Abstract
Objective
To evaluate the effect of the Chiranjeevi Yojana programme, a public–private partnership to improve maternal and neonatal health in Gujarat, India.
Methods
A household survey (n = 5597 households) was conducted in Gujarat to collect retrospective data on births within the preceding 5 years. In an observational study using a difference-in-differences design, the relationship between the Chiranjeevi Yojana programme and the probability of delivery in health-care institutions, the probability of obstetric complications and mean household expenditure for deliveries was subsequently examined. In multivariate regressions, individual and household characteristics as well as district and year fixed effects were controlled for. Data from the most recent District Level Household and Facility Survey (DLHS-3) wave conducted in Gujarat (n = 6484 households) were used in parallel analyses.
Findings
Between 2005 and 2010, the Chiranjeevi Yojana programme was not associated with a statistically significant change in the probability of institutional delivery (2.42 percentage points; 95% confidence interval, CI: −5.90 to 10.74) or of birth-related complications (6.16 percentage points; 95% CI: −2.63 to 14.95). Estimates using DLHS-3 data were similar. Analyses of household expenditures indicated that mean household expenditure for private-sector deliveries had either not fallen or had fallen very little under the Chiranjeevi Yojana programme.
Conclusion
The Chiranjeevi Yojana programme appears to have had no significant impact on institutional delivery rates or maternal health outcomes. The absence of estimated reductions in household spending for private-sector deliveries deserves further study.
Résumé
Objectif
Évaluer le programme Chiranjeevi Yojana, un partenariat public-privé établi pour améliorer la santé maternelle et néonatale au Gujarat, en Inde.
Méthodes
Une enquête sur les ménages (n = 5597 ménages) a été menée à Gujarat pour collecter les données rétrospectives sur les naissances ayant eu lieu au cours des 5 années précédentes. La relation entre le programme Chiranjeevi Yojana et la probabilité d'accouchement dans des établissements de soins de santé, la probabilité de complications obstétriques et les dépenses moyennes des ménages pour les accouchements a ensuite été examinée par une étude d'observation utilisant une approche de l'écart dans les différences. Les caractéristiques des individus et des ménages ainsi que les effets fixes des districts et de l'année ont été contrôlés en utilisant des régressions multivariées. Les données issues des dernières vagues d'enquêtes sur les installations et le niveau des ménages des districts (DLHS-3) menées au Gujarat (n = 6484 ménages) ont été utilisées dans des analyses parallèles.
Résultats
Entre 2005 et 2010, le programme Chiranjeevi Yojana n'était pas associé à un changement statistiquement significatif pour la probabilité d'accouchement en institutions (2,42 points de pourcentage; intervalle de confiance à 95%, IC: −5,90–10,74) ou pour les complications liées à l'accouchement (6,16 points de pourcentage; IC à 95%: −2,63–14,95). Les estimations utilisant les données DLHS-3 étaient semblables à ces résultats. Les analyses des dépenses des ménages ont indiqué que les dépenses moyennes des ménages pour les accouchements dans le secteur privé n'ont pas baissé ou très peu pendant le programme Chiranjeevi Yojana.
Conclusion
Le programme Chiranjeevi Yojana semble n'avoir eu aucun impact significatif sur le taux d'accouchement en institution ou dans les résultats de santé maternelle. L'absence de diminution estimée dans les dépenses des ménages pour les accouchements dans le secteur privé mérite une étude plus approfondie.
Resumen
Objetivo
Evaluar el efecto del programa Chiranjeevi Yojana, una asociación público-privada destinada a mejorar la salud materna y neonatal en Gujarat, India.
Métodos
Se llevó a cabo una encuesta doméstica (n = 5597 hogares) en Gujarat para recabar datos retrospectivos sobre los nacimientos en los últimos 5 años. En un estudio observacional, se examinó la relación entre el programa Chiranjeevi Yojana y la probabilidad de parto en instituciones de atención sanitaria, la probabilidad de complicaciones obstétricas y la media de gasto doméstico en partos, empleando un diseño de diferencia en las diferencias. En las regresiones multivariantes, se controlaron las características individuales y domésticas, así como los efectos fijos anuales y del distrito. Se emplearon los datos de la última ronda de encuestas domésticas y de las instalaciones a nivel de distrito (DLHS-3) realizadas en Gujarat (n = 6484 hogares) en análisis paralelos.
Resultados
Entre 2005 y 2010, el programa Chiranjeevi Yojana no se asoció con un cambio importante desde el punto de vista estadístico en la probabilidad de partos en instituciones (2,42 puntos porcentuales; intervalo de confianza del 95 %, IC −5,90 a 10,74) o de complicaciones relacionadas con el parto (6,16 puntos porcentuales; IC del 95 %: − 2,63 a 14,95). Las estimaciones que emplearon los datos DLHS-3 fueron similares. Los análisis de los gastos domésticos revelaron que el gasto doméstico en partos en el sector privado no había disminuido en absoluto o muy poco bajo elprograma Chiranjeevi Yojana.
Conclusión
El programa Chiranjeevi Yojana noparece haber tenido un impacto significativo en las tasas de parto en instituciones ni en los resultados de salud materna. La ausencia de las reducciones previstas en el gasto doméstico por partos en el sector privado merece un estudio más profundo.
ملخص
الغرض
تقييم تأثير برنامج شيرانجيفي يوجانا، إحدى الشراكات بين القطاع العام والخاص لتحسين صحة الأمهات والولدان في منطقة غوجارات بالهند.
الطريقة
تم إجراء مسح أسري (العدد = 5597 أسرة) في منطقة غوجارات بغية جمع البيانات الاسترجاعية بشأن حالات الولادة خلال الخمسة أعوام السابقة. وفي دراسة قائمة على الملاحظة باستخدام تصميم الفرق في الاختلافات، تم في مرحلة لاحقة دراسة العلاقة بين برنامج شيرانجيفي يوجانا واحتمالية الولادة في مؤسسات الرعاية الصحية واحتمالية حدوث مضاعفات الولادة ومتوسط إنفاق الأسر على الولادات. وفي الارتدادات متعددة المتغيرات، تم ضبط الخصائص الفردية والأسرية بالإضافة إلى التأثيرات الثابتة للمنطقة والسنة. وتم استخدام البيانات المستمدة من أحدث موجة مسح للأسر والمرافق على صعيد المنطقة (DLHS-3) أجريت في منطقة غوجارات (العدد = 6484 أسرة) في تحليلات موازية.
النتائج
في الفترة من 2005 إلى 2010، لم يرتبط برنامج شيرانجيفي يوجانا بتغير كبير من الناحية الإحصائية في احتمالية الولادة التي تتم في المؤسسات (2.42 في المائة نقطة؛ فاصل الثقة 95 %، فاصل الثقة: من -5.90 إلى 10.74) أو التعقيدات المرتبطة بالولادة (6.16 في المائة نقطة؛ فاصل الثقة 95%، فاصل الثقة: من -2.63 إلى 14.95). وكانت التقديرات باستخدام بيانات DLHS-3 متشابهة. وأشارت تحليلات نفقات الأسر إما إلى عدم انخفاض متوسط إنفاق الأسر على الولادات في القطاع الخاص أو انخفاضه على نحو طفيف جداً في ظل برنامج شيرانجيفي يوجانا.
الاستنتاج
يبدو أن برنامج شيرانجيفي يوجانا لم يكن له تأثير كبير على معدلات الولادة في المؤسسات أو حصائل صحة الأمهات. ويستوجب غياب الانخفاضات المقدرة في إنفاق الأسر على الولادات في القطاع الخاص مزيداً من الدراسة.
摘要
目的
评估赤拉尼维由旬计划的效果,这是一个改善印度古吉拉特邦母亲和新生儿健康的公私合作项目。
方法
对古吉拉特邦之前5年内回顾性出生数据进行家庭调查(n = 5597个家庭)。随后在使用双重差分设计的观察性研究中,调查赤拉尼维由旬计划和医疗机构分娩可能性、产科并发症可能性以及分娩的平均家庭费用之间的关系。在多元回归中,将个人和家庭特征以及地区和年固定影响作为控制变量。在平行分析中使用最近在古吉拉特邦(n = 6484个家庭)执行的地区级家庭和设施调查(DLHS-3)中的数据。
结果
在2005和2010年之间,赤拉尼维由旬计划与机构分娩的可能性(2.42百分点;95%置信区间,CI:-5.90至10.74)或出生相关并发症(6.16百分点;95% CI:-2.63至14.95)统计数据的显著变化没有相关性。使用DLHS-3数据的估算结果相似。家庭支出分析表明,私营机构分娩的平均家庭开支在赤拉尼维由旬计划中没有降低或降低非常少。
结论
赤拉尼维由旬计划似乎对机构分娩率或母亲健康结局没有显著影响。私人机构分娩的家庭估计开支没有减少,这一点需要进一步的研究。
Резюме
Цель
Оценить влияние программы Чирандживи Йоджана — государственно-частного партнерства, целью которого является улучшение медицинского обслуживания матерей и новорожденных в штате Гуджарат в Индии.
Методы
В штате Гуджарат было проведено обследование домохозяйств (n = 5597 домохозяйств) для сбора ретроспективных данных о рождаемости за последние 5 лет. В обсервационном исследовании с использованием модели «разница-в-различиях» были последовательно исследованы взаимосвязи между программой Чирандживи Йоджана и вероятностью родов в учреждениях здравоохранения, вероятностью осложнений во время родов и средним уровнем расходов домохозяйств на роды. В рамках многопараметрических регрессий была выполнена проверка характеристик отдельных лиц и домохозяйств, а также зафиксированных результатов по районам и годичным периодам. В ходе параллельного анализа также использовались данные самой последней кампании обследования домохозяйств и учреждений на уровне районов (DLHS-3), которая проводилась в Гуджарате (n = 6484 домохозяйств).
Результаты
В период 2005-2010 годов осуществление программы Чирандживи Йоджана не привело к статистически значимому изменению вероятности родов в учреждениях здравоохранения (2,42 процентных пункта; 95%-ный доверительный интервал, ДИ: –5, 90–10,74) или количества осложнений из-за родов (6,16 процентных пункта; 95%-ный ДИ: –2,63-14,95). Оценки с использованием данных DLHS-3 оказались схожими. Анализ расходов домохозяйств показал, что в результате осуществления программы Чирандживи Йоджана средние расходы домохозяйств на роды в частных учреждениях либо не снизились вовсе, либо снизились незначительно.
Вывод
Похоже, что программа Чирандживи Йоджана не оказала существенного влияния на количество родов, принимаемых в учреждениях здравоохранения, или на их последствия для материнского здоровья. Отсутствие предполагаемого сокращения расходов домохозяйств на роды в частных учреждениях здравоохранения требует дальнейшего изучения.
Introduction
Each year, over 500 000 women in the world die from birth-related complications1 and more than 5 million neonates die before they reach 12 months of age.2 All but 2% of the neonatal deaths occur in developing countries.2 In the last decade, global efforts to reduce maternal and neonatal mortality have grown rapidly. Between 2003 and 2008, global spending on maternal, neonatal and child health more than doubled – although it remained relatively constant as a share of official development assistance.3,4 This allowed various new initiatives, including those focusing on skilled birth attendance and emergency obstetric care, to be supported.3,4
As no single intervention can address the range of causes of maternal death, facility-based intrapartum care – “institutional delivery” – is generally recommended as the best option for improving maternal health.5 Facilities that provide maternity care are likely to have the trained staff, infrastructure and standardized delivery protocols needed to manage most neonatal and obstetric complications.
In general, public hospitals in India lack the capacity and reach to serve many rural areas, which means that many poor women have no access to key health-care services.6,7 Recognizing this limitation, in January 2006 the state government of Gujarat launched the Chiranjeevi Yojana programme, a public–private partnership designed to increase institutional delivery rates.8 It was subsequently estimated that this programme had led to a 90% reduction in maternal deaths and a 60% reduction in neonatal deaths among beneficiaries in Gujarat.8–12 The programme received the Asian Innovations Award in 2006,13 had covered almost 800 000 deliveries by March 2012, and is generally perceived as a successful model that should be followed in other Indian states.14
However, perceptions of the programme’s success are based on the results of studies – simple cross-sectional investigations or before-and-after comparisons – that had severe limitations. These studies did not address the role of the self-selection of institutional delivery by pregnant women and took no account of the “background” increases in institutional deliveries that probably occurred over each study period.10
The Chiranjeevi Yojana programme covers the costs of deliveries – at designated private-sector hospitals – for women from “below-poverty-line” (BPL) households. BPL status – which is either determined by multidimensional means testing or designated by the relevant village authority – confers a variety of other benefits, including public subsidies for food grains, sugar, oil and fuel. The programme pays the designated private-sector hospitals 1600 Indian rupees – approximately 37 United States dollars (US$) – per delivery. In exchange, the programme expects the hospitals both to offer vaginal deliveries or caesarean sections to poor women free of charge and to reimburse at least some of the women’s travel costs. The hospitals can offer additional hospital services to beneficiaries for a separate fee. By 2010, the programme covered more than 800 private-sector hospitals and had helped finance more than 400 000 deliveries.15
The aim of the present study was to estimate the relationship between the Chiranjeevi Yojana programme and the probability of institutional delivery, the use of maternal and neonatal services provided by trained health workers, birth-related maternal complications and household spending for delivery. We used population-based samples and adjusted for time-invariant differences across the districts of Gujarat, changes in outcomes over time that were common across the state, and a range of household-level characteristics. By matching information about programme placement and timing to population-level data – rather than data from participating hospitals – we were also able to minimize the influence of self-selection into institutional delivery among pregnant women.
Methods
The Chiranjeevi Yojana programme was launched in five northern districts of Gujarat in January 2006 and then expanded to the rest of the state between December 2006 and January 2007. We use a multivariate difference-in-differences regression framework to identify changes in primary outcomes associated with the spread of the programme across the state. The 21 “late-implementing” districts served as a control for the five “early-implementing” districts of Banaskantha, Dahod, Kachchh, Panch Mahal and Sabarkantha in 2006 and vice versa in 2007.
Data sources and outcome measures
We relied on two sources of data for our study: our own household survey in 2010 and analogous data from the third wave of the District Level Household and Facility Survey (DLHS-3).
In our survey – conducted in August to September 2010 – we collected retrospective information from a state-wide sample of women who had had deliveries since January 2005. We used stratified three-stage cluster sampling (Appendix A, available at: http://www.cohesiveindia.org/IMATCHINE/CY-BWHO2013Appendix.pdf). Within each study village we conducted a brief census of all households. We then randomly selected 10 households that had reported at least one delivery since January 2005. We selected households with BPL index scores between 16 and 25 in the year 2002 based on original plans to use a “fuzzy” regression discontinuity design.16,17 Unfortunately, widespread inconsistencies in classification of the BPL status of households prevented such analyses. Of the 6002 sampled households, 5663 (94.4%) agreed to provide data and 5597 (93.3%) provided full data and were included in the final analysis.
Through household surveys modelled after the well-known Demographic and Health Surveys, we recorded maternal and household demographic and socioeconomic characteristics as well as detailed retrospective information about antenatal and postnatal care and deliveries for all births since 2005. Our primary outcomes were: the place of delivery – public facility, private facility or home; who assisted with the delivery – a trained health professional or a relative; the type of delivery – vaginal or caesarean; whether the mother had received antenatal care, postnatal care or both and, if so, whether such care had been provided by a trained health professional; whether the mother suffered birth-related maternal complications such as premature labour, excessive bleeding or loss of consciousness; whether the neonate had been admitted to a neonatal intensive-care unit; and how much the household had spent on the delivery – both the hospital fees and total costs including transportation and other expenses.
We conducted parallel analyses using publicly available data from the third wave of the District Level Household and Facility Survey (DLHS-3). Such surveys have been routinely commissioned – by the Indian Ministry of Health and Family Welfare – to monitor reproductive and child health throughout India. In Gujarat, DLHS-3 was conducted in 2007 and 2008 across each of the state’s 26 districts. We restricted our DLHS-3 sample to women whose last delivery – at the time of the survey – had been in or after 2005, yielding a final sample of 6484 households. Because the sample was designed to be representative at the district level, no attempt was made to identify households that had below-poverty-line status. However, the demographic characteristics of the DLHS-3 sample were reasonably comparable to those of our own survey (Table 1), and both measured similar delivery-related outcomes.
Table 1. Summary statistics from two household surveys, Gujarat, India.
| Characteristic | Present studya | DLHS-3b |
|---|---|---|
| Mother’s age at marriage, years (SD) | 18.39 (2.12) | 18.08 (2.95) |
| Mother’s age at delivery, years (SD) | 24.52 (4.24) | 25.06 (4.73) |
| Hindu households, % (SD) | 94 (23) | 91 (29) |
| Mothers who had attended school, % (SD) | 57 (ND) | 58 (49) |
| Wealth index, SDc | ND | 0.15 (0.94) |
| Mother’s education, % | ||
| Illiterate | 43 | ND |
| Primary | 27 | ND |
| Middle or higher | 30 | ND |
| Monthly household income in Indian rupees,d % of households | ||
| < 250 | 1 | ND |
| 250–499 | 3 | ND |
| 500–1499 | 27 | ND |
| 1500–2500 | 42 | ND |
| > 2500 | 27 | ND |
| Caste,e % | ||
| General or other | 18 | 19 |
| “Scheduled” caste | 22 | 13 |
| “Scheduled” tribe | 21 | 30 |
| Other “backward” caste | 39 | 0 |
| No designated caste or tribe | 0 | 38 |
DLHS-3, District Level Household and Facility Survey for 2007–2008; ND, not determined; SD, standard deviation.
a 5597 households.
b 6484 households.
c Calculated using the method of Filmer and Pritchett.18
d Approximately 43 Indian rupees to one United States dollar.
e Different caste designations were used in the two surveys.
Data analysis
A multivariate difference-in-differences ordinary least-squares regression analysis was used to determine if changes in our primary outcomes were associated with the staggered introduction of the Chiranjeevi Yojana programme across Gujarat’s districts. We use the timing of births – as reported by mothers in the two surveys – together with mother’s district of residence to determine if the Chiranjeevi Yojana programme had been implemented when a delivery occurred.
Specifically, using birth-level observations, we regress our primary outcomes on an indicator variable denoting whether or not the Chiranjeevi Yojana programme was active. In all regressions we control for district and year fixed effects to account for unobserved interdistrict differences that did not vary over time and changes over time that were common to all districts;19 as well as maternal characteristics (mother’s age at marriage, age at delivery and level of education); and household characteristics (caste, religion, and wealth – BPL score, monthly household income in our data and a composite wealth index in the DLHS-3 data). We calculated robust standard errors that are clustered by block (the primary sampling unit) to relax the assumption of independent and identically distributed errors within districts.
Given our available data using a baseline of 0.56 (proportion of institutional deliveries), the minimum detectable effect size for test of proportions is 5 percentage points or more in the probability of institutional delivery (a change from 0.56 to 0.61). The summary statistics for all outcomes are shown in Table 2.
Results
Programme impact
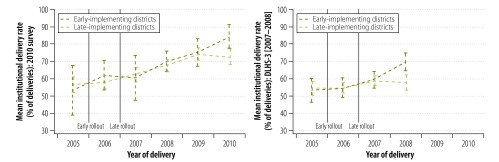
Fig. 1 shows the unadjusted mean institutional delivery rates (and confidence intervals, CIs) in the early- and late-implementation districts – separately using data from our 2010 survey and DLHS-3 from 2007–2008. Both panels show background increases in institutional delivery rates over time across Gujarat that are unrelated to the Chiranjeevi Yojana programme. Both panels also show modest changes in institutional delivery rates over time, but there are otherwise no relative changes in either early- or late-implementation districts that coincide with the introduction of the Chiranjeevi Yojana programme. The divergence between early- and late-implementation districts in 2008 shown using DLHS-3 data (left-hand panel of Fig. 1) is not present in 2008 (right-hand panel of Fig. 1) and disappears when the DLHS-3 data are weighted to compensate for between-survey differences in key BPL scoring components, such as household assets, sanitation and literacy. (The results with reweighted DLHS-3 data are available from the corresponding author on request).
Fig. 1.
Meana institutional delivery rates in Gujarat, India, 2005–2010
a Unadjusted mean.
Note: the data were collected specifically for the present study (left-hand panel) or in the District Level Household and Facility Survey for 2007–2008 (right-hand panel). They are plotted separately for the “early-implementing” districts – i.e. Banaskantha, Dahod, Kachchh, Panch Mahal and Sabarkantha, which implemented the Chiranjeevi Yojana programme in January 2006 – and the “late-implementing” districts – i.e. the other 21 districts of Gujarat, which implemented the same programme in December 2006 or January 2007. Error bars indicate 95% confidence intervals, adjusted for survey design.
The relationship between the Chiranjeevi Yojana programme and each of the primary outcomes we investigated is reported in Table 2. In Appendix A we also report odds ratios obtained using logistic regressions rather than linear probability models and note that the two approaches yield comparable inferences throughout. The data collected through our study indicated that implementation of the programme was not associated with a statistically significant change in the probability of institutional delivery (2.42 percentage points; 95% CI: −5.90 to 10.74). The CIs also imply that any association with institutional delivery too small to be detected in our samples could be no larger than an increase of 10.7 percentage points. The analysis using data from the DLHS-3 also confirms our findings that the programme’s implementation was not associated with a statistically significant change in institutional deliveries (−3.08 percentage points; 95% CI: –9.12 to 2.96). The DLHS-3 estimates are also more precise, which suggests that any programme impact too small to detect in our analysis could have been no larger than an increase of 2.9 percentage points. We find similar null estimates both for probability of delivery in private maternity hospitals and for birth attendance by physicians or nurses.
Table 2. Primary outcomes of the Chiranjeevi Yojana programme recorded for 2005, before the programme was launched, and for 2008, after the programme’s state-wide implementation, Gujarat, India.
| Outcome | Unadjusted mean value (SD) |
Difference-in-differences estimatea (95% CI) |
||||||
|---|---|---|---|---|---|---|---|---|
| Present studya |
DLHS-3b |
Present studya | DLHS-3b | |||||
| 2005 | 2008 | 2005 | 2008 | |||||
| Percentage of deliveries in year | ||||||||
| In health facility | 56.0 (49.7) | 68.0 (46.7) | 52.8 (49.9) | 60.3 (49.0) | 2.42 (−5.90 to 10.74) | –3.08 (−9.12 to 2.96) | ||
| In private health facilityc | 58.1 (49.4) | 58.2 (49.4) | 63.4 (48.2) | 60.4 (48.9) | –2.47 (−8.30 to 3.36) | –4.39 (−12.17 to 3.39) | ||
| Assisted by physician or nurse | 61.6 (48.7) | 72.1 (44.9) | 59.4 (49.1) | 65.5 (47.6) | 3.13 (−5.31 to 11.58) | –2.51 (−8.27 to 3.25) | ||
| Vaginal | 94.2 (23.4) | 92.7 (25.9) | 90.7 (29.0) | 91.6 (27.8) | 1.61 (−1.35 to 4.58) | 0.12 (−3.37 to 3.60) | ||
| With complications | 57.1 (49.6) | 53.8 (49.9) | 46.5 (49.9) | 44.0 (49.7) | 6.16 (−2.63 to 14.95) | 2.45 (−3.34 to 8.24) | ||
| With mother becoming unconscious | 8.8 (28.4) | 9.0 (28.7) | ND | ND | –1.82 (−6.83 to 3.19) | ND | ||
| With neonate admitted to NICU | 5.4 (22.6) | 5.1 (21.9) | ND | ND | 2.12 (−3.32 to 7.55) | ND | ||
| With excessive maternal bleeding | ND | ND | 6.8 (25.1) | 6.2 (24.1) | ND | 1.99 (−1.28 to 5.26) | ||
| With maternal convulsions | ND | ND | 3.8 (19.0) | 3.3 (17.8) | ND | –2.17 (−4.49 to 0.14) | ||
| With AN check-up | 85.2 (35.6) | 89.5 (30.6) | 68.3 (46.6) | 75.0 (43.3) | 3.18 (−1.69 to 8.06) | –2.09 (−8.07 to 3.90) | ||
| With AN check-up by physician or nursed | 87.4 (33.2) | 87.2 (33.4) | 97.7 (15.1) | 97.9 (14.5) | –3.76 (−11.75 to 4.24) | 0.12 (−2.89 to 3.13) | ||
| With AN testing | ND | ND | 95.6 (20.5) | 97.2 (16.4) | ND | 0.80 (−3.61 to 5.20) | ||
| With PN check-up | 74.4 (43.7) | 82.3 (38.2) | 60.4 (48.9) | 62.9 (48.3) | 4.99 (−2.15 to 12.13) | 2.23 (−3.50 to 7.96) | ||
| With PN check-up by physician or nursee | 84.3 (36.4) | 85.3 (35.4) | ND | ND | 0.77 (−9.79 to 11.33) | ND | ||
| With any household costs | 85.8 (34.9) | 86.9 (33.7) | 81.3 (39.0) | 80.5 (39.6) | 2.69 (−1.10 to 6.48) | –3.06 (−8.81 to 2.70) | ||
| Household costs associated with delivery, US$f | ||||||||
| Total | 55.57 (86.44) | 55.82 (82.82) | 47.15 (94.72) | 44.97 (86.52) | 0.42 (−0.23 to 1.08) | −0.49 (−0.87 to −0.11) | ||
| Health facility | 49.18 (84.24) | 49.38 (79.54) | ND | ND | 0.33 (−0.40 to 1.02) | ND | ||
| Non-facility | 6.37 (9.00) | 6.44 (11.13) | ND | ND | 0.03 (−0.47 to 0.52) | ND | ||
| Transportation | ND | ND | 5.81 (10.04) | 7.00 (10.97) | ND | 0.22 (−0.40 to 0.80) | ||
AN, antenatal; CI, confidence interval; DLHS-3, District Level Household and Facility Survey for 2007–2008; ND, not determined; NICU, neonatal intensive-care unit; PN, postnatal; SD, standard deviation; US$, United States dollars.
a 5597 households.
b 6484 households.
c Estimates for difference in change between 2005 and 2008, calculated using ordinary least-squares regression and with adjustment for the survey design. Difference-in-differences estimates for variables that are binary (such as the ones listed as a percentage of deliveries) are percentage point changes, while for last four rows, where the outcome (household costs) is a continuous variable, the difference-in-differences estimate of programme impact is interpreted as a percentage change.
d Percentages shown are of the deliveries that occurred in a health facility.
e Percentages shown are of the mothers that received such a check-up.
f Based on an exchange rate of approximately 43 Indian rupees to one United States dollar.
The programme was also not associated with changes in the incidence of birth-related maternal complications, the use of antenatal and postnatal services or the use of neonatal intensive care. Our survey data suggests that 54% of the mothers in our sample suffered complications, including premature delivery, prolonged and obstructed labour, excessive bleeding, breech presentation, convulsions, hypertension, fever, incontinence or other birth-related problems after the programme had been implemented – and that the probability of these complications did not significantly change under the Chiranjeevi Yojana programme.
The reimbursement offered to designated health facilities by the Chiranjeevi Yojana programme is intended to cover the costs of delivery for poor women who choose to give birth in a health facility. Even if the programme has not increased institutional delivery rates, we would expect to see lower mean household expenditures on deliveries, given that the programme had paid providers over US$ 32 million as of 2012. However, analysis of our survey data indicated that implementation of the programme had no significant relationship either with the probability that households reported any delivery-related spending (2.69 percentage points; 95% CI: −1.10 to 6.48) or with mean hospital spending for delivery conditional on any spending (18.22% change; 95% CI: –9.91 to 46.34).
In general, the DLHS-3 data also indicated that the programme was not associated with significant changes in household spending for institutional deliveries. The single exception is a 21.2% reduction in mean spending (95% CI: 4.71 to 37.69) among households reporting any expenditure, but this loses statistical significance after adjustment for the multiple comparisons (data not shown). Even among the households of women who delivered in private hospitals, spending on the deliveries appeared not to have changed significantly under the programme.
Discussion
Our findings indicate that the Chiranjeevi Yojana programme was not associated with changes in the probability of institutional delivery (including delivery at private institutions), maternal morbidity or delivery-related household expenditure. These findings differ from those reported by previous evaluations suggesting substantial benefits of the Chiranjeevi Yojana programme, including a 27% increase in institutional deliveries, a 90% reduction in maternal deaths and a 60% reduction in neonatal deaths.8,9,12 These earlier studies did not address self-selection of women into institutional delivery, reporting inaccuracies by hospitals, or any increases in institutional deliveries over time that were unrelated to the programme. The programme was rolled out in a period when the economy of Gujarat was growing by over 10% per year, for example.
Our study also has important limitations. One is that because it was not a randomized, controlled evaluation, we cannot rule out the possibility of confounding. However, we note that our results are robust to the inclusion of a wide variety of control variables and that the staggered introduction of the Chiranjeevi Yojana programme does not appear correlated with pre-existing trend differences in institutional delivery rates (see analysis of DLHS-2 data in Appendix A). Analyses using two independent sources of data (our survey and DLHS-3) also yielded very similar results. Another limitation of our study is that it relied on respondents’ recall of primary outcomes for a period of up to 5 years. Poor recall quality in the household surveys is a potential concern, although we followed the methods of the well regarded Demographic and Health Surveys’ “fertility roster” to collect these retrospective data.20 The degree of recall error is also unlikely to be related to the implementation of the Chiranjeevi Yojana programme.
There are several possible explanations for observing no increase in the probability of institutional delivery associated with the Chiranjeevi Yojana programme. One is that the quality of services provided by private maternity hospitals is poor or, at least, is perceived to be poor by the local population. As a result, demand for institutional delivery may be low even if such delivery is provided free of charge. Another is that – despite the support of the programme – institutional deliveries in Gujarat remain associated with large transportation costs, informal payments or other expenses that make programme benefits small relative to the full cost of institutional delivery.21
Our finding of little or no association between the Chiranjeevi Yojana programme and the out-of-pocket costs of deliveries is more puzzling. Even if the programme failed to make institutional delivery more attractive for any women, it should have reduced the household expenses for the many poor women who still chose institutional delivery. Although we cannot fully explain this finding, we note media reports of poor women still being asked to pay fees for deliveries in health facilities that were participating in the programme.22,23 It seems possible that some providers are providing extra, chargeable services – or simply increasing side charges. If charges are being made for extra services, those services do not appear to have any discernible health benefits. Further research on this issue is needed.
Acknowledgements
We thank the Department of Health and Family Welfare, Government of Gujarat, for its support. We are grateful to Manveen Kohli, Pragya Pranjali, Razdan Rahman, Harshad Vaidya and the Sambodhi team for their support.
Funding:
Research discussed in this publication has been financed with funds provided by the UK Department For International Financing (DFID) to the International Initiative for Impact Evaluation, Inc. (3ie) and managed through the Global Development Network (GDN), as well as support from the World Bank. The findings, interpretations, and conclusions expressed here are those of the authors and do not necessarily reflect the views of any of the funders, the Board of Executive Directors of the World Bank or the governments they represent.
Competing interests:
None declared.
References
- 1.Hill K, Thomas K, AbouZahr C, Walker N, Say L, Inoue M, et al. Maternal Mortality Working Group Estimates of maternal mortality worldwide between 1990 and 2005: an assessment of available data. Lancet. 2007;370:1311–9. doi: 10.1016/S0140-6736(07)61572-4. [DOI] [PubMed] [Google Scholar]
- 2.Hyder AA, Wali SA, McGuckin J. The burden of disease from neonatal mortality: a review of South Asia and sub-Saharan Africa. BJOG. 2003;110:894–901. doi: 10.1111/j.1471-0528.2003.02446.x. [DOI] [PubMed] [Google Scholar]
- 3.Pitt C, Greco G, Powell-Jackson T, Mills A. Countdown to 2015: assessment of official development assistance to maternal, newborn, and child health, 2003–08. Lancet. 2010;376:1485–96. doi: 10.1016/S0140-6736(10)61302-5. [DOI] [PubMed] [Google Scholar]
- 4.Bhutta ZA, Chopra M, Axelson H, Berman P, Boerma T, Bryce J, et al. Countdown to 2015 decade report (2000–10): taking stock of maternal, newborn, and child survival. Lancet. 2010;375:2032–44. doi: 10.1016/S0140-6736(10)60678-2. [DOI] [PubMed] [Google Scholar]
- 5.Campbell OMR, Graham WJ, Lancet Maternal Survival Series steering group Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368:1284–99. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- 6.Lim SS, Dandona L, Hoisington JA, James SL, Hogan MC, Gakidou E. India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. Lancet. 2010;375:2009–23. doi: 10.1016/S0140-6736(10)60744-1. [DOI] [PubMed] [Google Scholar]
- 7.Mazumdar S, Mills A, Powell-Jackson T. Financial incentives in health: new evidence from India’s Janani Suraksha Yojana Oxford: Health Economics Research Centre; 2011. Available from: http://www.herc.ox.ac.uk/people/tpowelljackson/financial%20incentives%20in%20health [accessed 7 November 2013]. [DOI] [PubMed]
- 8.Singh A, Mavalankar DV, Bhat R, Desai A, Patel SR, Singh PV, et al. Providing skilled birth attendants and emergency obstetric care to the poor through partnership with private sector obstetricians in Gujarat, India. Bull World Health Organ. 2009;87:960–4. doi: 10.2471/BLT.08.060228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mavalankar D, Singh A, Patel SR, Desai A, Singh PV. Saving mothers and newborns through an innovative partnership with private sector obstetricians: Chiranjeevi scheme of Gujarat, India. Int J Gynaecol Obstet. 2009;107:271–6. doi: 10.1016/j.ijgo.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 10.Acharya A, McNamee P. Assessing Gujarat’s ‘Chiranjeevi’ scheme. Econ Polit Wkly. 2009;44:13–5. [Google Scholar]
- 11.Krupp K, Madhivanan P. Leveraging human capital to reduce maternal mortality in India: enhanced public health system or public-private partnership? Hum Resour Health. 2009;7:18. doi: 10.1186/1478-4491-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhat R, Mavalankar DV, Singh PV, Singh N. Maternal healthcare financing: Gujarat’s Chiranjeevi scheme and its beneficiaries. J Health Popul Nutr. 2009;27:249–58. doi: 10.3329/jhpn.v27i2.3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramesh M. Innovation award for Gujarat. The Hindu Business Line. 6 November 2006. Available from: http://www.thehindubusinessline.in/bline/2006/11/06/stories/2006110600801500.htm [accessed 7 November 2013].
- 14.Outcome of Chiranjeevi scheme Gandhinagar: Gujarat Government Department of Health and Family Welfare; 2013. [Google Scholar]
- 15.Health statistics, Gujarat 2009–2010 Gandhinagar: Gujarat Government Vital Statistics Division; 2011. Available from: http://www.gujhealth.gov.in/images/pdf/Health-review-09-10.pdf [accessed 7 November 2003].
- 16.Sundaram K. On identification of households below the poverty line in the BPL Census 2002: some comments on the proposed methodology. Econ Polit Wkly. 2003;38:896–901. [Google Scholar]
- 17.Jinyong H, Todd P, Van der Klaauw W. Identification and estimation of treatment effects with a regression-discontinuity design. Econometrica. 2001;69:201–9. [Google Scholar]
- 18.Filmer D, Pritchett L. Estimating wealth effects without expenditure data – or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–32. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 19.Neyman J, Scott EL. Consistent estimates based on partially consistent observations. Econometrica. 1948;16:1–32. doi: 10.2307/1914288. [DOI] [Google Scholar]
- 20.Das J, Hammer J, Sánchez-Paramo C. The impact of recall periods on reported morbidity and health seeking behavior . J Dev Econ. 2012;98:76–88. doi: 10.1016/j.jdeveco.2011.07.001. [DOI] [Google Scholar]
- 21.Krishna A, Ananthpur K. Globalization, distance and disease: spatial health disparities in rural India. Millennial Asia. 2013;4:3–25. doi: 10.1177/0976399613480879. [DOI] [Google Scholar]
- 22.Chiranjeevi scheme failed to deliver: CAG report. Indian Express 31 March 2011. Available from: http://www.indianexpress.com/news/chiranjeevi-scheme-failed-to-deliver-cag-report/769645/ [accessed 7 November 2013].
- 23.Govt scheme to arrest infant mortality fails to deliver. Times of India. 31 March 2011. Available from: http://articles.timesofindia.indiatimes.com/2011-03-31/ahmedabad/29365735_1_mortality-rate-infant-mortality-govt-scheme [accessed 7 November 2013].


