Abstract
AIM: To compare the liver transplantation-free (LTF) survival rates between patients who underwent transjugular intrahepatic portosystemic shunts (TIPS) and those who underwent paracentesis by an updated meta-analysis that pools the effects of both number of deaths and time to death.
METHODS: MEDLINE, EMBASE, and the Cochrane Library were searched from the inception to October 2012. LTF survival, liver transplantation, liver disease-related death, non-liver disease-related death, recurrent ascites, hepatic encephalopathy (HE) and severe HE, and hepatorenal syndrome were assessed as outcomes. LTF survival was estimated using a HR with a 95%CI. Other outcomes were estimated using OR with 95%CIs. Sensitivity analyses were performed to assess the effects of potential outliers in the studies according to the risk of bias and the study characteristics.
RESULTS: Six randomized controlled trials with 390 patients were included. In comparison to paracentesis, TIPS significantly improved LTF survival (HR = 0.61, 95%CI: 0.46-0.82, P < 0.001). TIPS also significantly decreased liver disease-related death (OR = 0.62, 95%CI: 0.39-0.98, P = 0.04), recurrent ascites (OR = 0.15, 95%CI: 0.09-0.24, P < 0.001) and hepatorenal syndrome (OR = 0.32, 95%CI: 0.12-0.86, P = 0.02). However, TIPS increased the risk of HE (OR = 2.95, 95%CI: 1.87-4.66, P = 0.02) and severe HE (OR = 2.18, 95%CI: 1.27-3.76, P = 0.005).
CONCLUSION: TIPS significantly improved the LTF survival of cirrhotic patients with refractory ascites and decreased the risk of recurrent ascites and hepatorenal syndrome with the cost of increased risk of HE compared with paracentesis. Further studies are warranted to validate the survival benefit of TIPS in clinical practice settings.
Keywords: Transjugular intrahepatic portosystemic shunt, Ascites, Paracentesis, Survival, Meta-analysis
Core tip: We evaluated the effects of transjugular intrahepatic portosystemic shunts (TIPS) vs paracentesis on the liver transplantation-free (LTF) survival in patients with cirrhosis and refractory ascites. Both the number of deaths and the time to death were considered in the present meta-analysis. We found that TIPS significantly improved LTF survival, liver disease-related death, recurrence of ascites, and hepatorenal syndrome; however, TIPS increased the risk of post-TIPS hepatic encephalopathy.
INTRODUCTION
Refractory ascites is observed in 5%-10% of advanced cirrhosis cases and has a one-year mortality rate of 20%-50%[1-3]. Liver transplantation is the only definitive treatment for these patients, but the procedure is limited by donor liver resources and high cost. Repeated large-volume or total-volume paracentesis with intravenous albumin infusion is currently recommended as the first-line treatment for patients with refractory ascites[4,5]. Although therapeutic paracentesis relieves symptoms rapidly with few technical complications, it does not correct the underlying mechanisms of ascites formation and has negative effects on systemic hemodynamics and renal function[2]. Although surgical portal-caval shunts are effective in the treatment of refractory ascites by reducing the portosystemic pressure gradient (PSG), these shunts have been abandoned because of the high postoperative morbidity and mortality rates[6]. Transjugular intrahepatic portosystemic shunts (TIPS) decompress the PSG and correct the formation of ascites in most cases without the need for general anesthesia, avoiding the risk of major surgery[4,5,7].
Several randomized controlled trials (RCTs) have compared uncovered TIPS with paracentesis in the management of refractory ascites in cirrhotic patients[8-13]. Despite the demonstration by these studies that TIPS was effective in controlling ascites, it was associated with an increased risk of hepatic encephalopathy (HE) and controversial results in survival benefits[8-13]. Based on the data reported in the literature about the five available RCTs[8-12], four previous meta-analyses concluded that TIPS could not significantly decrease patient mortality when compared with paracentesis[6,14-16]. It is notable that all four of these meta-analyses simply combined the number of deaths without considering the effect of the time to death. Thereafter, a meta-analysis by Salerno et al[17] pooled individual patient data from four RCTs to overcome this inappropriate survival analysis and demonstrated that TIPS significantly improved liver transplantation-free (LTF) survival. However, the impossibility of collecting individual patient data from all of the identified RCTs is a potential drawback for the meta-analysis conducted by Salerno et al[17] and Higgins et al[18]. Most likely, the inconsistent conclusions among these meta-analyses were due in part to the hesitation of recommending TIPS as the primary therapy[4,5]. After these meta-analyses, one additional RCT was published in 2011[13]. Thus, it is useful to conduct an updated meta-analysis using an appropriate survival analysis method to evaluate the effect of TIPS on LTF survival in cirrhotic patients with refractory ascites.
The purpose of the present study was to update the previous meta-analyses to evaluate the effect of TIPS on patient survival by appropriate survival analysis. LTF survival was employed as the primary endpoint. Additionally, the causes of death, the number of patients who underwent liver transplantation, the frequency of recurrent ascites, the risk of HE, and the incidence of hepatorenal syndrome were evaluated.
MATERIALS AND METHODS
Searching for and selection of studies
Eligible studies were identified by a comprehensive search of MEDLINE, EMBASE, and the Cochrane Library from their inceptions to October 2012. The following key words were used in our searches: ascites, TIPS, paracentesis, and RCT. Reference lists in primary study publications, review articles, editorials, and the proceedings of international congresses were also manually examined.
The following criteria were employed for study selection: (1) study publication: full-text in the English language; (2) study design: RCT; (3) study participants: cirrhotic patients with refractory or recurrent ascites; (4) study interventions: TIPS vs large-volume or total-volume paracentesis (with/without intravenous albumin); and (5) one or more of the following outcomes estimated: LTF survival, liver transplantation, cause of death (liver disease-related death or non-liver disease-related death), recurrence of ascites, HE, and hepatorenal syndrome.
Outcomes and definitions
LTF survival (primary endpoint): patient survival without liver transplantation. Liver transplantation: number of patients who underwent liver transplantation. Liver disease-related death: number of patients who died of liver disease-related causes, including hepatic failure, variceal bleeding, hepatorenal syndrome, and hepatocellular carcinoma. Non-liver disease-related death: number of patients who died of non-liver disease-related causes, such as sepsis, cerebrovascular accident, and cardiac dysfunction[16]. Recurrence of ascites: number of patients who required a new paracentesis after the interventions. HE and severe HE: number of patients who presented with HE after intervention and the number of patients with severe HE (grades III/IV HE according to Conn et al[19] or equivalent classification), respectively. Hepatorenal syndrome: number of patients with type 1 or type 2 hepatorenal syndrome.
Risk of bias assessment
According to the Cochrane risk of bias tool[18], the following six items were used in the assessment of risk of bias: generation of random allocation sequence, concealment of allocation sequence, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective outcome reporting.
Data extraction
Determination of trial eligibility and extraction of data were performed independently by two investigators (Bai M and Qi X). Agreements on disagreements were made through discussion. The following data were extracted: patient selection criteria, number of patients screened, number of patients allocated to each study group, detailed information of interventions, study design, duration of follow-up, age, gender, etiology of cirrhosis, Child-Pugh class and score, HE, history of gastrointestinal bleeding, serum bilirubin, serum albumin, serum creatinine, serum sodium, technical results, method of randomization, allocation concealment, blinding, analysis methods, description of drop-outs, and detailed data of outcome measures.
Statistical analysis
For outcomes reported as time-to-event variables, the HRs are the most appropriate measures to be pooled because both the number of events and the time to events are important[20,21]. The Log (HR) and its standard error for a study are needed to evaluate the pooled HRs. These values were calculated according to the methods described by Parmar et al[22] and Tierney et al[20]. In summary, randomization ratio, number of analyzed patients, number of observed events, number of expected events, HR and its 95%CI, logrank variance, logrank observed-minus-expected events, and P value of logrank test were all used when available. When these variables were insufficient, Kaplan-Meier curves were employed to calculate the Log (HR) and its standard error. These calculations were accomplished by the calculation spreadsheet provided by Tierney et al[20]. For outcomes reported as binary variables, the numbers of observed events were extracted and OR were used to evaluate the pooled effect. Heterogeneity was assessed by the χ2 test and the I2 statistic. Upon confirmation that significant heterogeneity was absent, trials were combined using a fixed-effect model. Otherwise, the results of both fixed-effect and random-effect model were reported. To assess the stability of results, sensitivity analyses were performed on the effects of potential outlier studies according to the risk of bias and the study characteristics. A P value of 0.05 was adopted as the criterion for statistical significance. All analyses were performed using Review Manager (RevMan) [Computer program]. Version 5.1. Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2011.
RESULTS
Among the 155 identified publications, 40 duplicates were excluded. The remaining 115 papers underwent detailed examination, and 109 were subsequently excluded (Figure 1). Six RCTs including 390 patients reported between 1996 and 2011 were ultimately included in the meta-analysis[8-13].
Figure 1.
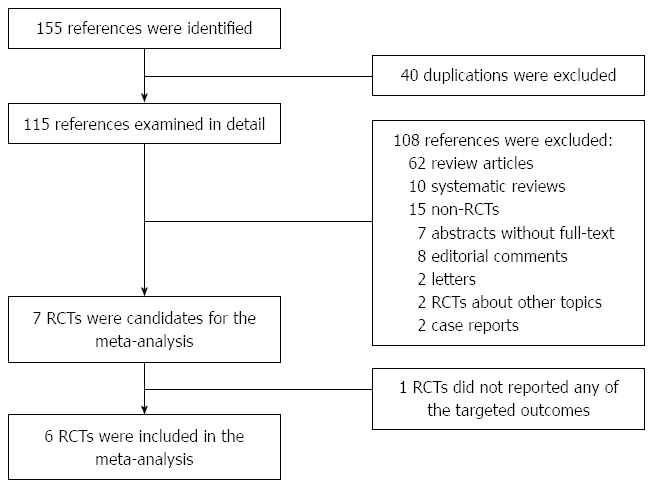
Randomized controlled trial selection flowchart. RCT: Randomized controlled trial.
Characteristics of the selected trials
The characteristics of the six included RCTs are summarized in Table 1. The control treatment was large-volume paracentesis[9,12,13] and total paracentesis[8,10,11] in three studies each. Intravenous albumin infusion was prescribed after paracentesis in four studies[8,11-13], employed when clinically indicated in one study[9], and used when patients had a creatinine clearance < 60 mL/min in the remaining studies[10]. In five studies[8,9,11-13], refractory ascites was defined according to the criteria reported by the International Ascites Club in 1996[23]. Two trials included patients with recidivant ascites, which was defined as more than three episodes of tense ascites within a 12-mo period despite the administration of standard treatment[9,12].
Table 1.
Characteristics of the included studies
| Study characteristics | Lebrec et al[10] | Rössle et al[9] | Ginès et al[8] | Sanyal et al[11] | Salerno et al[12] | Narahara et al[13] |
| Study design | Single-center, RCT | Multi-center, RCT | Multi-center, RCT | Multi-center, RCT | Multi-center, RCT | Single-center, RCT |
| Para | TP with albumin infusion (unclear dose) if creatinine clearance < 60 mL/min | LVP with albumin infusion (8 g/L of ascites removed) when clinically indicated | TP with albumin infusion (8 g/L of ascites removed) | TP with albumin infusion (6-8 g/L of ascites removed) | LVP with albumin infusion (8 g/L of ascites removed) | LVP with albumin infusion (6 g/L of ascites removed) |
| Study population | Cirrhotic patients with refractory ascites | Cirrhotic patients with refractory or recidivant ascites | Cirrhotic patients with refractory ascites | Cirrhotic patients with refractory ascites | Cirrhotic patients with refractory or recidivant ascites | Cirrhotic patients with refractory ascites |
| Definition of refractory ascites | Adequate diuretic and sodium restriction: body weight loss < 200 g/d in 5 d or > 2 tense ascites in 4 mo. | Definition reported in 1996 by International Ascites Club | Definition reported in 1996 by International Ascites Club | Definition reported in 1996 by International Ascites Club | Definition reported in 1996 by International Ascites Club | Definition reported in 1996 by International Ascites Club |
| Exclusion criteria | > 70 yr, HE, severe non-hepatic disease, pulmonary hypertension, PVT/HVT, HCC, active bacterial infection, severe alcoholic hepatitis, biliary obstruction, creatinine > 1.7 mg/dL | HE ≥ grade 2, bilirubin > 5 mg/dL, creatinine > 3 mg/dL, PVT, hepatic hydrothorax, advanced cancer, failure paracentesis | < 18 or > 75 yr, bilirubin > 10 mg/dL, INR > 2.5, PLT < 40000/mm3, creatinine > 3 mg/dL, HCC, complete PVT, cardiac or respiratory failure, organic renal failure, bacterial infection, and chronic HE | Bilirubin > 5 mg/dL, INR > 2, heart or renal failure, PVT, active bacterial infection, HE > grade 2, severe alcoholic hepatitis, HCC or incurable cancers, GI bleeding within 6 wk | > 72 yr, HE > grade 2, bilirubin > 6 mg/dL, Child-Pugh > 11, creatinine > 3 mg/dL, PVT, HCC, active bacterial infection, cardiac or pulmonary failure, GI bleeding within 15 d | > 70 yr, HE, HCC or other malignancy, PVT, active infection, severe cardiac or pulmonary disease, organic renal disease |
| Primary outcomes | Recurrence of ascites | Transplantation-free survival | Transplantation-free survival | Recurrence of ascites and transplantation-free survival | Transplantation-free survival | Overall survival |
| Secondary outcomes | Overall survival, HE, hemodynamic, liver and renal function | Recurrence of ascites, liver and renal function, HE | Recurrence of ascites, liver and renal function, HE, GI bleeding, HRS | Overall survival, HE, GI bleeding, liver and renal function, quality of life | Recurrence of ascites, HE, GI bleeding, liver and renal function, HRS | Recurrence of ascites, HE |
| Number of patients screened | NR | 155 | 119 | 525 | 137 | 78 |
| Randomized ratio | 1:01 | 1:01 | 1:01 | 1:01 | 1:01 | 1:01 |
| Number of patients randomized (total) | 25 | 60 | 70 | 109 | 66 | 60 |
| Number of participating centers | 1 | 2 | 4 | 6 | 3 | 1 |
| Mean follow-up time (TIPS/Para) | 7.5/12.4 | 45/44 | 9.5/10.8 | 41/38 | 21/15 | 27/13 |
RCT: Randomized controlled trial; NR: Not reported; TIPS: Transjugular intrahepatic portosystemic shunt; Para: Paracentesis; TP: Total paracentesis; LVP: Large-volume paracentesis; HE: Hepatic encephalopathy; PVT: Portal vein thrombosis; HVT: Hepatic vein thrombosis; HCC: Hepatocellular carcinoma; INR: International normalized ratio; PLT: Platelet count; GI: Gastrointestinal; HRS: Hepatorenal syndrome.
Five of the studies employed survival as the primary endpoint[8,9,11-13], and one study used recurrent ascites as such[10]. The frequencies of recurrence of ascites, HE, and liver transplantation were reported in all studies. Severe HE and hepatorenal syndrome were reported in four[8,10-12] and two trials[8,12], respectively.
Characteristics of patients in the selected trials
Table 2 summarizes the characteristics of the patients in the six selected trials. The number of randomized patients was at least 60 in all trials except for the study by Lebrec et al[10], which only enrolled 25 patients. The percentage of Child-Pugh C patients was 26%-33% in four studies[8-10,13], and 76% in the study by Salerno et al[12]. Baseline serum concentrations of bilirubin, albumin, creatinine, and sodium were not significantly different between the TIPS and paracentesis groups in all studies.
Table 2.
Characteristics of the patients in the included studies
| Patient characteristics | Lebrec et al[10] | Rössle et al[9] | Ginès et al[8] | Sanyal et al[11] | Salerno et al[12] | Narahara et al[13] |
| Number of randomized patients | 12/13 | 29/31 | 35/35 | 52/57 | 33/33 | 30/30 |
| Age, yr (mean) | 50/52 | 58/61 | 59/56 | 56/52 | 58/60 | 58/61 |
| Percentage of refractory ascites (total) | 100/100 (100) | 58/52 (55) | 100/100 (100) | 100/100 (100) | 72/64 (75) | 100/100 (100) |
| Percentage men (total) | 77/66 (72) | 72/68 (70) | 69/74 (71) | 63/70 (66) | 72/76 (74) | 77/70 (73) |
| Percentage alcohol-induced cirrhosis (total) | 77/83 (80) | 83/74 (78) | 51/60 (56) | 62/58 (60) | 45/39 (42) | 37/33 (35) |
| Percentage Child-Pugh class C (total) | 31/33 (32) | 38/22 (30) | 37/43 (26) | NR | 79/73 (76) | 37/30 (33) |
| Mean Child-Pugh score | 9.3/9.2 | 9.1/8.7 | 9.3/9.2 | 9.2/9.3 | 9.4/9.4 | 8.9/8.9 |
| Percentage with HE (total) | 15/17 (16) | 46/39 (40) | 37/40 (39) | NR | 27/21 (24) | 10/7 (8) |
| Percentage with previous GI bleeding (total) | NR | NR | 34/23 (29) | 23/25 (24) | 18/21 (20) | NR |
| Serum bilirubin, mg/dL | 2.04 ± 0.5/1.57 ± 0.2 | 1.8 ± 1.2/1.8 ± 1.0 | 2.0 ± 0.2/2.4 ± 0.3 | 1.9 ± 1.2/1.9 ± 1.4 | 1.7 ± 0.15/1.9 ± 0.24 | 1.3 ± 0.7/1.4 ± 0.7 |
| Serum albumin, g/dL | 3.0 ± 0.1/3.1 ± 0.2 | 3.5 ± 0.6/3.5 ± 0.4 | 2.8 ± 0.1/3.0 ± 0.1 | 2.9 ± 0.4/2.7 ± 0.4 | 2.9 ± 0.7/2.9 ± 0.8 | 2.7 ± 0.5/2.7 ± 0.6 |
| Serum creatinine, mg/dL | 0.9 ± 0.7/0.9 ± 0.6 | 1.3 ± 0.4/1.4 ± 0.9 | 1.4 ± 0.1/1.4 ± 0.1 | 1.1 ± 0.3/1.0 ± 0.3 | 1.12 ± 0.06/1.15 ± 0.09 | 1.03 ± 0.30/1.03 ± 0.35 |
| Serum sodium, mmol/L | 130 ± 2/130 ± 2 | 130 ± 6/131 ± 6 | 129 ± 1/130 ± 1 | NR | 133 ± 1/133 ± 1 | 134 ± 7/133 ± 5 |
All of the comparisons between groups were not statistically significant (P > 0.05) in any of the included studies. TIPS: Transjugular intrahepatic portosystemic shunt; HE: Hepatic encephalopathy; NR: Not reported; GI: Gastrointestinal.
Technical results
Table 3 presents the technical results of the included RCTs. The TIPS technical success rate was at least 89% in five studies[8,9,11-13] but was only 77% in the study by Lebrec et al[10]. The average post-TIPS PSGs were 14 mmHg in one study[10], and lower than 12 mmHg in all others[8,9,11-13]. Severe procedure-related complications were reported in three trials, including cardiac arrhythmias[10], hemolytic anemia[8], and cerebrovascular embolism[12]. The proportions of TIPS dysfunction ranged from 30% to 87%. The TIPS-assisted patency rates were higher than 80% in five studies[8,9,11-13]. However, more than 50% of the TIPS patients in the study by Lebrec et al[10] did not have TIPS-assisted patency during the follow-up.
Table 3.
Technical results of the included studies
| Technical results | Lebrec et al[10] | Rössle et al[9] | Ginès et al[8] | Sanyal et al[11] | Salerno et al[12] | Narahara et al[13] |
| Successful stent placement (n/randomized) | 10/13 (77) | 29/29 (100) | 34/35 (97) | 49/52 (94) | 29/33 (89) | 30/30 (100) |
| PSG change, mmHg | From 20 ± 1 to 14 ± 1 | From 24 ± 6 to 10 ± 4 | From 19.1 ± 0.8 to 8.7 ± 0.4 | From 19.8 ± 4.8 to 8.3 ± 3.6 | From 22.5 ± 1.1 to 8.7 ± 0.6 | From 20.3 ± 4.6 to 8.5 ± 4.7 |
| Severe TIPS procedure-related complications | 1 severe cardiac arrhythmias | None | 3 severe hemolytic anemia | NR | 1 cerebrovascular embolism | None |
| TIPS dysfunction | 3/10 (30) | 13/29 (45) | 13/34 (38) | 34/49 (70) | 12/29 (41) | 26/30 (87) |
| Irreversible stent obstruction | 1/10 (10) | 2/29 (7) | 1/34 (3) | NR | 2/29 (7) | 2/30 (7) |
| TIPS-assisted patency, (n/randomized) | 6/13 (46) | 27/29 (93) | 32/35 (91) | > 90% | 27/33 (82) | 26/30 (86) |
| Patients crossed over from paracentesis to TIPS | NR | 10/31 (32) | 3/35 (9) | 2/57 (4) | 11/33 (33) | 6/30 (20) |
| TIPS patency surveillance | Doppler sonography | Doppler sonography | Hepatic vein catheterization if ascites recurred | Angiography | Doppler sonography | Doppler sonography |
Data are expressed as absolute numbers (percentage) or mean ± SD. TIPS: Transjugular intrahepatic portosystemic shunt; PSG: Portosystemic pressure gradient.
Risk of bias assessment
All of the studies were unblinded to participants, personnel, and outcome assessment, employed intention-to-treat analysis with description of drop-outs, did not demonstrate the method of generation of random allocation sequence, and reported all of the outcomes described in the methods section (Table 4). The study by Rössle et al[9] did not state the concealment of the allocation sequence, while the others concealed the randomization numbers with sealed opaque envelopes (Table 4)[8,10-13].
Table 4.
Risk of bias assessment of the included studies
| Risk of bias | Lebrec et al[10] | Rössle et al[9] | Ginés et al[8] | Sanyal et al[11] | Salerno et al[12] | Narahara et al[13] |
| Generation of random allocation sequence (risk) | NR (unclear) | NR (unclear) | NR (unclear) | NR (unclear) | NR (unclear) | NR (unclear) |
| Concealment of allocation sequence (risk) | Sealed opaque envelopes (low) | NR (unclear) | Sealed opaque envelopes (low) | Sealed opaque envelopes (low) | Sealed opaque envelopes (low) | Sealed opaque envelopes (low) |
| Blinding of participants and personnel (risk) | Unblinded (high) | Unblinded (high) | Unblinded (high) | Unblinded (high) | Unblinded (high) | Unblinded (high) |
| Blinding of outcome assessment (risk) | Unblinded (high) | Unblinded (high) | Unblinded (high) | Unblinded (high) | Unblinded (high) | Unblinded (high) |
| Incomplete outcome data (risk) | Intention-to-treat analysis, description of drop-outs (low) | Intention-to-treat analysis, description of drop-outs (low) | Intention-to-treat analysis, description of drop-outs (low) | Intention-to-treat analysis, description of drop-outs (low) | Intention-to-treat analysis, description of drop-outs (low) | Intention-to-treat analysis, description of drop-outs (low) |
| Selective outcome reporting (risk) | All of the outcomes in the methods section were reported in the results section (low) | All of the outcomes in the methods section were reported in the results section (low) | All of the outcomes in the methods section were reported in the results section (low) | All of the outcomes in the methods section were reported in the results section (low) | All of the outcomes in the methods section were reported in the results section (low) | All of the outcomes in the methods section were reported in the results section (low) |
NR: Not reported.
LTF survival
LTF survival was directly reported in four studies[8,9,11,12]. Because no patient underwent liver transplantation during the follow-up in the study by Narahara et al[13], the LTF survival in this study was certainly equal to the overall survival. Thus, the HRs for LTF survival were available in five RCTs[8,9,11-13]. Compared with the paracentesis group, the LTF survival of the patients in the TIPS group was significantly increased in two studies[12,13], was almost significantly increased in one study[9], and was nearly equivalent in two studies[8,11]. After pooling the five studies with 365 patients, the estimated LTF survival was significantly in favor of the TIPS group using a fixed-effects model (HR = 0.61, 95%CI: 0.46-0.82, P < 0.001) without significant heterogeneity (I2 = 19%, P value for heterogeneity = 0.30, Figure 2).
Figure 2.
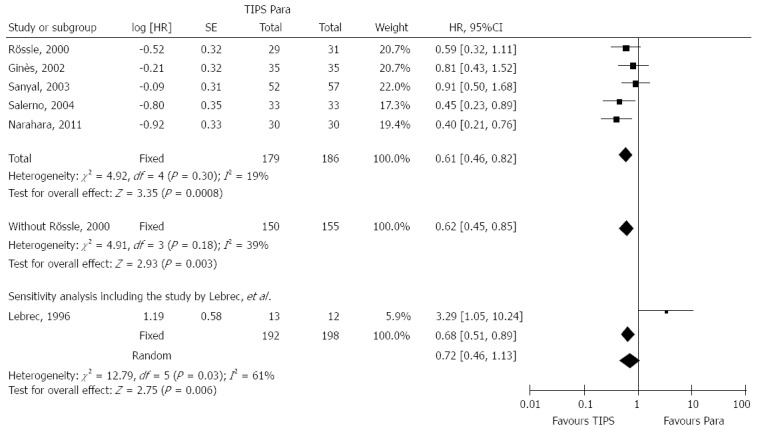
Liver transplantation-free survival in trials compared transjugular intrahepatic portosystemic shunt with paracentesis. Forest plots represent HR and 95%CI. TIPS: Transjugular intrahepatic portosystemic shunt.
In the study by Lebrec et al[10] patient LTF survival was not assessed. Only one patient in the paracentesis group underwent liver transplantation during follow-up. Thus, the estimated LTF survival of the patients in the paracentesis group would be higher than the overall survival, and the estimated LTF survival of the patients in the TIPS group would be similar to the overall survival. Therefore, we performed an additional sensitivity analysis that included the overall survival of this study to estimate a conservative pooled HR for LTF survival. The results significantly favored the TIPS group that underwent fixed-effect modeling (HR = 0.68, 95%CI: 0.51-0.89, P = 0.006, Figure 2) and tended to favor the TIPS group that underwent random-effect modeling (HR = 0.72, 95%CI: 0.46-1.13, P = 0.16, I2 = 61%, P value for heterogeneity = 0.03, Figure 2).
The subgroup analysis that included the two studies with both refractory and recidivant ascites patients[9,12] demonstrated that LTF survival significantly favored TIPS without significant heterogeneity (HR = 0.52, 95%CI: 0.33-0.83, P = 0.006, I2 = 0%, P value for heterogeneity = 0.55, Figure 3). Furthermore, the subgroup analysis that included the three studies with only refractory ascites patients[8,11,13] also demonstrated that LTF survival significantly favored TIPS without significant heterogeneity (HR = 0.68, 95%CI: 0.47-0.97, P = 0.04, I2 = 48%, P value for heterogeneity = 0.15, Figure 3).
Figure 3.
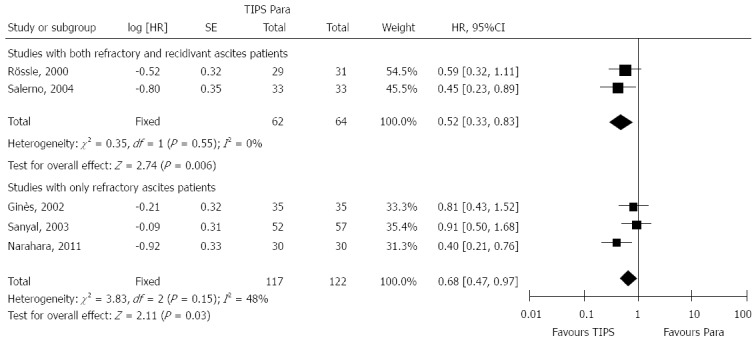
Subgroup analyses of liver transplantation-free survival in trials compared transjugular intrahepatic portosystemic shunt with paracentesis. Forest plots represent HR and 95%CI. TIPS: Transjugular intrahepatic portosystemic shunt.
Other outcomes
The proportions of liver disease-related death were 30% and 40% in the TIPS and paracentesis groups, respectively. The OR of liver disease-related death was 0.62 without significant heterogeneity (95%CI: 0.39-0.98, P = 0.04, I2 = 31%, P value for heterogeneity = 0.21, Table 5). The pooled proportions of non-liver disease-related death were not significant different between the two groups (OR = 1.27, 95%CI: 0.68-2.38, P = 0.46, I2 = 0%, P value for heterogeneity = 0.64, Table 5).
Table 5.
Results of each study and pooled estimations of recurrence of ascites, hepatic encephalopathy, severe hepatic encephalopathy, gastrointestinal bleeding and hepatorenal syndrome by sensitivity analysis
| Ref. |
Liver-transplantation |
Liver-disease-related mortality |
Non-liver-disease-related mortality |
Recurrence ascites |
HE |
Severe HE |
Hepatorenal syndrome |
||||||||||||||
| TIPS | Para | OR (95%CI) | TIPS | Para | OR (95%CI) | TIPS | Para | OR (95%CI) | TIPS | Para | OR (95%CI) | TIPS | Para | OR (95%CI) | TIPS | Para | OR (95%CI) | TIPS | Para | OR (95%CI) | |
| Lebrec et al[10] | 0/13 | 1/12 | 0.28 (0.01-7.67) | 41438 | 4/12 | 1.71 (0.34-8.68) | 3/13 | 0/12 | 8.33 (0.39-180.36) | 10/13 | 11/12 | 0.30 (0.03-3.41) | 3/13 | 0/12 | 8.33 (0.39-180.36) | 2/13 | 0/12 | 5.43 (0.24-125.59) | - | - | - |
| Rössle et al[9] | 0 | 2/31 | 0.52 (0.04-6.04) | 10/29 | 20/31 | 0.29 (0.10-0.84) | 5/29 | 3/31 | 1.94 (0.42-8.99) | 14/29 | 26/31 | 0.18 (0.05-0.60) | 6/29 | 3/31 | 2.43 (0.55-10.82) | - | - | - | - | - | - |
| Ginés et al[8] | 7/35 | 7/35 | 1.00 (0.31-3.23) | - | - | - | - | - | - | 17/35 | 29/35 | 0.20 (0.06-0.59) | 27/35 | 23/35 | 1.76 (0.61-5.05) | 21/35 | 12/35 | 2.88 (1.09-7.60) | 3/35 | 11/35 | 0.20 (0.05-0.81) |
| Sanyal et al[11] | 16/52 | 17/57 | 1.05 (0.46-2.37) | 13/52 | 13/57 | 1.13 (0.47-2.72) | 5/52 | 6/57 | 0.90 (0.26-3.16) | 22/52 | 48/57 | 0.14 (0.06-0.34) | 22/52 | 13/57 | 2.48 (1.08-5.68) | 15/52 | 10/57 | 1.91 (0.77-4.73) | - | - | - |
| Salerno et al[12] | 4/33 | 4/33 | 1.00 (0.23-4.39) | 10/33 | 16/33 | 0.46 (0.17-1.27) | 3/33 | 4/33 | 0.72 (0.15-3.53) | 13/33 | 32/33 | 0.02 (0.00-0.17) | 20/33 | 13/33 | 2.37 (0.88-6.35) | 14/33 | 10/33 | 1.69 (0.61-4.67) | 3/33 | 5/33 | 0.56 (0.12-2.56) |
| Narahara et al[13] | 0/30 | 0/30 | - | 8/30 | 13/30 | 0.48 (0.16-1.41) | 9/30 | 8/30 | 1.18 (0.38-3.63) | 22/30 | 27/30 | 0.31 (0.07-1.29) | 20/30 | 5/30 | 10.00 (2.94-34.01) | - | - | - | - | - | - |
| Total | 28/192 | 31/198 | 0.94 (0.53-1.67) | 47/157 | 66/163 | 0.62 (0.39-0.98)a | 25/157 | 21/163 | 1.27 (0.68-2.38) | 98/192 | 173/198 | 0.15 (0.09-0.24)b | 98/192 | 57/198 | 2.95 (1.87-4.66)b | 52/133 | 32/137 | 2.18 (1.27-3.76)b | 6/68 | 16/68 | 0.32 (0.12-0.86)a |
| Subgroup without the study by Lebrec et al, 1996 | 28/179 | 30/186 | 0.98 (0.54-1.77) | 41/144 | 62/151 | 0.56 (0.34-0.91)a | 22/144 | 21/151 | 1.11 (0.57-2.14) | 88/179 | 162/186 | 0.14 (0.08-0.24)b | 95/179 | 57/186 | 2.86 (1.80-4.54)b | 50/120 | 32/125 | 2.10 (1.21-3.67)b | - | - | - |
P < 0.05,
P < 0.01; No significant heterogeneity was observed among these meta-analyses (I2 = 0%-31%). All of these meta-analyses were performed under the fixed-effect model. TIPS: Transjugular intrahepatic portosystemic shunt; Para: Paracentesis; HE: Hepatic encephalopathy.
The proportions of patients who underwent liver transplantation ranged from 0% to 30%[8-12]. No significant difference was observed between the TIPS and the paracentesis groups in the numbers of patients who underwent liver transplantation (OR = 0.94, 95%CI: 0.53-1.67, P = 0.83, I2 = 0%, P value for heterogeneity = 0.94, Table 5).
TIPS was significantly more effective in the reduction of recurrent ascites than paracentesis in four of the included RCTs[8,9,11,12] but was not significantly more effective in the other two studies[10,13]. The overall proportions of patients with recurrent ascites were 51% for the TIPS group and 87% for the paracentesis group (OR = 0.15, 95%CI: 0.09-0.24, P < 0.001). Values for this variable showed no statistically significant heterogeneity (I2 = 2%, P value for heterogeneity = 0.40, Table 5).
HE occurred more frequently in the patients who underwent TIPS procedures (51% vs 29%). The OR of any degree of HE between the two groups was 2.95 (95%CI: 1.87-4.66, P < 0.001) without significant heterogeneity (I2 = 11%, P value for heterogeneity = 0.35, Table 5). Patients treated with TIPS presented a significantly higher risk of severe HE than those treated with paracentesis (39% vs 23%, OR = 2.18, 95%CI: 1.27-3.76, P = 0.005, Table 5).
Hepatorenal syndrome was assessed in two studies with 136 patients[8,12] and was less frequently observed in the TIPS group (9% vs 24%, OR = 0.32, 95%CI: 0.12-0.86, P = 0.02, I2 = 0%, P value for heterogeneity = 0.34, Table 5).
Potential outlier studies and sensitivity analyses
The study by Lebrec et al[10] was considered an outlier for the following two reasons: (1) it was the only trial that employed survival as a secondary endpoint; and (2) it achieved the lowest successful TIPS placement rate, the highest post-TIPS PSG, and the lowest TIPS-assisted patency rate, which indicated a less refined TIPS technique compared with the subsequent trials published 4-15 years later[6,8,9,11-13]. Sensitivity analyses that excluded this trial yielded very similar results (Figure 2, Table 5).
DISCUSSION
This updated meta-analysis, including appropriate survival analysis of six RCTs, shows that TIPS significantly improves LTF survival and decreases the risk of liver disease-related death in cirrhotic patients with refractory ascites. Additionally, the rates of recurrent ascites and hepatorenal syndrome were significantly reduced, but the risk of HE was significantly increased in the patients who underwent TIPS in comparison to those who underwent paracentesis.
Four previously reported meta-analyses only evaluated the number of deaths without considering the effect of time to death. All of them showed similar mortality between the TIPS group and the paracentesis group[6,14-16]. According to the PRISMA Statement, the HR is the most appropriate measure to be pooled, because both the number of deaths and the time to the death are important to time-to-event outcomes[21]. For example, in the meta-analysis by D’Amico et al[6], the pooled mortality was not significantly different (OR = 0.90, 95%CI: 0.44-1.81). Despite excluding the outlier RCT by Lebrec et al[10] which was the only trial that favored paracentesis on survival, the pooled mortality of the remaining four RCTs was still not significantly different (OR = 0.74, 95%CI: 0.40-1.37)[6]. However, if the HRs of the same four RCTs were pooled, the benefit of TIPS on survival was significant (HR = 0.68, 95%CI: 0.50-0.94). This heterogeneity suggested that these two groups of patients had similar numbers of deaths but different survival times. Thus, the HRs were pooled in our present meta-analysis[20,21]. Conversely, because liver transplantation has a very important role in the survival of patients with end-stage liver cirrhosis, this meta-analysis evaluated LTF survival, which isolated the important effect of liver transplantation on survival.
The accumulated LTF survival was available for five of the six included RCTs[8,9,11-13]. All five of these trials evaluated LTF survival using a Kaplan-Meier curve and log-rank test, which gave us facilities to estimate survival difference between the TIPS group and the paracentesis group by pooling the HRs.
After pooling the HRs of the five RCTs, the estimated LTF survival was significantly improved by TIPS compared with paracentesis. Similar improvements were observed when the study by Lebrec et al[10] was excluded as an outlier. Furthermore, two of the six RCTs included patients with recidivant ascites (three recurrences of ascites within 12 mo), which represents an earlier stage and has a potentially better prognosis than patients with refractory ascites (recurrence within 4 wk)[23]. Thus, subgroup analyses were performed and showed that TIPS significantly improved LTF survival regardless of if recidivant ascites patients were included or not in the trials.
In a previous study that showed relatively poor survival with TIPS[10], the technical failure rate was more than two-fold higher than the remaining five RCTs (23% vs < 11%)[8,9,11-13], and all three of the patients with unsuccessful TIPS procedures died within 3 mo after TIPS. All of these characteristics obviously had a negative contribution to the survival of the TIPS group. We pooled the overall survival of this study in a sensitivity analysis to demonstrate a conservative result, which also showed an improvement of LTF survival in the TIPS group. All of these results suggest that TIPS could improve LTF survival in selected cirrhotic patients with refractory ascites.
An improvement of LTF survival was also reported in a previous meta-analysis that pooled individual patient data from four RCTs[17]. The present study confirmed the effect of TIPS on LTF survival with appropriate survival analysis by pooling data from the literature from six available RCTs. The consistency of survival improvement in these two meta-analyses with different methods makes us more confident that TIPS can do better than paracentesis in the management of refractory ascites.
The improvement of LTF survival in the patients who underwent a TIPS procedure is mostly attributed to the reduction of liver disease-related deaths, especially deaths related to severe complications of portal hypertension. Three studies reported the number of deaths caused by massive variceal bleeding, and all three of the studies showed a lower risk of this type of death in the TIPS group[9-11]. Another cause of the improved LTF survival is that TIPS prolonged the time to liver transplantation, which was reported by two of the enrolled trials[11,12].
TIPS dramatically reduced the incidence of recurrent ascites in the present meta-analysis. This result was consistent with the results of previous meta-analyses[6,14-17]. TIPS procedure also has a positive effect on renal function[2,24]. Thus, it is reasonable that the risk of developing hepatorenal syndrome was reduced by TIPS by more than a half when compared to paracentesis (from 24% to 9%). Because spontaneous bacterial peritonitis and hyponatremia occur more frequently in patients with ascites, TIPS most likely can reduce these events by eliminating the ascites and improving renal function[4,17]. Because hepatorenal syndrome, spontaneous bacterial peritonitis, and hyponatremia are usually associated with high mortality, TIPS most likely improves patient survival by reducing these complications[4,17].
Furthermore, the pooled results showed that TIPS increased the risk of HE and severe HE by almost two-fold in comparison to paracentesis (HE: 51% vs 29%, severe HE: 39% vs 23%). Similar results were also found in the sensitivity analyses. Although almost all of the post-TIPS HE cases could be successfully managed by medical treatment[8-13,25,26], the reduction level of PSG should be considered with caution, especially in patients with high post-TIPS HE risk (old age, previous HE or high Child-Pugh class)[27-29].
One limitation of this meta-analysis is that all of the included RCTs were designed as open-label trials, which could most likely bias the results by affecting the judgment of actual outcomes, especially subjective outcomes (i.e., HE)[30]. Because blinding is unavailable for these two obviously different interventions, the results presented are most likely the highest quality evidence we can currently obtain. Furthermore, only one of the six RCTs provided raw data by Child-Pugh class[8]. Thus, the subgroup analysis according to liver function is not evaluated in this meta-analysis. However, patient survival was improved by TIPS in both the study including a high proportion of Child-Pugh C patients (76%)[12] and the study including a low proportion of Child-Pugh C patients (33%)[12]. This result indicates that TIPS may be superior to paracentesis regardless of Child-Pugh classes. Additionally, only 48% (median, 21% to 77%, Table 1) of the screened patients could be included in the RCTs, which suggests that studies based on real clinical practice scenarios are needed to validate the universal nature of the results of the present meta-analysis.
In conclusion, this updated meta-analysis of data from six RCTs shows that TIPS significantly improves the LTF survival, the control of refractory ascites, and the prevention of hepatorenal syndrome in patients with cirrhosis and refractory ascites. The increased risk of HE is a major drawback of the TIPS procedure. Further studies based on real clinical practice scenarios are needed.
COMMENTS
Background
The survival benefit of transjugular intrahepatic portosystemic shunt (TIPS) in cirrhotic patients with refractory ascites requires further evaluations. Previous meta-analyses of the data reported in the literature considered only the number of deaths, but not the time to death. Furthermore, an additional study on this subject has been recently published. The primary aim of the present study is to compare the liver transplantation-free (LTF) survival between TIPS and paracentesis groups by pooling the effects of both number of deaths and time to death.
Research frontiers
A meta-analysis was conducted to evaluate the effectiveness of TIPS vs paracentesis in patients with cirrhosis and refractory ascites.
Innovations and breakthroughs
In the present meta-analysis of randomized controlled trials, it was observed that TIPS significantly improved the LTF survival of patients with cirrhosis and refractory ascites. Additionally, TIPS was superior to paracentesis in terms of liver disease-related death, recurrence of ascites, and hepatorenal syndrome. However, patients who underwent TIPS were associated with an increased risk of hepatic encephalopathy (HE) and severe HE.
Applications
The results of the present meta-analysis suggest that TIPS could potentially be recommended as the first-line treatment for patients with cirrhosis and refractory ascites.
Terminology
LTF survival (primary endpoint): patient survival without liver transplantation. Liver-disease-related death: number of patients who died of liver-disease-related causes including hepatic failure, variceal bleeding, hepatorenal syndrome, and hepatocellular carcinoma. Recurrence of ascites: number of patients requiring a new paracentesis after the interventions. HE and severe HE: the number of patients presenting with HE after intervention and the number of patients with severe HE (grades III/IV HE or equivalent classification), respectively. Hepatorenal syndrome: number of patients with type 1 or type 2 hepatorenal syndrome.
Peer review
The effects of TIPS vs paracentesis for patients with cirrhosis and refractory ascites have been investigated for more than two decades. The present meta-analysis included the updated data and found that TIPS could improve the LTF survival rate and alleviate recurrence of ascites, hepatorenal syndrome, and liver disease-related death alone with an increase in HE risk. The paper is exciting and important and brings forth new knowledge.
Footnotes
P- Reviewer: Busk TM S- Editor: Zhai HH L- Editor: Wang TQ E- Editor: Ma S
References
- 1.Arroyo V, Colmenero J. Ascites and hepatorenal syndrome in cirrhosis: pathophysiological basis of therapy and current management. J Hepatol. 2003;38 Suppl 1:S69–S89. doi: 10.1016/s0168-8278(03)00007-2. [DOI] [PubMed] [Google Scholar]
- 2.Rössle M, Gerbes AL. TIPS for the treatment of refractory ascites, hepatorenal syndrome and hepatic hydrothorax: a critical update. Gut. 2010;59:988–1000. doi: 10.1136/gut.2009.193227. [DOI] [PubMed] [Google Scholar]
- 3.Salerno F, Guevara M, Bernardi M, Moreau R, Wong F, Angeli P, Garcia-Tsao G, Lee SS. Refractory ascites: pathogenesis, definition and therapy of a severe complication in patients with cirrhosis. Liver Int. 2010;30:937–947. doi: 10.1111/j.1478-3231.2010.02272.x. [DOI] [PubMed] [Google Scholar]
- 4.European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397–417. doi: 10.1016/j.jhep.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Runyon BA. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009;49:2087–2107. doi: 10.1002/hep.22853. [DOI] [PubMed] [Google Scholar]
- 6.D’Amico G, Luca A, Morabito A, Miraglia R, D’Amico M. Uncovered transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis. Gastroenterology. 2005;129:1282–1293. doi: 10.1053/j.gastro.2005.07.031. [DOI] [PubMed] [Google Scholar]
- 7.Ochs A, Rössle M, Haag K, Hauenstein KH, Deibert P, Siegerstetter V, Huonker M, Langer M, Blum HE. The transjugular intrahepatic portosystemic stent-shunt procedure for refractory ascites. N Engl J Med. 1995;332:1192–1197. doi: 10.1056/NEJM199505043321803. [DOI] [PubMed] [Google Scholar]
- 8.Ginès P, Uriz J, Calahorra B, Garcia-Tsao G, Kamath PS, Del Arbol LR, Planas R, Bosch J, Arroyo V, Rodés J. Transjugular intrahepatic portosystemic shunting versus paracentesis plus albumin for refractory ascites in cirrhosis. Gastroenterology. 2002;123:1839–1847. doi: 10.1053/gast.2002.37073. [DOI] [PubMed] [Google Scholar]
- 9.Rössle M, Ochs A, Gülberg V, Siegerstetter V, Holl J, Deibert P, Olschewski M, Reiser M, Gerbes AL. A comparison of paracentesis and transjugular intrahepatic portosystemic shunting in patients with ascites. N Engl J Med. 2000;342:1701–1707. doi: 10.1056/NEJM200006083422303. [DOI] [PubMed] [Google Scholar]
- 10.Lebrec D, Giuily N, Hadengue A, Vilgrain V, Moreau R, Poynard T, Gadano A, Lassen C, Benhamou JP, Erlinger S. Transjugular intrahepatic portosystemic shunts: comparison with paracentesis in patients with cirrhosis and refractory ascites: a randomized trial. French Group of Clinicians and a Group of Biologists. J Hepatol. 1996;25:135–144. doi: 10.1016/s0168-8278(96)80065-1. [DOI] [PubMed] [Google Scholar]
- 11.Sanyal AJ, Genning C, Reddy KR, Wong F, Kowdley KV, Benner K, McCashland T. The North American Study for the Treatment of Refractory Ascites. Gastroenterology. 2003;124:634–641. doi: 10.1053/gast.2003.50088. [DOI] [PubMed] [Google Scholar]
- 12.Salerno F, Merli M, Riggio O, Cazzaniga M, Valeriano V, Pozzi M, Nicolini A, Salvatori F. Randomized controlled study of TIPS versus paracentesis plus albumin in cirrhosis with severe ascites. Hepatology. 2004;40:629–635. doi: 10.1002/hep.20364. [DOI] [PubMed] [Google Scholar]
- 13.Narahara Y, Kanazawa H, Fukuda T, Matsushita Y, Harimoto H, Kidokoro H, Katakura T, Atsukawa M, Taki Y, Kimura Y, et al. Transjugular intrahepatic portosystemic shunt versus paracentesis plus albumin in patients with refractory ascites who have good hepatic and renal function: a prospective randomized trial. J Gastroenterol. 2011;46:78–85. doi: 10.1007/s00535-010-0282-9. [DOI] [PubMed] [Google Scholar]
- 14.Saab S, Nieto JM, Lewis SK, Runyon BA. TIPS versus paracentesis for cirrhotic patients with refractory ascites. Cochrane Database Syst Rev. 2006;(1):CD004889. doi: 10.1002/14651858.CD004889.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deltenre P, Mathurin P, Dharancy S, Moreau R, Bulois P, Henrion J, Pruvot FR, Ernst O, Paris JC, Lebrec D. Transjugular intrahepatic portosystemic shunt in refractory ascites: a meta-analysis. Liver Int. 2005;25:349–356. doi: 10.1111/j.1478-3231.2005.01095.x. [DOI] [PubMed] [Google Scholar]
- 16.Albillos A, Bañares R, González M, Catalina MV, Molinero LM. A meta-analysis of transjugular intrahepatic portosystemic shunt versus paracentesis for refractory ascites. J Hepatol. 2005;43:990–996. doi: 10.1016/j.jhep.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 17.Salerno F, Cammà C, Enea M, Rössle M, Wong F. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology. 2007;133:825–834. doi: 10.1053/j.gastro.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 18.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. 2011. Available from: http://www.cochrane-handbook.org.
- 19.Conn HO, Liebertal MM. The hepatic coma syndromes and lactulose. Baltimore: Williams & Wilkins; 1979. [Google Scholar]
- 20.Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. doi: 10.1186/1745-6215-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151:W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 22.Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17:2815–2834. doi: 10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 23.Arroyo V, Ginès P, Gerbes AL, Dudley FJ, Gentilini P, Laffi G, Reynolds TB, Ring-Larsen H, Schölmerich J. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. International Ascites Club. Hepatology. 1996;23:164–176. doi: 10.1002/hep.510230122. [DOI] [PubMed] [Google Scholar]
- 24.Arroyo V, Fernández J. Management of hepatorenal syndrome in patients with cirrhosis. Nat Rev Nephrol. 2011;7:517–526. doi: 10.1038/nrneph.2011.96. [DOI] [PubMed] [Google Scholar]
- 25.Boyer TD, Haskal ZJ. The role of transjugular intrahepatic portosystemic shunt in the management of portal hypertension. Hepatology. 2005;41:386–400. doi: 10.1002/hep.20559. [DOI] [PubMed] [Google Scholar]
- 26.Boyer TD, Haskal ZJ. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in the Management of Portal Hypertension: update 2009. Hepatology. 2010;51:306. doi: 10.1002/hep.23383. [DOI] [PubMed] [Google Scholar]
- 27.Zuckerman DA, Darcy MD, Bocchini TP, Hildebolt CF. Encephalopathy after transjugular intrahepatic portosystemic shunting: analysis of incidence and potential risk factors. AJR Am J Roentgenol. 1997;169:1727–1731. doi: 10.2214/ajr.169.6.9393198. [DOI] [PubMed] [Google Scholar]
- 28.Riggio O, Angeloni S, Salvatori FM, De Santis A, Cerini F, Farcomeni A, Attili AF, Merli M. Incidence, natural history, and risk factors of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt with polytetrafluoroethylene-covered stent grafts. Am J Gastroenterol. 2008;103:2738–2746. doi: 10.1111/j.1572-0241.2008.02102.x. [DOI] [PubMed] [Google Scholar]
- 29.Bai M, Qi X, Yang Z, Yin Z, Nie Y, Yuan S, Wu K, Han G, Fan D. Predictors of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in cirrhotic patients: a systematic review. J Gastroenterol Hepatol. 2011;26:943–951. doi: 10.1111/j.1440-1746.2011.06663.x. [DOI] [PubMed] [Google Scholar]
- 30.Wood L, Egger M, Gluud LL, Schulz KF, Jüni P, Altman DG, Gluud C, Martin RM, Wood AJ, Sterne JA. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ. 2008;336:601–605. doi: 10.1136/bmj.39465.451748.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]


