Abstract
Exposure and response prevention (EX/RP) is an efficacious treatment for obsessive-compulsive disorder (OCD). However, patients often do not adhere fully to EX/RP procedures. Motivational Interviewing (MI) has been shown to improve treatment adherence in other disorders. This pilot study used a randomized controlled design to examine whether MI can be successfully added to EX/RP and whether this intervention (EX/RP+MI) could improve patient adherence to between-session EX/RP procedures relative to EX/RP alone. Thirty adults with OCD were randomized to 18 sessions of EX/RP or EX/RP+MI. Therapists rated patient adherence at each exposure session. Independent evaluators assessed change in OCD and depressive symptoms, and patients completed self-report measures of readiness for change and quality of life. The two treatment conditions differed in degree of congruence with MI but not in conduct of EX/RP procedures. Both groups experienced clinically significant improvement in OCD symptoms, without significant group differences in patient adherence. There are several possible reasons why EX/RP+MI had no effect on patient adherence compared to standard EX/RP, each of which has important implications for the design of future MI studies in OCD. We recommend that MI be further evaluated in OCD by exploring alternative modes of delivery and by focusing on patients less ready for change than the current sample.
Keywords: obsessive-compulsive disorder, motivational interviewing, exposure and response prevention, adherence, OCD
Introduction
Cognitive-behavioral therapy consisting of exposure and response prevention (EX/RP) is a first-line treatment for obsessive-compulsive disorder (OCD), either as monotherapy or combined with pharmacotherapy (American Psychiatric Association, 2007). EX/RP requires patients to confront feared situations (exposures) and to stop ritualizing (response prevention; Kozak & Foa, 1997). When patients adhere to these procedures, EX/RP is highly efficacious (Foa et al., 2005), yet patients often fail to adhere by dropping out of treatment or by not fully implementing the procedures as recommended (Abramowitz, Franklin, Zoellner, & DiBernardo, 2002; Foa et al., 1983; Simpson, Huppert, Petkova, Foa, & Liebowitz, 2006). Reducing dropout and improving patient adherence to EX/RP procedures could potentially improve treatment outcomes substantially.
One conceptualization of why OCD patients enter but then drop out or adhere poorly to EX/RP procedures is that they are “ambivalent” or caught between mutually exclusive courses of action. Specifically, although patients may wish to improve their lives by reducing the time spent obsessing and ritualizing (leading them to seek EX/RP treatment), they may also be unwilling or unable to adhere to the EX/RP procedures designed to achieve that goal (e.g., because they find exposures too aversive or perceive some benefit to their rituals). Motivational interviewing (MI) is a client-centered, goal-oriented method designed to enhance motivation to change by helping patients explore and resolve such ambivalence (Miller, 2006; Miller & Rollnick, 2002). In MI, the therapist expresses empathy by evoking and reflecting patients’ perceptions of their situation and the advantages and disadvantages of change. Therapists enhance motivation by eliciting and strengthening patients’ articulation of their desire, ability, reasons, need, and ultimately commitment to change and treatment (“change talk”). To accomplish this, therapists develop discrepancy between patients’ current behavior and important values and goals and support self-efficacy by exploring and affirming efforts and abilities to overcome obstacles. Emphasizing collaboration, supporting patient autonomy, and avoiding confrontation and directives, therapists roll with resistance when it arises. The goal is to help patients talk themselves into change.
Used as a prelude or integrated with other treatments, MI has reduced dropout and enhanced treatment adherence in substance use, health behavior, and mental health contexts (Hettema, Steele, & Miller, 2005; Zweben & Zuckoff, 2002). For example, Westra and colleagues (2009) provided MI as a prelude to group CBT in patients with generalized anxiety disorder and found that these patients had better homework adherence and treatment outcome than those receiving CBT alone. Lewis-Fernandez and colleagues (in review) integrated MI into medication management for depressed Hispanics and found significantly improved retention and outcome compared to historical controls.
We wondered whether MI could improve EX/RP adherence. Thus, we created an EX/RP+MI intervention that included explicit MI strategies in the introductory sessions to enhance motivation for treatment and an MI module for use during exposure sessions if resistance to treatment emerged. Delivering this intervention to 6 patients in an open trial (Simpson, Zuckoff, Page, Franklin, & Foa, 2008), we found it yielded comparable outcomes to standard EX/RP. However, this study did not address whether EX/RP+MI differs in its dose of MI or improves patient adherence relative to EX/RP alone. These are key questions since there can be overlap between MI and CBT approaches (Wilson & Schlam, 2004). At the same time, adding MI to a structured, expert-driven treatment like EX/RP might dilute the integrity of MI.
Consistent with recommended stages of psychosocial treatment development (Carroll & Onken, 2005), we conducted a small randomized controlled trial to directly compare EX/RP and EX/RP+MI in adults with OCD. Our aims were to evaluate whether EX/RP+MI was more congruent with MI than standard EX/RP and to determine whether EX/RP+MI led to better patient adherence. To assess MI fidelity, we used the Motivational Interviewing Treatment Integrity scale, a measure widely used in MI clinical trials. To assess patient adherence to EX/RP procedures, we used the Patient EX/RP Adherence Scale (Simpson et al., 2010). We hypothesized: 1) EX/RP+MI would be more congruent with MI than standard EX/RP during treatment segments designed to emphasize MI elements; and 2) EX/RP+MI would lead to better patient adherence to between-session EX/RP procedures. We also explored the effects of the two treatments on OCD outcome, knowing a priori that the small sample had adequate power to detect only large effects.
Methods
Setting and Recruitment
This study was conducted at the Anxiety Disorders Clinic (ADC), an outpatient research clinic at the New York Psychiatric Institute (NYSPI) and Columbia University. Patients were recruited (May 2007-January 2009) by advertisements and referral. The study was approved by the NYSPI institutional review board. Participants provided written informed consent.
Participants
Participants were between the ages of 18 and 70, met DSM-IV criteria for OCD for at least one year and had at least moderate symptoms on the Yale-Brown Obsessive Compulsive Scale (Y-BOCS ≥16). Patients could participate either off or on a serotonin reuptake inhibitor (SRI), and concomitant medications like benzodiazepines and antipsychotics were allowed. However, if receiving medications, patients had to be on a stable SRI dose prior to entering for at least 12 weeks (and four weeks for concomitant medications), and the dose had to remain stable during the study. Patients were excluded for lifetime mania or psychosis, current suicidal ideation or an attempt in the past 6 months, a Hamilton Depression Rating Scale (HAM-D, 17 item) score >17, substance abuse or dependence in the past 2 months, an unstable medical condition, or an adequate prior trial of EX/RP (≥ 8 sessions within 2 months). Other comorbid conditions were permitted only if OCD was the most severe and impairing condition. Psychotherapy outside of this study was not permitted. Eligibility was determined by a clinical interview with a senior clinician (MD or PhD). Psychiatric diagnoses were confirmed by an independent rater using the Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon, & Williams, 1996).
Procedures
Participants were randomized in blocks of four to EX/RP or EX/RP+MI. Randomization included stratification by therapist and by presence of prominent hoarding symptoms to ensure equal distribution of the two treatment conditions across these variables.
EX/RP consisted of three introductory sessions followed by 15 twice-weekly exposure sessions; all sessions lasted 90 minutes. Treatment followed the procedures outlined by Kozak and Foa (1997). During the introductory sessions, therapists assessed patients’ OCD, presented the treatment rationale, and developed an exposure hierarchy. During exposure sessions, therapists first reviewed patients’ progress with between-session EX/RP procedures, then helped patients to confront their fears for prolonged periods of time without ritualizing (i.e., in vivo and imaginal exposures), and ended each session by assigning specific exposures for patients to practice (at least one hour per day) before the next session. Patients were instructed to stop rituals after the first exposure session and to record any rituals that occurred. At least two exposure sessions occurred in the home environment. Between exposure sessions, therapists spoke briefly with patients by phone (for <20 minutes) to review progress with between-session EX/RP practice.
EX/RP+MI followed the same format: three introductory sessions and 15 exposure sessions (including at least two in the home environment); daily homework assignments; and between-session phone calls. However, MI strategies were specifically and strategically added as described in detail elsewhere (Simpson, Zuckoff, Page, Franklin, & Foa, 2008). In brief, although the introductory sessions accomplished the same tasks as in standard EX/RP (assessment, psychoeducation, and treatment planning), therapists used an MI-congruent approach whenever possible and introduced specific MI strategies to assess and evoke commitment to change and to treatment. During exposure sessions, standard procedures were followed (review of between-session EX/RP practice, therapist-supervised exposures, assignment of between-session EX/RP practice). However, a short (15-30 minute) MI module was available for use if resistance occurred (e.g., repeated failure to do between-session EX/RP procedures, expressed reluctance to proceed with treatment). The objective of this module was to use MI strategies to assess and enhance commitment to the time-limited and intensive EX/RP used in this protocol and to reengage the patient before proceeding with in-session exposures. Therapists were trained to recognize signs of resistance using the Miller & Rollnick (2002) adaptation of a rubric developed by Chamberlain and colleagues for use in studies of resistance. Therapists were instructed to shift into the MI module if initial efforts to reengage the patient into adhering to the treatment procedures using standard EX/RP methods (e.g., psychoeducation, encouragement) were not effective.
Treatment was conducted by two doctoral level therapists (JP and MM). Each therapist treated an equal number of patients in each condition (8 per condition for JP, 7 per condition for MM). Both had expertise in EX/RP, serving as EX/RP therapists on other NIMH-funded clinical trials. To ensure that patients in both treatment conditions received the key components of EX/RP as intended, weekly group EX/RP phone supervision of all cases was conducted by Dr. Foa and her faculty who were blind to treatment condition.
Neither therapist was formally trained in MI prior to the study. Training included: reviewing the MI text (Miller & Rollnick, 2002), training tapes (Miller, Rollnick, & Moyers, 1998), and EX/RP+MI manual; participating in three daylong in-person small-group MI skills-building sessions run by Dr. Zuckoff, a member of the Motivational Network of Trainers (MINT); conducting four MI sessions with at least one OCD patient who had expressed resistance to treatment; and completing at least one EX/RP+MI test case to practice the integration of MI with EX/RP. In addition, one therapist (JP) treated six cases in our open trial of EX/RP+MI (Simpson, Zuckoff, Page, Franklin, & Foa, 2008) and worked with Drs. Simpson and Zuckoff to develop the written manual for the EX/RP+MI condition. Therapists received weekly group supervision of audiotaped EX/RP+MI sessions from Drs. Simpson and Zuckoff that focused on MI.
Assessments
Independent Evaluations
Independent evaluators (IEs) blind to treatment assignment evaluated patients at baseline, after sessions 3 and 11, and at post-treatment (after session 18/week 9) with measures widely used in clinical research and shown to be reliable and valid. These measures were:
Yale-Brown Obsessive Compulsive Scale
(Y-BOCS, Goodman, Price, Rasmussen, Mazure, Delgado et al., 1989; Y-BOCS, Goodman, Price, Rasmussen, Mazure, Fleischmann et al., 1989). The Y-BOCS measures severity of obsessions and compulsions using 10 items yielding a total score ranging from 0 to 40. The total score was also used to calculate rates of response (a Y-BOCS decrease of ≥ 25%) and of excellent treatment response (a Y-BOCS of 12 or less; Simpson, Huppert, Petkova, Foa, & Liebowitz, 2006).
Hamilton Depression Rating Scale
(HAM-D; Hamilton, 1960): The 17-item HAM-D assesses depressive severity and yields a total score ranging from 0 to 68.
Patient Self-Reports of Quality of Life and Readiness to Change
Quality of Life and Enjoyment Questionnaire
(Q-LES-Q; Endicott, Nee, Harrison, & Blumenthal, 1993): Before and after treatment, patients completed the short version of the QLES-Q (16 items). This scale assesses satisfaction with life in the past week across different domains (e.g., work, economic status, family and social relationships, and health) on a 5 point scale; higher scores indicate less impairment. The summary score is scored as a percent of the maximum and has been shown to be sensitive to change with treatment (Kocsis et al., 1997).
University of Rhode Island Change Assessment
(URICA; McConnaughy, DiClemente, Prochaska, & Velicer, 1989; URICA; McConnaughy, Prochaska, & Velicer, 1983): Patients completed the URICA before starting treatment. The URICA was developed to assess an individual's “stage of change” in the transtheoretical model (Prochaska, DiClemente, & Norcross, 1992). A composite “readiness” score (ranging from –2 to 14), reflecting a second order factor (DiClemente & Prochaska, 1998), was calculated by subtracting the Precontemplation subscale score from the sum of the Contemplation, Action, and Maintenance subscales (Carbonari, DiClemente, & Zweben, 1994); higher scores indicate greater readiness to change. This composite score predicted drinking outcomes in Project MATCH (Project MATCH Research Group, 1998).
Readiness Rulers (Biener & Abrams, 1991; Rollnick, Mason, & Butler, 1999)
Prior to treatment, patients completed readiness rulers to assess on a scale of 1 (Not Ready) to 10 (Already Trying) their readiness to: 1) stop rituals or compulsions; 2) stop avoiding situations that trigger obsessions or rituals; and 3) participate in EX/RP treatment. Readiness rulers similar to these correlate highly with readiness questionnaires and outperform them in predicting behavioral intentions in multiple domains (Amodei & Lamb, 2004; Heather, Smailes, & Cassidy, 2008; LaBrie, Quinlan, Schiffman, & Earleywine, 2005).
Patient Adherence to EX/RP
Patient adherence to between-session EX/RP procedures was assessed at each exposure session by the therapist using the Patient EX/RP Adherence Scale (PEAS, Simpson et al., 2010), a new instrument with excellent inter-rater reliability and good construct validity. The PEAS measures patient adherence to three key EX/RP procedures: 1) the quantity of attempted exposures (compared to the quantity assigned); 2) the quality of exposures attempted; and 3) the degree of ritual prevention. Each procedure is rated separately on a Likert scale (1 to 7) with higher scores indicating better adherence. For example, a score of 5 on all items (“good” adherence) is equivalent to attempting assigned exposures and resisting urges to ritualize about 75% of the time and to completing attempted exposures with minimal compulsions or safety aids. A score of 6 (“very good” adherence) is equivalent to attempting assigned exposures and resisting urges to ritualize >90% of the time and completing assigned exposures with no ritualizing or safety aids. The total PEAS score is calculated by summing the three items and dividing by three. For each patient, the mean PEAS score was based on sessions in which between-session practice was discussed (i.e., the second through to the last exposure session). In intent-to-treat analyses, sessions missed because the patient dropped out of treatment were assigned a total PEAS score of 1 (i.e., the worst adherence possible).
Treatment Integrity
Therapist Adherence to EX/RP
Patients in both treatment conditions were intended to receive the key components of EX/RP. Therapist EX/RP adherence was assessed by a trained rater who was blind to treatment condition and outcome and had no contact with study patients. The rater performed: 1) a chart review to confirm that a detailed treatment hierarchy was created for each patient and to determine how many therapist-guided exposure sessions each patient received; 2) a random assessment of 10% of all exposure sessions (N=37 total [19 EX/RP, 18 EX/RP+MI] with at least one session from each patient) to confirm that sessions were conducted as intended; and 3) a review of all introductory sessions (N=12) from four randomly selected patients (15% of all patients [2 EX/RP, 2 EX/RP+MI]) to confirm that the key procedures (assessment, presentation of rationale, development of exposure hierarchy) occurred as outlined in the manual.
Therapist Adherence to MI
The use of MI procedures in both treatment conditions was evaluated using the global scales of the Motivational Interviewing Treatment Integrity scale (MITI 3.0; Moyers, Martin, Manuel, Miller, & Ernst). The MITI includes five global ratings (each on a scale from 1 [low] to 5 [high]) along the following dimensions: Empathy, Collaboration, Autonomy, Evocation, and Direction. Global ratings of 3.5 indicate beginning MI proficiency; scores of 4.0 indicate competency. MITI ratings were performed by a trained MI therapist (Dr. Ivan Balan) who was blind to treatment condition and had no contact with study patients. He was trained by Dr. Theresa Moyers, a developer of the MITI. As the MITI requires a 20-minute segment to achieve reliable ratings, for each patient the rater coded the opening 20 minutes from five sessions (Session #1, Session #3 and three exposure sessions randomly chosen from the beginning, middle, and end of treatment). We chose the opening segment of sessions to assess MI fidelity based upon the likelihood from the therapy manual that this would be the period during which MI would be used most consistently by therapists throughout all five selected sessions. Study therapists were aware that fidelity assessments would be conducted but were blind to the schedule for those assessments.
Data Analysis
Baseline demographic and clinical variables were compared using independent t-tests for continuous variables and Pearson chi-square or Fisher's Exact Test for categorical variables. Independent t-tests compared PEAS ratings between the treatment groups. To compare MITI ratings, MITI ratings at each time block (introductory Session 1, introductory Session 3, Block 1, Block 2, Block 3) were modeled using linear mixed effects models (LMMs) with a random subject-specific intercept (Diggle, Liang, & Zeger, 1992) and Proc MIXED in SAS.® A separate regression was used for the introductory sessions 1 and 3 and the Exposure blocks 1, 2 and 3 due to their different nature. The time trend was modeled as linear. For each subscale, group MITI differences were judged by the significance of corresponding model parameters. To compare outcomes between treatment groups on continuous measures with four time points (Y-BOCS, HAM-D), the change scores from baseline at Session 3, Session 11, and Session 18 (end of treatment) were modeled as a function of time, treatment, and treatment-by-time interaction using LMMs. Since the Q-LES-Q was measured only before and after treatment, a 2 sample t-test on the change score was used. Response and excellent response rates at Session 18 (using the last available observation) were compared between treatment groups using Pearson chi-squared tests.
All tests were conducted at two-sided level of significance α=0.05 with one exception. To minimize the possibility of findings MITI differences between the two treatments by chance, an alpha level of 0.01 was used to judge the significance of the MITI ratings to adjust for the fact that each MITI subscale was tested at five time points (0.05/5=0.01).
Results
Patient Flow and Description of Sample
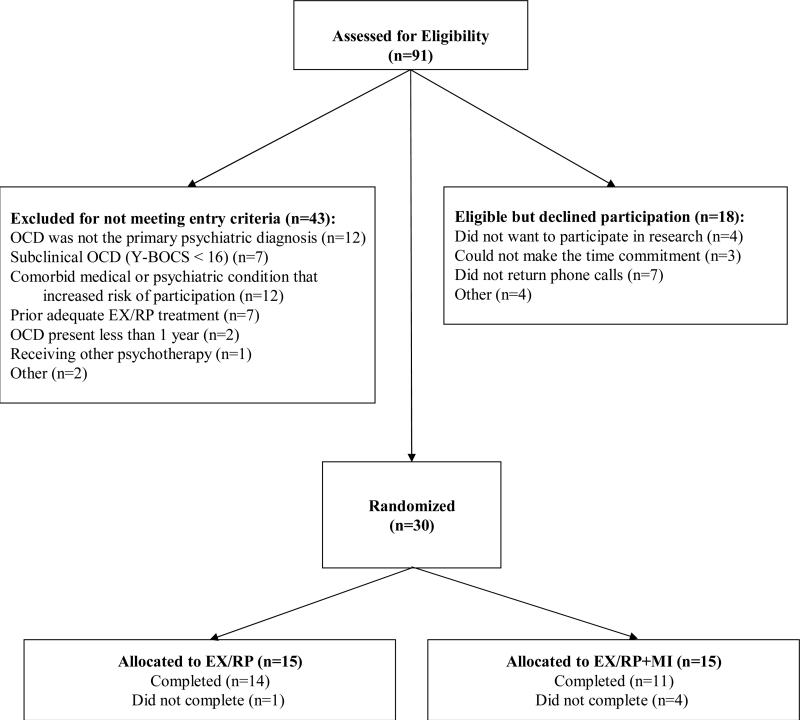
Figure 1 illustrates patient flow through the study. Thirty patients were randomized to EX/RP (N=15) or EX/RP+MI (N=15). Twenty-five patients completed treatment. More patients dropped from EX/RP+MI than from EX/RP, although the difference in attrition was not significant (EX/RP: 1/15 [at session 4]; EX/RP+MI: 4/15 [at sessions 5, 9, 11, & 15]; Fisher's exact test, p=0.33). Stated reasons for dropout included: exposures too distressing (N=1 EX/RP; N=2 EX/RP+MI); hospitalization due to worsening OCD (N=1 EX/RP+MI), and change in work schedule (N=1 EX/RP+MI).
Figure 1.
Flowchart of Study Participants
Demographic and pretreatment clinical characteristics are presented in Table 1. There were no significant differences on these variables (all p values >0.25, except years of education and baseline Y-BOCS [p values=0.06] and proportion single [Fisher's Exact Test, p=0.08]). Patients had a range of OCD symptoms, with a similar proportion of patients with primary hoarding symptoms in each treatment group. About a third of patients maintained a stable SRI dose (N=4 on fluoxetine, N=2 on sertraline, N=1 on paroxetine, N=1 on citalpram, N=2 on escitalopram, N=1 on fluvoxamine; mean weeks (SD) on current SRI: 89 (81), range 26 to 312). Four received a concomitant medication (benzodiazepines, n=2; bupropion, n=2), and one was only on a benzodiazepine; all had been on these medications for more than five months. Nearly half (47%) had at one time tried an SRI; of these patients, most had tried more than one (mean total SRI trials [standard deviation, SD]: EX/RP 3.0 [1.8]; EX/RP+MI 2.3 [1.4]). Few reported prior EX/RP treatment; those who did received four or fewer prior exposure sessions. Participants were moderately ready for change and for treatment as indicated by the URICA and Readiness Rulers (all p values for group comparisons > 0.39).
Table 1.
Demographic and Clinical Characteristicsa
| Characteristic | EX/RP (n=15) | EX/RP+MI (n=15) | All (n=30) |
|---|---|---|---|
| Age, y, mean (SD) | 39.1 (15.7) | 40.7 (11.1) | 39.9 (13.4) |
| Female, Number (%) | 7 (47) | 7 (47) | 14 (47) |
| Caucasian, Number (%) | 9 (60) | 10 (68) | 19 (63) |
| Marital Status, Number (%): | |||
| Single | 14 (93) | 9 (60) | 23 (77) |
| Married-Partnered | 0 (0) | 6 (40) | 6 (20) |
| Divorced- S eparated | 1 (7) | 0 (0) | 1 (3) |
| Education, y, mean (SD) | 15.3 (2.0) | 16.8 (2.1) | 16.1 (2.1) |
| Employment: working or in school at least part-time, Number (%) | 7 (47) | 11 (73) | 18 (60) |
| Y-BOCS at Week 0, mean (SD) | 29.6 (4.4) | 26.7 (3.6) | 28.1 (4.2) |
| HAM-D at Week 0, mean (SD) | 8.6 (6.8) | 7.9 (3.2) | 8.2 (5.2) |
| Age of OCD Onset, y, mean (SD) | 19.8 (11.5) | 21.2 (8.5) | 20.5 (10.0) |
| Duration of OCD, y, mean (SD) | 19.3 (13.8) | 17.7 (10.1) | 18.5 (11.9) |
| Hoarding subtype, Number (%) | 2 (13) | 2 (13) | 2 (13) |
| Comorbid Axis I diagnosis present, Number (%): | 7 (47) | 8 (53) | 15 (50) |
| Comorbid Axis I diagnoses, mean (SD) | 0.67 (0.82) | 0.80 (0.94) | 0.73 (0.87) |
| Currently taking SRI medication, Number (%) | 4 (27) | 7 (47) | 11 (37) |
| Currently taking non-SRI medication: | |||
| with an SRI, Number (%) | 3 (20) | 1 (7) | 4 (13) |
| without an SRI, Number (%) | 0 (0) | 1 (7) | 1 (3) |
| History of SRI medication, Number (%) | 7(47) | 7(47) | 14 (47) |
| History of Prior Exposure Sessions, Number (%) | 2(13) | 2(13) | 4 (13) |
| URICA Readiness Score, mean (SD) | 9.49 (1.72) | 9.79 (2.53) | 9.64 (2.13) |
| Readiness Ruler, mean (SD) | |||
| Ready to Stop Rituals/Compulsions | 7.4 (2.1) | 6.7 (2.2) | 7.1 (2.1) |
| Ready to Confront Feared Situations | 7.0 (2.0) | 6.7 (2.1) | 6.9 (2.0) |
| Ready to Participate in EX/RP | 7.7 (1.3) | 7.1 (2.3) | 7.4 (1.9) |
Abbreviations: EX/RP, Exposure and Ritual Prevention; MI, Motivational Interviewing; SRI, Serotonin Reuptake Inhibitor; OCD, Obsessive Compulsive Disorder; SD, standard deviation; URICA, University of Rhode Island Change Assessment; Y-BOCS, Yale-Brown Obsessive Compulsive Scale; y, year
There were no significant differences on these variables (all p values >0.25, except years of education and baseline Y-BOCS [p values=0.06] and proportion single [Fisher's Exact Test, p=0.08]).
Therapist Adherence
Adherence to EX/RP
Therapist adherence to EX/RP procedures was excellent in both treatment conditions as assessed by three indices. First, chart review confirmed that a detailed treatment hierarchy was created for each patient and that all patients who completed treatment participated in at least 12 sessions of therapist-guided exposures (out of a maximum possible of 15). There was no significant difference between treatments in mean number of therapist-guided exposure sessions (all randomized: EX/RP: 12.5 (3.2); EX/RP+MI: 10.8 (4.1); t=-1.23, df=28, p=0.23; all completers: EX/RP: 13.3 (0.7); EX/RP+MI: 12.8 (0.8); t=-1.57, df=23, p=0.13.) Second, 10% of all exposure sessions (19 EX/RP, 18 EX/RP+MI) were assessed by an independent rater: all contained therapist-supervised exposures, and homework was reviewed and assigned in all but one session. Finally, introductory sessions from two patients in each treatment condition (15% of patients) were listened to in their entirety: assessment, presentation of the treatment rationale, and creation of the exposure hierarchy occurred as outlined in the manual.
Adherence to MI
As shown in Table 2, the two groups differed in the degree to which therapist behaviors were congruent with MI principles, and these differences were consistent with the treatment protocols described above. For EX/RP, the mean MITI global ratings were less than 2.0 at all time points (Introductory Session 1 and 3, Exposure blocks 1, 2, & 3) on all subscales except Direction. Direction may be exerted in an MI-incongruent or MI-congruent manner. High Direction scores in the absence of high scores on the other subscales indicate the former. Overall, these data demonstrate that standard EX/RP as delivered in this study did not routinely contain MI elements, but in fact appeared to be counter to it (given that a rating of 3.0 is considered MI-neutral). As the same therapists delivered both treatment conditions, they also indicate that therapists trained in MI were able to deliver standard EX/RP without contamination.
Table 2.
MITI Ratings for EX/RP and EX/RP+MI Estimated Using Linear Mixed Effects Models
| Global MITI Ratings | Intro 1 | Intro 3 | Block 1 | Block 2 | Block 3 |
|---|---|---|---|---|---|
| Empathy, mean (SE) | |||||
| EX/RP | 1.60(0.19) | 1.33(0.19) | 1.29(0.21) | 1.29(0.19) | 1.30(0.21) |
| EX/RP+MI | 3.47(0.19) | 3.37(0.19) | 2.40(0.22) | 2.05(0.19) | 1.70(0.22) |
| P value | <.0001* | <.0001* | 0.0005* | 0.0071* | 0.195 |
| Evocation, mean (SE) | |||||
| EX/RP | 1.33(0.18) | 1.53(0.18) | 1.37(0.20) | 1.34(0.18) | 1.31(0.20) |
| EX/RP+MI | 3.53(0.18) | 3.38(0.18) | 2.43(0.21) | 2.22(0.18) | 2.02(0.21) |
| P value | <.0001* | <.0001* | 0.0005* | 0.0011* | 0.019 |
| Collaboration, mean (SE) | |||||
| EX/RP | 1.27(0.16) | 1.40(0.16) | 1.28(0.20) | 1.39(0.16) | 1.51(0.20) |
| EX/RP+MI | 3.27(0.16) | 3.02(0.16) | 2.49(0.21) | 2.17(0.17) | 1.86(0.21) |
| P value | <.0001* | <.0001* | <.0001* | 0.0015* | 0.245 |
| Autonomy, mean (SE) | |||||
| EX/RP | 1.93(0.17) | 1.40(0.17) | 1.20(0.20) | 1.42(0.16) | 1.64(0.20) |
| EX/RP+MI | 3.27(0.17) | 3.02(0.17) | 2.33(0.21) | 2.26(0.17) | 2.18(0.21) |
| P value | <.0001* | <.0001* | 0.0002* | 0.0008* | 0.071 |
| Direction, mean (SE) | |||||
| EX/RP | 4.93(0.11) | 4.93(0.11) | 4.91(0.12) | 4.84(0.08) | 4.76(0.13) |
| EX/RP+MI | 4.67(0.11) | 4.80(0.11) | 4.67(0.13) | 4.52(0.09) | 4.37(0.14) |
| P value | 0.091 | 0.379 | 0.180 | 0.011 | 0.038 |
Abbreviations: EX/RP, Exposure and Ritual Prevention; MI, Motivational Interviewing; MITI, Motivational Interviewing Treatment Integrity scale; SE, standard error
Significance was judged to be P <0.01 based on a Bonferroni correction for multiple comparisons to account for the fact that each scale was assessed at five time points (alpha=0.05/5=0.01)
In the EX/RP+MI condition, introductory sessions had the highest overall MITI global ratings (all means >3.0). These MITI ratings were significantly higher than those from standard EX/RP on all subscales but Direction. During exposure sessions, the two treatments differed significantly on all global MITI ratings but Direction during the first and second block of exposure sessions, but not the third block. However, the mean global MITI ratings were below 3.0 in both treatment conditions, indicating that these sessions were not generally MI-congruent even in the EX/RP+MI condition.
Patient Adherence to EX/RP procedures
On average, patients demonstrated good adherence to assigned EX/RP procedures (i.e., attempting and completing about 75% of assigned exposures with good effort and successfully resisting about 75% of urges to ritualize). There was no significant difference in the observed total PEAS scores (SD) between the two treatment groups (EX/RP: 5.08 (0.88), 95% CI [4.58, 5.59], range 3.57 to 6.12; EX/RP+MI: 5.26 (1.01), 95% CI [4.68, 5.85], range 3.22 to 6.40; t=0.51, df=26, p=0.61). There also were no significant differences on individual PEAS items (Quantity of exposure: EX/RP: 5.37 (0.93); EX/RP+MI: 5.46 (1.14); t=0.23, df=26, p=0.81; Quality exposure: EX/RP: 5.04 (0.97); EX/RP+MI: 5.09 (1.09); t=0.13, df=26, p=0.90; Degree of Ritual Prevention: EX/RP: 4.83 (1.21); EX/RP+MI: 5.24 (1.15); t=0.91, df=26, p=0.36). If sessions were assigned the lowest possible PEAS rating after a patient dropped out, then the mean PEAS scores for EX/RP+MI patients were lower than for EX/RP patients because attrition was higher in EX/RP+MI. However, the difference did not approach significance (EX/RP: 4.81 (1.35), 95% CI [4.06, 5.56], range 1.00 to 6.12; EX/RP+MI: 4.69 (1.81), 95% CI [3.69, 5.69], range 1.00 to 6.40; t=0.20, df=28, p=0.84).
Symptom Outcome
Symptom severity scores at each assessment point are shown in Table 3. Both treatment groups showed clinically meaningful decreases in OCD severity as measured by the Y-BOCS with no significant difference in the change in severity between the two treatment groups (MEM results: mean difference in change of slope 0.09 [Standard Error (SE)=0.18], p=0.51). There also was no significant difference in rates of response (EX/RP: 10/15 [67%]; EX/RP+MI: 9/15 [60%]; Pearson chi-square=0.144, df=1, p=0.70) or of excellent response (EX/RP: 6/15 [40%]; EX/RP+MI: 6/15 [40%]; Pearson chi-square=0, df=1, p=1.00). Both treatment groups also showed a small decrease in depressive severity and an increase in quality of life, with no significant group differences (HAM-D: mean difference in change of slope 0.01 [SE= 0.11], p=0.86); Q-LES-Q: mean difference in change score, 6.13 [SE =6.85], p=0.38).
Table 3.
Symptom Severity Scores Estimated Using Linear Mixed Effects Modelsa
| EX/RP N=15 | EX/RP+MI N=15 | |
|---|---|---|
| Y-BOCS mean (SD) | ||
| Week 0 mean score | 29.60(4.39) | 26.67(3.64) |
| Session 3 mean score | 27.43(3.50) | 24.42(2.64) |
| Session 11 mean score | 20.08(3.60) | 17.38(2.34) |
| Session 18 mean score | 13.75(3.60) | 11.90(2.35) |
| HAM-D mean (SD) | ||
| Session 0 mean score | 8.60(6.79) | 7.87(3.16) |
| Session 3 mean score | 8.19(4.07) | 7.18(2.45) |
| Session 11 mean score | 6.49(4.12) | 4.79(2.10) |
| Session 18 mean score | 4.80(4.12) | 3.17(2.19) |
| Q-LES-Q mean (SD) | ||
| Session 0 mean score | 47.67(12.76) | 53.60(20.53) |
| Session 18 mean score | 60.79(19.14) | 68.50(13.72) |
Abbreviations: EX/RP, Exposure and Response Prevention; HAM-D, Hamilton Depression Scale; MI, Motivational Interviewing; N, number; Q-LES-Q, Quality of Life and Enjoyment Satisfaction Questionnaire; SD, standard deviation, Y-BOCS, Yale-Brown Obsessive Compulsive Scale
Observed mean scores are shown at Week 0.
Discussion
This small randomized controlled trial examined whether adding MI elements to EX/RP (EX/RP+MI) would improve patient adherence compared to EX/RP alone. Patient adherence to between-session EX/RP procedures was good on average in both treatment groups. Moreover, both treatments produced clinically significant changes in OCD symptoms that were comparable to prior EX/RP studies (i.e., mean Y-BOCS decreases of more than 10 points and rates of response ≥ 60% and of excellent response ≥ 40% in the intent-to-treat sample). Although the treatments did not differ in their conduct of EX/RP procedures, they did differ in their degree of MI congruence. Despite this difference, EX/RP+MI did not yield better patient adherence than did EX/RP alone.
Several explanations can be offered as to why EX/RP+MI had no affect on patient adherence. One explanation is that MI cannot resolve ambivalence about change in patients with OCD or, perhaps, that poor EX/RP adherence is unrelated to ambivalence about change. On the other hand, two pilot studies suggest the opposite: a readiness intervention that included MI elements yielded superior treatment acceptance in adults who had previously refused EX/RP (Maltby & Tolin, 2005) and three sessions of MI provided by a separate therapist at key moments during an intensive family-based CBT protocol appeared to accelerate treatment progress in pediatric patients with OCD (Merlo et al., 2009). Moreover, in a small pilot study, we found MI procedures helpful at engaging some OCD patients in evidence-based treatment (Simpson & Zuckoff, in press). Given the variable findings and study designs, we believe that it is as yet premature to conclude that MI cannot improve treatment adherence in OCD.
A second possibility is that MI can enhance EX/RP adherence but not in the sample of patients that we studied. Other studies found MI most effective with angry patients (Waldron, Miller, & Tonigan, 2001) or those lower in motivation to change (Rohsenow et al., 2004). Yet our patients sought EX/RP, and their average URICA and readiness ruler ratings indicated that patients in both treatment conditions were ready for treatment. The fact that patient EX/RP adherence was good on the average in both treatment groups supports this explanation, i.e., that the absence of differences reflects a ceiling effect. Future studies need to determine whether MI would be more effective in patients less ready for EX/RP (e.g., EX/RP refusers or patients with poor prior EX/RP participation).
A third possible explanation is that MI can enhance EX/RP adherence in OCD, but that the protocol we used did not provide a sufficient MI dose to yield significant effects. On the one hand, there were significant differences in MITI ratings between EX/RP and EX/RP+MI during the introductory sessions and the first and second block of exposure sessions. On the other hand, even in the introductory sessions, when the maximum amount of MI elements were designed to be present, the MI dose was minimal, with mean MITI global ratings in the EX/RP+MI group at the level of beginning MI proficiency (viz. 3.5). These MITI ratings might reflect the fact that the MITI was designed to assess pure MI sessions, not MI elements added to a structured treatment like EX/RP; alternatively, these ratings might reflect the fact that the therapists were new to MI (although expert in EX/RP) and delivering expert level MI within a highly structured treatment like EX/RP takes even more MI training than provided herein (Miller & Moyers, 2006).
Our findings raise several issues for the design of future MI studies in OCD. One is which patients such studies should target. Theoretically, patients who should benefit most would be those “ambivalent” about the change that treatment promotes, as MI's presumed mechanism is to resolve ambivalence about opposing courses of action. Identifying such patients requires a reliable measure of this construct. It is unclear whether the URICA, designed to measure stage of readiness for change (McConnaughy, DiClemente, Prochaska, & Velicer, 1989; McConnaughy, Prochaska, & Velicer, 1983) not readiness for treatment, or our readiness rulers can serve this purpose. It is also possible that other factors (e.g., psychological reactance; Karno & Longabaugh, 2007; Madsen, McQuaid, & Craighead, 2009) might affect whether the MI approach (with its emphasis on evocation and support for autonomy) is preferable to the standard EX/RP approach (with its focus on expert instruction).
Another issue is how best to quantify the dose of MI delivered. In an integrated protocol, this involves both the quality and the quantity of MI provided. To assess quality, we focused on segments designed to be relatively high in MI elements in our protocol (introductory sessions and openings of exposure sessions) and used the MITI, a widely used measure in the MI field. No prior MI study in OCD independently measured the quality of the MI provided. Thus, we can only compare our MITI ratings to pure MI protocols, perhaps an excessively high standard. With regards to quantity, our protocol added more MI to the introductory sessions and provided an optional MI module for use during exposure sessions if therapists noticed signs of resistance. Our rationale was that too much time spent on MI during exposure sessions could dilute EX/RP's effects. A post-hoc review revealed that the MI module was variably used: not at all in some patients, occasionally in others, and at nearly every session in a few. Although consistent with the protocol, the result was that the amount of MI received in exposure sessions varied between subjects and complicated the interpretation of MITI ratings: low MITI ratings could mean low quality MI or that no MI was needed because no resistance was noted. An alternative approach would be to develop and train therapists on a specific set of verbal and non-verbal cues that should trigger the shift into the MI module and then measure MI fidelity after this shift ought to have occurred. The feasibility of creating a reliable algorithm of this kind, given the subtlety of some signs of resistance, remains to be explored.
A related issue is how best to deliver MI: as a prelude, interdigitated with another treatment, or added to another treatment as we did here? Our approach required therapists to shift back and forth between MI and EX/RP if resistance was encountered during exposure sessions. In some cases, the signs of resistance were clear (e.g., patients expressed the desire to dropout of treatment), and shifting into MI seemed natural. However, in most cases, signs of resistance were more subtle (e.g., partial but not total adherence with between-session practice) and varied from session to session. In such patients, therapists had to judge at each session whether the degree of resistance warranted the MI module. Unless resistance was obvious, their tendency was not to shift and to rely upon familiar CBT strategies. This perhaps was to be expected given that the therapists had expertise in CBT and were relatively new to MI; moreover, the protocol explicitly stated that the MI module was only to be used during exposure sessions if standard CBT procedures were ineffective. Perhaps a more integrated protocol, where MI elements are used even when subtle signs of resistance are noted, would have increased the dose of MI and led to different results. However, if expertise in both treatments is necessary to conduct such an integrated protocol, the applicability of this model to routine treatment settings may be limited.
A structural solution is to deliver MI separately. For example, in a trial of 76 GAD patients, Westra and colleagues (2009) found that MI sessions as a prelude to group CBT enhanced outcome and that this effect was mediated by patient homework adherence. Moreover, a meta-analysis found that the longest lasting effects of MI occurred when used as a prelude (Hettema, Steele, & Miller, 2005). MI as a prelude might increase the likelihood of delivering an adequate “dose” of good-quality MI. At the same time, resistance to treatment can occur at any point in EX/RP treatment and is common as one reaches the top of the exposure hierarchy. An alternative mode of delivery is to interdigitate MI sessions in-between key exposure sessions as was recently done in a pilot study (Merlo et al., 2009). This might ensure that all patients receive a minimal amount of MI during exposure sessions and would avoid the necessity of therapists switching back and forth within a session. However, the feasibility of this model in the real world of clinical care is uncertain.
Several limitations of our study design should be noted. First, the small sample meant there was adequate power to detect only large effects, although there were no trends for any group differences in patient adherence ratings or outcome. Second, the study focused on patient adherence to between-session EX/RP procedures, limiting our conclusions to this specific aspect of adherence, although it is notable that EX/RP+MI had a higher rate of dropout than EX/RP alone. Third, therapists rated patient adherence based on patient self-report. Independent ratings by those with no knowledge of the patients’ outcomes would be preferable. As a partial check on the validity of the adherence ratings, two independent raters assessed a subset of sessions (30/420 [7%]) as part of another study, and their agreement with the therapist was excellent (Simpson et al., 2010). Finally, many participants were relatively treatment naïve (only half had ever had an SRI trial), and few had prior EX/RP experience. As already noted, this may not have been the ideal sample in which to test the effects of MI.
In sum, in this sample of EX/RP-naïve patients, MI procedures added to standard EX/RP (as described above) had no effect on patient adherence to between-session EX/RP procedures. Future studies should further evaluate the effectiveness of MI at improving treatment adherence in OCD by focusing on patients who are less ready to start treatment and by studying alternative modes of delivery.
Acknowledgments
We thank members of the Anxiety Disorders Clinic for helpful comments on an earlier version of this manuscript and for help with the conduct of this trial (with particular thanks to the research assistants [Jessica McCarthy and Rena Staub], independent evaluators [Donna Vermes, Anthony Pinto], and raters of treatment integrity [Ivan Balan, Kim Glazier].We also thank Shawn Cahill for helping with EX/RP supervision, Naihua Duan for consulting on statistical analysis, and Yuanyuan Bao for help with statistical programming. This study was funded by a treatment development grant from the National Institutes of Mental Health (R34 MH071570) and by a 2005 NARSAD Young Investigator to Dr. Simpson. We thank Stephen and Constance Lieber for supporting the first author as a NARSAD Lieber Investigator. Finally, we are grateful to the patients who participated.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abramowitz JS, Franklin ME, Zoellner LA, DiBernardo CL. Treatment compliance and outcome in obsessive-compulsive disorder. Behavior Modification. 2002;26(4):447–463. doi: 10.1177/0145445502026004001. [DOI] [PubMed] [Google Scholar]
- Amodei N, Lamb RJ. Convergent and concurrent validity of the Contemplation Ladder and URICA scales. Drug Alcohol Depend. 2004;73(3):301–306. doi: 10.1016/j.drugalcdep.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Association AP. American Psychiatric Association: Practice guideline for the treatment of patients with obsessive-compulsive disorder. American Journal of Psychiatry. 2007;164(suppl):1–56. [PubMed] [Google Scholar]
- Biener L, Abrams DB. The Contemplation Ladder: validation of a measure of readiness to consider smoking cessation. Health Psychol. 1991;10(5):360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- Carbonari J, DiClemente CC, Zweben A. A readiness to change scale: Its development, validation,and usefulness. Paper presented at the Conference Name|. 1994 Retrieved Access Date|. from URL|. [Google Scholar]
- Carroll KM, Onken LS. Behavioral therapies for drug abuse. Am J Psychiatry. 2005;162(8):1452–1460. doi: 10.1176/appi.ajp.162.8.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiClemente CC, Prochaska JO. Toward a comprehensive, transtheoretical model of change: Stages of change and addictive behaviors. In: Miller WR, Heather N, editors. Treating Addictive Behaviors. Plenum Press; New York: 1998. pp. 3–24. [Google Scholar]
- Diggle P, Liang KY, Zeger S. Analysis of Longitudinal Data. Oxford University Press; Oxford: 1992. [Google Scholar]
- Endicott J, Nee J, Harrison W, Blumenthal R. Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacology Bulletin. 1993;29(2):321–326. [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Biometrics Research Department, New York State Psychiatric Institute; New York, NY: 1996. Structured Clinical Interveiw for DSM-IV Axis I Disorders-Patient Edition. [Google Scholar]
- Foa EB, Grayson JB, Steketee GS, Doppelt HG, Turner RM, Latimer PR. Success and failure in the behavioral treatment of obsessive-compulsives. J Consult Clin Psychol. 1983;51(2):287–297. doi: 10.1037//0022-006x.51.2.287. [DOI] [PubMed] [Google Scholar]
- Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, et al. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. Am J Psychiatry. 2005;162(1):151–161. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, et al. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch Gen Psychiatry. 1989;46(11):1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46(11):1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A Rating Scale for Depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heather N, Smailes D, Cassidy P. Development of a Readiness Ruler for use with alcohol brief interventions. Drug Alcohol Depend. 2008;98(3):235–240. doi: 10.1016/j.drugalcdep.2008.06.005. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Karno MP, Longabaugh R. Does matching matter? Examining matches and mismatches between patient attributes and therapy techniques in alcoholism treatment. Addiction. 2007;102(4):587–596. doi: 10.1111/j.1360-0443.2007.01754.x. [DOI] [PubMed] [Google Scholar]
- Kocsis JH, Zisook S, Davidson J, Shelton R, Yonkers K, Hellerstein DJ, et al. Double-blind comparison of sertraline, imipramine, and placebo in the treatment of dysthymia: psychosocial outcomes. Am J Psychiatry. 1997;154(3):390–395. doi: 10.1176/ajp.154.3.390. [DOI] [PubMed] [Google Scholar]
- Kozak MJ, Foa EB. Mastery of obsessive-compulsive disorder: A cognitive-behavioral approach. The Psychological Corporation; San Antonio, Texas: 1997. [Google Scholar]
- LaBrie JW, Quinlan T, Schiffman JE, Earleywine ME. Performance of alcohol and safer sex change rulers compared with readiness to change questionnaires. Psychol Addict Behav. 2005;19(1):112–115. doi: 10.1037/0893-164X.19.1.112. [DOI] [PubMed] [Google Scholar]
- Madsen JW, McQuaid JR, Craighead WE. Working with reactant patients: are we prescribing nonadherence? Depress Anxiety. 2009;26(2):129–134. doi: 10.1002/da.20523. [DOI] [PubMed] [Google Scholar]
- Maltby N, Tolin DF. A brief motivational intervention for treatment-refusing OCD patients. Cogn Behav Ther. 2005;34(3):176–184. doi: 10.1080/16506070510043741. [DOI] [PubMed] [Google Scholar]
- McConnaughy EA, DiClemente CC, Prochaska JO, Velicer WF. Stages of change in psychotherapy: A follow-up report. Psychotherapy: Theory, Research, Practice, Training. 1989;26:494–503. [Google Scholar]
- McConnaughy EA, Prochaska JO, Velicer WF. Stages of change in psychotherapy: Measurement and sample. Psychotherapy. 1983;20:368–375. [Google Scholar]
- Merlo LJ, Storch EA, Lehmkuhl HD, Jacob ML, Murphy TK, Goodman WK, et al. Cognitive Behavioral Therapy Plus Motivational Interviewing Improves Outcome for Pediatric Obsessive-Compulsive Disorder: A Preliminary Study. Cogn Behav Ther. 2009;1 doi: 10.1080/16506070902831773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR. Motivational factors in addictive behaviors. In: Miller WR, Carroll KM, editors. Rethinking substance abuse: What the science shows, and what we should do about it. Guilford; New York: 2006. pp. 143–150. [Google Scholar]
- Miller WR, Moyers TB. Eight stages in learning motivational interviewing. Journal of Teaching in the Addictions. 2006;5:3–17. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing. second edition The Guilford Press; New York: 2002. [Google Scholar]
- Miller WR, Rollnick S, Moyers TB. Motivational Interviewing: Professional Training Series. CASAA, University of New Mexico; Albuquerque: 1998. [Google Scholar]
- Moyers T, Martin T, Manuel JK, Miller WR, Ernst D. http://casaa.unm.edu/download/miti3.pdf.
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Martin RA, Colby SM, Myers MG, Gulliver SB, et al. Motivational enhancement and coping skills training for cocaine abusers: effects on substance use outcomes. Addiction. 2004;99(7):862–874. doi: 10.1111/j.1360-0443.2004.00743.x. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Mason P, Butler C. Health Behavior Change: A guide for practitioners. Churchill Livingstone; Edinburgh: 1999. [Google Scholar]
- Simpson HB, Huppert JD, Petkova E, Foa EB, Liebowitz MR. Response versus remission in obsessive-compulsive disorder. J Clin Psychiatry. 2006;67(2):269–276. doi: 10.4088/jcp.v67n0214. [DOI] [PubMed] [Google Scholar]
- Simpson HB, Maher M, Page JR, Gibbons CJ, Franklin ME, Foa EB. Development of a patient adherence scale for exposure and response prevention therapy. Behav Ther. 2010;41(1):30–37. doi: 10.1016/j.beth.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson HB, Zuckoff A, Page JR, Franklin ME, Foa EB. Adding motivational interviewing to exposure and ritual prevention for obsessive-compulsive disorder: an open pilot trial. Cogn Behav Ther. 2008;37(1):38–49. doi: 10.1080/16506070701743252. [DOI] [PubMed] [Google Scholar]
- Simpson HB, Zuckoff AM. Using Motivational Interviewing to Enhance Treatment Outcome in People with OCD. Cognitive and Behavioural Practice. doi: 10.1016/j.cbpra.2009.06.009. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldron H, Miller W, Tonigan J. Client anger as a predictor of differential response to treatment. In: Longabaugh R, Wirtz P, editors. Project MATCH hypotheses: Results and causal chain analyses. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. pp. 134–148. [Google Scholar]
- Westra HA, Arkowitz H, Dozois DJ. Adding a motivational interviewing pretreatment to cognitive behavioral therapy for generalized anxiety disorder: a preliminary randomized controlled trial. J Anxiety Disord. 2009;23(8):1106–1117. doi: 10.1016/j.janxdis.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson GT, Schlam TR. The transtheoretical model and motivational interviewing in the treatment of eating and weight disorders. Clinical Psychology Review. 2004;24:361–378. doi: 10.1016/j.cpr.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Zweben A, Zuckoff A. Motivational interviewing and treatment adherence. In: Miller WR, Rollnick S, editors. Motivational interviewing: Preparing people for change. Guilford Press; New York: 2002. [Google Scholar]