Abstract
Researchers designed learner-directed journal clubs to develop literature evaluation skills in preclinical students. Sessions balanced student-led discussion with structured objectives and faculty support. During the pilot with preclinical MD/PhD students, self-rated mastery improved over all 17 measured objectives. Six exercises have since been incorporated into the full medical school curriculum.
Keywords: Clinical and translational research, evidence based medicine, journal clubs, student-directed learning, critical appraisal
Introduction
A clinician workforce trained in the principles of medical research is necessary both to conduct research and to apply findings in daily clinical practice. Clinicians must be involved in the design, implementation, and dissemination of research so that the questions addressed are clinically relevant and results are meaningfully reported in the literature. All clinicians, not only clinician-scientists, must be informed consumers of medical literature in order to apply advances to evidence-based patient care.1
Journal clubs are ubiquitous at all levels of medical training to help healthcare professionals become informed consumers of the literature. Ironically, only limited evidence exists to suggest that journal clubs effectively support evidence-based decision making. The literature on this topic is limited by a lack of high-level, outcomes-based reporting. Additionally, the heterogeneity journal club formats described in published studies makes their conclusions difficult to generalize.2
At the University of Cincinnati College of Medicine (UCCOM), the MD/PhD Medical Scientist Training Program (MSTP) holds a weekly one-hour journal club for its physician-scientist trainees. As of 2010 this journal club had historically poor attendance and participation. In the summer of 2010, an average of 9/32 (28%) preclinical MSTP students attended sessions which typically ended after 30–45 minutes despite being scheduled for an hour.
As the MSTP identified concerns with its journal club, a UCCOM self-study demonstrated that the medical curriculum needed improvement in clinical and translational research training. This topic was particularly important given that education on how such research “is conducted, evaluated, explained to patients, and applied to patient care” is an accreditation requirement for U.S. and Canadian medical schools.3 A journal club format was chosen to address these concerns due to the perceived parallels between preparing for journal club and the reality of self-directed literature interpretation in clinical practice. Enhancements to the MSTP journal club thus became a pilot for a journal club to be incorporated into the small group learning sessions for all preclinical students.
The authors, tasked with leading the MSTP journal club during this transformation, noted that the journal club format was somewhat automatically selected as the method to teach critical literature evaluation skills. The authors conducted both a literature search and an informal survey of MSTP students to assess the strengths and weaknesses of this learning modality. The results were surprisingly similar.
Student participants reported that the student-directed format and actual application of literature review skills in journal club was a welcome departure from lectures. However, students were concerned about the inconsistent quality of student-selected articles and an overall lack of direct relevance of the journal club to their preclinical medical training. Similarly, a Best Evidence in Medical Education review stated that the major strengths of journal clubs are the active, learner-directed components. However, unclear learning objectives often make journal clubs problematic.2 Journal clubs with more structure appear to be more effective. Characteristics of successful journal clubs include: regularly scheduled meetings, mandatory attendance, clear long- and short- term goals, and adequate time for learners to read papers before the session.4
The authors concluded from literature review and student survey that, for a journal club to be successful, it must have learning components tailored to its target audience and a clearly defined purpose. Two major objectives for this innovation were chosen: (1) tailor the MSTP journal club to the unique needs and skills of preclinical students and (2) create a generalizable, team-based learning format to give students the skills necessary to be informed consumers of the clinical and translational research literature.
Methods
The curriculum, described in Table 1, consisted of ten weekly sessions scheduled for one hour each. With support from the institutional Center for Clinical and Translational Research and Training (CCTST), the authors identified topics, learning objectives, and faculty content experts for each session. Depending upon the topic and learning objectives, additional elements beyond literature review were incorporated into the discussion, such as discussion of ethical dilemmas and how research can be presented to patients.
Table 1.
Program curriculum.
| Session topic | Learning Objectives | Session Components |
|---|---|---|
| What is clinical and translational research? |
|
|
| Study design |
|
|
| Peer review |
|
|
| Patient and recruitment bias |
|
|
| Placebos and placebo effects |
|
|
| Clinical vs. statistical significance |
|
|
| Conflict of Interest (COI) |
|
|
| Cost effectiveness |
|
|
| Literature Wars |
|
|
| Real World Validity |
|
|
Two to four students signed up to lead each session based on personal interest and availability. Session leaders were provided with learning objectives and contact information for the session’s content expert. Leaders and content experts collaboratively identified an article relevant to the topic and appropriate for preclinical students. This article was provided to participants at least five days before each session.
Student leaders were responsible for a 10–15 minute introduction intended to give preclinical attendees the background necessary to participate in group discussion. This introduction typically covered the pre-defined learning objectives, definitions of relevant terms, and clinical information relevant to the article at hand. Afterwards, student leaders, assisted by the content expert, facilitated a group discussion of each table/figure and the article’s overall relevance to clinical practice.
The pilot program was evaluated through attendance numbers and anonymous, paired pre- and post- intervention surveys as well as solicited participant feedback. Survey questions included both close-ended, five-point Likert scale items and open-ended reflections on the educational program. Seventeen closed-ended questions evaluated students’ achievement of learning objectives, while eight closed-ended questions evaluated the journal club’s overall efficacy before and after intervention. While this activity was optional, fourteen MSTP students received a credit hour by attending at least 8/10 sessions and leading one.
Representative Session
The “Literature Wars” session aimed to develop students’ skills in clinical decision-making in the face of conflicting research evidence. Students critically compared two conflicting articles describing different randomized controlled trials of tissue plasminogen activator (t-PA) for the treatment of acute ischemic stroke.
The student-led introduction provided an overview of t-PA use in stroke. The group discussion then focused on a side-by-side comparison of figures and methodological differences in each article to understand the differing conclusions. Students next discussed their own clinical conclusions on the effectiveness of t-PA and how they would present these conclusions to a patient. Students then explored if they would follow this recommendation for themselves or a loved one in the same clinical situation, and the ethical implications of the disparity in patient vs. personal recommendation identified by several students.
Results
These sessions consistently exceeded the scheduled hour and were attended by 26/32 (81%) of preclinical MSTP students, a significant improvement from the previous year. Additionally, four preclinical medical students conducting summer research heard about the journal club through the CCTST and participated. An average of 17 preclinical students attended each session.
The pre-intervention survey was open to MSTP students who participated in the first or second session, and had a response rate of 76% (14/19). The post-intervention survey was open to all participating MSTP students and had a response rate of 62% (16/26). We received paired pre-and post-intervention surveys for 61% (11/18) of MSTP students who attended at least half of the sessions.
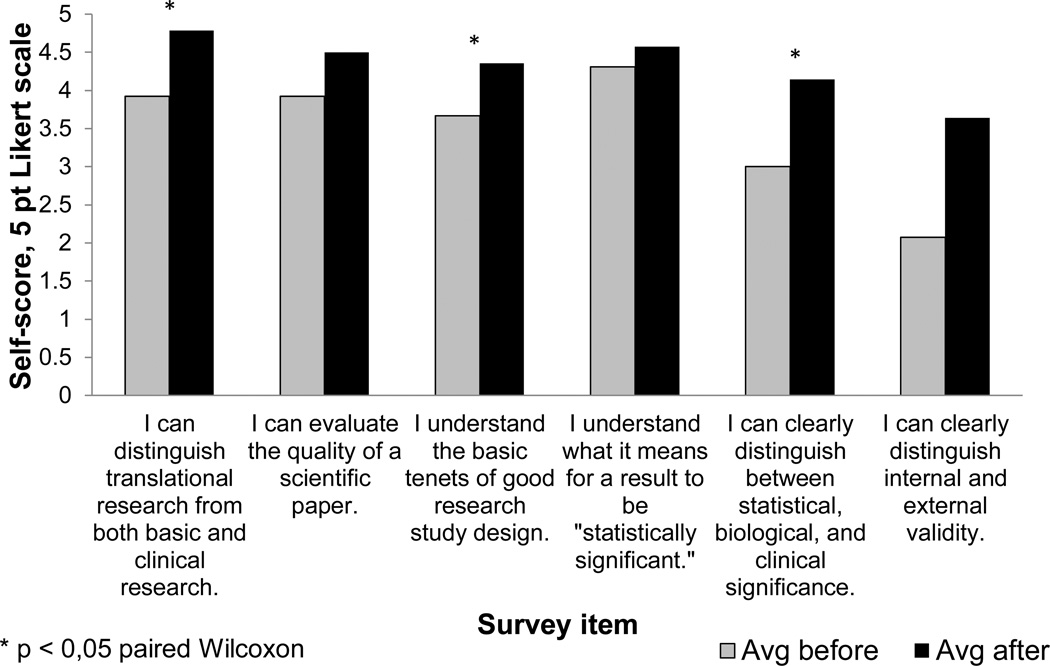
Students’ self-reported achievement of learning objectives improved for all 17 objectives assessed, shown in Figure 1. Space limitations prevent showing all results. To reduce bias, these six representative objectives were chosen before the authors viewed the results.
Figure 1.
Self-Reported Achievement of Learning Objectives. Self-rated knowledge scores for six representative learning objectives (n=16 students who attended at least 5/10 sessions.). Students showed significant improvement in three learning objectives by the paired Wilcoxon Rank Sum test (n = 11 students completing both pre- and post-surveys).
Students gave ratings of 4 or 5 (of 5) for all 11 questions regarding the educational utility of the new format. Student comments suggested an appreciation of the structure provided to this student-directed activity. Representative comments include:
“There was a theme for each journal club session. As a student, this gave me a more concrete goal to what I should be learning.”
“There was a clear topic each week & I liked the structure that provided, rather than let's-just-discuss-this-paper-&-see-what-we-come-up-with.”
“Being honest, a lot of people (including myself) pick papers that feature science that isn't solid or are otherwise lacking…(because we don't have time or whatever) and that makes the journal clubs not as useful as they could be. Having good exemplar papers was definitely helpful.”
To our knowledge, during this summer activity students were not participating in additional journal clubs or other organized academic activities which might otherwise explain this improvement.
Discussion
This innovation sought to take a deliberate approach to the ubiquitous tool of journal club by tailoring it to the specific needs of preclinical medical students. Defined learning objectives and a mix of structured and learner-directed components contributed to the innovation’s success. The most encouraging indicator of this innovation’s success was the sustained, enthusiastic student participation in this optional pilot program. The voluntary participation of 30 preclinical students and the high feedback scores suggest achievement of our first objective to tailor the journal club to these students.
The second objective to design a generalizable team-based learning format for clinical and translational research education was fully achieved. After the pilot’s success, UCCOM partnered with student coordinators to develop six sessions for the medical school which were implemented in 2012–2013.
A limitation of this innovation, inherent in its pilot sample size, is the ability to evaluate its impact beyond student self-report. This problem is common to published reports on journal clubs.2,4 It is possible that results are positively biased due to the self-selection of participants in this pilot program or students’ skewed perception of personal progress. These potential biases suggest that the survey results should be taken as broad indicators of this format’s usefulness in the preclinical setting rather than unqualified proof of its success.
As this program is scaled up to the full preclinical curriculum, evaluation will include direct assessment of students’ knowledge. Because preclinical students attending a required medical school activity have different needs than students self-selecting for interest in research, the exercises developed for the medical school have an even greater emphasis on patient care and explaining results to patients. One exercise in development, recently piloted, involves having students discuss popular media reports on medical research with non-medical friends and family before locating the original research and discussing it in journal club. Exercises involving student explanation of research to patients are also being developed, which will allow for external assessment of student attitudes and changes in practice.
Institutions considering similar educational programs may wish to pay attention to the careful balance between providing structure and context for preclinical learners while still allowing students to direct their own learning. Pre-defined learning objectives, a semi-structured format, suggestions of quality papers, and faculty support give students the tools to lead a successful small group. Such structured student-led groups allow students to learn and present new concepts, strengthen faculty and student connections, and develop student confidence in self-directed learning and presentation skills.5
This innovation is now an official part of the UCCOM physician-scientist training curriculum, with outgoing coordinators advising incoming coordinators to ensure sustainability. The authors look forward to further piloting innovations in clinical and translational research education for general preclinical training.
Acknowledgements
The authors wish to thank Dr. Patrick Tso and Dr. Gurjit Hershey for their leadership of the Medical Scientist Training Program during this work, Ms. Bettie Durant for administrative support, Mr. Paul Catalanotto and Ms. Sarah Currier for their thoughtful review of this manuscript, Dr. Joseph Kiesler for collaboration in adapting this program to the preclinical medical curriculum, and Dr. Anne Gunderson for assistance with protection of human subjects and survey design. The authors wish to especially thank mentors Dr. Ardythe Morrow and Dr. Melissa DelBello for encouraging student involvement in both scientific and medical education research.
Funding Disclosures
This work was supported by the Medical Scientist Training Program of the University of Cincinnati (NIH T32 GM063483-10), Center for Clinical and Translational Science and Training (8UL1TR000077-04), and the Short Term Medical Student Training Grant (T35DK60444). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Student stipends during this project were supported by “The Role of Human Milk” (NIH P01 HD013021-31), “Multimodal Neuroimaging of Treatment Effects in Adolescent Mania” (NIH R01 MH080973), and “Molecular Epidemiology in Children’s Environmental Health Training Program” (2T32ES010957-11).
Biographies
REBECCA L. CURRIER is an MD/PhD student in the Medical Scientist Training Program, University of Cincinnati College of Medicine, Cincinnati, Ohio, USA and Division of Epidemiology and Biostatistics, Department of Environmental Health, Cincinnati, OH, USA.
MARGUERITE REID SCHNEIDER is an MD/PhD student in the Medical Scientist Training Program, University of Cincinnati College of Medicine, Cincinnati, Ohio, USA and Neuroscience Graduate Program, University of Cincinnati College of Medicine, Cincinnati, OH, USA.
JAMES E. HEUBI, MD, is co-Director of the Center for Clinical and Translational Science and Training, a collaborative effort of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA.
Footnotes
Ethical Approval
The Institutional Review Board (IRB) of the University of Cincinnati has ruled that surveys of medical students regarding medical education curricula, under supervision of the Assistant Dean for Academic Support, is a quality improvement process and therefore exempt from IRB review (Dr. Anne Gunderson, Principal Investigator).
References
- 1.Westfall JM, Mold J, Fagnan L. Practice-based research--"Blue Highways" on the NIH roadmap. JAMA. 2007;297(4):403–406. doi: 10.1001/jama.297.4.403. [DOI] [PubMed] [Google Scholar]
- 2.Harris J, Kearley K, Heneghan C, Meats E, Roberts N, Perera R, et al. Are journal clubs effective in supporting evidence-based decision making? A systematic review. Best Evidence in Medical Education Guide No. 16. Med Teach. 2011;33(1):9–23. doi: 10.3109/0142159X.2011.530321. [DOI] [PubMed] [Google Scholar]
- 3.Liaison Committee on Medical Education (LCME) Functions and Structure of a Medical School: Standards for Accreditation of Medical Education Programs Leading to the M.D. Degree. [Accessed November 15, 2013];2013 Jun; http://www.lcme.org/publications/functions2013june.pdf. [Google Scholar]
- 4.Deenadayalan Y, Grimmer-Somers K, Prior M, Kumar S. How to run an effective journal club: a systematic review. J Eval Clin Pract. 2008;14(5):898–911. doi: 10.1111/j.1365-2753.2008.01050.x. [DOI] [PubMed] [Google Scholar]
- 5.Anderson GL, Passmore JC, Wead W, Falcone JC, Stremel RW, Schuschke DA. Using “Active Learning” Methods to Teach Physiology. Med Sci Ed. 2011;21(1):8–20. [Google Scholar]