Abstract
Background
Although diabetes is a well-known risk factor for death, its impact on cancer death is not clearly understood. Furthermore, it remains controversial whether impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT) are associated with increased risk of mortality. We investigated the impact of diabetes or glucose tolerance categories on all cause and cause-specific mortality.
Methods
Mortality analysis was conducted in three population-based cohort studies of 3,801 participants, divided according to fasting plasma glucose (FPG) (normal; stage 1 IFG [5.6≤FPG<6.1 mmol/L]; stage 2 IFG [6.1≤FPG<7.0 mmol/L]; diabetes mellitus [DM]-FPG); or 2-hour glucose after 75 g glucose loading (2hPG) (normal; IGT; DM-2hPG), or a combination of FPG and 2hPG criteria.
Results
During a median follow-up of 11.0 years, 474 subjects died from all causes. Hazard ratios (HRs) for all cause death were higher in those with diabetes as defined by either FPG or 2hPG criteria than their normal counterparts (HR, 2.2, 95% confidence interval [CI], 1.6 to 2.9 for DM-FPG; HR, 2.0, 95% CI, 1.5 to 2.7 for DM-2hPG). Similarly, diabetes defined by either FPG or 2hPG was associated with cancer death (HR, 2.9, 95% CI, 1.7 to 5.0; and HR, 2.1, 95% CI, 1.2 to 3.9, respectively). Although neither IFG nor IGT conferred higher risk for death, when combining stage 2 IFG and/or IGT, the risk of all cause death was higher than in subjects with normal glucose regulation (HR, 1.3; 95% CI, 1.0 to 1.6).
Conclusion
Diabetes is associated with higher risk of death from all causes and cancer. In subjects without diabetes, stage 2 IFG and/or IGT confers increased risk for mortality.
Keywords: Diabetes mellitus, Glucose intolerance, Mortality
INTRODUCTION
There has been rapid growth in the prevalence of diabetes in recent years, especially in Asia. Indeed, the prevalence of diabetes in Korea increased from 1.5% to 9.9% over the past 40 years [1]. Diabetes-related mortality data was not included among major leading causes of death in 1983 in South Korea, but in 2011, they ranked as the fourth leading cause of natural death, following malignancy, cerebrovascular disease, and cardiovascular disease (CVD) [2]. There is increasing concern about the role of diabetes as a risk factor for certain types of cancers, such as pancreas, liver, and colon/rectum [3], and for cancer mortality in some population studies [4,5]. However, diabetes was not associated with increased risk of death from cancer in a male population in the United Kingdom [6] or in the Second National Health and Nutrition Examination Survey (NHANES II) in the United States [7].
Impaired glucose regulation can be indicated by either impaired fasting glucose (IFG) by the American Diabetes Association (ADA) criteria [8] or impaired glucose tolerance (IGT) by World Health Organization criteria [9]. Some epidemiologic studies support the importance of one or the other in predicting mortality [10], and a few indicate that neither IFG nor IGT confer increased risk for mortality [11,12]. Studies evaluating whether cancer mortality is associated with IFG or IGT are limited and highly controversial [6,7,13-15]. In addition, although ADA lowered the cutoff point for normal fasting glucose (NFG) from 6.1 to 5.6 mmol/L [16], the prognostic implications of this lower cutoff point are still controversial [17,18].
Although the epidemic of diabetes in Korea is steadily increasing, no longitudinal data exist on the association between glucose tolerance categories and mortality in South Korean population. As an extension of a pooled analysis of four community-based cohort studies in Korea, which had examined fasting and 2-hour glucose after glucose loading [19], this study determined the association between glucose tolerance status and all cause and cause specific mortality.
METHODS
Participants
Among several population-based cohort studies in Korea, the Yonchon [20], Chongup [21], and Ansan [22] studies were selected because each of these studies: 1) was conducted after 1990, 2) included both men and women 30 years or older, 3) used the standard 2-hour 75 g oral glucose tolerance test (OGTT), and 4) included participants with a residence identification number. The Yonchon study was held in 1993 in Yonchon county, a rural area in northern South Korea. The Chongup study was conducted in 1997 in rural southern South Korea, and the Ansan study was conducted in 2000 in an urban area near Seoul, South Korea. All subjects participated in the study voluntarily, and informed consent was obtained from all participants. The appropriate ethics committees approved the protocols of each study. Of 5,139 subjects (Yonchon, n=2,304; Chongup, n=1,105; Ansan, n=1,730), we selected 3,801 subjects whose status of diabetes could be identified by fasting plasma glucose (FPG) and 2-hour glucose after 75 g glucose loading (2hPG) concentrations and previous history of medication for diabetes.
Study procedure
Standard anthropometric data and lifestyle factors were collected in all participants. Height and weight measurements were taken while the subjects were barefoot and dressed in light clothing. Blood pressure was measured after subjects had rested for at least 10 minutes. Every subject who had not been diagnosed previously with diabetes was asked to complete a 75 g OGTT. Blood samples were centrifuged on site. Plasma glucose concentration was measured using the glucose oxidase method. Total cholesterol, triglycerides, and high density lipoprotein cholesterol concentrations were measured by enzymatic methods. Each subject's vital status and causes of death as of 31 December 2007 were determined after linking these cohort data with death certificate data from Korean National Statistical Office. ICD-10 codes were used to classify the underlying cause of death as due to cancer (ICD-10 codes C00-C97), CVD (ICD-10 codes I00-I79), and others.
Glucose tolerance categories
Mortality for various glucose tolerance categories was computed separately based on FPG or 2hPG. FPG ≥7.0 mmol/L or taking diabetes medication was classified as diabetes by FPG criteria (diabetes mellitus [DM]-FPG). Similarly, 2hPG ≥11.1 mmol/L or taking diabetes medication was defined as diabetes by 2hPG criteria (DM-2hPG). A Korean study recently reported that subjects with stage 2 IFG (6.1≤FPG<7.0 mmol/L) showed different clinical characteristics compared to stage 1 IFG (5.6≤FPG<6.1 mmol/L) [19]. Therefore, as of 2011 the clinical practice guidelines for type 2 diabetes in Korea recommended different screening methods according to stage of IFG [23]. We divided our IFG participants into two groups according to aforementioned criteria with or without IGT. Similarly, by only 2hPG criteria, normal glucose tolerance (NGT: 2hPG <7.8 mmol/L) or IGT (7.8≤2hPG<11.1 mmol/L) with or without IFG was defined by the 2003 ADA criteria [16]. We also analyzed the mortality according to the combination of FPG and 2hPG criteria (normal glucose regulation I [NGR I]: FPG <5.6 mmol/L [normal fasting glucose, NFG] and 2hPG <7.8 mmol/L; prediabetes: IFG and/or IGT; and diabetes: FPG or 2hPG criteria). In order to compare the prognostic implications of different FPG cutoff points, subjects were also categorized by the higher cutoff point for FPG (6.1 mmol/L) as NGR II (FPG <6.1 mmol/L and 2hPG <7.8 mmol/L), prediabetes (stage 2 IFG and/or IGT), and diabetes.
Statistical analysis
Baseline characteristics were compared among the three study population studies using analysis of variance for numeric variables and a chi-square test for categorical variables. Nonnormally distributed variables such as triglycerides were presented as the median and interquartile range for each group, and differences were tested after logarithmic transformation. For mortality analysis, the period at risk extended from the date of research examination to death or the end of 2007, whichever came first. Cause specific hazard ratios (HRs) for death are presented for cancer and CVD, as these were the leading causes of death. Other causes are not presented because of the few numbers of deaths due to these causes.
The effects of the variables of interest on all cause and cause specific mortality were assessed according to the various glucose categories in the proportional hazards models. Baseline age, sex, study center, smoking status, systolic blood pressure, dyslipidemia, and body mass index were included in the proportional hazards analysis because of their potential confounding effects on the outcome. Product terms of predictor variables did not significantly improve the regression models and were not included. The assumptions of proportionality were tested using log follow-up time interaction terms for each baseline variable. Analyses were performed with SAS software version 9.1 (SAS Institute, Cary, NC, USA).
RESULTS
Baseline characteristics of the study participants are presented in Table 1. Subjects in Chongup were the oldest, and those in Ansan were the youngest. Those in Chongup had the least favorable metabolic profile among the three cohorts. During a median follow-up of 11.0 years (range, 0.2 to 15.0 years), 474 deaths from all causes occurred among the 3,801 subjects (1,583 men, 2,218 women), of which 111 were attributed to cancer and 106 to CVD. When comparing the subjects with NGR, IFG and/or IGT, and diabetes, the anthropometric and metabolic variables were the worst in those with diabetes, intermediate in IFG and/or IGT compared to NGR (Table 2).
Table 1.
Baseline characteristics of the study population
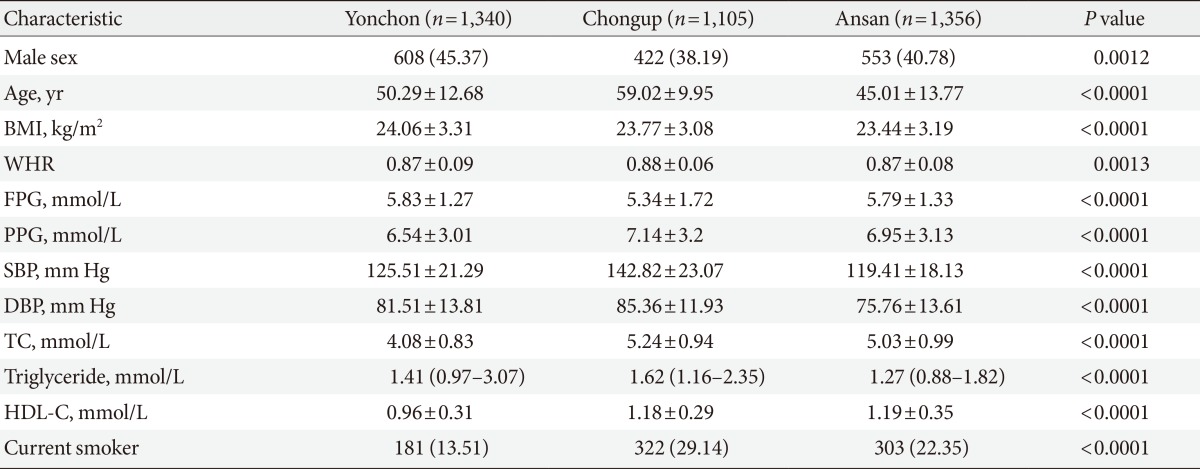
Values are presented as number (%), mean±standard deviation, or median (1st quartile.3rd quartile).
BMI, body mass index; WHR, waist-hip ratio; FPG, fasting plasma glucose; PPG, 2-hour glucose after 75 g glucose loading; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; HDL-C, high density lipoprotein cholesterol.
Table 2.
Characteristics of the subjects according to the glucose tolerance categories
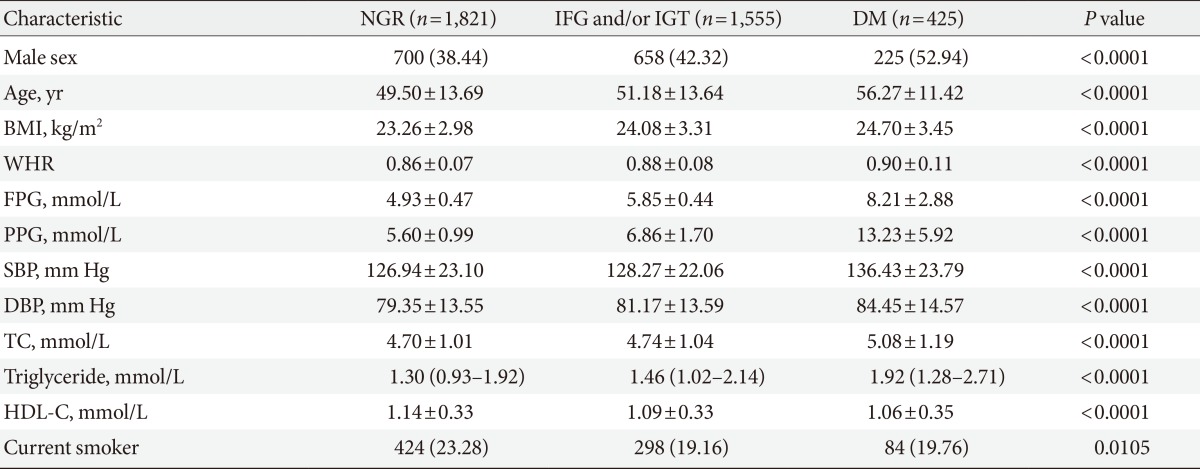
Values are presented as number (%), mean±standard deviation, or median (1st quartile-3rd quartile).
NGR, normal glucose regulation; IFG, impaired fasting glucose; IGT, impaired glucose tolerance; DM, diabetes mellitus; BMI, body mass index; WHR, waist-hip ratio; FPG, fasting plasma glucose; PPG, 2-hour glucose after 75 g glucose loading; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; HDL-C, high density lipoprotein cholesterol.
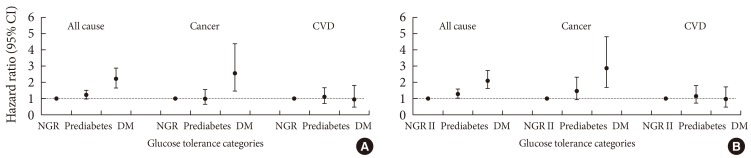
The multivariate-adjusted HR for death from all causes was about 2-fold higher in subjects with diabetes defined by either FPG or 2hPG criteria than in their normal counterparts, whereas it did not increase in the IFG or IGT groups compared to those with NGR I (Table 3). When prediabetes was defined as IFG and/or IGT, the HR for all-cause death was not higher than those with NGR I (HR, 1.23; 95% CI, 1.00 to 1.52) (Fig. 1). However, when stage 2 IFG and/or IGT was used to define prediabetes, all-cause death was higher in subjects with prediabetes than NGR II (HR, 1.27; 95% CI, 1.02 to 1.59) (Fig. 1).
Table 3.
Hazard ratios and 95% confidence interval of death from all causes, cancer, and cardiovascular disease according to fasting plasma glucose or 2-hour glucose after 75 g glucose loading concentrations and presence/absence of diabetes
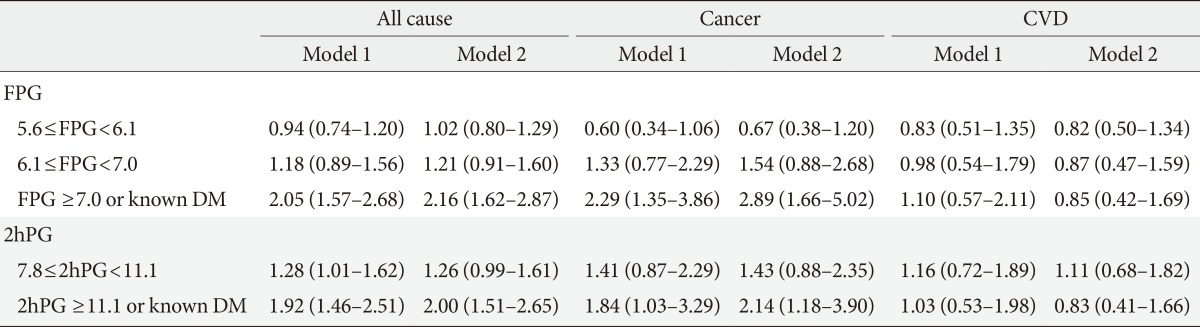
Values are presented as hazard ratios (95% confidence interval). Reference group: FPG <5.6 mmol/L, 2hPG <7.8 mmol/L. Model 1, adjusted for age, sex, and study center. Model 2, adjusted for age, sex, study center, body mass index, systolic blood pressure, total cholesterol, high density lipoprotein cholesterol, and smoking status.
CVD, cardiovascular disease; FPG, fasting plasma glucose; 2hPG, 2-hour glucose after 75 g glucose loading; DM, diabetes mellitus.
Fig. 1.
Hazard ratios and 95% confidence interval (CI) of death from all causes, cancer, and cardiovascular disease (CVD) according to glucose categories by fasting plasma glucose and 2-hour glucose after 75 g glucose loading criteria. Prediabetes was defined as (A) impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT), or (B) stage 2 IFG and/or IGT. NRG, normal glucose regulation; DM, diabetes mellitus.
The HR for cancer death was 2.89 (95% CI, 1.66 to 5.02) and 2.14 (95% CI, 1.18 to 3.90) for subjects with diabetes defined by FPG or 2hPG criteria, respectively, after adjusting for several confounding variables (Table 3). Subjects with stage 2 IFG or IGT had an elevated HR for cancer death, but this finding was not statistically significant (Table 3). Even in subjects with stage 2 IFG and/or IGT, the HR for cancer death was not statistically significant (HR, 1.47; 95% CI, 0.93 to 2.33) (Fig. 1). Neither diabetes nor prediabetes was associated with CVD death.
DISCUSSION
Compared to Western countries, the proportion of people with diabetes has dramatically increased throughout Asia. People in Asia tend to develop diabetes with a lesser degree of obesity at a younger age, suffer more from complications of diabetes, and die sooner than people in other regions [24]. This is the first Korean population-based study to show that diabetes, as determined using an OGTT, is associated with increased all cause and cancer mortality.
Diabetes is a well-known risk factor for all-cause mortality. An increasing number of epidemiologic studies have found that diabetes may alter the risk of developing a variety of cancers [3] and that diabetes is associated with death from cancer [5,6]. In agreement with previous publications, this study found that the HR for cancer death was more than 2-fold higher in subjects with diabetes defined by FPG or 2hPG after adjusting for other risk factors such as obesity, which is a confounding factor of cancer mortality. This risk is even higher than the risk reported by the Korean Cancer Prevention Study (KCPS) [4]. The KCPS reported HRs for cancer death of 1.29 (95% CI, 1.22 to 1.37) in men and 1.23 (95% CI, 1.09 to 1.39) in women with an FPG ≥7.8 mmol/L, compared to subjects with an FPG <5 mmol/L. However, the KCPS did not show the impact of postload hyperglycemia on cancer death. The exact mechanism of increased risk for cancer death in individuals with diabetes is not clear. Insulin resistance and compensatory hyperinsulinemia has been known to promote carcinogenesis, since insulin is an important growth factor for cancer cells [25]. In recent epidemiologic studies, insulin-like growth factor 1 (IGF-1) has been associated with increased risk of colorectal cancer [26], and higher blood IGF-1 levels were observed in prostate and breast cancer [27]. Direct effects of hyperglycemia via increased oxidative stress and accumulating advanced glycation end-products may play a role in the development of cancer [28]. Diabetes may also affect the treatment of cancer, as some types of cancer are treated less aggressively in patients with diabetes than in patients without diabetes [29]. Furthermore, certain glucose-lowering medications may modify the risk and prognosis of cancer [30].
There have been inconsistencies in the prognostic implication of fasting and postload hyperglycemia. Subjects with IFG had a greater impairment in early phase insulin secretion and increased endogenous glucose output, whereas IGT was associated with peripheral insulin resistance. In the Diabetes Epidemiology: Collaborative Analysis of Diagnostic Criteria in Europe (DECODE) study, 2hPG was a stronger risk factor for death than FPG [10]; however, two other studies showed that neither IFG nor IGT increased the risk for all-cause mortality [11,12]. The present study also suggested that hyperglycemia according to FPG or 2hPG criteria had a similar risk of death not only in subjects with diabetic glucose ranges, but also in those with nondiabetic glucose ranges. However, the prognostic implication of lowering the IFG cutoff point from 6.1 to 5.6 mmol/L, as proposed in 2003 by the ADA, remains controversial [17,18]. Recently, Kim et al. [18] showed that stage 2 IFG was associated with future risk of CVD after adjusting for cardiovascular risk factors, whereas stage 1 IFG was not. In accordance with their study, the present finding that subjects with prediabetes, defined as stage 2 IFG and/or IGT, had a higher risk for all cause death suggests that stage 1 and 2 IFG have different prognoses. This difference may be attributed to the higher metabolic risk in subjects with stage 2 IFG than in subjects with NFG, as shown in a baseline study of this population [19].
The present study also demonstrated that cancer death did not significantly increase in subjects with stage 2 IFG (HR, 1.54; 95% CI, 0.88 to 2.68) or IGT (HR, 1.43; 95% CI, 0.88 to 2.35) when compared to subjects with NGR II. The association of cancer mortality and IFG and/or IGT is not yet clear. In the NHANES II, IGT was a strong risk factor for cancer mortality (HR, 1.87; 95% CI, 1.06 to 3.31), and in a pooled analysis of three longitudinal studies in Mauritius, Fiji, and Nauru, the HR for cancer death was 8.0 in men with isolated postload hyperglycemia compared to those with NGR (95% CI, 3.6 to 17.9) [13]. However, two other studies showed that IGT was not associated with increased cancer death, whereas diabetes was [6,14]. In the DECODE study [15], which included 44,655 subjects from a number of European population-based studies, the HR for cancer mortality was 1.13 (95% CI, 1.00 to 1.28) in men and 1.11 (95% CI, 0.94 to 1.3) in women with IFG and/or IGT, compared to those with NGR. Although there are some inconsistencies, these studies demonstrate the importance of both FPG and 2hPG in predicting fatal cancer even in subjects without diabetes.
Diabetes is a well-known risk factor for CVD; however, we could not find any relation between death from CVD and diabetes by either FPG or 2hPG criteria. Only subjects with a long duration of diabetes had a high risk of CVD death in a study involving Pima Indians [12]. Thus, the fact that there was no association between diabetes and CVD death in the present study could be attributed to the short duration of diabetes in the study participants. Other explanations include a limited number of CVD deaths and potential inaccuracies in the causes of death as reported on the death certificate. Compared to deaths from CVD, cancer mortality can be proven more accurately due to the National Cancer Registration Program. Another limitation of this study is the heterogeneity of the three cohort studies used in this pooled analysis. Different ages and lifestyles, which are often found in different residential areas, may be important confounding factors. However, this study adjusted for age, study center, and other risk factors associated with mortality in the regression model to minimize the heterogeneity issue. Nevertheless, this is the first population-based Korean study to evaluate mortality risk according to discrete glucose tolerance categories as defined by a glucose tolerance test.
In conclusion, diabetes is a significant risk factor for both all cause and cancer mortality, independent of obesity. In those with stage 2 IFG and/or IGT, the rates of all-cause mortality increase relative to NGR II.
ACKNOWLEDGMENTS
This project was supported by a grant from the Korean Diabetes Association (P.Y., 2008). The funding sources had no role in the collection of the data or in the decision to submit the manuscript for publication. The authors wish to thank the members of the Committee on the Epidemiology of Diabetes Mellitus, Korean Diabetes Association.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011;35:303–308. doi: 10.4093/dmj.2011.35.4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Statistics Korea: Causes of death statistics in 2011. [updated 2012 Sep 13]. Available from: http://www.index.go.kr.
- 3.Johnson JA, Carstensen B, Witte D, Bowker SL, Lipscombe L, Renehan AG Diabetes and Cancer Research Consortium. Diabetes and cancer (1): evaluating the temporal relationship between type 2 diabetes and cancer incidence. Diabetologia. 2012;55:1607–1618. doi: 10.1007/s00125-012-2525-1. [DOI] [PubMed] [Google Scholar]
- 4.Jee SH, Ohrr H, Sull JW, Yun JE, Ji M, Samet JM. Fasting serum glucose level and cancer risk in Korean men and women. JAMA. 2005;293:194–202. doi: 10.1001/jama.293.2.194. [DOI] [PubMed] [Google Scholar]
- 5.Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ. Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol. 2004;159:1160–1167. doi: 10.1093/aje/kwh161. [DOI] [PubMed] [Google Scholar]
- 6.Batty GD, Shipley MJ, Marmot M, Smith GD. Diabetes status and post-load plasma glucose concentration in relation to site-specific cancer mortality: findings from the original Whitehall study. Cancer Causes Control. 2004;15:873–881. doi: 10.1007/s10552-004-1050-z. [DOI] [PubMed] [Google Scholar]
- 7.Saydah SH, Loria CM, Eberhardt MS, Brancati FL. Abnormal glucose tolerance and the risk of cancer death in the United States. Am J Epidemiol. 2003;157:1092–1100. doi: 10.1093/aje/kwg100. [DOI] [PubMed] [Google Scholar]
- 8.Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 1997;20:1183–1197. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 9.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 10.The DECODE study group, Diabetes Epidemiology: Collaborative analysis Of Diagnostic criteria in Europe; European Diabetes Epidemiology Group. Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria. Lancet. 1999;354:617–621. [PubMed] [Google Scholar]
- 11.Pankow JS, Kwan DK, Duncan BB, Schmidt MI, Couper DJ, Golden S, Ballantyne CM. Cardiometabolic risk in impaired fasting glucose and impaired glucose tolerance: the Atherosclerosis Risk in Communities Study. Diabetes Care. 2007;30:325–331. doi: 10.2337/dc06-1457. [DOI] [PubMed] [Google Scholar]
- 12.Kim NH, Pavkov ME, Looker HC, Nelson RG, Bennett PH, Hanson RL, Curtis JM, Sievers ML, Knowler WC. Plasma glucose regulation and mortality in pima Indians. Diabetes Care. 2008;31:488–492. doi: 10.2337/dc07-1850. [DOI] [PubMed] [Google Scholar]
- 13.Harding JL, Soderberg S, Shaw JE, Zimmet PZ, Pauvaday V, Kowlessur S, Tuomilehto J, Alberti KG, Magliano DJ. All-cause cancer mortality over 15 years in multi-ethnic Mauritius: the impact of diabetes and intermediate forms of glucose tolerance. Int J Cancer. 2012;131:2385–2393. doi: 10.1002/ijc.27503. [DOI] [PubMed] [Google Scholar]
- 14.Stengard JH, Tuomilehto J, Pekkanen J, Kivinen P, Kaarsalo E, Nissinen A, Karvonen MJ. Diabetes mellitus, impaired glucose tolerance and mortality among elderly men: the Finnish cohorts of the Seven Countries Study. Diabetologia. 1992;35:760–765. doi: 10.1007/BF00429097. [DOI] [PubMed] [Google Scholar]
- 15.Zhou XH, Qiao Q, Zethelius B, Pyorala K, Soderberg S, Pajak A, Stehouwer CD, Heine RJ, Jousilahti P, Ruotolo G, Nilsson PM, Calori G, Tuomilehto J DECODE Study Group. Diabetes, prediabetes and cancer mortality. Diabetologia. 2010;53:1867–1876. doi: 10.1007/s00125-010-1796-7. [DOI] [PubMed] [Google Scholar]
- 16.Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, Kitzmiller J, Knowler WC, Lebovitz H, Lernmark A, Nathan D, Palmer J, Rizza R, Saudek C, Shaw J, Steffes M, Stern M, Tuomilehto J, Zimmet P Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26:3160–3167. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 17.Kanaya AM, Herrington D, Vittinghoff E, Lin F, Bittner V, Cauley JA, Hulley S, Barrett-Connor E. Impaired fasting glucose and cardiovascular outcomes in postmenopausal women with coronary artery disease. Ann Intern Med. 2005;142:813–820. doi: 10.7326/0003-4819-142-10-200505170-00006. [DOI] [PubMed] [Google Scholar]
- 18.Kim HK, Kim CH, Kim EH, Bae SJ, Choe J, Park JY, Park SW, Yun YD, Baek SJ, Mok Y, Jee SH. Impaired fasting glucose and risk of cardiovascular disease in Korean men and women: the Korean Heart Study. Diabetes Care. 2013;36:328–335. doi: 10.2337/dc12-0587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oh JY, Lim S, Kim DJ, Kim NH, Kim DJ, Moon SD, Jang HC, Cho YM, Song KH, Ahn CW, Sung YA, Park JY, Shin C, Lee HK, Park KS Committee of the Korean Diabetes Association on the Diagnosis and Classification of Diabetes Mellitus. A report on the diagnosis of intermediate hyperglycemia in Korea: a pooled analysis of four community-based cohort studies. Diabetes Res Clin Pract. 2008;80:463–468. doi: 10.1016/j.diabres.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 20.Park Y, Lee H, Koh CS, Min H, Yoo K, Kim Y, Shin Y. Prevalence of diabetes and IGT in Yonchon County, South Korea. Diabetes Care. 1995;18:545–548. doi: 10.2337/diacare.18.4.545. [DOI] [PubMed] [Google Scholar]
- 21.Park JY, Kim YI, Choi CS, Chung YE, Kim SW, Lee MS, Lee SI, Hong SK, Lee KU. Prevalence of diabetes, impaired glucose tolerance, and impaired fasting glucose in a rural population of Korea, according to 1997 American Diabetes Association and 1985 World Health Organization criteria. Diabetes Care. 2000;23:707–708. doi: 10.2337/diacare.23.5.707. [DOI] [PubMed] [Google Scholar]
- 22.Jo I, Ahn Y, Lee J, Shin KR, Lee HK, Shin C. Prevalence, awareness, treatment, control and risk factors of hypertension in Korea: the Ansan study. J Hypertens. 2001;19:1523–1532. doi: 10.1097/00004872-200109000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Ko SH, Kim SR, Kim DJ, Oh SJ, Lee HJ, Shim KH, Woo MH, Kim JY, Kim NH, Kim JT, Kim CH, Kim HJ, Jeong IK, Hong EK, Cho JH, Mok JO, Yoon KH Committee of Clinical Practice Guidelines, Korean Diabetes Association. 2011 Clinical practice guidelines for type 2 diabetes in Korea. Diabetes Metab J. 2011;35:431–436. doi: 10.4093/dmj.2011.35.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–1688. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 25.Pollak M. Insulin and insulin-like growth factor signalling in neoplasia. Nat Rev Cancer. 2008;8:915–928. doi: 10.1038/nrc2536. [DOI] [PubMed] [Google Scholar]
- 26.Ma J, Pollak MN, Giovannucci E, Chan JM, Tao Y, Hennekens CH, Stampfer MJ. Prospective study of colorectal cancer risk in men and plasma levels of insulin-like growth factor (IGF)-I and IGF-binding protein-3. J Natl Cancer Inst. 1999;91:620–625. doi: 10.1093/jnci/91.7.620. [DOI] [PubMed] [Google Scholar]
- 27.Bohlke K, Cramer DW, Trichopoulos D, Mantzoros CS. Insulin-like growth factor-I in relation to premenopausal ductal carcinoma in situ of the breast. Epidemiology. 1998;9:570–573. [PubMed] [Google Scholar]
- 28.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 29.van de Poll-Franse LV, Houterman S, Janssen-Heijnen ML, Dercksen MW, Coebergh JW, Haak HR. Less aggressive treatment and worse overall survival in cancer patients with diabetes: a large population based analysis. Int J Cancer. 2007;120:1986–1992. doi: 10.1002/ijc.22532. [DOI] [PubMed] [Google Scholar]
- 30.Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, Pollak M, Regensteiner JG, Yee D. Diabetes and cancer: a consensus report. Diabetes Care. 2010;33:1674–1685. doi: 10.2337/dc10-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]