Abstract
In patients with chronic liver diseases, identification of significant liver fibrosis and cirrhosis is essential for determining treatment strategies, assessing therapeutic response, and stratifying long-term prognosis. Although liver biopsy remains the reference standard for evaluating the extent of liver fibrosis in patients with chronic liver diseases, several non-invasive methods have been developed as alternatives to liver biopsies. Some of these non-invasive methods have demonstrated clinical accuracy for diagnosing significant fibrosis or cirrhosis in many cross-sectional studies with the histological fibrosis stage as a reference standard. However, non-invasive methods cannot be fully validated through cross-sectional studies since liver biopsy is not a perfect surrogate endpoint marker. Accordingly, recent studies have focused on assessing the performance of non-invasive methods through long-term, longitudinal, follow-up studies with solid clinical endpoints related to advanced stages of liver fibrosis and cirrhosis. As a result, current view is that these alternative methods can independently predict future cirrhosis-related complications, such as hepatic decompensation, liver failure, hepatocellular carcinoma, or liver-related death. The clinical role of non-invasive models seems to be shifting from a simple tool for predicting the extent of fibrosis to a surveillance tool for predicting future liver-related events. In this article, we will summarize recent longitudinal studies of non-invasive methods for predicting forthcoming complications related to liver cirrhosis and discuss the clinical value of currently available non-invasive methods based on evidence from the literature.
Keywords: Non-invasive model, Prediction, Cirrhosis, Complication, Liver-related events
Core tip: In this article, we summarized recent longitudinal studies of non-invasive methods - including transient elastography, European Liver Fibrosis scoring system, Fibrotest, and acoustic radiation force impulse technique - for predicting forthcoming complications related to liver cirrhosis. We also discussed the clinical value of currently available non-invasive methods based on evidence from the literature and finally proposed areas for future research directions.
INTRODUCTION
Viral hepatitis accounts for the majority of chronic liver diseases (CLDs) worldwide[1-4]. In the absence of appropriate therapeutic interventions, CLD can progress to significant liver fibrosis or cirrhosis, resulting in complications, such as portal hypertension, ascites, or hepatocellular carcinoma (HCC)[5-7]. In recent years, secondary prevention of CLD progression to significant liver fibrosis or cirrhosis has been quite successful due to the development and application of antiviral therapies. However, liver-related events (LREs), especially cirrhosis-related complications, occur despite appropriate management with antiviral treatments. These LREs are clinically important and abruptly change the prognosis of patients with CLD.
Therefore, the identification of significant liver fibrosis and cirrhosis is essential for determining treatment strategies, assessing therapeutic response, and stratifying long-term prognosis based on the risk of developing LREs. For evaluating the extent of liver fibrosis, liver biopsy remains the reference standard. However, liver biopsies are often considered “imperfect” surrogate markers for liver fibrosis because of inherent limitations, including invasiveness, risk of life-threatening complications, intra- and inter-observer variability, and sampling error[8-11]. Moreover, monitoring the extent of liver fibrosis through serial liver biopsies during antiviral or anti-fibrotic treatments is not feasible in practice.
Accordingly, several non-invasive methods have been developed as alternatives to liver biopsies for evaluating the extent of liver fibrosis in patients with CLDs. Alternative approaches include measuring serum hyaluronic acid levels, the ratio of aspartate aminotransferase (AST) to alanine aminotransferase (ALT), AST-to-platelet ratio index (APRI), age-spleen-platelet ratio index (ASPRI), Fibrosis-4 (FIB-4), Forns’ index, Fibrotest (FT), FIBROSpect, Hepascore, Lok index, European Liver Fibrosis (ELF) panel scoring system, and transient elastography (TE, FibroScan®)[12-25]. The diagnostic performance of these non-invasive methods has been assessed in many cross-sectional studies by comparing the area-under-the-receiver operating curves (AUROCs) for these methods with the histological fibrosis stage as a reference standard. Accordingly, some of these tools have demonstrated clinical accuracy for diagnosing significant fibrosis or cirrhosis and have provided reproducible and reliable results[26-30].
However, liver biopsy is not a perfect surrogate endpoint marker for the aforementioned reasons. Thus, non-invasive methods cannot be fully validated through cross-sectional studies[31]. Recent studies have focused on assessing the performance of non-invasive methods through long-term, longitudinal, follow-up studies with solid clinical endpoints related to advanced stages of liver fibrosis and cirrhosis, including liver failure, hepatic decompensation, development of HCC, and/or liver-related death. These longitudinal studies do more than simply comparing the AUROCs with an imperfect histological reference. They also help to establish the clinical importance of non-invasive methods, including prediction of long-term prognosis[31,32]. Recent studies suggest that serial assessments of non-invasive methods reflect changes in the risk of developing LREs in patients with CLD[33]. Thus, non-invasive methods are proposed to be valuable tools for monitoring changes in prognosis, which cannot be assessed with a liver biopsy.
In this article, we will summarize recent longitudinal studies of non-invasive methods for predicting forthcoming complications related to liver cirrhosis, such as hepatic decompensation, liver failure, development of HCC, or liver-related death. We will also discuss the clinical value of currently available non-invasive methods based on evidence from the literature. Finally, we will discuss future research directions.
TRANSIENT ELASTOGRAPHY
Measurement of liver stiffness (LS) by TE has been proposed as a new non-invasive method for assessing the degree of liver fibrosis. The ability of TE to predict development of cirrhosis-related complications has also been explored in several prospective, longitudinal studies (Table 1).
Table 1.
Description of prognostic studies assessing non-invasive tools for the prediction of forthcoming cirrhosis-related complications
| Ref. | Etiology of liver disease | n | Assessment modality1 | Endpoint | AUROC |
| Kim et al[45] | LC (HBV) | 577 | LSPS | Esophageal variceal bleeding | 0.929 |
| Berzigotti et al[46] | LC (mostly HCV) | 117 (T)/56 (V) | LSPS, platelet count, spleen diameter, LS | Esophageal varices | 0.882 (T), 0.808 (V) |
| Clinically significant portal hypertension | 0.918 (T), 0.906 (V) | ||||
| Masuzaki et al[49] | CLD (HCV) | 866 | LS | Hepatocellular carcinoma | N/A |
| Jung et al[33] | LC (HBV) | 1130 | LS | Hepatocellular carcinoma | N/A |
| Kim et al[50] | LC (HBV) | 217 | LS, LSPS | Hepatic decompensation | 0.773 (LS); 0.790 (LSPS) |
| Kim et al[51] | CLD (HBV) | 128 | LS | Liver-related events | 0.772 |
| Chon et al[52] | CLD (HBV) | 1126 | LS, LSPS, | Hepatocellular carcinoma | 0.789 (LS); 0.790 (LSPS) |
| ASPRI, P2/MS, FIB-4 | Hepatic decompensation | 0.820 (LS); 0.848 (LSPS) | |||
| Kim et al[53] | CLD (HBV) on antiviral therapy | 162 | LS | Liver-related events | 0.736 |
| Kim et al[54] | LC (HBV) on antiviral therapy | 103 | LS | Liver-related events | N/A |
| Singh et al[56]2 | CLD (various) | 7058 | LS | Liver-related events | N/A |
| Parkes et al[58] | CLD (various) | 457 | ELF | Liver-related events | 0.82 |
| Kim et al[62] | CLD (HBV) | 170 | ELF | Liver-related events | 0.808 |
| Vergniol et al[66] | CLD (HCV) | 1457 | FT, LS, APRI, FIB-4, LB | Overall survival (5-yr) | 0.861 (FT) |
| de Ledinghen et al[67] | CLD (HBV) | 600 | FT, LS, APRI, FIB-4, LB | Overall survival (5-yr) | 0.82 (FT) |
| Park et al[68] | CLD (HBV) | 151 | FT, LS, FT + LS, FT × LS, LB | Liver-related events | 0.748 (FT + LS); 0.868 (FT × LS) |
| Morishita et al[77]3 | LC (HCV) | 135 | ARFI (LS) | Esophageal varices (high-risk) | 0.890 (0.868) |
| Takuma et al[78]3 | LC (mostly HCV) | 340 | ARFI (SS, LS) | Esophageal varices (high-risk) | 0.993 (0.930) |
Bold face denotes main assessment modality;
Meta-analysis;
Cross-sectional study. AUROC: Area-under-the-receiver-operating curve; LC: Liver cirrhosis; CLD: Chronic liver disease; HBV: Hepatitis B virus; HCV: Hepatitis C virus; T: Training set; V: Validation set; LSPS: Liver stiffness-spleen diameter to platelet ratio score; LS: Liver stiffness; ASPRI: Age-spleen-platelet ratio index; ELF: European Liver Fibrosis; FT: Fibrotest; APRI: Aspartate aminotransferase to platelet ratio index; ARFI: Acoustic radiation force impulse; SS: Spleen stiffness; N/A: Not available.
Gastroesophageal varices
An important cirrhosis-related complication is the development of gastroesophageal varices and bleeding. Gastroesophageal varices are present in 30%-60% of patients with liver cirrhosis. Variceal bleeding is an independent predictor of mortality[34-36]. Although several cross-sectional studies[37-42] have reported significant correlations between TE and the presence of esophageal varices (EVs) and/or EV bleeding, the performance of TE alone as a predictor of EVs is far from satisfactory. Thus, it has been suggested that TE alone cannot replace esophagogastroduodenoscopy for identifying patients with EVs[43]. A novel prediction model was recently introduced by Kim et al[44]. This model combines TE with different pathophysiological parameters of liver cirrhosis. The LS-spleen diameter to platelet ratio score (LSPS) combines the LS measurement obtained by TE with the spleen diameter measured by ultrasonography and the platelet count from a routine complete blood count. The LSPS has excellent accuracy for diagnosing and predicting high-risk EVs in patients with compensated hepatitis B virus-related CLD (AUROC = 0.953; negative predictive value 94.7%, positive predictive value 93.3%).
Based on a follow-up prospective, longitudinal study, Kim et al[45] concluded that LSPS is a reliable method for predicting variceal bleeding in hepatitis B virus-related liver cirrhosis. In this study, patients with LSPS ≥ 5.5 showed higher cumulative incidences of EV bleeding during the follow-up period. Among those with high-risk EVs, those with an LSPS ≥ 6.5 were at an increased risk of developing variceal bleeding (Figure 1).
Figure 1.
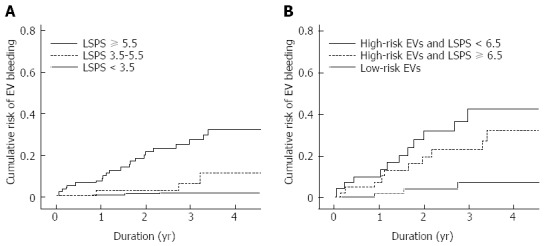
Cumulative incidence rate of variceal bleeding based on liver stiffness measurement-spleen diameter to platelet ratio score values. Reproduced with permission from Kim et al[45]. A: Among patients with liver cirrhosis related to hepatitis B virus, those with higher LSPS values had significantly higher cumulative incidences of bleeding from EVs during the follow-up period; n = 577; B: Among patients with high-risk EVs, patients with LSPS ≥ 6.5 had higher risks for variceal bleeding; n = 150. LSPS: Liver stiffness measurement-spleen diameter to platelet ratio score; EV: Esophageal varice.
The clinical significance of LSPS for predicting EVs in patients with compensated cirrhosis of different etiologies was further confirmed by Berzigotti et al[46]. In this European multi-center study, which included a training set of 117 patients and a validation set of 56 patients with compensated cirrhosis, LSPS showed good diagnostic performance for predicting the presence of EVs (AUROC = 0.882; negative predictive value 90.8%, positive predictive values 73.2%). Patients with LSPS ≥ 3.21 were considered to have EVs with an accuracy of 84.6% in the training set and 75.0% in the validation set. Interestingly, whereas the diagnostic performance of LSPS by AUROC was similar between the two studies[45,46], the cut-offs were different: 5.5 vs 3.21. The disparity between cut-offs is presumably due to differences in the etiologies of the CLDs. The original publication consisted of patients with hepatitis B virus-related liver cirrhosis only, whereas the latter study included patients with liver cirrhosis of various etiologies, mainly hepatitis C virus. The cross-sectional utility of LSPS demonstrated in Asian studies was validated in a European multicenter trial. However, similar to variceal bleeding, the utility of LSPS as a long-term prognostic factor should be validated through longitudinal, prospective studies performed by multiple investigators in patients of varying ethnicities and disease etiologies.
Hepatocellular carcinoma
Advanced liver fibrosis and cirrhosis are regarded as major risk factors for the development of HCC. Early detection of HCC is critical for successful treatment[47,48]. In addition to the clinical application of TE for diagnosing the extent of liver fibrosis and predicting the development of gastroesophageal varices and hepatic decompression, recent studies suggest that TE can predict the development of HCC. Masuzaki et al[49] performed a large, prospective cohort study to assess the ability of TE to predict the development of HCC among Japanese patients with hepatitis C-related liver cirrhosis. In addition to age, male gender, and clinical cirrhosis, the LS value stratified by TE was identified as an independent risk factor for developing HCC. Compared to patients with LS values ≤ 10 kPa, patients with higher LS values had a significantly increased risk of developing HCC (LS values, 10.1-15 kPa, HR = 16.7; LS values, 15.1-20 kPa, HR = 20.9; LS values, 20.1-25 kPa, HR = 25.6; and LS values > 25 kPa, HR = 45.5). In addition, the cumulative incidence of HCC increased in a step-wise manner according to the stratified LS value (Figure 2A). These findings suggested that a greater extent of liver fibrosis, as assessed by higher LS values, was closely associated with an increased risk of developing HCC. Thus, TE is a clinically useful method for predicting development of HCC.
Figure 2.
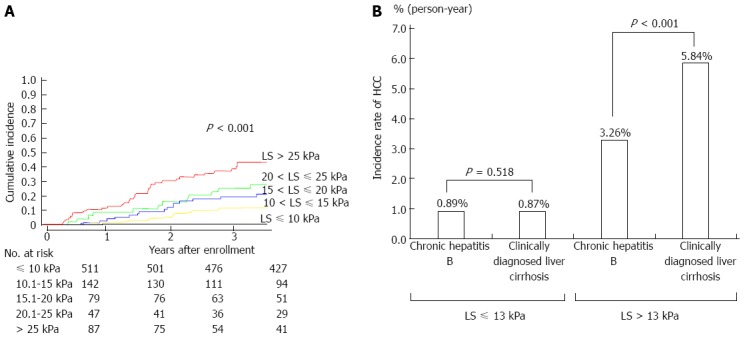
Cumulative incidence of hepatocellular carcinoma. A: The cumulative incidence of hepatocellular carcinoma (HCC) showed a step-wise increase according to the stratified liver stiffness (LS) measurement; n = 866. Reproduced with permission from Masuzaki et al[49]; B: Patients with higher LS values had significantly higher risks of developing HCC. Transient elastography (TE) and clinical criteria produced conflicting results for diagnosing liver cirrhosis. Patients diagnosed with liver cirrhosis based on TE findings were at higher risk of developing HCC than those diagnosed by clinical criteria (3.26% vs 0.87% per person-year); n = 1110. Reproduced with permission from Jung et al[33].
The clinical role of TE for predicting the development of HCC was further validated in patients with liver cirrhosis of different etiologies. Jung et al[33] conducted a study in Korean patients with chronic hepatitis B. In this large, prospective cohort study, a significant step-wise association was confirmed between LS values and the risk of developing HCC. Compared to patients with LS values ≤ 8 kPa, patients with higher LS values had significantly increased risks of developing HCC (LS values, 8.1-13 kPa, HR = 3.07; LS values, 13.1-18 kPa, HR = 4.68; LS values, 18.1-23 kPa, HR = 5.55; and LS values > 23 kPa, HR = 6.60). The diagnosis of liver cirrhosis may show conflicting results based on TE findings and clinical criteria. Patients diagnosed with liver cirrhosis based on TE findings showed increased risks of developing HCC than those diagnosed with liver cirrhosis based on clinical criteria (3.26% vs 0.87% per person-year) (Figure 2B). These findings indicate that TE might be a more precise indicator of compensated liver cirrhosis in comparison to clinical criteria. Furthermore, changes in the risk of developing HCC according to the pattern of changes in LS values were observed in the study. These data suggest that serial TE measurement may be a dynamic monitoring tool for estimating the risk of developing HCC in patients with liver cirrhosis.
These two large studies confirmed the clinical implications of TE as a non-invasive tool for assessing the risk of developing HCC. However, incorporation of TE into the routine surveillance strategy should be further investigated to determine if this increases the accuracy of detecting risk.
Hepatic decompensation and liver-related events
Development of overall hepatic decompensation, not merely variceal bleeding, is another critical factor related to morbidity in advanced stages of liver fibrosis and cirrhosis. Hence, early prediction of hepatic decompensation is important for establishing therapeutic plans. Kim et al[50] conducted a prospective, longitudinal study to assess the abilities of TE and LSPS to predict the first event of hepatic decompensation in patients with liver cirrhosis. The study included patients with cirrhosis related to hepatitis B virus without histories of hepatic decompensation, which was defined as a newly-developed ascites, hepatic encephalopathy, variceal bleeding, and/or deterioration of liver function to Child-Pugh class B or C. The risk of hepatic decompensation was stratified into three groups based on the LS or LSPS value. The results suggested that patients with higher LS values (13-18 and ≥ 18 kPa) had significantly higher risks of developing hepatic decompensation compared to those with lower values (< 13 kPa) (HR = 4.547, P = 0.044 and HR = 12.446, P < 0.001, respectively). Similarly, the risk of developing hepatic decompensation was increased in patients with higher LSPS values (1.1-2.5 and ≥ 2.5) compared to those with lower values (< 1.1) (HR = 5.796, P = 0.004 and HR = 13.618, P < 0.001, respectively).
Another study[51] investigated the potential role of TE for predicting the development of overall LREs in patients with hepatitis B virus-related CLD. Overall LREs included HCC, hepatic decompensation, and liver-related mortality. In this prospective study, 128 patients with chronic hepatitis B who were receiving antiviral therapy and had histologically-confirmed advanced liver fibrosis (≥ F3) and high viral loads (pre-treatment levels of HBV DNA ≥ 2000 IU/mL) were stratified into two groups based on the optimal cut-off (19 kPa). The patients with high LS values (≥ 19 kPa) had an increased risk of developing LREs compared with those who had lower LS values (< 19 kPa) (HR = 7.176; P = 0.001). The incidence of LREs in patients with F3 and F4 were not statistically different (22.2% vs 13.6%; P = 0.472). However, there was a significant difference in the incidence of LREs between patients with higher and lower LS values (44.4% in ≥ 19 kPa vs 6.9% in < 19 kPa; P < 0.001). These results suggest that TE has superior performance for predicting LREs compared to that of histology for predicting long-term prognosis.
The role of TE-based non-invasive tools for predicting development of cirrhosis-related events was also analyzed in another study[52]. In this prospective study, the LS values and LSPS showed good performance for predicting the development of HCC (AUROC, 0.789 for LS value, 0.788 for LSPS) and hepatic decompensation (AUROC, 0.820 for LS value, 0.848 for LSPS). Furthermore, the LS value and LSPS were identified as independent predictors of HCC (HR = 1.040 for LS value, 1.001 for LSPS) and hepatic decompensation (HR = 1.033 for LS value, 1.002 for LSPS).
Antiviral treatments are actively administered to patients with hepatitis B virus. It is important to understand if TE can predict the long-term prognosis of patients with advanced liver fibrosis or cirrhosis who are being treated for hepatitis B viral infection. Recently, there were two publications attempting to answer this issue. One study[53] indicated that the LS value can predict the development of LREs in patients with chronic hepatitis B receiving entecavir therapy. Another prospective, longitudinal study[54] showed that stratified LS values based on the Laennec system for histologically sub-classifying liver cirrhosis[55] and dynamic changes in LS values at follow up were significantly related to different risks of developing LREs in patients with advanced liver fibrosis who were receiving antiviral therapy for chronic hepatitis B virus infection.
Recently, Singh et al[56] performed a comprehensive meta-analysis of 17 prospective cohort studies and confirmed the association between LS values and LREs in patients with CLDs. According to this meta-analysis, a greater degree of LS was significantly associated with an increased risk of developing LREs, including hepatic decompensation (RR = 1.07), HCC (RR = 1.11), overall mortality (RR = 1.22), or a composite of these events (RR = 1.32). Furthermore, a high LS value predicted the development of liver-related events, such as hepatic decompensation, HCC, and overall mortality, in a dose-dependent manner.
Thus, in addition to identifying liver fibrosis, TE appears to accurately predict long-term prognosis. However, several issues, such as determination of cut-off values, TE measurement interval, and cost-effectiveness, remain unresolved.
ELF SCORING SYSTEM
Serum levels of extracellular matrix proteins and degradation products are increased in advanced liver fibrosis. The Original European Liver Fibrosis (OELF) panel of serum markers (aminoterminal propeptide of procollagen type III, hyaluronic acid, and tissue inhibitor of matrix metalloproteinases-1), which reflects the dynamics of liver fibrosis, was combined with age in 2004[23]. It showed good diagnostic accuracy for evaluating liver fibrosis in CLDs of different etiologies[23]. Later, this panel was simplified to the ELF scoring system by removing age as a factor from the OELF panel, and the diagnostic accuracy remained intact[57]. ELF accurately predicted the extent of liver fibrosis in several cross-sectional validation studies[58-61]. However, there are limited studies on the longitudinal performance of the ELF scoring system for predicting LREs in patients with liver cirrhosis beyond the cross-sectional aspects of ELF.
Parkes et al[58] investigated the performance of the ELF scoring system for predicting the development of LREs in Caucasian patients with diverse etiologies of CLDs using paired ELF scores and liver biopsy data. In this multi-center study from the United Kingdom, the study population was stratified into four groups according to the ELF score for precise assessment of the risk of developing LREs. The performance of the ELF scoring system was compared with that of histopathology of a liver biopsy. The fully adjusted HRs for LREs showed a graded response according to the stratified ELF-score group. Compared to patients with ELF scores < 8.34, patients with higher ELF scores had significantly higher risks of developing LREs (ELF score, 12.52-16.67, HR = 75; ELF score, 10.426-12.51, HR = 20; and ELF score, 8.34-10.425, HR = 5) (Figure 3). Similarly, compared to patients with no fibrosis or mild fibrosis on liver biopsies, patients with advanced liver fibrosis were at increased risk of developing LREs (HR = 2.4 for moderate fibrosis; 8.3 for severe fibrosis/cirrhosis). Thus, the ELF scoring system was better than a liver biopsy for predicting development of LREs.
Figure 3.
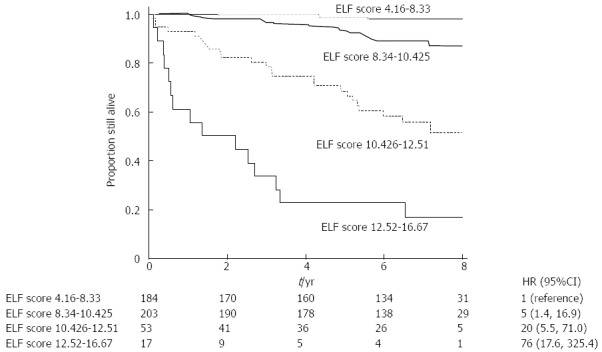
Kaplan-Meier analysis of liver-related events in patients stratified according to enhanced liver fibrosis scores. Reproduced with permission from Parkes et al[58]. The study population was stratified into four groups according to the enhanced liver fibrosis (ELF) score for precise assessment of the risks of developing liver-related events (LREs). LREs showed a graded response according to the stratified ELF score groups. Patients with higher ELF scores had significantly higher risks of having LREs; n = 457.
In addition, during the follow-up period, 82% of patients within the highest ELF-score group (12.52-16.67) experienced an LRE. In contrast, only 46% of those identified with severe fibrosis/cirrhosis based on a liver biopsy experienced an LRE. Moreover, when the risk of developing an LRE was analyzed with ELF as a continuous variable, the fully-adjusted OR for LRE was 2.2 (95%CI: 1.7-2.9). This result indicates that a unit increase in the ELF score was associated with a two-fold risk of developing an LRE. Furthermore, the ELF scoring system showed better diagnostic performance than a liver biopsy (AUROC, 0.82 for ELF, 0.70 for liver biopsy; P = 0.004) for predicting overall mortality.
Recently, the ELF scoring system was further confirmed to predict the development of LREs in a prospective study with a cohort of 170 Asian patients with hepatitis B virus-related CLDs[62]. The ELF scoring system showed good diagnostic performance for predicting the development of LREs (AUROC = 0.808). There was a significant association between the ELF score and the risk of developing LREs (ρ = 0.449; P < 0.01). A unit increase in the ELF score was associated with a 1.4-fold increase in the risk of developing an LRE. A higher ELF score at enrollment was correlated with an increased incidence of LREs (HR = 1.438; P < 0.001). Patients were subdivided into two groups based on a calculated optimal cut-off of 10.1. Patients with lower ELF scores had significantly reduced risks of developing LREs compared with those who had higher ELF scores (HR = 0.24; P < 0.001). Similar to the original publication[58], stratification of patients into three groups based on the ELF score showed that the fully-adjusted HRs for LREs had a graded response. Compared to patients with ELF score ≥ 10.40, patients with lower ELF scores had significantly lower risks of developing LREs (ELF score, < 8.10, HR = 0.072; and ELF score, 8.10-10.39, HR = 0.286). The superior diagnostic performance of the ELF scoring system for predicting overall mortality compared with a liver biopsy was also confirmed in this study (AUROC, 0.749 for ELF, 0.651 for liver biopsy).
Similar to TE, the ability of ELF to predict the development of cirrhosis-related complications has been confirmed in several studies. However, the clinical utility of the ELF scoring system is limited to centers at which extracellular matrix serum markers can be routinely measured. Thus, the general clinical applicability of the ELF scoring system requires extensive validation and a cost-effective analysis.
FIBROTEST
The FT scoring system was developed by Imbert-Bismut et al[17] in 2001. The system is based on a panel of five serum markers, which includes α2-macroglobulin, haptoglobin, apolipoprotein A1, gamma-glutamyl transpeptidase (GGT), and total bilirubin adjusted by age and gender. The performance of FT as a surrogate marker for liver biopsy has been extensively studied. FT is accepted as a promising non-invasive method with a high degree of accuracy and reproducibility for predicting advanced liver fibrosis and cirrhosis in patients with CLDs[63,64]. The prognostic value of FT for predicting five-year survival in patients with CLDs of various etiologies has been previously studied[65-67]. Vergniol et al[66] conducted a prospective five-year study to assess whether FT can predict overall survival (OS) in patients with chronic hepatitis C. In this study, FT showed a high level of accuracy for predicting OS with an AUROC of 0.861. The risk of mortality was increased with a cut-off value of 7.4 (adjusted HR = 90). Furthermore, risk stratification based on the FT score was able to predict five-year OS (FT, ≤ 0.75, OS = 97%; FT, 0.75-0.80, OS = 87%; FT, 0.81-0.85, OS = 84%; FT, 0.86-0.90, OS = 75%; FT, 0.91-0.95, OS = 69%; and FT > 0.95, OS = 0%). Comparable results were observed in a similar prospective, single-center study in patients with chronic hepatitis B[67]. The prognostic performance of FT for predicting OS was good with an AUROC of 0.82. The five-year OS rates were 96.8% for FT ≤ 0.73 and 49.2% for FT > 0.85, respectively.
The FT and measurement of LS by TE have high degrees of accuracy and reproducibility for predicting the extent of liver fibrosis and development of LREs in patients with CLDs. Thus, combined application of these two methods may provide additional discriminatory potential for predicting LREs. Indeed, the combination of LS and FT increased the cross-sectional diagnostic performance for assessing the degree of liver fibrosis and the diagnosis of liver cirrhosis (AUROC, 0.910 for LS only; 0.866 for FT only; 0.915 for FT + LS; and 0.929 for FT × LS)[64]. Park et al[68] recently conducted a prospective five-year longitudinal study to assess if the combination of FT with LS values enhanced the overall performance of predicting LREs in patients with hepatitis B virus-related liver cirrhosis. The combination was calculated as either the sum or multiplication of the FT score and LS values (FT + LS or FT × LS, respectively). In this study, 151 patients were analyzed, and the time-dependent AUROCs for predicting LREs were 0.748 (95%CI: 0.621-0.868) and 0.785 (95%CI: 0.647-0.906) at five-year follow-ups of FT + LS and FT × LS, respectively. Data were adjusted for age and histological fibrosis staging, which were the two significant factors according to univariate analysis (P < 0.05). Multivariate analysis revealed that FT + LS and FT × LS were independent predictors of LREs (P = 0.001, HR = 1.116; P = 0.001, HR = 1.137, respectively). Stratification of the study population into three groups showed that the cumulative risk of developing LREs was significantly graded according to the stratification. The study population was stratified with cut-off values of 9.4 and 17.5 for the FT + LS analysis. The cumulative incidence rates of developing LREs at 2, 3, and 5 years were 2.1%, 4.4%, and 6.7%, respectively, for the low group (FT + LS < 9.4); 3.9%, 6.7%, and 13.0%, respectively, for the intermediate group (FT + LS 9.4-17.5); and 8.0%, 12.2%, and 16.8%, respectively, for the high group (FT + LS > 17.5) (P = 0.029). Similarly, for the FT × LS analysis, the study population was stratified with cut-off values of 3.6 and 11.0. The cumulative incidence rates of developing LREs at 2, 3, and 5 years were 1.8%, 2.7%, and 4.5%, respectively, for the low group (FT × LS < 3.6); 3.8%, 6.1%, and 14.2%, respectively, for the intermediate group (FT × LS 3.6-11.0); and 8.3%, 12.8%, and 17.5%, respectively, for the high group (FT × LS > 11.0) (P = 0.008).
The prognostic role of FT was demonstrated exclusively in a French study of a cohort of patients with chronic hepatitis C. Thus, the clinical value of FT requires further validation in a diverse population of patients with CLDs of varying etiologies. Fortunately, the prognostic performance of FT has recently been demonstrated in several Asian studies of a cohort of patients with chronic hepatitis B in cross-sectional and longitudinal studies[64,69]. Based on current findings, further research is warranted to define the clinical utility of FT for predicting the long-term prognosis of patients with liver cirrhosis.
OTHER MODELS
Several simple non-invasive methods including APRI, FIB-4, Forns’ index and Lok index have been found to be useful in assessing the extent of fibrosis in patients with CLD. Given their universal availability without additional economic burden, several studies evaluated the clinical significance of these simple non-invasive scoring systems for prediction of forthcoming complications related to liver cirrhosis.
A retrospective, multicenter, large-scale study of cirrhotic patients by Sebastiani et al[70] demonstrated that a combination of the Lok index and the Forns’ index had a high negative predictive value (> 90%) to exclude clinically relevant EVs with an AUROC of 0.80, and suggested that these non-invasive markers may be useful as an initial screening tool for cirrhotic patients to exclude the presence of clinically relevant EVs. Another study by Angulo et al[71] showed that simple non-invasive methods including APRI and FIB-4 can identify patients with nonalcoholic fatty liver disease at higher risk for development of LREs and higher overall mortality. However, due to the limitations inherent in the retrospective studies, the clinical value of these non-invasive methods needs to be further validated in additional large-scale, prospective, and preferably, longitudinal studies.
Acoustic radiation force impulse (ARFI) elastography is a novel technology based on conventional B-mode ultrasonography, which provides numeric measurements of tissue stiffness as the shear wave velocity[72]. Several publications suggest that LS values and spleen stiffness measured by ARFI elastography both correlate well with the extent of liver fibrosis in patients with CLDs[73-75]. The role of ARFI elastography for assessing the risk of cirrhosis-related complications has been investigated in several studies[76-79].
A recent cross-sectional study by Morishita et al[77] showed that LS measurements by ARFI elastography predicted the presence of EVs (cut-off value of 2.05 m/s) or high-risk EVs (cut-off value of 2.39 m/s) in patients with hepatitis C virus-related liver cirrhosis. The diagnostic performance of this method was good (AUROC, 0.890 for EVs; 0.868 for high-risk EVs) with a high negative-predictive value (81% for EVs; 89% for high-risk EVs) and an acceptable positive-predictive value (78% for EVs; 69% for high-risk EVs).
In addition, a study by Bota et al[79] proposed a scoring system for predicting high-risk EVs based on liver stiffness and spleen stiffness assessed by ARFI elastography. The diagnostic performance of this scoring system was acceptable (AUROC = 0.721), yet further validation is desired.
Several studies[78,80] also reported that spleen stiffness measurement by TE can provide non-invasive assessment of the presence of EVs in patients with liver cirrhosis. Recently, a prospective study by Takuma et al[78] showed that spleen stiffness assessed by ARFI elastography was able to predict the presence of EVs (cut-off value of 3.18 m/s) or high-risk EVs (cut-off value of 3.30 m/s) in patients with liver cirrhosis. This method showed excellent diagnostic performance (AUROC, 0.933 for EVs; 0.930 for high-risk EVs) and a high negative-predictive value (98.4% for EVs; 99.4% for high-risk EVs). However, the positive-predictive value was low (61.0% for EVs; 47.8% for high-risk EVs). In contrast, Vermehren et al[81] reported that the diagnostic performance of spleen stiffness measured by ARFI elastography for predicting large EVs was not satisfactory (AUROC = 0.58). Moreover, Mori et al[82] showed that there was no significant association between spleen stiffness measured by ARFI elastography and the presence of EVs in patients with chronic hepatitis C. Furthermore, a recent meta-analysis conducted by Singh et al[83] showed that the current techniques of spleen stiffness measurement - either by ARFI or TE - are suboptimal for predicting EVs in patients with CLDs. Hence, further well-designed prospective studies are desired for evaluating the diagnostic role of spleen stiffness measurement in predicting EVs.
There have been no longitudinal studies of the role of LS measurements by ARFI elastography and spleen stiffness measurements with TE or ARFI elastography for risk assessment of LREs in patients with CLDs. Therefore, longitudinal, multi-center studies are warranted to establish a standardized protocol for measuring LS values by ARFI elastography and spleen stiffness by TE or ARFI elastography. Further studies are also needed to validate the clinical role of these non-invasive tools for assessing the risk of liver cirrhosis-related complications.
CONCLUSION
The current view from a limited number of studies is that the recently-introduced non-invasive models can independently predict future cirrhosis-related complications, such as hepatic decompensation, liver failure, HCC, or liver-related death. In addition, some non-invasive tools, such as TE or TE-based models (i.e., LSPS), appear to exhibit superior performance compared to histology and other non-invasive methods for predicting development of LREs.
Non-invasive models may no longer simply be tools for predicting the extent of fibrosis in patients with CLDs. Instead, current literature supports the use of these methods as surveillance tools for predicting future LREs and determining long-term prognosis, which will help to make informed treatment decisions. Future studies should assess whether serial changes in non-invasive measurements or scores reflect the dynamic changes in the risk of developing LREs. In addition, the combination of two or more non-invasive methods should be tested to determine if this approach provides greater discriminatory power for predicting LREs. Significant progress in this field will allow new strategies for risk management in patients with CLD to be developed in the near future.
Footnotes
Supported by The Liver Cirrhosis Clinical Research Center, a grant from the Korea Healthcare Technology RandD Project, Ministry of Health and Welfare, South Korea, No. HI10C2020; the Bilateral International Collaborative RandD Program from the Ministry of Knowledge Economy, South Korea
P- Reviewers: Sebastiani G, Sirli R S- Editor: Zhai HH L- Editor: A E- Editor: Liu XM
References
- 1.Hoofnagle JH, di Bisceglie AM. The treatment of chronic viral hepatitis. N Engl J Med. 1997;336:347–356. doi: 10.1056/NEJM199701303360507. [DOI] [PubMed] [Google Scholar]
- 2.Marcellin P, Boyer N. Transition of care between paediatric and adult gastroenterology. Chronic viral hepatitis. Best Pract Res Clin Gastroenterol. 2003;17:259–275. doi: 10.1016/s1521-6918(03)00014-3. [DOI] [PubMed] [Google Scholar]
- 3.Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004;11:97–107. doi: 10.1046/j.1365-2893.2003.00487.x. [DOI] [PubMed] [Google Scholar]
- 4.Lavanchy D. The global burden of hepatitis C. Liver Int. 2009;29 Suppl 1:74–81. doi: 10.1111/j.1478-3231.2008.01934.x. [DOI] [PubMed] [Google Scholar]
- 5.Fattovich G. Natural history and prognosis of hepatitis B. Semin Liver Dis. 2003;23:47–58. doi: 10.1055/s-2003-37590. [DOI] [PubMed] [Google Scholar]
- 6.McMahon BJ. The natural history of chronic hepatitis B virus infection. Semin Liver Dis. 2004;24 Suppl 1:17–21. doi: 10.1055/s-2004-828674. [DOI] [PubMed] [Google Scholar]
- 7.Afdhal NH. The natural history of hepatitis C. Semin Liver Dis. 2004;24 Suppl 2:3–8. doi: 10.1055/s-2004-832922. [DOI] [PubMed] [Google Scholar]
- 8.McGill DB, Rakela J, Zinsmeister AR, Ott BJ. A 21-year experience with major hemorrhage after percutaneous liver biopsy. Gastroenterology. 1990;99:1396–1400. doi: 10.1016/0016-5085(90)91167-5. [DOI] [PubMed] [Google Scholar]
- 9.Bedossa P, Dargère D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology. 2003;38:1449–1457. doi: 10.1016/j.hep.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 10.Jin SY. [Role of liver biopsy in the assessment of hepatic fibrosis--its utility and limitations] Korean J Hepatol. 2007;13:138–145. [PubMed] [Google Scholar]
- 11.Regev A, Berho M, Jeffers LJ, Milikowski C, Molina EG, Pyrsopoulos NT, Feng ZZ, Reddy KR, Schiff ER. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol. 2002;97:2614–2618. doi: 10.1111/j.1572-0241.2002.06038.x. [DOI] [PubMed] [Google Scholar]
- 12.Sheth SG, Flamm SL, Gordon FD, Chopra S. AST/ALT ratio predicts cirrhosis in patients with chronic hepatitis C virus infection. Am J Gastroenterol. 1998;93:44–48. doi: 10.1111/j.1572-0241.1998.044_c.x. [DOI] [PubMed] [Google Scholar]
- 13.Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, Lok AS. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38:518–526. doi: 10.1053/jhep.2003.50346. [DOI] [PubMed] [Google Scholar]
- 14.Kim BK, Kim SA, Park YN, Cheong JY, Kim HS, Park JY, Cho SW, Han KH, Chon CY, Moon YM, et al. Noninvasive models to predict liver cirrhosis in patients with chronic hepatitis B. Liver Int. 2007;27:969–976. doi: 10.1111/j.1478-3231.2007.01519.x. [DOI] [PubMed] [Google Scholar]
- 15.Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, S Sulkowski M, Torriani FJ, Dieterich DT, Thomas DL, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43:1317–1325. doi: 10.1002/hep.21178. [DOI] [PubMed] [Google Scholar]
- 16.Forns X, Ampurdanès S, Llovet JM, Aponte J, Quintó L, Martínez-Bauer E, Bruguera M, Sánchez-Tapias JM, Rodés J. Identification of chronic hepatitis C patients without hepatic fibrosis by a simple predictive model. Hepatology. 2002;36:986–992. doi: 10.1053/jhep.2002.36128. [DOI] [PubMed] [Google Scholar]
- 17.Imbert-Bismut F, Ratziu V, Pieroni L, Charlotte F, Benhamou Y, Poynard T. Biochemical markers of liver fibrosis in patients with hepatitis C virus infection: a prospective study. Lancet. 2001;357:1069–1075. doi: 10.1016/S0140-6736(00)04258-6. [DOI] [PubMed] [Google Scholar]
- 18.Patel K, Gordon SC, Jacobson I, Hézode C, Oh E, Smith KM, Pawlotsky JM, McHutchison JG. Evaluation of a panel of non-invasive serum markers to differentiate mild from moderate-to-advanced liver fibrosis in chronic hepatitis C patients. J Hepatol. 2004;41:935–942. doi: 10.1016/j.jhep.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 19.Zaman A, Rosen HR, Ingram K, Corless CL, Oh E, Smith K. Assessment of FIBROSpect II to detect hepatic fibrosis in chronic hepatitis C patients. Am J Med. 2007;120:280.e9–280.14. doi: 10.1016/j.amjmed.2006.06.044. [DOI] [PubMed] [Google Scholar]
- 20.Christensen C, Bruden D, Livingston S, Deubner H, Homan C, Smith K, Oh E, Gretch D, Williams J, McMahon B. Diagnostic accuracy of a fibrosis serum panel (FIBROSpect II) compared with Knodell and Ishak liver biopsy scores in chronic hepatitis C patients. J Viral Hepat. 2006;13:652–658. doi: 10.1111/j.1365-2893.2006.00743.x. [DOI] [PubMed] [Google Scholar]
- 21.Adams LA, Bulsara M, Rossi E, DeBoer B, Speers D, George J, Kench J, Farrell G, McCaughan GW, Jeffrey GP. Hepascore: an accurate validated predictor of liver fibrosis in chronic hepatitis C infection. Clin Chem. 2005;51:1867–1873. doi: 10.1373/clinchem.2005.048389. [DOI] [PubMed] [Google Scholar]
- 22.Lok AS, Ghany MG, Goodman ZD, Wright EC, Everson GT, Sterling RK, Everhart JE, Lindsay KL, Bonkovsky HL, Di Bisceglie AM, et al. Predicting cirrhosis in patients with hepatitis C based on standard laboratory tests: results of the HALT-C cohort. Hepatology. 2005;42:282–292. doi: 10.1002/hep.20772. [DOI] [PubMed] [Google Scholar]
- 23.Rosenberg WM, Voelker M, Thiel R, Becka M, Burt A, Schuppan D, Hubscher S, Roskams T, Pinzani M, Arthur MJ. Serum markers detect the presence of liver fibrosis: a cohort study. Gastroenterology. 2004;127:1704–1713. doi: 10.1053/j.gastro.2004.08.052. [DOI] [PubMed] [Google Scholar]
- 24.Sandrin L, Fourquet B, Hasquenoph JM, Yon S, Fournier C, Mal F, Christidis C, Ziol M, Poulet B, Kazemi F, et al. Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol. 2003;29:1705–1713. doi: 10.1016/j.ultrasmedbio.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 25.Jung KS, Kim SU. Clinical applications of transient elastography. Clin Mol Hepatol. 2012;18:163–173. doi: 10.3350/cmh.2012.18.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friedrich-Rust M, Ong MF, Martens S, Sarrazin C, Bojunga J, Zeuzem S, Herrmann E. Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology. 2008;134:960–974. doi: 10.1053/j.gastro.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 27.Chon YE, Choi EH, Song KJ, Park JY, Kim do Y, Han KH, Chon CY, Ahn SH, Kim SU. Performance of transient elastography for the staging of liver fibrosis in patients with chronic hepatitis B: a meta-analysis. PLoS One. 2012;7:e44930. doi: 10.1371/journal.pone.0044930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith JO, Sterling RK. Systematic review: non-invasive methods of fibrosis analysis in chronic hepatitis C. Aliment Pharmacol Ther. 2009;30:557–576. doi: 10.1111/j.1365-2036.2009.04062.x. [DOI] [PubMed] [Google Scholar]
- 29.Morra R, Lebray P, Ingiliz P, Ngo Y, Munteanu M, Ratziu V, Poynard T. FibroTest has better diagnostic and prognostic values than the aspartate aminotransferase-to-platelet ratio index in patients with chronic hepatitis C. Hepatology. 2008;47:353–354; author reply 354-356. doi: 10.1002/hep.22046. [DOI] [PubMed] [Google Scholar]
- 30.Shaheen AA, Myers RP. Diagnostic accuracy of the aspartate aminotransferase-to-platelet ratio index for the prediction of hepatitis C-related fibrosis: a systematic review. Hepatology. 2007;46:912–921. doi: 10.1002/hep.21835. [DOI] [PubMed] [Google Scholar]
- 31.Kim SU, Han KH, Ahn SH. Non-invasive assessment of liver fibrosis: time to move from cross-sectional studies to longitudinal ones. J Gastroenterol Hepatol. 2010;25:1472–1473. doi: 10.1111/j.1440-1746.2010.06432.x. [DOI] [PubMed] [Google Scholar]
- 32.Kim SU, Han KH, Ahn SH. Non-invasive assessment of liver fibrosis: the gap between ideal and real. J Gastroenterol Hepatol. 2011;26:937–939. doi: 10.1111/j.1440-1746.2011.06741.x. [DOI] [PubMed] [Google Scholar]
- 33.Jung KS, Kim SU, Ahn SH, Park YN, Kim do Y, Park JY, Chon CY, Choi EH, Han KH. Risk assessment of hepatitis B virus-related hepatocellular carcinoma development using liver stiffness measurement (FibroScan) Hepatology. 2011;53:885–894. doi: 10.1002/hep.24121. [DOI] [PubMed] [Google Scholar]
- 34.Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922–938. doi: 10.1002/hep.21907. [DOI] [PubMed] [Google Scholar]
- 35.Jensen DM. Endoscopic screening for varices in cirrhosis: findings, implications, and outcomes. Gastroenterology. 2002;122:1620–1630. doi: 10.1053/gast.2002.33419. [DOI] [PubMed] [Google Scholar]
- 36.Merli M, Nicolini G, Angeloni S, Rinaldi V, De Santis A, Merkel C, Attili AF, Riggio O. Incidence and natural history of small esophageal varices in cirrhotic patients. J Hepatol. 2003;38:266–272. doi: 10.1016/s0168-8278(02)00420-8. [DOI] [PubMed] [Google Scholar]
- 37.Kazemi F, Kettaneh A, N’kontchou G, Pinto E, Ganne-Carrie N, Trinchet JC, Beaugrand M. Liver stiffness measurement selects patients with cirrhosis at risk of bearing large oesophageal varices. J Hepatol. 2006;45:230–235. doi: 10.1016/j.jhep.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 38.Lemoine M, Katsahian S, Ziol M, Nahon P, Ganne-Carrie N, Kazemi F, Grando-Lemaire V, Trinchet JC, Beaugrand M. Liver stiffness measurement as a predictive tool of clinically significant portal hypertension in patients with compensated hepatitis C virus or alcohol-related cirrhosis. Aliment Pharmacol Ther. 2008;28:1102–1110. doi: 10.1111/j.1365-2036.2008.03825.x. [DOI] [PubMed] [Google Scholar]
- 39.Castéra L, Le Bail B, Roudot-Thoraval F, Bernard PH, Foucher J, Merrouche W, Couzigou P, de Lédinghen V. Early detection in routine clinical practice of cirrhosis and oesophageal varices in chronic hepatitis C: comparison of transient elastography (FibroScan) with standard laboratory tests and non-invasive scores. J Hepatol. 2009;50:59–68. doi: 10.1016/j.jhep.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 40.Pritchett S, Cardenas A, Manning D, Curry M, Afdhal NH. The optimal cut-off for predicting large oesophageal varices using transient elastography is disease specific. J Viral Hepat. 2011;18:e75–e80. doi: 10.1111/j.1365-2893.2010.01375.x. [DOI] [PubMed] [Google Scholar]
- 41.Nguyen-Khac E, Saint-Leger P, Tramier B, Coevoet H, Capron D, Dupas JL. Noninvasive diagnosis of large esophageal varices by Fibroscan: strong influence of the cirrhosis etiology. Alcohol Clin Exp Res. 2010;34:1146–1153. doi: 10.1111/j.1530-0277.2010.01191.x. [DOI] [PubMed] [Google Scholar]
- 42.Sporea I, Raţiu I, Sirli R, Popescu A, Bota S. Value of transient elastography for the prediction of variceal bleeding. World J Gastroenterol. 2011;17:2206–2210. doi: 10.3748/wjg.v17.i17.2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med. 2013;34:238–253. doi: 10.1055/s-0033-1335375. [DOI] [PubMed] [Google Scholar]
- 44.Kim BK, Han KH, Park JY, Ahn SH, Kim JK, Paik YH, Lee KS, Chon CY, Kim do Y. A liver stiffness measurement-based, noninvasive prediction model for high-risk esophageal varices in B-viral liver cirrhosis. Am J Gastroenterol. 2010;105:1382–1390. doi: 10.1038/ajg.2009.750. [DOI] [PubMed] [Google Scholar]
- 45.Kim BK, Kim do Y, Han KH, Park JY, Kim JK, Paik YH, Lee KS, Chon CY, Ahn SH. Risk assessment of esophageal variceal bleeding in B-viral liver cirrhosis by a liver stiffness measurement-based model. Am J Gastroenterol. 2011;106:1654–162, 1730. doi: 10.1038/ajg.2011.160. [DOI] [PubMed] [Google Scholar]
- 46.Berzigotti A, Seijo S, Arena U, Abraldes JG, Vizzutti F, García-Pagán JC, Pinzani M, Bosch J. Elastography, spleen size, and platelet count identify portal hypertension in patients with compensated cirrhosis. Gastroenterology. 2013;144:102–111.e1. doi: 10.1053/j.gastro.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 47.Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–1022. doi: 10.1002/hep.24199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.European Association For The Study Of The Liver, European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908–943. doi: 10.1016/j.jhep.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 49.Masuzaki R, Tateishi R, Yoshida H, Goto E, Sato T, Ohki T, Imamura J, Goto T, Kanai F, Kato N, et al. Prospective risk assessment for hepatocellular carcinoma development in patients with chronic hepatitis C by transient elastography. Hepatology. 2009;49:1954–1961. doi: 10.1002/hep.22870. [DOI] [PubMed] [Google Scholar]
- 50.Kim BK, Park YN, Kim do Y, Park JY, Chon CY, Han KH, Ahn SH. Risk assessment of development of hepatic decompensation in histologically proven hepatitis B viral cirrhosis using liver stiffness measurement. Digestion. 2012;85:219–227. doi: 10.1159/000335430. [DOI] [PubMed] [Google Scholar]
- 51.Kim SU, Lee JH, Kim do Y, Ahn SH, Jung KS, Choi EH, Park YN, Han KH, Chon CY, Park JY. Prediction of liver-related events using fibroscan in chronic hepatitis B patients showing advanced liver fibrosis. PLoS One. 2012;7:e36676. doi: 10.1371/journal.pone.0036676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chon YE, Jung ES, Park JY, Kim do Y, Ahn SH, Han KH, Chon CY, Jung KS, Kim SU. The accuracy of noninvasive methods in predicting the development of hepatocellular carcinoma and hepatic decompensation in patients with chronic hepatitis B. J Clin Gastroenterol. 2012;46:518–525. doi: 10.1097/MCG.0b013e31825079f1. [DOI] [PubMed] [Google Scholar]
- 53.Kim MN, Kim SU, Park JY, Kim do Y, Han KH, Chon CY, Ahn SH. Risk Assessment of Liver-related Events Using Transient Elastography in Patients With Chronic Hepatitis B Receiving Entecavir. J Clin Gastroenterol. 2014;48:272–278. doi: 10.1097/MCG.0b013e31829a7247. [DOI] [PubMed] [Google Scholar]
- 54.Kim BK, Oh HJ, Park JY, Kim do Y, Ahn SH, Han KH, Park Y, Yoo EJ, Park YN, Kim SU. Early on-treatment change in liver stiffness predicts development of liver-related events in chronic hepatitis B patients receiving antiviral therapy. Liver Int. 2013;33:180–189. doi: 10.1111/liv.12020. [DOI] [PubMed] [Google Scholar]
- 55.Kim MY, Cho MY, Baik SK, Park HJ, Jeon HK, Im CK, Won CS, Kim JW, Kim HS, Kwon SO, et al. Histological subclassification of cirrhosis using the Laennec fibrosis scoring system correlates with clinical stage and grade of portal hypertension. J Hepatol. 2011;55:1004–1009. doi: 10.1016/j.jhep.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 56.Singh S, Fujii LL, Murad MH, Wang Z, Asrani SK, Ehman RL, Kamath PS, Talwalkar JA. Liver stiffness is associated with risk of decompensation, liver cancer, and death in patients with chronic liver diseases: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2013;11:1573–1584.e1-2; quiz e88-89. doi: 10.1016/j.cgh.2013.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Parkes J, Guha IN, Roderick P, Harris S, Cross R, Manos MM, Irving W, Zaitoun A, Wheatley M, Ryder S, et al. Enhanced Liver Fibrosis (ELF) test accurately identifies liver fibrosis in patients with chronic hepatitis C. J Viral Hepat. 2011;18:23–31. doi: 10.1111/j.1365-2893.2009.01263.x. [DOI] [PubMed] [Google Scholar]
- 58.Parkes J, Roderick P, Harris S, Day C, Mutimer D, Collier J, Lombard M, Alexander G, Ramage J, Dusheiko G, et al. Enhanced liver fibrosis test can predict clinical outcomes in patients with chronic liver disease. Gut. 2010;59:1245–1251. doi: 10.1136/gut.2009.203166. [DOI] [PubMed] [Google Scholar]
- 59.Crespo G, Fernández-Varo G, Mariño Z, Casals G, Miquel R, Martínez SM, Gilabert R, Forns X, Jiménez W, Navasa M. ARFI, FibroScan, ELF, and their combinations in the assessment of liver fibrosis: a prospective study. J Hepatol. 2012;57:281–287. doi: 10.1016/j.jhep.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 60.Friedrich-Rust M, Rosenberg W, Parkes J, Herrmann E, Zeuzem S, Sarrazin C. Comparison of ELF, FibroTest and FibroScan for the non-invasive assessment of liver fibrosis. BMC Gastroenterol. 2010;10:103. doi: 10.1186/1471-230X-10-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim BK, Kim HS, Park JY, Kim do Y, Ahn SH, Chon CY, Park YN, Han KH, Kim SU. Prospective validation of ELF test in comparison with Fibroscan and FibroTest to predict liver fibrosis in Asian subjects with chronic hepatitis B. PLoS One. 2012;7:e41964. doi: 10.1371/journal.pone.0041964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kim SU, Yoo EJ, Kim BK, Park JY, Kim DY, Ahn SH, Han KH, Chon CY. Enhanced Liver Fibrosis test can predict the forthcoming development of liver-related events in patients with chronic hepatitis B. 7th International Liver Cancer Association (ILCA) Annual Conference.2013 Sep 13-15; Washington D.C [Google Scholar]
- 63.Poynard T, Ngo Y, Munteanu M, Thabut D, Ratziu V. Noninvasive Markers of Hepatic Fibrosis in Chronic Hepatitis B. Curr Hepat Rep. 2011;10:87–97. doi: 10.1007/s11901-011-0096-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kim BK, Kim SU, Kim HS, Park JY, Ahn SH, Chon CY, Cho IR, Joh DH, Park YN, Han KH, et al. Prospective validation of FibroTest in comparison with liver stiffness for predicting liver fibrosis in Asian subjects with chronic hepatitis B. PLoS One. 2012;7:e35825. doi: 10.1371/journal.pone.0035825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Poynard T, Ngo Y, Perazzo H, Munteanu M, Lebray P, Moussalli J, Thabut D, Benhamou Y, Ratziu V. Prognostic value of liver fibrosis biomarkers: a meta-analysis. Gastroenterol Hepatol (N Y) 2011;7:445–454. [PMC free article] [PubMed] [Google Scholar]
- 66.Vergniol J, Foucher J, Terrebonne E, Bernard PH, le Bail B, Merrouche W, Couzigou P, de Ledinghen V. Noninvasive tests for fibrosis and liver stiffness predict 5-year outcomes of patients with chronic hepatitis C. Gastroenterology. 2011;140:1970–1979, 1979.e1-3. doi: 10.1053/j.gastro.2011.02.058. [DOI] [PubMed] [Google Scholar]
- 67.de Lédinghen V, Vergniol J, Barthe C, Foucher J, Chermak F, Le Bail B, Merrouche W, Bernard PH. Non-invasive tests for fibrosis and liver stiffness predict 5-year survival of patients chronically infected with hepatitis B virus. Aliment Pharmacol Ther. 2013;37:979–988. doi: 10.1111/apt.12307. [DOI] [PubMed] [Google Scholar]
- 68.Park MS, Kim BK, Kim SU, Park JY, Kim DY, Ahn SH, Han KH. Prognostic value of combined use of liver stiffness measurement using transient elastography and FibroTest in patients with chronic hepatitis B; The 64th Annual Meeting of the American Association for the Study of Liver Diseases. 2013 Nov 1-5; Washington D.C [Google Scholar]
- 69.Park MS, Kim BK, Cheong JY, Kim DJ, Park JY, Kim do Y, Ahn SH, Han KH, Chon CY, Kim SU. Discordance between liver biopsy and FibroTest in assessing liver fibrosis in chronic hepatitis B. PLoS One. 2013;8:e55759. doi: 10.1371/journal.pone.0055759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sebastiani G, Tempesta D, Fattovich G, Castera L, Halfon P, Bourliere M, Noventa F, Angeli P, Saggioro A, Alberti A. Prediction of oesophageal varices in hepatic cirrhosis by simple serum non-invasive markers: Results of a multicenter, large-scale study. J Hepatol. 2010;53:630–638. doi: 10.1016/j.jhep.2010.04.019. [DOI] [PubMed] [Google Scholar]
- 71.Angulo P, Bugianesi E, Bjornsson ES, Charatcharoenwitthaya P, Mills PR, Barrera F, Haflidadottir S, Day CP, George J. Simple noninvasive systems predict long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2013;145:782–789.e4. doi: 10.1053/j.gastro.2013.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Friedrich-Rust M, Wunder K, Kriener S, Sotoudeh F, Richter S, Bojunga J, Herrmann E, Poynard T, Dietrich CF, Vermehren J, et al. Liver fibrosis in viral hepatitis: noninvasive assessment with acoustic radiation force impulse imaging versus transient elastography. Radiology. 2009;252:595–604. doi: 10.1148/radiol.2523081928. [DOI] [PubMed] [Google Scholar]
- 73.Friedrich-Rust M, Nierhoff J, Lupsor M, Sporea I, Fierbinteanu-Braticevici C, Strobel D, Takahashi H, Yoneda M, Suda T, Zeuzem S, et al. Performance of Acoustic Radiation Force Impulse imaging for the staging of liver fibrosis: a pooled meta-analysis. J Viral Hepat. 2012;19:e212–e219. doi: 10.1111/j.1365-2893.2011.01537.x. [DOI] [PubMed] [Google Scholar]
- 74.Rizzo L, Calvaruso V, Cacopardo B, Alessi N, Attanasio M, Petta S, Fatuzzo F, Montineri A, Mazzola A, L’abbate L, et al. Comparison of transient elastography and acoustic radiation force impulse for non-invasive staging of liver fibrosis in patients with chronic hepatitis C. Am J Gastroenterol. 2011;106:2112–2120. doi: 10.1038/ajg.2011.341. [DOI] [PubMed] [Google Scholar]
- 75.Takahashi H, Ono N, Eguchi Y, Eguchi T, Kitajima Y, Kawaguchi Y, Nakashita S, Ozaki I, Mizuta T, Toda S, et al. Evaluation of acoustic radiation force impulse elastography for fibrosis staging of chronic liver disease: a pilot study. Liver Int. 2010;30:538–545. doi: 10.1111/j.1478-3231.2009.02130.x. [DOI] [PubMed] [Google Scholar]
- 76.Ye XP, Ran HT, Cheng J, Zhu YF, Zhang DZ, Zhang P, Zheng YY. Liver and spleen stiffness measured by acoustic radiation force impulse elastography for noninvasive assessment of liver fibrosis and esophageal varices in patients with chronic hepatitis B. J Ultrasound Med. 2012;31:1245–1253. doi: 10.7863/jum.2012.31.8.1245. [DOI] [PubMed] [Google Scholar]
- 77.Morishita N, Hiramatsu N, Oze T, Harada N, Yamada R, Miyazaki M, Yakushijin T, Miyagi T, Yoshida Y, Tatsumi T, et al. Liver stiffness measurement by acoustic radiation force impulse is useful in predicting the presence of esophageal varices or high-risk esophageal varices among patients with HCV-related cirrhosis. J Gastroenterol. 2013:Epub ahead of print. doi: 10.1007/s00535-013-0877-z. [DOI] [PubMed] [Google Scholar]
- 78.Takuma Y, Nouso K, Morimoto Y, Tomokuni J, Sahara A, Toshikuni N, Takabatake H, Shimomura H, Doi A, Sakakibara I, et al. Measurement of spleen stiffness by acoustic radiation force impulse imaging identifies cirrhotic patients with esophageal varices. Gastroenterology. 2013;144:92–101.e2. doi: 10.1053/j.gastro.2012.09.049. [DOI] [PubMed] [Google Scholar]
- 79.Bota S, Sporea I, Sirli R, Focsa M, Popescu A, Danila M, Strain M. Can ARFI elastography predict the presence of significant esophageal varices in newly diagnosed cirrhotic patients? Ann Hepatol. 2012;11:519–525. [PubMed] [Google Scholar]
- 80.Stefanescu H, Grigorescu M, Lupsor M, Procopet B, Maniu A, Badea R. Spleen stiffness measurement using Fibroscan for the noninvasive assessment of esophageal varices in liver cirrhosis patients. J Gastroenterol Hepatol. 2011;26:164–170. doi: 10.1111/j.1440-1746.2010.06325.x. [DOI] [PubMed] [Google Scholar]
- 81.Vermehren J, Polta A, Zimmermann O, Herrmann E, Poynard T, Hofmann WP, Bojunga J, Sarrazin C, Zeuzem S, Friedrich-Rust M. Comparison of acoustic radiation force impulse imaging with transient elastography for the detection of complications in patients with cirrhosis. Liver Int. 2012;32:852–858. doi: 10.1111/j.1478-3231.2011.02736.x. [DOI] [PubMed] [Google Scholar]
- 82.Mori K, Arai H, Abe T, Takayama H, Toyoda M, Ueno T, Sato K. Spleen stiffness correlates with the presence of ascites but not esophageal varices in chronic hepatitis C patients. Biomed Res Int. 2013;2013:857862. doi: 10.1155/2013/857862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Singh S, Eaton JE, Murad MH, Tanaka H, Iijima H, Talwalkar JA. Accuracy of Spleen Stiffness Measurement in Detection of Esophageal Varices in Patients With Chronic Liver Disease: Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2013:Epub ahead of print. doi: 10.1016/j.cgh.2013.09.013. [DOI] [PubMed] [Google Scholar]


