Abstract
Aim
This paper is a report of an international study of barriers to asthma care from the perspectives of school nurses in Reykjavik, Iceland and St. Paul, Minnesota, in the context of their schools, communities and countries.
Background
Globally, asthma affects the health and school performance of many adolescents. School nurses play a key role by providing care to adolescents with asthma in school settings. Understanding universal barriers to asthma management in schools is important for developing interventions that are effective in multiple societal contexts.
Design
Exploratory, descriptive study.
Methods
Parallel studies were conducted from September 2008 - January 2009, through six focus groups among school nurses (N=32, in Reykjavik n=17 and St. Paul n=15) who were managing asthma in adolescents. Focus groups were audio-recorded and transcribed verbatim in English or Icelandic. The Icelandic transcripts were translated into English. Descriptive content analytic techniques were used to systematically identify and categorize types of barriers to asthma care.
Results
School nurses in both countries identified common barriers such as time constraints, communication challenges and school staff barriers. The primary difference was that St. Paul school nurses identified more socioeconomic and health access barriers than school nurses in Reykjavik.
Conclusion
Greater cultural and linguistic diversity and socioeconomic differences in the student population in St. Paul and lack of universal health care coverage in the U.S. contributed to school nurses’ need to focus more on asthma management than school nurses in Reykjavik, who were able to focus more on asthma prevention and education.
Keywords: School nurse roles, asthma management by school nurses, barriers to care in school nursing
INTRODUCTON
Asthma is a major global health problem among children and adolescents. A sharp increase has been reported over the last decades in morbidity, mortality and economic burden associated with asthma in children (Global Initiative for Asthma 2010). About 7 million children in the U.S. were reported as ever having a diagnosis of asthma and over 4 million reported experiencing an asthma episode or attack during the previous 12 months (Akinbami et al. 2009). Asthma rates are high in Iceland as well. Despite Iceland being a low allergen country with the absence of dust mites, low pet ownership and relatively low pollen counts (Clausen et al. 2008), rates among school children with asthma in Iceland are 9% (Clausen et al. 2002, Gudbjornsdottir et al. 2009) compared with 14% among American children (Centers for Disease Control and Prevention [CDC] 2009).
Worldwide, asthma affects functioning of many children and adolescents. Youth with asthma are more likely to have their activities restricted and miss days of school (Mizan et al. 2011, Pruitt et al. 2009) and their academic performance and health related quality of life (HRQOL) affected (Moonie et al. 2008, Svavarsdottir et al. 2011, Taras et al. 2004) and even to experience depression (Burkhart et al. 2009). However, research suggests that if children receive evidence-based care that includes school health services, the rate of school attendance among children with asthma can equal that of children without asthma (Millard et al. 2009, Splett et al. 2006).
Children and adolescents with asthma are the largest group of children with chronic illness attending schools and in many countries, nurses play a key role in providing care to children with asthma in the school setting. An examination of the literature reveals that there are some known barriers to optimum care of children with asthma at multiple system levels, but findings are largely situated in the context of single geographic regions or countries.
An ecological framework was used to identify and compare individual student and systems level barriers to asthma care identified by school nurses in Reykjavik, Iceland and St. Paul, Minnesota. In the ecological systems framework, the school is one of several microsystems within which the individual student with asthma exists, other microsystems include the family (home), health care systems and community-level contexts. The connections and processes between two microsystems (e.g., family and school) represent a mesosystem, the broader social, political and cultural contexts comprise the macrosystem (Bronfenbrenner 1979). School nurse asthma management primarily occurs in connections between nested systems. The broader macrosystem also influences the management provided. The ecological framework informed the development of the focus group interview guide and the cross country analysis. In this paper, we explore barriers to asthma management for youth in schools in two Western nations with a focus on the interactions of school nurses with individual students, families, communities and school and health care systems.
Background
Individual, family, school, community and health care setting
Researchers have found that nurses identified families as presenting barriers to effective asthma care in school (Getch & Neuharth-Pritchett 2009, Kielb et al. 2007, Winkelstein et al., 2006). These studies included reports of high levels of outside emergency calls attributed to parents and children who were uneducated about asthma, who underestimated its severity and consequences and who did not have rescue medicine available at school (Major et al. 2006). Forbis et al. (2006) reported that school nurses identified several parent-related barriers, including parents not returning medication forms to school, difficulty in contacting parents, noncompliance with asthma plans, failure to pick up a child after an asthma episode and a lack of education and understanding about asthma. The nurses in these focus groups indicated that the most important link in providing adequate care at school was an involved and well-informed parent.
School-age urban minority youth have a disproportionately high prevalence of poorly controlled asthma, with a negative impact on academic achievement (Basch 2011). Factors related to poverty, increased prevalence of mental illness, single parent status and financial stress, may affect a parent's ability to effectively manage asthma (Smith et al. 2005). Laster et al. (2009) found that parent and child beliefs and perceptions regarding the use of daily controller medications were a significant barrier to asthma care and proper self-management at home and at school.
Barriers can also stem from a lack of resources at the school, such as time and asthma resources. The school nurses’ lack of time has been related to staffing issues, with the school nurse being responsible for hundreds of children (Bartholomew et al. 2006, Bruzzese et al. 2006, Calabrese et al. 1999, Hillemeier et al. 2006), that limits the direct care nurses can gave. School nurses often need to rely on unlicensed personnel, some of whom had limited understanding of asthma and asthma management (Calabrese et al. 1999, Hillemeier et al. 2006). Lack of asthma medications and supplies in school settings have also been reported (Hillemeier et al. Kielb et al. 2007, Major et al. 2006).
School nurses have indicated that providing optimal asthma care in the school is limited by difficult communication between those in the educational system, providers in the healthcare system, the family and the child. A commonly reported problem is lack of communication with the school by both parents and providers. In fact, nurses report that they are not always aware that a child in the school has asthma (Borgmeyer et al. 2005, Hillemeier et al. 2006, Major et al. 2006, Nabors et al. 2005). Reports of poor communication with schools regarding children with asthma are not restricted only to the United States. In Israel, Shohat and colleagues (2005) found that over 44% of the children with asthma reported that the school nurse did not know about their asthma and almost 14% reported that no one at school knew about their asthma. On the other hand, Calabrese et al. (1999) found that only 1/3 of the school nurses surveyed in their study reported sending a letter to parents if their child had an asthma episode at school and 12% of the school nurses reported never having spoken with school staff about asthma. More recently, Bruzzese (2010) found that communication between school nurses and teachers and parents regarding students with asthma was lacking.
The current evidence related to management of asthma in schools reflects potential barriers at multiple system levels, but this evidence is largely based on studies conducted in single geographic regions. The result is lack of clarity about the degree to which barriers are unique to certain macrosystem qualities, such as social policy and culture. To identify common and unique barriers to asthma care and provide guidance for universally relevant interventions, this paper presents the results of an international study of barriers to working with youth with asthma from the perspectives of school nurses.
THE STUDY
Aim
The aim of this qualitative international study was to identify and compare the types of barriers to asthma management from the perspectives of school nurses in Reykjavik, Iceland and St. Paul, MN, USA from an ecological perspective.
Design
The data for the barriers to asthma care study were drawn from a larger international research study, the International School Nurse Asthma Project (I-SNAP). I-SNAP focused on identifying and comparing school nurses’ roles and challenges in providing asthma care from the perspectives of school nurses who were coordinating and managing asthma care among pre-adolescents and adolescents in the capital city of Iceland and in the capital city of Minnesota (MN) in the United States. The design was an exploratory descriptive study of school nurses in St. Paul, MN, U.S. and Reykjavik, Iceland, using focus groups. The St. Paul School system was selected for the U.S. site because of its population size that is similar to that of the school system in Reykjavik, Iceland.
The investigators from the University of Iceland and University of Minnesota worked collaboratively in person and via videoconference calls and e-mails to design a common background survey and focus group interview protocol guide relevant to school nurses in both countries. Data were collected between September 2008-January 2009.
Sample
A convenience sample of school nurses (N=32) in Reykjavik (n=17) and in St Paul (n=15), who were coordinating and managing asthma care with younger (ages 10-14) and older (ages 15-18) adolescents, participated in this study. The unit of analysis was the focus group and not the individual participants.
Data collection
A series of three focus groups with school nurses (5-6 per group) were conducted in both Reykjavik and St. Paul using the same protocol. Core research teams at each site included two nursing faculty and one school nursing administrator. After informed consent was obtained, each school nurse participant completed a brief, self-report background questionnaire developed by the I-SNAP team. Demographic items were originally written in English and then translated into Icelandic. The School Nurse Background Information Survey (Svavarsdottir et al. 2008) includes 22 items in three parts. Items regarding the school nurses’ demographic information and characteristics of the school population served were selected for cross-country comparison (Table 1).
Table 1.
Demographic characteristics among school nurses in Reykjavik, Iceland and Saint Paul, Minnesota (N=32)
| Reykjavik (N=17) | St Paul (N=15) | |||
|---|---|---|---|---|
| N | % | N | % | |
| Gender | ||||
| Female | 17 | 100 | 14 | 93.4 |
| Male | 0 | 0 | 1 | 6.6 |
| Educational level | ||||
| Bachelors in nursing | 16 | 94.1 | 7 | 46.7 |
| Masters in nursing | 1 | 5.9 | 8 | 53.0 |
| Serve more than one school | 5 | 26.3 | 4 | 27.0 |
| Contact with parents of children with asthma | ||||
| 1-2 times per school year | 13 | 68.4 | 5 | 33.3 |
| > 3 times per school year | 1 | 5.25 | 10 | 66.7 |
| Contact with health care providers of children with asthma | ||||
| 1-2 times per school year | 6 | 31.6 | 7 | 46.6 |
| > 3 times per school year | 1 | 5.3 | 8 | 53.3 |
| Mean | Mean | |||
| School nurse age, in years | 38.2 | 53.7 | ||
| Years employed at school | 4.3 | 7.7 | ||
| Mean number of students served by school nurses | 1 nurse to 559 students | 1 nurse to 883 students | ||
Next, school nurses participated in a focus group discussion that included semi-structured interview questions. This paper focuses on responses to questions about challenges and barriers to asthma care in schools. A facilitator and co-facilitator moderated each focus group session. The focus group sessions were convened in a school or university meeting rooms and lasted between 60-90 minutes. The focus group interviews were audiotaped and transcribed verbatim. The Icelandic transcripts were then translated into English.
Ethical consideration
Ethics committee approval was received from universities in both cities and accepted by both school systems. No personal identifiable information was collected in the survey or the focus group interviews.
Data Analysis
Descriptive statistics were used to characterize the school nurse participants in Reykjavik, Iceland and in St. Paul, Minnesota. Descriptive content analytic techniques (Neuendorf, 2002) were used to systematically identify and compare types of barriers to asthma care identified by school nurses within and across focus groups by country. First, team members from both countries independently read and reread the transcripts in their entirety and discussed core findings. Then one member of the research team, who has extensive qualitative research expertise, systematically identified and categorized the types of barriers to asthma care in the St. Paul and next in the Reykjavik transcripts and developed the coding scheme. Next, a second coder in each country used the coding scheme to independently review and check the accuracy of the coding. Then the coders from both countries convened to verify the similarities and differences in the types of barriers by location.
In addition to informing the focus group questions, the ecological framework was used to group and compare types of barriers to asthma care by system level and by country. Barriers to asthma care identified by school nurses were categorized at these levels: (a) individual student, (b) family/parental, (c) school, (d) community and (e) health care system.
Rigor
A pilot focus group was conducted in St. Paul with the Icelandic team observing the process via videoconference to ensure that the same methodology would be used consistently across sites in subsequent focus groups. Participants also completed and commented on the demographic survey to ensure items elicited the types of responses intended.
Trustworthiness of the qualitative findings (Lincoln & Guba 1986) was established by (a) checking the accuracy of the transcriptions against the audio recordings, (b) verifying the accuracy of the translation of the Icelandic to English focus group transcripts, (c) having two research team members with qualitative expertise independently code the data and then a third member from each country validated the coding scheme and resolved a few coding discrepancies, (d) verifying the interpretation of the data with the focus group facilitators and school nurse administrators in both countries and (e) maintaining and periodically reviewing the audit trail of the raw data, the coding scheme and records of the steps in the analysis.
RESULTS
Characteristics of sample
All of the nurses in Reykjavik were females (n=17, 100%) and the majority in St. Paul were females (n=14, 93.4%). The school nurses mean age in Reykjavik was 38.2 years (range = 27-47) and 53.7 years in St. Paul (range from 32-66 years). About one-fourth of school nurses in both countries served more than one school. The mean number of students served by St. Paul school nurses was greater than those served by Reykjavik school nurses (Table 1). School population characteristics (size and number of schools) versus individual nurse characteristics (e.g., age, years of experience) were evident in the focus group discussions about barriers in both countries.
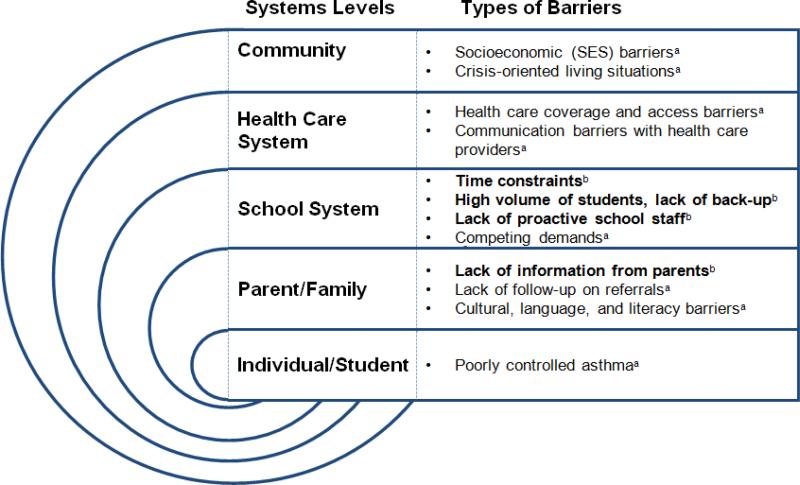
School nurses in Reykjavik (Reyk) and in St. Paul (St.P) identified a variety of types of barriers to managing asthma in school settings that were summarized and compared by country at the (a) individual student, (b) family/parental, (d) school system, (d) community or (e) health care system level (Figure 1). Examplars are identified by location and focus group (FG) number.
Figure 1.
A Comparison of Types of Barriers to Asthma Management in Schools by Systems Level and Location
aBarriers identified primarily by school nurses in St. Paul, MN
bBarriers identified by school nurses in St. Paul, MN and Reykjavik, Iceland
Individual Student Level Barriers
Students with poorly controlled asthma
Overall, school nurses in Reykjavik described asthma as well controlled in their student populations. In contrast, St. Paul nurses regularly encountered students whose poorly controlled asthma was considered the norm from the student and/or the family's perspective. Examples included:
Kids ...who are normally always with asthma in the yellow zone and that feels normal to them. And so they don't come and tell us that they're having trouble. (St. P, FG 4)
Parents or grandparents who have asthma and their way of thinking about it is completely different. Like they come to school and they need a ride in the elevator because their asthma's out of control and they view it as normal. That's really challenging. (St. P, FG 4)
Parental/Family Level Barriers
Lack of information about asthma from parents
School nurses in both locations noted that communication with parents could be challenging. For example, school nurses were concerned that they did not always get the information from families that they needed to prevent or manage asthma episodes:
There are sometimes when you are asking for information from parents or a doctor's note or something- it is like you are asking for a kidney or something. It is hard to get [information] from parents. (Reyk, FG 3)
I think parents ...would let [the nurse] know if the child had severe [asthma] but if the asthma was mild, I am not sure the parents are necessarily letting us know so that is of course a certain barrier. (Reyk, FG 3)
Lack of follow-up on school nurses’ referrals
School nurses in St. Paul described alerting parents when a child with asthma symptoms needed evaluation by a health care provider, but noted that it didn't always happen:
You call them and you say, ‘You know, your child needs to be re-assessed by the doctor.’ And frequently they just don't do anything, which makes it very difficult to do follow through. (St. P, FG 4)
Part of the worry I have too is sometimes the parent will say that they're going to bring them to the doctor. The kid comes back the next day, still in the red zone and you say, did you go to the doctor? ‘Nope.’ Did you take any medicine last night? ‘No.’ And they're exactly the same as they were before. (St. P, FG 5)
Cultural, language and literacy barriers
Only school nurses in St. Paul, MN described challenges related to educating and working with families from diverse cultural, educational, linguistic and socioeconomic backgrounds. Low English reading and health literacy levels were identified by school nurses who worked with families from low socioeconomic backgrounds and with immigrant families in St. Paul, MN and interpreters were not readily available:
Our populations are so diverse, we have all these barriers. We have cultural barriers, we have language barriers and a lot of times when people of a second language, they'll say, ‘Yes, I understand.’ And really, they're not getting it. (St. P, FG 5)
There are a fair amount of parents who don't read, or can't read very well. And all of that literature and information about the [asthma] drugs...I think it's just beyond a lot of their reading level. (St. P, FG 5)
School System Level Barriers
Time constraints
Limited time to focus on asthma prevention and management was a common issue for school nurses in both cities. School nurses had multiple role responsibilities, working not only with individual youth with chronic conditions such as asthma, but also addressing school system needs (e.g., for staff education and health promotion for the population of school children):
You have to give yourself time to get to know [the childen with asthma] and that is maybe just one of the barriers, you are a little short on time.... because the work always waits for you. (Reyk, FG 3)
Other barriers are time... In a perfect world, I'd check in on a periodic basis with a bunch of kids and I don't. (St. P, FG 4)
Competing demands
School nurses in St. Paul talked about frequent interruptions at work. Often minor ailments competed for nurses’ attention. Episodic needs demanded care in the moment and limited time for educating youth with asthma:
‘Cause a lot of it—I mean it's real involved teaching and a lot of it in senior high you start doing some of it and boom, you're interrupted. (St. P, FG 4)
Having a lot of minor little ailments that need attention...eats up a huge part of my day. (St. P, FG 4)
High volume of students and lack of professional nursing back-up
Both Reykjavik and St. Paul nurses spoke of feeling stretched to cover the needs of the student populations they served, particularly when they had more than one school to cover. Lack of professional nursing substitutes or coverage was a common barrier in both locations:
I could see it as a barrier if I would have to give medications. Some days I am not at school all day. Some days I am at meetings and sometimes I am sick and there is no one to substitute for me. (Reyk, FG 1)
I'm in three different schools. So it's like, you can call me here on Monday, you can call me here on Tuesday, you can call me here on Wednesday. (St. P, FG 6)
I'm the only one there...there's no one else that would be there to take my place. (St. P, FG 4)
Lack of proactivity among school staff regarding asthma management
Both St. Paul and Reykjavik school nurses found it difficult when school staff weren't proactive about students’ asthma management and didn't inform them about information that could affect children's asthma status in advance:
I find it a barrier, that they [the teaching staff] are not telling me if they are leaving the building and things like that and then she [the student] is just in the dairy factory [field trip] or something when I am supposed to help her with the inhaler. (Reyk, FG 2)
I think teachers... a lot of times they don't listen until...they really need the information. Then they wonder why you never told them anything. And that's kind of a problem for everybody, not just at my school. (St. P, FG 5)
Community Level Barriers
Socio-economic barriers
Only school nurses in St. Paul spontaneously identified socioeconomic barriers to asthma care. Hardships related to poverty and transportation barriers among students were commonly encountered. For example, one school nurse noted that poverty limited access to care:
In our student population as far as getting to the doctor... I think the most challenging group are the working poor... When they work they make just enough money to not qualify for health insurance or for anything through the state, but not enough to really be able to afford to pay out of pocket. (St. P, FG 5)
Another school nurse described a variety of common barriers, such as ‘transportation to the doctor, affording the inhalers, affording access to insurance or assistance.’ (St. P, FG 5)
Crisis-oriented living situations
Only school nurses in St. Paul described crisis-oriented family living situations as barriers to continuity of care. Some students were in family situations where health issues weren't dealt with until a crisis happened that demanded attention. Financial family emergencies also contributed to their lack of focus on preventive care:
Until they're really in crisis they don't really feel like they need it. And then when they're in crisis they need it now and they'll go sit at the hospital as many hours as it takes to get seen. And then it's not an emergency anymore...So when that crisis is gone, it might move on to their eviction, or having no gas in the car, or—you know, just that crisis-oriented living. (St. P, FG 4)
Health Care System Barriers
Health care coverage and access barriers
Lack of health care coverage was only identified as a barrier by school nurses in St. Paul. They described lack of health care coverage as a formidable challenge for many of their students, as evident in their lack of access to affordable asthma medication. Some families described sharing inhalers in response to tough economic times:
I have a family that has insurance, but then I finally found out that they were paying 100% for their prescriptions, so even though they were bringing them in to the appointments and they were getting prescriptions written, they weren't always picking them up. Or if they were picking them up, they were using them sparingly, because they were paying full [price]. (St. P, FG 5)
The other thing I see, now that the economy is [worse]—I've seen more sharing of inhalers [among family members]. (St. P, FG 5)
Communication barriers with other health care providers when managing asthma
St. Paul nurses identified barriers to communication with providers, an issue not mentioned by Reykjavik nurses. It was not always possible to contact the provider directly, making lines of communication unwieldy and time intensive. The large number of providers in different health care systems with whom nurses needed to communicate was also daunting:
This is a huge challenge just because of our community, the number of providers we have. It's not like we're in rural America where they might only have a choice of five providers to go to. But we have so many different providers. (St. P, FG 5)
Discussion
The present study contributes to a broader understanding of barriers to asthma management identified among school nurses in two Western nations. Knowing the challenges school nurses across nations are facing contributes to a more international understanding of asthma management. Furthermore, such knowledge can inform the development of cross-cultural interventions for adolescents with asthma in school settings. School nurses in Reykjavik as well as in St. Paul, MN identified similar types of barriers at the parent/family and school level, however, nurses in St. Paul described additional barriers (e.g., lack of follow up on school nurses’ referrals and cultural, language and literacy challenges) related to poorly controlled asthma.
Nurses in both countries reported parent and family level barriers, such as lack of communications between parents and the school nurses. School nurses felt that parents did not always give them the information they needed to prevent or manage asthma episodes. Similar findings were reported by Forbis and colleagues (2006) who found parents who were not involved in asthma care nor well informed about asthma to be a barrier to asthma management. Other challenges with families have also been identified in the international literature. School nurses in Northern America and in Europe have both reported poor communication between families and school nurses as a problem area (Borgmeyer et al. 2005, Bruzzese et al. 2010, Major et al. 2006, Shohat, et al. 2005), and nurses have reported that they are not even always aware that a child in the school has asthma (Shohat et al. 2005). Family-school partnerships have long been recognized as key to children's cognitive and emotional development (Christenson 2003), yet interventions that engage school nurses and families for improved health outcomes are rare. Developing effective communication strategies between school nurses and families is essential for school nurses to manage asthma effectively and be able to provide evidence based health care services.
There were several commonalities between countries in the types of school system barriers identified. Participants in both countries identified that lack of time, the high volume of students per school nurse (mean =549 in Reykjavik, mean =883 in St. Paul) and the lack of professional nursing back up were barriers to optimal asthma management. These findings are consistent with findings reported by Bartholomew and colleagues (2006) and by Jones et al. (2009) who indicated that lack of resources (e.g., equipment) and time constraints among school nurses were barriers to asthma care. In the case of school administrative processes, such as resource allocation, child health is affected by system-level decisions that limit the availability of school nurses. Gaining insight into both individual as well as system level barriers is crucial to ensuring quality asthma care in schools.
Similarly, school system staff barriers identified by both the nurses in Reykjavik and in St. Paul, such as the lack of proactivity among school staff regarding asthma management, are consistent with Hillemeier et al.'s (2006) findings. These authors identified difficulties in communications between those in the educational system, providers in the healthcare system and with the family and the child, to be the most cited barriers to coordinating and managing asthma care in schools. In the wider international context of increased movement towards community- and school-based health care, nursing leaders need to initiate policies that validate the roles and responsibilities in asthma management among school nurses, both at the individual, the family and the system level.
Individual Student, Community and Health Care System Level Barriers
It is noteworthy that challenges regarding individual student level barriers, community level barriers and health care system barriers were only emphasized by the school nurses in St. Paul. While the nurses in Reykjavik noted that asthma was generally well controlled in their student population, St. Paul school nurses identified more youth with poorly controlled asthma.
The asthma management challenges identified by school nurses in St. Paul can be explained by the diverse student population served. St. Paul school nurses encountered some students for whom poorly controlled asthma was considered to be the norm from the student and/or the family perspective. Also, the nurses in St. Paul schools worked with families from diverse cultural, educational, linguistic and socioeconomic backgrounds, which was not the case for the nurses in Reykjavik who served more homogeneous, middle-class families. Serving families from low socioeconomic backgrounds and immigrant families with low English reading and health literacy levels calls for more intensive school health care services to be offered by school nurses in St. Paul. These nurses needed to focus more on coordinating and managing asthma care with students with poorly controlled asthma. School nurses in Reykjavik, on the other hand, were able to focus more on asthma prevention and education because students’ asthma was largely well controlled.
Even though asthma treatment is very similar in Iceland and the United States, the health care system in Iceland is quite different from the health care system in the U.S. While Iceland has socialized medicine with health care services available and nearly free to all Icelanders, the U.S. has an insurance-based method of distributing care. The complex and fragmented structure of the USA health care system affects access to health care services for the families in St. Paul. Lack of health care coverage and difficulties communicating with health care providers had an impact on some families’ ability to follow up on school nurses’ referrals to health care professionals as well as on the families’ ability to afford and or use asthma medication as recommended by providers.
Despite the differences in health care systems between the two countries, school nurses in both Iceland and in Minnesota offer evidence based health care services to children and adolescents with asthma in their schools. To provide quality asthma care, the nurses need their health and school systems to offer appropriate back up at the schools and minimize unnecessary paperwork. Further, safety factors regarding the number of students served per nurse need to be considered in both countries, especially when the numbers of children with chronic illnesses such as asthma and or special needs are increasing in schools. Nurses in Reykjavik, Iceland as well as in St. Paul, Minnesota need to be able to work effectively across systems and to focus on the needs of their student population both at the individual as well as at the population level.
Study limitations
The findings from these companion international studies need to be interpreted in the context of the cities and countries where they were conducted. Also, the sample sizes were small. The findings themselves may not generalize to other countries, but the types of barriers identified from this study using the ecological perspective provide the basis for future studies of barriers to asthma care in other locations.
CONCLUSION
An ecological systems framework provides a way to understand the interconnectedness of individual students, families, health systems and school systems in asthma care. The findings of this cross-national study underscore the importance of communication among systems for successful asthma management in schools. The ecological approach, with its focus on interactions in and among systems, was particularly helpful in identifying similarities and differences in barriers to asthma care by country. The primary differences in barriers were related to cultural and linguistic diversity in St. Paul where there has been a large influx of immigrants in the past decade compared with Reykjavik, which has a more homogenous population. Despite differences in the health care systems in Iceland and the U.S., international interventions need to focus both on reducing barriers to asthma care in schools and supporting school nurses in their efforts to prevent and manage asthma in school settings.
What is already known about this topic
Worldwide, children and adolescents with asthma are the largest group of children with chronic illnesses attending schools.
Nurses play a key role in providing care to children with asthma in the school setting.
There are numerous barriers that have been identified, mainly in Northern America, at the individual, family and systems levels, which prevent the optimum care of children with asthma in school settings.
What this paper adds
Information on challenges faced by school nurses in Iceland and Minnesota regarding asthma care provides a global perspective on common barriers to asthma care coordination and asthma management in school settings.
School nurses in both countries identified time constraints, communication barriers, staff challenges and school system barriers as common challenges to asthma management in school systems.
School nurses in Saint Paul, Minnesota recognized more socioeconomic, cultural and linguistic related barriers to asthma care, emphasizing their need to focus more on asthma management than the school nurses in Iceland, who could focus more on asthma prevention and education.
Implications for practice and/or policy
Interventions promoting communication between school nurses and families may improve asthma management in schools.
Barriers at multiple systems levels need to be taken into consideration when evaluating the effectiveness of asthma care in school systems across nations.
Administrative and policy-level changes may help school systems function more efficiently in supporting school nurses’ roles and responsibilities regarding coordinating and managing asthma care. These include recognizing safety concerns when nurse to student ratios are high, easing nurses’ ability to work across systems, focusing both on individual and population levels of asthma management, providing appropriate back up at schools and minimizing paperwork.
Acknowledgements
The authors would like to thank all the Icelandic and the U.S. school nurses who participated in the study and the school nursing administrators, Ragnheiður Ó. Erlendsdóttir, RN, MS, MA and Denise Herrmann, RN, CNP, DNP who facilitated this study.
Funding:
This study was funded by a grant from the Icelandic Nurse Association Science Fund2 and from the University of Minnesota School of Nursing Foundation1 and the NIH Institutional CTSA (UW-Madison; 1KL2RR025012-01).3
Footnotes
Conflict of interest:
No conflict of interest has been declared by the authors.
Author Contributions:
- substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
- drafting the article or revising it critically for important intellectual content.
References
- Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980-2007. Pediatrics 123 Suppl. 2009;3(3):S131–145. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- Bartholomew LK, Sockrider M, Abramson SL, Swank PR, Czyzewski DI, Tortolero SR. Partners in school asthma management: Evaluation of a self-management program for children with asthma. Journal of School Health. 2006;76(6):283–290. doi: 10.1111/j.1746-1561.2006.00113.x. [DOI] [PubMed] [Google Scholar]
- Basch CE. Asthma and the achievement gap among urban minority youth. Journal of School Health. 2011;81(10):606–613. doi: 10.1111/j.1746-1561.2011.00634.x. [DOI] [PubMed] [Google Scholar]
- Borgmeyer A, Jamerson P, Gyr P, Westhus N, Glynn E. The school nurse role in asthma management: Can the action plan help? Journal of School Nursing. 2005;21(1):23–30. doi: 10.1622/1059-8405(2005)021[0023:tsnria]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development. Harvard University Press; Cambridge, MA: 1979. [Google Scholar]
- Bruzzese J, Evans D, Wiesemann S, Pinkett-Heller M, Levison MJ, Du Y. Using school staff to establish a preventive network of care to improve elementary school students' control of asthma. Journal of School Health. 2006;76(6):307–312. doi: 10.1111/j.1746-1561.2006.00118.x. [DOI] [PubMed] [Google Scholar]
- Bruzzese JM, Unikel LH, Evans D, Bornstein L, Surrence K, Mellins RB. Asthma knowledge and asthma management behavior in urban elementary school teachers. Journal of Asthma. 2010;47(2):185–191. doi: 10.3109/02770900903519908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkhart PV, Svavarsdottir EK, Rayens MK, Oakley MG, Orlygsdottir B. Adolescents with asthma: Predictors of quality of life. Journal of Advanced Nursing. 2009;65(4):860–866. doi: 10.1111/j.1365-2648.2008.04948.x. [DOI] [PubMed] [Google Scholar]
- Calabrese BJ, Nanda JP, Huss K, Winkelstein M, Quartey RI, Rand CS. Asthma knowledge, roles, functions and educational needs of school nurses. Journal of School Health. 1999;69(6):233–238. doi: 10.1111/j.1746-1561.1999.tb06395.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] [March 2010];Summary health statistics for U.S. children: National Health Interview Survey. 2009 2008 from http://www.cdc.gov/nchs/data/series/sr_10/sr10_244.pdf.
- Christenson SL. The family-school partnership: An opportunity to promote the learning competence of all students. School Psychology Quarterly. 2003;18:454–482. [Google Scholar]
- Clausen M, Kristjansson S, Haraldsson A, Bjorksten B. High prevalence of allergic diseases and sensitization in a low allergen country. Acta Paediatrica. 2008;97(9):1216–1220. doi: 10.1111/j.1651-2227.2008.00887.x. [DOI] [PubMed] [Google Scholar]
- Clausen M, Björkstén B, Haraldsson Á, Kristjánsson S. Prevalence of atopy and atopic diseases in Icelandic schoolchildren. Journal of Allergy and Clinical Immunology. 2002;109:S74–75. [Google Scholar]
- Forbis S, Rammel J, Huffman B, Taylor R. Barriers to care of inner-city children with asthma: School nurse perspective. Journal of School Health. 2006;76(6):205–207. doi: 10.1111/j.1746-1561.2006.00097.x. [DOI] [PubMed] [Google Scholar]
- Getch YQ, Neuharth-Pritchett S. Teacher characteristics and knowledge of asthma. Public Health Nursing. 2009;26(2):124–133. doi: 10.1111/j.1525-1446.2009.00763.x. [DOI] [PubMed] [Google Scholar]
- Global Initiative for Asthma (GINA) [July 2011];Global strategy for asthma management and prevention. 2010 from: http://www.ginasthma.org.
- Gudbjörnsdottir MI, Norbäck D, Björnsson E, Soon A, Jarvis D, Jõgi R, Gislason D, Gislason T, Janson C. Indoor environment in three North European cities in relationship to atopy and respiratory symptoms. The Clinical Respiratory Journal. 2009;3(2):85–94. doi: 10.1111/j.1752-699X.2008.00122.x. [DOI] [PubMed] [Google Scholar]
- Hillemeier MM, Gusic ME, Bai Y. Rural and urban children with asthma: Are school health services meeting their needs? Pediatrics. 2006;118(3):1097–1103. doi: 10.1542/peds.2005-2239. [DOI] [PubMed] [Google Scholar]
- Jones SE, Wheeler LS, Smith AM, McManus T. Adherence to National Asthma Education and Prevention Program's “How Asthma-Friendly Is Your School?”. Recommendations. Journal of School Nursing. 2009;25(5):382–394. doi: 10.1177/1059840509343292. [DOI] [PubMed] [Google Scholar]
- Kielb C, Lin S, Hwang SA. Asthma prevalence, management and education in New York State elementary schools: A survey of school nurses. Journal of School Nursing. 2007;23(5):267–275. doi: 10.1177/10598405070230050501. [DOI] [PubMed] [Google Scholar]
- Laster N, Holsey CN, Shendell DG, Mccarty FA, Celano M. Barriers to asthma management among urban families: Caregiver and child perspectives. Journal of Asthma. 2009;46(7):731–739. doi: 10.1080/02770900903082571. [DOI] [PubMed] [Google Scholar]
- Lincoln YS, Guba EG. But is it rigorous? Trustworthiness and authenticity in naturalistic inquiry. In: Williams DD, editor. Naturalistic evaluation. Jossey-Bass; San Francisco: 1986. pp. 144–151. [Google Scholar]
- Major DA, Clarke SM, Cardenas RA, Taylor-Fishwick JC, Kelly CS, Butterfoss FD. Providing asthma care in elementary schools: Understanding barriers to determine best practices. Family & Community Health. 2006;29(4):256–265. doi: 10.1097/00003727-200610000-00004. [DOI] [PubMed] [Google Scholar]
- Millard MW, Johnson PT, Hilton A, Hart M. Children with asthma miss more school: Fact or fiction? Chest. 2009;135(2):303–306. doi: 10.1378/chest.08-1642. [DOI] [PubMed] [Google Scholar]
- Mizan SS, Shendell DG, Rhoads GG. Absence, extended absence and repeat tardiness related to asthma status among elementary school children. Journal of Asthma. 2011;48:228–234. doi: 10.3109/02770903.2011.555038. [DOI] [PubMed] [Google Scholar]
- Moonie S, Sterling DA, Figgs LW, Castro M. The relationship between school absence, academic performance and asthma status. Journal of School Health. 2008;78(3):140–148. doi: 10.1111/j.1746-1561.2007.00276.x. [DOI] [PubMed] [Google Scholar]
- Nabors L, Troillett A, Nash T, Masiulis B. School nurse perceptions of barriers and supports for children with diabetes. Journal of School Health. 2005;75(4):119–124. [PubMed] [Google Scholar]
- Neuendorf KA. The Content Analytic Guidebook. Sage Publications; Newbury Park, CA, USA: 2002. [Google Scholar]
- Pruitt K, Nolen J, Garcia-Reyes K, Edelman N, Schachter N. Improving asthma outcomes: Evidence-based health policy priorities. Pediatric Asthma, Allergy & Immunology. 2009;22(4):189–196. [Google Scholar]
- Shohat T, Graif Y, Garty B, Livne I, Green MS. The child with asthma at school: Results from a national asthma survey among schoolchildren in Israel. Journal of Adolescent Health. 2005;37(4):275–280. doi: 10.1016/j.jadohealth.2004.12.013. [DOI] [PubMed] [Google Scholar]
- Smith LA, Hatcher-Ross JL, Wertheimer R, Kahn RS. Rethinking race/ethnicity, income and childhood asthma: Racial/ethnic disparities concentrated among the very poor. Public Health Reports. 2005;120:109–120. doi: 10.1177/003335490512000203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Splett PL, Erickson CD, Belseth SB, Jensen C. Evaluation and sustainability of the Healthy Learners Asthma Initiative. Journal of School Health. 2006;76(6):276–282. doi: 10.1111/j.1746-1561.2006.00112.x. [DOI] [PubMed] [Google Scholar]
- Svavarsdottir EK, Burkhart PV, Rayens MK, Orlygsdottir B, Oakley MG. Icelandic and United States families of adolescents with asthma: Predictors of health-related quality of life from the parents’ perspective. Journal of Clinical Nursing. 2011;20:1–2. 267–273. doi: 10.1111/j.1365-2702.2009.03110.x. [DOI] [PubMed] [Google Scholar]
- Svavarsdottir EK, Orlygsdottir B, Garwick A, Looman W. The School Nurse Background Information survey. University of Iceland, Faculty of Nursing. 2008:1–3. [Google Scholar]
- Taras H, Wright S, Brennan J, Campana J, Lofgren R. Impact of school nurse case management on students with asthma. Journal of School Health. 2004;74(6):213–219. doi: 10.1111/j.1746-1561.2004.tb07935.x. [DOI] [PubMed] [Google Scholar]
- Winkelstein ML, Quartey R, Pham L, Lewis-Boyer L, Lewis C, Hill K. Asthma education for rural school nurses: Resources, barriers and outcomes. Journal of School Nursing. 2006;22(3):170–177. doi: 10.1177/10598405060220030801. [DOI] [PubMed] [Google Scholar]