicate that approximately 60% of joint replacement procedures are for the knee compared with 40% for the hip.18 These values are consistent with our findings.
Studies of rehabilitation outcomes using follow-up data from a large national sample are rare. The majority of follow-up studies in medical rehabilitation are based on small samples from one or two facilities. Our results provide longitudinal information for a large sample of patients who represent an important group of rehabilitation consumers. The size of the sample allowed us to use linear mixed models to help account for repeated measurements across individual patients and more accurately model longitudinal outcomes related to function.
CONCLUSION
Patients with unilateral total hip and total knee replacements demonstrated substantial improvements in motor functioning during inpatient rehabilitation. Both groups showed continued improvement at follow-up. At 3 to 6 months after discharge, mean ratings on all four motor subscales were above the level requiring assistance from another person based on the FIM instrument scoring criteria.14 Additional research is needed to explore the trajectories of change in function following discharge from inpatient medical rehabilitation in other impairment groups as the Affordable Care Act is implemented and the venues for post-acute care expand.
Acknowledgments
Acknowledgments/Disclosures
Supported in part by a grant from the Eunice Kennedy Shriver Institute for Child Health and Human Development and the National Institute of Neurological Disease and Stroke (R24 HD065702, K. Ottenbacher, J. Graham, and A. Karmarkar).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
No conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
REFERENCES
- 1.Medicare Payment Advisory Commission (MedPAC) Report to the Congress: Medicare Payment Policy. Washington, DC: 2012. [Google Scholar]
- 2.The United States Bone and Joint Decade (USBJD) The Burden of Musculoskeletal Diseases in the United States: Prevalence, Societal and Economic Cost. Rosemont, IL: 2008. [Google Scholar]
- 3.Vincent KR, Vincent HK, Lee LW, Alfano AP. Outcomes in total knee arthroplasty patients after inpatient rehabilitation: influence of age and gender. Am J Phys Med Rehabil. 2006;85:482–489. doi: 10.1097/01.phm.0000219151.18749.50. [DOI] [PubMed] [Google Scholar]
- 4.Lieberman D, Friger M. Inpatient rehabilitation outcome after hip fracture surgery in elderly patients: a prospective cohort study of 946 patients. Arch Phys Med Rehabil. 2006;87:167–171. doi: 10.1016/j.apmr.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Vincent HK, Vincent KR. Influence of admission hematocrit on inpatient rehabilitation outcomes after total knee and hip arthroplasty. Am J Phys Med Rehabil. 2007;86:806–817. doi: 10.1097/PHM.0b013e318151fe19. [DOI] [PubMed] [Google Scholar]
- 6.Khan F, Ng L, Gonzalez S, Hale T, Turner-Stokes L. Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy. Cochrane Database Syst Rev. 2008:CD004957. doi: 10.1002/14651858.CD004957.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahomed NN, Davis AM, Hawker G, et al. Inpatient compared with home-based rehabilitation following primary unilateral total hip or knee replacement: a randomized controlled trial. J Bone Joint Surg Am. 2008;90:1673–1680. doi: 10.2106/JBJS.G.01108. [DOI] [PubMed] [Google Scholar]
- 8.Johanson MA, Cohen BA, Snyder KH, McKinley AJ, Scott ML. Outcomes for aging adults following total hip arthroplasty in an acute rehabilitation facility versus a subacute rehabilitation facility: a pilot study. J Geriatr Phys Ther. 2009;32:73–78. [PubMed] [Google Scholar]
- 9.Herbold JA, Bonistall K, Walsh MB. Rehabilitation following total knee replacement, total hip replacement, and hip fracture: a case-controlled comparison. J Geriatr Phys Ther. 2011;34:155–160. doi: 10.1519/JPT.0b013e318216db81. [DOI] [PubMed] [Google Scholar]
- 10.Tian W, DeJong G, Horn SD, Putman K, Hsieh CH, DaVanzo JE. Efficient rehabilitation care for joint replacement patients: skilled nursing facility or inpatient rehabilitation facility? Med Decis Making. 2012;32:176–187. doi: 10.1177/0272989X11403488. [DOI] [PubMed] [Google Scholar]
- 11.Buntin M, Partha D, Escarce J, Hoverman C, Paddock S, Sood N. Comparison of Medicare Spending and Outcomes for Beneficiaries with Lower Extremity Joint Replacements. Santa Monica, CA: RAND; 2005. [Google Scholar]
- 12.DeJong G, Tian W, Smout RJ, et al. Long-term outcomes of joint replacement rehabilitation patients discharged from skilled nursing and inpatient rehabilitation facilities. Arch Phys Med Rehabil. 2009;90:1306–1316. doi: 10.1016/j.apmr.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 13.Sood N, Huckfeldt PJ, Escarce JJ, Grabowski DC, Newhouse JP. Medicare's bundled payment pilot for acute and postacute care: analysis and recommendations on where to begin. Health Aff (Millwood) 2011;30:1708–1717. doi: 10.1377/hlthaff.2010.0394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Granger CV, Markello SJ, Graham JE, Deutsch A, Reistetter TA, Ottenbacher KJ. The uniform data system for medical rehabilitation: report of patients with lower limb joint replacement discharged from rehabilitation programs in 2000–2007. Am J Phys Med Rehabil. 2010;89:781–794. doi: 10.1097/PHM.0b013e3181f1c83a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77:1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 16.Segal ME, Gillard M, Schall R. Telephone and in-person proxy agreement between stroke patients and caregivers for the functional independence measure. Am J Phys Med Rehabil. 1996;75:208–212. doi: 10.1097/00002060-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Smith PM, Illig SB, Fiedler RC, Hamilton BB, Ottenbacher KJ. Intermodal agreement of follow-up telephone functional assessment using the Functional Independence Measure in patients with stroke. Arch Phys Med Rehabil. 1996;77:431–435. doi: 10.1016/s0003-9993(96)90029-5. [DOI] [PubMed] [Google Scholar]
- 18.American Joint Replacement Registry. Annual Report: 2011. Rosemont, IL: The American Academy of Orthopaedic Surgeons; 2011. [Google Scholar]
- 19.DeJong G, Hsieh CH, Gassaway J, et al. Characterizing rehabilitation services for patients with knee and hip replacement in skilled nursing facilities and inpatient rehabilitation facilities. Arch Phys Med Rehabil. 2009;90:1269–1283. doi: 10.1016/j.apmr.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 20.DeJong G, Tian W, Smout RJ, et al. Use of rehabilitation and other health care services by patients with joint replacement after discharge from skilled nursing and inpatient rehabilitation facilities. Arch Phys Med Rehabil. 2009;90:1297–1305. doi: 10.1016/j.apmr.2008.12.029. [DOI] [PubMed] [Google Scholar]
- 21.Magaziner J, Fredman L, Hawkes W, et al. Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community-dwelling aged. Am J Epidemiol. 2003;157:1023–1031. doi: 10.1093/aje/kwg081. [DOI] [PubMed] [Google Scholar]