Abstract
Objective
To estimate the prevalence of diabetes and prediabetes in Bangladesh using national survey data and to identify risk factors.
Methods
Sociodemographic and anthropometric data and data on blood pressure and blood glucose levels were obtained for 7541 adults aged 35 years or more from the biomarker sample of the 2011 Bangladesh Demographic and Health Survey (DHS), which was a nationally representative survey with a stratified, multistage, cluster sampling design. Risk factors for diabetes and prediabetes were identified using multilevel logistic regression models, with adjustment for clustering within households and communities.
Findings
The overall age-adjusted prevalence of diabetes and prediabetes was 9.7% and 22.4%, respectively. Among urban residents, the age-adjusted prevalence of diabetes was 15.2% compared with 8.3% among rural residents. In total, 56.0% of diabetics were not aware they had the condition and only 39.5% were receiving treatment regularly. The likelihood of diabetes in individuals aged 55 to 59 years was almost double that in those aged 35 to 39 years. Study participants from the richest households were more likely to have diabetes than those from the poorest. In addition, the likelihood of diabetes was also significantly associated with educational level, body weight and the presence of hypertension. The prevalence of diabetes varied significantly with region of residence.
Conclusion
Almost one in ten adults in Bangladesh was found to have diabetes, which has recently become a major public health issue. Urgent action is needed to counter the rise in diabetes through better detection, awareness, prevention and treatment.
Résumé
Objectif
Estimer la prévalence du diabète et du prédiabète au Bangladesh en utilisant les données de l'enquête nationale et identifier les facteurs de risque.
Méthodes
Les données sociodémographiques et anthropométriques, ainsi que les données sur la tension artérielle et la glycémie, ont été obtenues pour 7541 adultes âgés de 35 ans ou plus, à partir de l’échantillon de biomarqueurs de l'Enquête sur la démographie et la santé au Bangladesh en 2011, qui était une enquête représentative au niveau national avec une conception d'échantillonnage par grappe stratifiée et à plusieurs étages. Les facteurs de risque pour le diabète et le prédiabète ont été identifiés en utilisant des modèles de régression logistiques multiniveaux avec ajustement pour le regroupement au sein des ménages et des communautés.
Résultats
La prévalence globale du diabète et du prédiabète, ajustée en fonction de l'âge, était de 9,7% et 22,4%, respectivement. Chez les personnes habitant en zone urbaine, la prévalence du diabète ajustée en fonction de l'âge était de 15,2% contre 8,3% chez les personnes habitant en zone rurale. Au total, 56,0% des diabétiques ne savaient pas qu'ils l'étaient et seulement 39,5% recevaient un traitement régulier. La probabilité de diabète chez les individus âgés de 55 à 59 ans était presque deux fois plus élevée que chez les personnes âgées de 35 à 39 ans. Les participants de l'étude qui faisaient partie des ménages les plus riches, étaient plus susceptibles d'avoir le diabète que ceux faisant partie des ménages les plus pauvres. En outre, la probabilité de diabète était également significativement associée avec le niveau d'étude, le poids corporel et la présence d'hypertension. La prévalence du diabète variait significativement selon la région de résidence.
Conclusion
Près d'un adulte sur dix au Bangladesh s'avère être diabétique, ce qui est devenu récemment un problème majeur de santé publique. Il est urgent de prendre des mesures pour lutter contre l’augmentation des cas de diabète via une amélioration du dépistage, de la sensibilisation, de la prévention et du traitement.
Resumen
Objetivo
Estimar la prevalencia de la diabetes y la prediabetes en Bangladesh a partir de datos de encuestas nacionales e identificar los factores de riesgo.
Métodos
Se obtuvieron datos sociodemográficos y antropométricos sobre la presión arterial y los niveles de glucosa en sangre de 7541 adultos de 35 años o mayores de la muestra de biomarcadores de la Encuesta demográfica y de salud de Bangladesh 2011(DHS), esta fue una encuesta representativa a nivel nacional con un diseño de muestreo por conglomerados estratificado y multietápico. Se identificaron los factores de riesgo de la diabetes y la prediabetes mediante modelos de regresión logística multinivel, con ajustes para el agrupamiento en los hogares y las comunidades.
Resultados
La prevalencia general ajustada por edad de la diabetes y la prediabetes fue de 9,7 % y 22,4 %, respectivamente. Entre los residentes urbanos, la prevalencia ajustada por edad de la diabetes fue de 15,2 %, en comparación con el 8,3 % entre los residentes rurales. En total, el 56,0 % de los diabéticos no sabían que padecían la condición y solo el 39,5 % recibían tratamiento con frecuencia. La probabilidad de padecer diabetes en individuos de 55 a 59 años era casi el doble que en las mujeres de 35 a 39 años. Los participantes del estudio de los hogares más ricos tenían más posibilidades de padecer diabetes que aquellos de los más pobres. Además, la probabilidad de padecer diabetes también estuvo asociada de forma significativa con el nivel educativo, el peso corporal y la presencia de hipertensión. La prevalencia de diabetes varió según la región de residencia.
Conclusión
Se halló que casi uno de cada diez adultos en Bangladesh padece diabetes, la cual se ha convertido recientemente en un problema de salud pública importante. Se necesitan medidas urgentes para contrarrestar el aumento de la diabetes, mediante la mejora de la detección, la conciencia, la prevención y el tratamiento.
ملخص
الغرض
تقدير انتشار داء السكري ومقدماته في بنغلاديش باستخدام بيانات المسح الوطني وتحديد عوامل الخطر الخاصة به.
الطريقة
تم الحصول على البيانات الديموغرافية الاجتماعية والقياسات البشرية وبيانات تتعلق بضغط الدم ومستويات غلوكوز الدم من 7541 شخصاً بالغاً فوق سن 35 عاماً أو أكثر من عينة الواصمة البيولوجية للمسح الديموغرافي والصحي لبنغلاديش (DHS) لعام 2011، وكان عبارة عن مسح تمثيلي على الصعيد الوطني مع تصميم أخذ العينات الجماعية متعدد المراحل والمقسم إلى طبقات. وتم تحديد عوامل الخطر الخاصة بداء السكري ومقدماته باستخدام نماذج ارتداد لوجستي متعددة المستويات مع تعديل التجميع داخل الأسر والمجتمعات.
النتائج
كانت نسبة الانتشار الإجمالي المعدل باحتساب العمر لداء السكري ومقدماته 9.7 % و22.4 % على التوالي. وبين سكان الحضر، كانت نسبة الانتشار باحتساب العمر لداء السكري 15.2 % مقارنة بنسبة 8.3 % بين سكان الريف. وإجمالاً، لم تكن نسبة 56.0% من المصابين بداء السكري مدركة لإصابتها، بينما كانت نسبة 39.5 % فقط تتلقى العلاج بانتظام. وتضاعفت تقريباً احتمالية الإصابة بداء السكري لدى الأفراد الذين تتراوح أعمارهم بين 55 و59 عاماً عن الأشخاص الذين تتراوح أعمارهم بين 35 و39 عاماً. وكانت احتمالية إصابة المشاركين في الدراسة من الأسر الأكثر ثراءً بداء السكري أعلى عن الأسر الفقيرة. علاوة على ذلك، كانت احتمالية داء السكري أيضاً مرتبطة بشكل كبير بالمستوى التعليمي ووزن الجسم ووجود ارتفاع ضغط الدم. وتنوع انتشار داء السكري بشكل كبير حسب منطقة الإقامة.
الاستنتاج
واحد من بين كل عشرة بالغين تقريباً في بنغلاديش مصاب بداء السكري، وهو ما أصبح مؤخراً مسألة صحية عامة رئيسية. ويتعين اتخاذ إجراء عاجل للتصدي للارتفاع في الإصابة بداء السكري من خلال الاكتشاف والوعي والوقاية والعلاج الأفضل.
摘要
目的
使用全国性调查数据估计孟加拉国糖尿病和前驱糖尿病的患病率并确定风险因素。
方法
从2011年孟加拉人口和健康调查(DHS)的生物标志物样本中获取7541名年满35岁的成年人的社会人口、人体测量数据和有关血压及血糖水平的数据,该调查是采用分层、多级、群集采样设计的全国性典型调查。使用多级逻辑回归模型确定糖尿病和前驱糖尿病的风险因素,在家庭和社区范围内进行群集调整。
结果
糖尿病和前驱糖尿病的整体年龄调整患病率分别为9.7%和22.4%。在城市居民中,糖尿病的年龄调整患病率是15.2%,而农村居民中则为8.3%。总体而言,56.0% 的糖尿病患者不知道自己患有糖尿病,仅39.5%的患者接受定期的治疗。在55至59岁的个人中,患糖尿病的可能性几乎是35至39岁人群的两倍。最富有家庭的研究参与者比最贫穷家庭的参与者更有可能患有糖尿病。此外,患糖尿病的可能性和教育水平、体重以及高血压也有很大关系。糖尿病的患病率在不同的居住区域中有很大差异。
结论
卡拉奇几乎十分之一的成年人患有糖尿病,成为当前主要的公共卫生问题。亟需通过更好的检测、认知、预防和治疗等措施来应对糖尿病蔓延趋势。
Резюме
Цель
Определить распространенность диабета и преддиабетного состояния в Бангладеш на основе данных национального исследования и идентифицировать факторы риска.
Методы
Получены социально-демографические и антропометрические данные и данные об артериальном давлении и уровне глюкозы в крови у 7541 человека в возрасте 35 лет и старше из выборки биомаркеров, полученных в рамках Исследования в области демографии и здравоохранения Бангладеш (2011 г.), представлявшего собой национальное репрезентативное исследование со стратифицированной многоступенчатой кластерной выборкой. Факторы риска диабета и преддиабетного состояния определялись с помощью многоуровневых логистических регрессионных моделей с поправкой на кластеризацию в пределах домохозяйств и общин.
Результаты
Стандартизованная по возрасту общая распространенность диабета и преддиабетного состояния составляла 9,7% и 22,4% соответственно. Среди городских жителей стандартизованная по возрасту распространенность диабета составляла 15,2% по сравнению с 8,3% среди сельских жителей. В итоге, 56,0% больных диабетом не подозревали о наличии у них подобного состояния и только 39,5% регулярно проходили лечение. Вероятность заболевания диабетом у лиц в возрасте 55-59 лет была почти вдвое выше, чем у лиц в возрасте 35-39 лет. Вероятность заболевания диабетом была выше у участников исследования из богатейших домохозяйств, чем из беднейших. К тому же, вероятность заболевания диабетом также в значительной степени была связана с уровнем образования, массой тела и наличием гипертензии. Распространенность диабета значительно варьировалась по регионам проживания.
Вывод
Почти у одной десятой взрослого населения Бангладеш обнаруживается диабет, который недавно стал одной из основных проблем здравоохранения. Необходимо принятие срочных мер по противодействию повышению заболеваемости диабетом посредством улучшения диагностики, информированности, профилактики и лечения.
Introduction
Diabetes mellitus is a leading cause of death and disability worldwide.1,2 Its global prevalence was about 8% in 2011 and is predicted to rise to 10% by 2030.3 Nearly 80% of people with diabetes live in low- and middle-income countries.3 Asia and the eastern Pacific region are particularly affected:3–8 in 2011, China was home to the largest number of adults with diabetes (i.e. 90.0 million, or 9% of the population), followed by India (61.3 million, or 8% of the population) and Bangladesh (8.4 million, or 10% of the population).3 However, many governments and public health planners remain largely unaware of the current prevalence of diabetes and prediabetes, the potential for a future rise in prevalence and the serious complications associated with the disease. Consequently, knowledge of the prevalence of diabetes and prediabetes and of related risk factors could raise awareness of the disease and lead to new policies and strategies for prevention and management.
In Bangladesh, which had a population of 149.8 million in 2011,9 a recent meta-analysis showed that the prevalence of diabetes among adults had increased substantially, from 4% in 1995 to 2000 and 5% in 2001 to 2005 to 9% in 2006 to 2010.5 According to the International Diabetes Federation, the prevalence will be 13% by 2030.3 However, no nationally representative, epidemiological study of the prevalence of diabetes mellitus and its risk factors has been carried out in the country. Previous studies have been limited to specific urban or rural regions or to a single sex or had a small sample.4,10–13 Moreover, no previous study has fully assessed the effect of individual, household and community factors on diabetes and prediabetes. The aims of this study, therefore, were to obtain a nationally representative estimate of the age-adjusted prevalence of diabetes and prediabetes in Bangladesh and to identify individual, household and community factors associated with the conditions.
Methods
The study used data from the most recent Bangladesh Demographic and Health Survey (DHS), which was carried out between July and December 2011 in collaboration with the Bangladesh National Institute of Population Research and Training. Nationally representative, probability samples of men and women were selected for interview using a two-stage, stratified cluster sample of households that included strata for rural and urban areas and for the seven administrative divisions of Bangladesh.14 The primary sampling units, each of which contained 120 households on average, were taken from the most recent census enumeration areas. In the first stage of sampling, 600 sampling units were selected, with the probability of selection proportional to the unit size. In the second stage, 30 households were selected within each primary sampling unit by systematic random sampling. Of the 17 964 households selected using this procedure, 17 511 were eligible for inclusion in the survey. Interviews were completed successfully in 17 141 households containing a total of 83 731 household members. The overall response rate for eligible households was 97.9%.
The 2011 DHS was the first national survey in Bangladesh to incorporate the measurement of biomarkers, including blood pressure and blood glucose levels. One in three of the 17 511 eligible households was selected for biomarker measurement. This subsample included 8835 household members aged 35 years or older: 4524 men and 4311 women. After exclusion of nonresponders and individuals with missing data, the final working sample included 7541 respondents (participation rate: 89.17%). The survey received ethical approval from the Institutional Review Board of Macro International in Calverton, United States of America, and from the National Ethical Review Committees in Bangladesh. Informed consent was obtained from all subjects.
Detailed information on the sociodemographic characteristics of all participants was collected by trained staff using a standard questionnaire, which contained questions on the diagnosis and treatment of diabetes and hypertension. Each data collection team included a health technician who was trained to measure blood pressure and collect blood samples. Blood pressure, blood glucose concentration, body weight and height were assessed using standard methods, as previously described.15 Blood pressure was measured using a LifeSource UA-767 Plus blood pressure monitor (A&D Medical, San Jose, USA), as recommended by the World Health Organization (WHO). Three measurements were taken at approximately 10-minute intervals and the respondent’s blood pressure was obtained by averaging the second and third measurements. Blood glucose was measured using the HemoCue Glucose 201 Analyzer (Teleflex Medical L.P., Markham, Canada) in whole blood obtained by finger prick from capillaries in the middle or ring finger after an overnight fast – an approach that is widely used in resource-limited countries.10,15,16 Blood glucose measurements were adjusted to obtain equivalent plasma glucose levels.17
Prediabetes and diabetes were defined according to WHO and American Diabetes Association criteria.16,18 Prediabetes was defined as a fasting blood glucose level of 6.1 mmol/L to 6.9 mmol/L, without medication. Diabetes was defined as a level greater than or equal to 7.0 mmol/L or self-reported diabetes medication use. These levels have been used in previous studies in Bangladesh15 and in other Asian countries.19–21
We investigated whether the following characteristics of individuals, their communities and their households were associated with the risk of diabetes or prediabetes: the respondent’s age, sex, marital status, educational level, working status and body mass index; the presence of hypertension, which was defined as a systolic blood pressure ≥ 140 mmHg or a diastolic blood pressure ≥ 90 mmHg or current treatment with antihypertensive medication; rural or urban residence; region of residence; and household socioeconomic status. Household socioeconomic status was derived from the household wealth index reported in the Bangladesh DHS, which was based on the household’s amenities, assets and living conditions.22 Households were classified as belonging to a socioeconomic status quintile according to the household wealth index quintile to which they belonged.
Statistical analysis
The study was designed and reported in accordance with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.23 Differences in variables between individuals with diabetes and those without were assessed using a t test or χ2 test for continuous and categorical variables, respectively. The prevalence of diabetes and prediabetes was estimated for the whole study population and for population subgroups. The age-adjusted prevalence of diabetes and prediabetes was derived using logistic regression models. Prevalence estimates took into account the complex survey design and sampling weights.
In the Bangladesh DHS data, individuals were mainly nested in households, which were nested in communities. Thus, individuals in the same household and households in the same community were strongly clustered. Multilevel models were used to compensate for the effect of clustering at individual and household levels.24 Consequently, we assessed associations between individual, household and community characteristics and the presence or absence of diabetes and the presence or absence of prediabetes using three separate multilevel logistic regression models. The first model included only individual and household characteristics and the random intercept at the household and community level. The second model included only community characteristics and had no random intercept. The third (i.e. full) model included individual, household and community characteristics to account for clustering of individuals within households and households within communities. Imputation, based on a regression model, was used to estimate missing values from known values to account for missing data, most frequently for the body mass index (i.e. in 30.6% of respondents).25 Age, sex and place of residence were included as covariates in the imputation. All statistical analyses were performed using Stata version 12.1 (StataCorp. LP, College Station, USA).
Results
The sociodemographic and health characteristics of individuals in the study population and details of their households and communities are presented in Table 1 (available at: http://www.who.int/bulletin/volumes/92/3/13-128371), according to whether or not they had diabetes. Individuals with diabetes were significantly older than those without, they were significantly less likely to have no formal education or to be hypertensive and they were significantly more likely to be currently working or to be overweight or obese. In addition, diabetics were more likely to come from a household with a high socio-economic status: 40.7% came from the richest quintile, whereas 12.7% came from the poorest quintile.
Table 1. Characteristics of the study population aged 35 years or more, Bangladesh, 2011.
| Characteristic | No. (%)a,b |
Pc | ||
|---|---|---|---|---|
| All (n = 7541) | No. without diabetes (n = 6746) | No. with diabetes (n = 795) | ||
| Individual | ||||
| Age in years, mean ± SE | 51.48 ± 0.17 | 51.31 ± 0.18 | 53.01 ± 0.54 | < 0.01 |
| Sex | 0.19 | |||
| Male | 3721 (49.3) | 3342 (49.6) | 379 (46.9) | NA |
| Female | 3820 (50.7) | 3404 (50.4) | 416 (53.1) | NA |
| Educational level | < 0.01 | |||
| No education | 3418 (48.2) | 3156 (49.6) | 262 (36.1) | NA |
| Primary education | 2080 (26.8) | 1869 (26.8) | 211 (26.7) | NA |
| Secondary education | 1403 (17.4) | 1217 (16.9) | 186 (21.3) | NA |
| Higher education | 640 (7.6) | 504 (6.7) | 136 (15.9) | NA |
| Currently working | < 0.01 | |||
| Yes | 3898 (52.2) | 3439 (51.5) | 459 (58.7) | NA |
| No | 3643 (47.8) | 3307 (48.5) | 336 (41.3) | NA |
| Marital status | 0.09 | |||
| Currently married | 6329 (84.2) | 5683 (84.5) | 646 (81.8) | NA |
| Divorced, widowed or other | 1212 (15.8) | 1063 (15.5) | 149 (18.2) | NA |
| Hypertension | < 0.01 | |||
| Yes | 5568 (74.5) | 5093 (76.0) | 475 (60.1) | NA |
| No | 1973 (25.5) | 1653 (24.0) | 320 (39.9) | NA |
| Body weight | < 0.01 | |||
| Normal | 6915 (92.8) | 6272 (93.9) | 643 (82.8) | NA |
| Overweight or obese | 626 (7.2) | 474 (6.1) | 152 (17.2) | NA |
| Household | ||||
| Socioeconomic status | < 0.01 | |||
| Poorest | 1343 (19.5) | 1252 (20.3) | 91 (12.7) | NA |
| Poorer | 1351 (19.1) | 1267 (19.8) | 84 (12.2) | NA |
| Middle | 1461 (19.8) | 1364 (20.6) | 97 (12.7) | NA |
| Richer | 1581 (20.7) | 1422 (20.6) | 159 (21.8) | NA |
| Richest | 1805 (20.9) | 1441 (18.7) | 364 (40.7) | NA |
| Community | ||||
| Place of residence | < 0.01 | |||
| Urban | 2480 (23.3) | 2115 (22.0) | 365 (35.4) | NA |
| Rural | 5061 (76.7) | 4631 (78.0) | 430 (64.6) | NA |
| Region of residence | < 0.01 | |||
| Khulna division | 1204 (13.2) | 1112 (13.7) | 92 (8.6) | NA |
| Barisal division | 860 (5.7) | 755 (5.5) | 105 (6.7) | NA |
| Chittagong division | 1116 (16.7) | 973 (16.1) | 143 (21.4) | NA |
| Dhaka division | 1312 (32.7) | 1172 (32.5) | 140 (33.4) | NA |
| Rajshahi division | 1064 (14.4) | 949 (14.3) | 115 (14.4) | NA |
| Rangpur division | 1068 (12.0) | 977 (12.2) | 91 (9.8) | NA |
| Sylhet division | 917 (5.7) | 808 (5.6) | 109 (5.8) | NA |
NA, not applicable; SE, standard error.
a All values represent absolute numbers and percentages unless otherwise stated.
b In estimating percentages, the complex survey design and sampling weights were taken into account.
c P-values were derived using a t test or χ2 test for continuous and categorical variables, respectively.
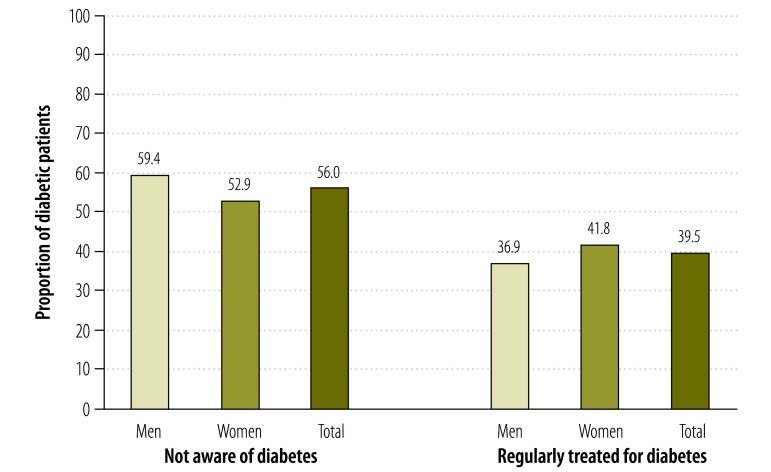
The unadjusted and age-adjusted prevalence of diabetes and prediabetes are presented in Table 2, according to the characteristics of individuals in the study population and their households and communities. Overall, the age-adjusted prevalence of diabetes and prediabetes was 9.7% and 22.4%, respectively, and there was no significant difference between the sexes. However, the age-adjusted prevalence of diabetes among urban residents was almost double that in rural residents: 15.2% versus 8.3%, respectively. In contrast, the age-adjusted prevalence of prediabetes was slightly lower among urban than rural residents: 19.0% versus 23.5%, respectively. Among diabetics, 56.0% were unaware they had the condition and only 39.5% were receiving treatment regularly (Fig. 1).
Table 2. Prevalence of diabetes and prediabetes in individuals aged 35 years or more, by characteristic, Bangladesh, 2011.
| Characteristic | Diabetes prevalence, % (95% CI) |
Prediabetes prevalence, % (95% CI) |
|||
|---|---|---|---|---|---|
| Unadjusted | Age-adjusted | Unadjusted | Age-adjusted | ||
| Individual | |||||
| Sex | |||||
| Male | 9.4 (8.3–10.5) | 9.3 (8.2–10.4) | 22.6 (20.6–24.6) | 22.4 (20.4–24.4) | |
| Female | 10.3 (9.2–11.4) | 10.4 (9.3–11.5) | 22.4 (20.5–24.4) | 22.5 (20.6–24.5) | |
| Educational level | |||||
| No education | 7.4 (6.3–8.4) | 7.0 (6.1–8.0) | 22.6 (20.6–24.9) | 22.3 (20.2–24.5) | |
| Primary education | 9.9 (8.4–11.3) | 10.1 (8.6–11.6) | 23.2 (20.7–25.8) | 23.3 (20.7–25.8) | |
| Secondary education | 12.1 (10.1–14.1) | 12.8 (10.7–15.0) | 21.9 (19.1–24.9) | 22.2 (19.3–25.2) | |
| Higher education | 20.6 (17.3–23.9) | 21.9 (18.4–25.5) | 20.5 (16.6–25.0) | 21.2 (16.9–25.4) | |
| Currently working | |||||
| Yes | 11.1 (9.9–12.3) | 10.9 (9.8–12.1) | 22.2 (20.3–24.4) | 22.5 (20.4–24.5) | |
| No | 8.5 (7.5–9.6) | 8.7 (7.6–9.7) | 22.7 (20.7–24.8) | 22.5 (20.4–24.5) | |
| Marital status | |||||
| Currently married | 9.6 (8.7–10.5) | 9.7 (8.8–10.6) | 22.3 (20.6–24.1) | 22.5 (20.7–24.3) | |
| Divorced, widowed or other | 11.4 (9.2–13.5) | 10.7 (8.6–12.7) | 23.4 (20.6–26.6) | 22.3 (19.2–25.3) | |
| Hypertension | |||||
| Yes | 8.0 (7.1–8.8) | 8.0 (7.2–8.9) | 24.0 (22.1–25.9) | 17.6 (15.4–19.8) | |
| No | 15.4 (13.4–17.5) | 15.1 (13.1–17.0) | 18.2 (16.0–20.5) | 24.2 (22.3–26.1) | |
| Body weight | |||||
| Normal | 8.8 (8.0–9.6) | 8.8 (8.0–9.7) | 22.3 (20.6–24.1) | 22.3 (20.5–24.0) | |
| Overweight or obese | 23.5 (19.1–27.8) | 22.8 (18.7–27.0) | 25.2 (21.5–29.4) | 25.2 (21.2–29.1) | |
| Household | |||||
| Socioeconomic status | |||||
| Poorest | 6.4 (4.8–8.0) | 6.4 (4.8–8.0) | 23.6 (20.2–27.3) | 23.5 (20.0–27.1) | |
| Poorer | 6.3 (4.7–7.9) | 6.3 (4.7–7.8) | 23.8 (20.7–27.3) | 23.8 (20.5–27.2) | |
| Middle | 6.3 (5.0–7.6) | 6.3 (5.0–7.6) | 24.5 (21.5–27.7) | 24.4 (21.2–27.5) | |
| Richer | 10.4 (8.5–12.2) | 10.4 (8.6–12.2) | 21.2 (18.6–24.1) | 21.2 (18.4–23.9) | |
| Richest | 19.2 (16.9–21.5) | 19.3 (17.0–21.6) | 19.6 (17.0–22.4) | 19.7 (17.0–22.5) | |
| Community | |||||
| Place of residence | |||||
| Urban | 15.0 (13.0–16.9) | 15.2 (13.2–17.2) | 18.8 (16.4–21.5) | 19.0 (16.4–21.6) | |
| Rural | 8.3 (7.4–9.2) | 8.3 (7.4–9.2) | 23.6 (21.6–25.7) | 23.5 (21.5–25.6) | |
| Region of residence | |||||
| Khulna division | 6.4 (5.2–7.6) | 6.4 (5.2–7.6) | 17.0 (14.1–20.4) | 17.0 (13.9–20.1) | |
| Barisal division | 11.7 (9.4–14.0) | 11.6 (9.3–13.8) | 29.1 (24.9–33.7) | 28.9 (24.5–33.3) | |
| Chittagong division | 12.7 (10.4–14.9) | 12.4 (10.3–14.7) | 29.3 (25.0–34.1) | 29.2 (24.7–33.8) | |
| Dhaka division | 10.1 (8.2–12.0) | 10.2 (8.2–12.1) | 19.5 (16.4–23.1) | 19.5 (16.1–22.9) | |
| Rajshahi division | 9.9 (8.0–11.9) | 10.2 (8.2–12.2) | 23.7 (19.2–28.8) | 23.8 (19.0–28.6) | |
| Rangpur division | 8.1 (6.0–10.2) | 8.0 (6.0–10.1) | 19.9 (15.7–24.9) | 20.0 (15.4–24.5) | |
| Sylhet division | 10.2 (8.1–12.0) | 10.0 (8.1–12.0) | 27.8 (22.7–33.5) | 27.8 (22.4–33.1) | |
| Overall prevalence | 9.9 (9.0–10.7) | 9.7 (4.2–10.5) | 22.5 (20.8–24.2) | 22.4 (20.7–24.1) | |
CI, confidence interval.
Fig. 1.
Diabetics aged 35 years or older who are not aware of their condition and receiving regular treatment, Bangladesh, 2011
Table 3 shows the risk factors associated with prediabetes identified using the three multilevel logistic regression models. The fully adjusted model indicated that older age, high educational level and high body weight were significantly and positively associated with prediabetes. The risk of prediabetes in individuals aged 60 to 69 years was 1.64 times that in younger individuals aged 35 to 39 years; in those aged 70 years or more, the risk was 1.81 times that in the younger age group. The risk in overweight or obese individuals was more than double that in normal-weight individuals. Risk also varied with region of residence: residents in the Barisal division had more than double the risk of prediabetes than those in the Khulna division.
Table 3. Risk factors associated with prediabetes in individuals aged 35 years or more, Bangladesh, 2011.
| Characteristic | Logistic regression modela |
|||||||
|---|---|---|---|---|---|---|---|---|
| Firstb |
Secondc |
Fulld |
||||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |||
| Individual | ||||||||
| Age group (years) | ||||||||
| 35–39 | 1.00 | NA | NA | NA | 1.00 | NA | ||
| 40–44 | 1.18 (0.94–1.47) | 0.16 | NA | NA | 1.16 (0.92–1.45) | 0.21 | ||
| 45–49 | 1.27 (1.01–1.60) | 0.04 | NA | NA | 1.27 (1.01–1.60) | 0.04 | ||
| 50–54 | 1.43 (1.12–1.82) | < 0.01 | NA | NA | 1.39 (1.09–1.77) | 0.01 | ||
| 55–59 | 1.40 (1.06–1.86) | 0.02 | NA | NA | 1.36 (1.03–1.81) | 0.03 | ||
| 60–69 | 1.69 (1.31–2.18) | < 0.01 | NA | NA | 1.64 (1.27–2.12) | < 0.01 | ||
| ≥ 70 | 1.84 (1.37–2.47) | < 0.01 | NA | NA | 1.81 (1.35–2.43) | < 0.01 | ||
| Sex | ||||||||
| Male | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Female | 1.16 (0.92–1.45) | 0.21 | NA | NA | 1.18 (0.94–1.48) | 0.16 | ||
| Educational level | ||||||||
| No education | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Primary education | 1.16 (0.98–1.38) | 0.09 | NA | NA | 1.11 (0.93–1.31) | 0.25 | ||
| Secondary education | 1.22 (0.98–1.51) | 0.07 | NA | NA | 1.17 (0.95–1.46) | 0.15 | ||
| Higher education | 1.51 (1.1–2.07) | 0.01 | NA | NA | 1.49 (1.09–2.03) | 0.01 | ||
| Currently working | ||||||||
| Yes | 0.93 (0.74–1.16) | 0.51 | NA | NA | 0.98 (0.78–1.22) | 0.85 | ||
| No | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Marital status | ||||||||
| Currently married | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Divorced, widowed or other | 0.96 (0.77–1.19) | 0.70 | NA | NA | 0.92 (0.74–1.15) | 0.48 | ||
| Hypertension | ||||||||
| Yes | 0.67 (0.57–0.8) | < 0.01 | NA | NA | 0.71 (0.60–0.84) | < 0.01 | ||
| No | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Body weight | ||||||||
| Normal | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Overweight or obese | 2.04 (1.57–2.65) | < 0.01 | NA | NA | 2.05 (1.58–2.67) | < 0.01 | ||
| Household | ||||||||
| Socioeconomic status | ||||||||
| Poorest | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Poorer | 1.04 (0.82–1.32) | 0.77 | NA | NA | 0.99 (0.78–1.25) | 0.91 | ||
| Middle | 1.01 (0.79–1.28) | 0.96 | NA | NA | 0.96 (0.76–1.21) | 0.72 | ||
| Richer | 0.81 (0.64–1.03) | 0.09 | NA | NA | 0.81 (0.64–1.04) | 0.10 | ||
| Richest | 0.85 (0.65–1.11) | 0.23 | NA | NA | 0.88 (0.67–1.17) | 0.40 | ||
| Community | ||||||||
| Place of residence | ||||||||
| Urban | NA | NA | 1.00 | NA | 1.00 | NA | ||
| Rural | NA | NA | 1.20 (0.95–1.51) | 0.12 | 1.10 (0.92–1.31) | 0.31 | ||
| Region of residence | ||||||||
| Khulna division | NA | NA | 1.00 | NA | 1.00 | NA | ||
| Barisal division | NA | NA | 2.20 (1.58–3.06) | < 0.01 | 2.52 (1.89–3.35) | < 0.01 | ||
| Chittagong division | NA | NA | 2.30 (1.64–3.23) | < 0.01 | 2.04 (1.56–2.67) | < 0.01 | ||
| Dhaka division | NA | NA | 1.28 (0.93–1.77) | 0.13 | 1.13 (0.86–1.47) | 0.38 | ||
| Rajshahi division | NA | NA | 1.60 (1.12–2.29) | 0.01 | 1.50 (1.14–1.97) | < 0.01 | ||
| Rangpur division | NA | NA | 1.23 (0.84–1.81) | 0.28 | 1.12 (0.85–1.48) | 0.43 | ||
| Sylhet division | NA | NA | 1.99 (1.39–2.87) | < 0.01 | 1.98 (1.50–2.63) | < 0.01 | ||
CI, confidence interval; NA, not applicable; OR, odds ratio.
a The analysis included data from 600 communities, 4162 households and 6746 household members.
b The first logistic regression model considered only individual and household characteristics.
c The second model considered only community characteristics.
d The full model considered individual, household and community characteristics.
Table 4 shows the risk factors associated with diabetes. The risk factors identified using the logistic regression model based on sociodemographic and health characteristics only were similar to those identified using the fully adjusted model. There was a positive association between older age and the risk of diabetes. The risk was significantly higher in individuals aged 45 to 49 years and in those aged 55 years or older than in younger individuals aged 35 to 39 years; for example, in those aged 55 to 59 years, the risk was about twice that in those aged 35 to 39 years. In addition, the risk of diabetes was significantly associated with a high educational level, hypertension, being overweight or obese and belonging to one of the richest households. The fully adjusted model showed that the risk in individuals currently working was 0.72 more than in those who were not. There was a striking variation in risk among the seven administrative divisions of Bangladesh: the risk in individuals living in Barisal and Chittagong divisions was around double that of those living in the Khulna division. Moreover, the risk of diabetes was also significantly higher in individuals from the Dhaka, Rajshahi and Sylhet divisions than in those from the Khulna division.
Table 4. Risk factors associated with diabetes in individuals aged 35 years or more, Bangladesh, 2011.
| Characteristic | Logistic regression modela |
|||||||
|---|---|---|---|---|---|---|---|---|
| Firstb |
Secondc |
Fulld |
||||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |||
| Individual | ||||||||
| Age group (years) | ||||||||
| 35–39 | 1.00 | NA | NA | NA | 1.00 | NA | ||
| 40–44 | 1.16 (0.86–1.56) | 0.33 | NA | NA | 1.17 (0.87–1.57) | 0.30 | ||
| 45–49 | 1.46 (1.09–1.95) | 0.01 | NA | NA | 1.46 (1.09–1.96) | 0.01 | ||
| 50–54 | 1.35 (0.98–1.85) | 0.06 | NA | NA | 1.33 (0.97–1.82) | 0.08 | ||
| 55–59 | 1.94 (1.40–2.69) | < 0.01 | NA | NA | 1.94 (1.40–2.68) | < 0.01 | ||
| 60–69 | 1.52 (1.10–2.10) | 0.01 | NA | NA | 1.51 (1.09–2.08) | 0.01 | ||
| ≥ 70 | 1.81 (1.27–2.6) | < 0.01 | NA | NA | 1.82 (1.27–2.60) | < 0.01 | ||
| Sex | ||||||||
| Male | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Female | 0.95 (0.73–1.25) | 0.72 | NA | NA | 0.96 (0.73–1.25) | 0.75 | ||
| Educational level | ||||||||
| No education | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Primary education | 1.39 (1.12–1.73) | < 0.01 | NA | NA | 1.36 (1.09–1.69) | 0.01 | ||
| Secondary education | 1.55 (1.21–2.00) | < 0.01 | NA | NA | 1.52 (1.18–1.96) | < 0.01 | ||
| Higher education | 2.18 (1.58–3.00) | < 0.01 | NA | NA | 2.12 (1.53–2.92) | < 0.01 | ||
| Currently working | ||||||||
| Yes | 0.71 (0.54–0.92) | 0.01 | NA | NA | 0.72 (0.55–0.94) | 0.01 | ||
| No | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Marital status | ||||||||
| Currently married | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Divorced, widowed or other | 1.09 (0.84–1.40) | 0.52 | NA | NA | 1.06 (0.82–1.36) | 0.67 | ||
| Hypertension | ||||||||
| Yes | 1.54 (1.29–1.84) | < 0.01 | NA | NA | 1.57 (1.31–1.88) | < 0.01 | ||
| No | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Body weight | ||||||||
| Normal | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Overweight or obese | 1.93 (1.51–2.47) | < 0.01 | NA | NA | 1.93 (1.52–2.47) | < 0.01 | ||
| Household | ||||||||
| Socioeconomic status | ||||||||
| Poorest | 1.00 | NA | NA | NA | 1.00 | NA | ||
| Poorer | 0.82 (0.59–1.14) | 0.23 | NA | NA | 0.79 (0.57–1.10) | 0.17 | ||
| Middle | 0.82 (0.59–1.13) | 0.22 | NA | NA | 0.80 (0.58–1.10) | 0.17 | ||
| Richer | 1.14 (0.84–1.55) | 0.39 | NA | NA | 1.12 (0.82–1.52) | 0.48 | ||
| Richest | 2.22 (1.64–3.02) | < 0.01 | NA | NA | 2.15 (1.55–2.98) | < 0.01 | ||
| Community | ||||||||
| Place of residence | ||||||||
| Urban | NA | NA | 1.00 | NA | 1.00 | NA | ||
| Rural | NA | NA | 0.51 (0.42–0.63) | < 0.01 | 0.94 (0.77–1.15) | 0.57 | ||
| Region of residence | ||||||||
| Khulna division | NA | NA | 1.00 | NA | 1.00 | NA | ||
| Barisal division | NA | NA | 2.01 (1.49–2.71) | < 0.01 | 2.06 (1.47–2.88) | < 0.01 | ||
| Chittagong division | NA | NA | 2.06 (1.54–2.76) | < 0.01 | 1.90 (1.39–2.60) | < 0.01 | ||
| Dhaka division | NA | NA | 1.48 (1.10–1.98) | 0.01 | 1.42 (1.04–1.94) | 0.03 | ||
| Rajshahi division | NA | NA | 1.65 (1.22–2.23) | < 0.01 | 1.68 (1.22–2.33) | < 0.01 | ||
| Rangpur division | NA | NA | 1.36 (0.96–1.92) | 0.08 | 1.44 (1.03–2.03) | 0.03 | ||
| Sylhet division | NA | NA | 1.70 (1.26–2.29) | < 0.01 | 1.71 (1.23–2.39) | < 0.01 | ||
CI, confidence interval; NA, not applicable; OR, odds ratio.
a The analysis included data from 600 communities, 4162 households and 6746 household members.
b The first logistic regression model considered only individual and household characteristics.
c The second model considered only community characteristics.
d The full model considered individual, household and community characteristics.
Discussion
In this, the first, nationally representative study in Bangladesh, we estimated the prevalence of prediabetes and diabetes and quantified the effect of risk factors for these conditions associated with the characteristics of individuals and their households and communities. The findings suggest that diabetes has become epidemic among the adult population of Bangladesh: around 10% of study participants had diabetes and around 23% had prediabetes. We also found that the prevalence of prediabetes and diabetes varied substantially with the individual’s age, educational level and body weight, the presence of hypertension, household socioeconomic status and region of residence.
Our study’s findings are consistent with the increasing prevalence of diabetes in Bangladesh observed in a previous systematic review.5 Similar figures have been noted recently in most Asian countries: 10% in China,7,8 9% in India,3 8% in the Islamic Republic of Iran,26 11% in Pakistan6 and 8% in the Republic of Korea.20 However, the prevalence was only 4% in Viet Nam, perhaps due to differences in climate or dietary habits.19 We also found that the prevalence of prediabetes was slightly lower among urban than rural residents (19% versus 24%, respectively), as was observed in a study in China.7 In contrast, the prevalence of diabetes was significantly higher among urban than rural residents (15% versus 8%, P < 0.001). Similar findings have been reported previously in Bangladesh (8% versus 4% in the two groups, respectively),27 China (11% versus 8%)7 and the Islamic Republic of Iran (18% versus 15%).26 Diabetes may be more common among urban residents in these countries because they have a more sedentary lifestyle or different dietary habits or are more likely to be overweight or obese.28,29
The associations we found between diabetes and age and body weight are similar to those observed around the world. However, associations with educational level and household socioeconomic status vary internationally. The positive associations we found between these two factors and diabetes have also been observed previously in Bangladesh,27 China7,30 and India.31 In contrast, another study in China found that the prevalence of diabetes was generally unaffected by educational level but was higher in the high-income group.32 Moreover, studies from both developing and developed countries have found inverse associations between diabetes and educational level and household socioeconomic status, perhaps because the better-educated were more health-conscious.19,33–35 However, obesity appears to be an independent risk factor for diabetes and a study from Brazil showed that better-educated and wealthier individuals were more likely to be obese.36 Several other studies in developing countries also showed that the risk of obesity and diabetes increased with socioeconomic status.11,37,38 In our study, the risk of diabetes was greater in individuals with hypertension than in those without, as has been reported elsewhere.4,7,11,12 The reason for the regional variation we found in the prevalence of diabetes and prediabetes is unclear and needs further investigation.
In our study, 56% of diabetics were not aware they had the disease and only 40% were receiving treatment regularly. Similarly, the International Diabetes Federation reported recently that over 50% of people with diabetes in south Asia were unaware of their condition.3 The epidemic of diabetes in developing countries is affecting young people and is causing disability, loss of income and early death.1–3,39,40 Since the working-age population is especially susceptible, the economic potential of these countries could be reduced. A study in Bangladesh showed that about 12% of households either borrow money or sell household assets to pay for diabetes treatment.41 Consequently, diabetes is not only causing serious health problems but is also placing a financial burden on households.
Although diabetes and other chronic diseases are serious public health problems in Bangladesh, they are given only a low priority by the health-care system. In particular, achieving good outcomes in individuals with diabetes in Bangladesh is hampered by: (i) the unavailability of health insurance, except in small areas of the country where it is provided by programmes run by nongovernmental organizations; (ii) inadequately trained staff and limited health-care facilities in rural areas; (iii) rapid lifestyle changes caused by urbanization; and (iv) the absence of health awareness programmes in the education curriculum. The best way to ensure accessible and affordable care is by introducing universal health coverage.42,43 Given that an epidemiological transition currently appears to be under way in Bangladesh, it is important that any mechanism for pooling risk introduced into the country on the way to universal health coverage should incorporate support for public health programmes that target the prevention and management of diabetes. This will ensure a central role for noncommunicable diseases from the start. In addition, patient-related risk factors, such as tobacco use, being overweight or obese and physical inactivity, have also become public health problems in Bangladesh.44,45 Tackling these factors could also make an important contribution to the management of diabetes in the country.46,47
Our study has several strengths and limitations. The main strengths are the large sample size, the coverage of both rural and urban areas and the nationally representative study population. In addition, the findings provide detailed information on a wide range of risk factors for diabetes and prediabetes. However, the study’s cross-sectional nature means that it was not possible to establish a causal relationship between these risk factors and the occurrence of the two conditions. In addition, no information was collected on physical activity levels, tobacco use or dietary habits, which have all been associated with obesity, prediabetes and diabetes in other studies.30,35,48 Consequently, we were unable to control for, or assess, the independent effects of these factors on the prevalence of diabetes and prediabetes. Since understanding the influence of these factors is important for improving the prevention and management of diabetes, further studies in Bangladeshi adults are needed.
In conclusion, our findings show that diabetes and prediabetes are highly prevalent among individuals aged 35 years or more in Bangladesh. The risk of both diabetes and prediabetes was increased in older, wealthier and better-educated individuals, in those with hypertension and in those living in the Barisal and Chittagong divisions. A substantial proportion of diabetics was not aware they had the disease and the majority were not receiving regular treatment.
The challenge of diabetes in Bangladesh could be tackled by: (i) incorporating information on the prevention and control of diabetes into government health promotion programmes; (ii) encouraging all adults to participate in an annual screening programme; (iii) paying more attention to prediabetes, which can be ameliorated by lifestyle changes; and (iv) managing body weight, which was associated with diabetes and prediabetes in our study, by means of lifestyle measures since this will prevent or delay the complications of diabetes.49
Acknowledgements
The authors thank MEASURE DHS for permission to use data from the 2011 Bangladesh DHS. M Mizanur Rahman is also affiliated with the Department of Population Science and Human Resource Development, University of Rajshahi, Rajshahi, Bangladesh.
Competing interests:
None declared.
References
- 1.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 3.International Diabetes Federation (IDF) [Internet]. Country estimates table 2011. IDF diabetes atlas. 6th ed. 2012. Available from: http://www.idf.org/sites/default/files/EN_6E_Atlas_Full_0.pdf [accessed 7 June 2013].
- 4.Rahim MA, Hussain A, Azad Khan AK, Sayeed MA, Keramat Ali SM, Vaaler S. Rising prevalence of type 2 diabetes in rural Bangladesh: a population based study. Diabetes Res Clin Pract. 2007;77:300–5. doi: 10.1016/j.diabres.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 5.Saquib N, Saquib J, Ahmed T, Khanam MA, Cullen MR. Cardiovascular diseases and type 2 diabetes in Bangladesh: a systematic review and meta-analysis of studies between 1995 and 2010. BMC Public Health. 2012;12:434. doi: 10.1186/1471-2458-12-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shera AS, Rafique G, Khawaja IA, Baqai S, King H. Pakistan National Diabetes Survey: prevalence of glucose intolerance and associated factors in Baluchistan province. Diabetes Res Clin Pract. 1999;44:49–58. doi: 10.1016/S0168-8227(99)00017-0. [DOI] [PubMed] [Google Scholar]
- 7.Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. China National Diabetes and Metabolic Disorders Study Group Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090–101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 8.Zhang H, Xu W, Dahl AK, Xu Z, Wang HX, Qi X. Relation of socio-economic status to impaired fasting glucose and type 2 diabetes: findings based on a large population-based cross-sectional study in Tianjin, China. Diabet Med. 2013;30:e157–62. doi: 10.1111/dme.12156. [DOI] [PubMed] [Google Scholar]
- 9.Bangladesh population and housing census 2011 Dhaka: Bangladesh Bureau of Statistics, Government of the People’s Republic of Bangladesh; 2012. [Google Scholar]
- 10.Abu Sayeed M, Banu A, Khan AR, Hussain MZ. Prevalence of diabetes and hypertension in a rural population of Bangladesh. Diabetes Care. 1995;18:555–8. doi: 10.2337/diacare.18.4.555. [DOI] [PubMed] [Google Scholar]
- 11.Ahasan HN, Islam MZ, Alam MB, Miah MT, Nur Z, Mohammed FR, et al. Prevalence and risk factors of type 2 diabetes mellitus among Secretariat employees of Bangladesh. J Med. 2011;12:125–30. [Google Scholar]
- 12.Bhowmik B, Afsana F, My Diep L, Binte Munir S, Wright E, Mahmood S, et al. Increasing prevalence of type 2 diabetes in a rural Bangladeshi population: a population based study for 10 years. Diabetes Metab J. 2013;37:46–53. doi: 10.4093/dmj.2013.37.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hussain A, Rahim MA, Azad Khan AK, Ali SM, Vaaler S. Type 2 diabetes in rural and urban population: diverse prevalence and associated risk factors in Bangladesh. Diabet Med. 2005;22:931–6. doi: 10.1111/j.1464-5491.2005.01558.x. [DOI] [PubMed] [Google Scholar]
- 14.MEASURE DHS [Internet]. Demographic and Health Surveys. Publications by country. Available from: http://www.measuredhs.com/Publications/Publications-by-Country.cfm [accessed 10 February 2013].
- 15.Bangladesh Demographic and Health Survey 2011. Dhaka: National Institute of Population Research and Training (NIPORT); 2013. Available from: http://www.measuredhs.com/publications/publication-FR265-DHS-Final-Reports.cfm [accessed 10 February 2013]. [Google Scholar]
- 16.International Diabetes Federation. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: report of a WHO/IDF consultation Geneva: World Health Organization; 2006. [Google Scholar]
- 17.D’Orazio P, Burnett RW, Fogh-Andersen N, Jacobs E, Kuwa K, Külpmann WR, et al. International Federation of Clinical Chemistry Scientific Division Working Group on Selective Electrodes and Point of Care Testing Approved IFCC recommendation on reporting results for blood glucose (abbreviated). Clin Chem. 2005;51:1573–6. doi: 10.1373/clinchem.2005.051979. [DOI] [PubMed] [Google Scholar]
- 18.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2005;28(Suppl 1):S37–42. doi: 10.2337/diacare.28.suppl_1.S37. [DOI] [PubMed] [Google Scholar]
- 19.Duc Son LN, Kusama K, Hung NT, Loan TTH, Chuyen NV, Kunii D, et al. Prevalence and risk factors for diabetes in Ho Chi Minh City, Vietnam. Diabet Med. 2004;21:371–6. doi: 10.1111/j.1464-5491.2004.01159.x. [DOI] [PubMed] [Google Scholar]
- 20.Kim SM, Lee JS, Lee J, Na JK, Han JH, Yoon DK, et al. Prevalence of diabetes and impaired fasting glucose in Korea: Korean National Health and Nutrition Survey 2001. Diabetes Care. 2006;29:226–31. doi: 10.2337/diacare.29.02.06.dc05-0481. [DOI] [PubMed] [Google Scholar]
- 21.Khambalia A, Phongsavan P, Smith BJ, Keke K, Dan L, Fitzhardinge A, et al. Prevalence and risk factors of diabetes and impaired fasting glucose in Nauru. BMC Public Health. 2011;11:719. doi: 10.1186/1471-2458-11-719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rutstein SO, Johnson K. The DHS wealth index DHS comparative reports no. 6. Calverton: ORC Macro; 2004. [Google Scholar]
- 23.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;85:867–72. doi: 10.2471/BLT.07.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rabe-Hesketh S, Skrondal A. Multilevel and longitudinal modeling using Stata 3rd ed. College Station: Stata press; 2012. [Google Scholar]
- 25.Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338(jun29):b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Esteghamati A, Gouya MM, Abbasi M, Delavari A, Alikhani S, Alaedini F, et al. Prevalence of diabetes and impaired fasting glucose in the adult population of Iran: National Survey of Risk Factors for Non-Communicable Diseases of Iran. Diabetes Care. 2008;31:96–8. doi: 10.2337/dc07-0959. [DOI] [PubMed] [Google Scholar]
- 27.abu Sayeed M, Ali L, Hussain MZ, Rumi MA, Banu A, Azad Khan AK. Effect of socioeconomic risk factors on the difference in prevalence of diabetes between rural and urban populations in Bangladesh. Diabetes Care. 1997;20:551–5. doi: 10.2337/diacare.20.4.551. [DOI] [PubMed] [Google Scholar]
- 28.Shafique S, Akhter N, Stallkamp G, de Pee S, Panagides D, Bloem MW. Trends of under- and overweight among rural and urban poor women indicate the double burden of malnutrition in Bangladesh. Int J Epidemiol. 2007;36:449–57. doi: 10.1093/ije/dyl306. [DOI] [PubMed] [Google Scholar]
- 29.Muntner P, Gu D, Wildman RP, Chen J, Qan W, Whelton PK, et al. Prevalence of physical activity among Chinese adults: results from the International Collaborative Study of Cardiovascular Disease in Asia. Am J Public Health. 2005;95:1631–6. doi: 10.2105/AJPH.2004.044743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pan XR, Yang WY, Li GW, Liu J, National Diabetes Prevention and Control Cooperative Group Prevalence of diabetes and its risk factors in China, 1994. Diabetes Care. 1997;20:1664–9. doi: 10.2337/diacare.20.11.1664. [DOI] [PubMed] [Google Scholar]
- 31.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al. Diabetes Epidemiology Study Group in India (DESI) High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44:1094–101. doi: 10.1007/s001250100627. [DOI] [PubMed] [Google Scholar]
- 32.Hu D, Sun L, Fu P, Xie J, Lu J, Zhou J, et al. Prevalence and risk factors for type 2 diabetes mellitus in the Chinese adult population: the InterASIA Study. Diabetes Res Clin Pract. 2009;84:288–95. doi: 10.1016/j.diabres.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 33.Borrell LN, Dallo FJ, White K. Education and diabetes in a racially and ethnically diverse population. Am J Public Health. 2006;96:1637–42. doi: 10.2105/AJPH.2005.072884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seeman T, Merkin SS, Crimmins E, Koretz B, Charette S, Karlamangla A. Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988–1994). Soc Sci Med. 2008;66:72–87. doi: 10.1016/j.socscimed.2007.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–9. doi: 10.1001/jama.289.1.76. [DOI] [PubMed] [Google Scholar]
- 36.Monteiro CA, Conde WL, Popkin BM. Independent effects of income and education on the risk of obesity in the Brazilian adult population. J Nutr. 2001;131:881S–6S. doi: 10.1093/jn/131.3.881S. [DOI] [PubMed] [Google Scholar]
- 37.Jebb SA, Moore MS. Contribution of a sedentary lifestyle and inactivity to the etiology of overweight and obesity: current evidence and research issues. Med Sci Sports Exerc. 1999;31(Supp 1):S534–41. doi: 10.1097/00005768-199911001-00008. [DOI] [PubMed] [Google Scholar]
- 38.Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93(Suppl 1):S9–30. doi: 10.1210/jc.2008-1595. [DOI] [PubMed] [Google Scholar]
- 39.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abegunde D, Stanciole A. An estimation of the economic impact of chronic noncommunicable diseases in selected countries Geneva: World Health Organization; 2006. [Google Scholar]
- 41.Rahman MM, Gilmour S, Saito E, Sultana P, Shibuya K. Self-reported illness and household strategies for coping with health-care payments in Bangladesh. Bull World Health Organ. 2013;91:449–58. doi: 10.2471/BLT.12.115428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Savedoff WD, de Ferranti D, Smith AL, Fan V. Political and economic aspects of the transition to universal health coverage. Lancet. 2012;380:924–32. doi: 10.1016/S0140-6736(12)61083-6. [DOI] [PubMed] [Google Scholar]
- 43.Moreno-Serra R, Smith PC. Does progress towards universal health coverage improve population health? Lancet. 2012;380:917–23. doi: 10.1016/S0140-6736(12)61039-3. [DOI] [PubMed] [Google Scholar]
- 44.Giovino GA, Mirza SA, Samet JM, Gupta PC, Jarvis MJ, Bhala N, et al. GATS Collaborative Group Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet. 2012;380:668–79. doi: 10.1016/S0140-6736(12)61085-X. [DOI] [PubMed] [Google Scholar]
- 45.Bhuiyan MU, Zaman S, Ahmed T. Risk factors associated with overweight and obesity among urban school children and adolescents in Bangladesh: a case-control study. BMC Pediatr. 2013;13:72. doi: 10.1186/1471-2431-13-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Beaglehole R, Epping-Jordan J, Patel V, Chopra M, Ebrahim S, Kidd M, et al. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet. 2008;372:940–9. doi: 10.1016/S0140-6736(08)61404-X. [DOI] [PubMed] [Google Scholar]
- 47.Levitt NS. Diabetes in Africa: epidemiology, management and healthcare challenges. Heart. 2008;94:1376–82. doi: 10.1136/hrt.2008.147306. [DOI] [PubMed] [Google Scholar]
- 48.Qiu SH, Sun ZL, Cai X, Liu L, Yang B. Improving patients' adherence to physical activity in diabetes mellitus: a review. Diabetes Metab J. 2012;36:1–5. doi: 10.1136/hrt.2008.147306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]