With ever increasing number of pre and peri-operative patients presenting for surgery with co-morbid endocrine disorders, the challenges for the anesthesiologists have grown manifold. Apart from caring for the impact of surgical pathology on endocrine functions, anesthesiologist also confronts endocrine disorders and manages their possible implications during anesthesia procedures.[1,2]
DIFFERENT YET SOME COMMON BASE
Though on the surface, there does not seem to be any similarity between endocrinology and anesthesiology specialties if one explores them in chthonic depth, a lot of common ground can be observed. Endocrine anesthesia (EA), an amalgam of these two medical sciences, is fast becoming a distinct specialty on its own and the present editorial aims to focus on these.
ENDOCRINOLOGICAL CHALLENGES IN ANESTHESIOLOGY
Anesthesia for endocrine surgery is different from that for routine procedures. Peri-operative neurotransmitter and hormonal secretion occurring with a deranged endocrinal milieu in the background can be highly variable and unpredictable. This may have a direct impact on the morbidity and mortality. In both non-endocrine and endocrine surgery, the role of pituitary, thyroid, parathyroid, pancreas, adrenal, and various other hormone releasing tissues and organs can have a direct impact on the surgical outcome.[3,4,5,6,7] Endocrine complications are more likely to occur in routine daily anesthesia practice in patients presenting with endocrinopathy, but may occur in all. It is therefore mandatory that an anesthesiologist should be thoroughly well-versed with all endocrine pathologies and complications, which can be encountered during surgical practice so as to “suspect,” “prevent,” “diagnose,” and “manage” them in a timely and appropriate manner. Hypoglycemia, hyperglycemia, hypocalcemia, hyperkalemia, hypokalemia, and many more electrolyte and metabolic abnormalities are commonly encountered in surgical patients and optimal management of these complications can greatly help in achieving a better surgical outcome.[8,9]
ANESTHETIC TECHNIQUE: A DIFFICULT CHOICE
The choice of anesthesia is also determined by pathophysiological alterations due to different endocrinopathies related to pancreas, thyroid, parathyroid, adrenal, pituitary, and others.[3,4,5,6,7] Autonomic function and integrity is of utmost importance while formulating the plan of anesthesia. As autonomic dysfunction is commonly encountered in many of the endocrine disorders such as diabetes, adrenal disease, and other, pre-operative assessment and intra-operative vigilance is important.[3,4,5,6,7,10] Equally, crucial is the assessment of cardiovascular status, neuro-muscular functions, renal parameters and various other organ systems, which are directly or indirectly affected by various endocrinopathies.
ENDOCRINOPATHIES IN ANESTHESIA AND CRITICAL CARE
The modern day anesthesiologist has to look after intensive care services as well. Occurrence of co-morbid endocrinopathies does impact the management and prognosis of critically ill patients. Timely detection and management of endocrinopathies in such patients can be life-saving.[9,10,11,12] Often, patients are either primarily admitted with uncontrolled diabetes and/or its related complications of diabetes may present as a major co-morbidity during such hospitalization. Similarly, many other endocrine and metabolic disorders may necessitate critical care admissions or are diagnosed for the first time during admission only.[3,4,5,6,7,13,14,15] Still, many new endocrinopathies and metabolic disorders develop de novo during the course of treatment either due to infections and drug effects/interaction or can arise as a complication of various therapeutic procedures such as de novo endocrinopathy: Acute hypoparathyroidism after thyroid surgery; hypopituitarism after pituitary surgery; longterm Nelson's syndrome after adrenal surgery; diabetes after transplant new onset diabetes after transplantation (NODAT) and many more.[3,4,5,6,7,8]
However, it is generally felt that there is a relative shortage of endocrinologists in the developing countries, which makes it mandatory that intensivists should gear up to diagnose and treat such endocrinological disorders.
PHARMACOLOGICAL ASPECTS OF EA
Pharmaco-therapeutic properties of various drugs have to be kept in consideration during management of such patients in intensive care unit (ICU) and operation theaters. Most importantly, anesthetic drugs should be chosen on an individual basis as various anesthetic drugs are known to interfere in endocrine functions.[3,4,5,6,7,8,16] Dopamine, TSH, T4, glucocorticoids causing hyperglycemia in surgical patients are the best example of such pharmacological interaction. Though controversial, nitrous oxide has been incriminated as a cause of impaired sperm function and teratogenicity by acting on methionine synthetase enzyme. Concerns have also been ignited about the genetic modifications induced by the effect of inhalational anesthetics.
At the same time, many endocrine drugs are being increasingly used in anesthesiology and intensive care practice. To enumerate, vasopressin antagonists for hyponatremia, insulin for treatment of hyperglycemia and hyperkalemia, use of testosterone for cessation of uterine bleeding, vasopressin, and terlipressin for stoppage of upper gastro-intestinal (GI) bleeding, glucocorticoids, fludrocortisone, and other steroids for various indications are a few of them. The clinical effects of these drugs have to be kept in consideration both during elective and emergency surgeries.
NEED FOR INCREASED COLLABORATION
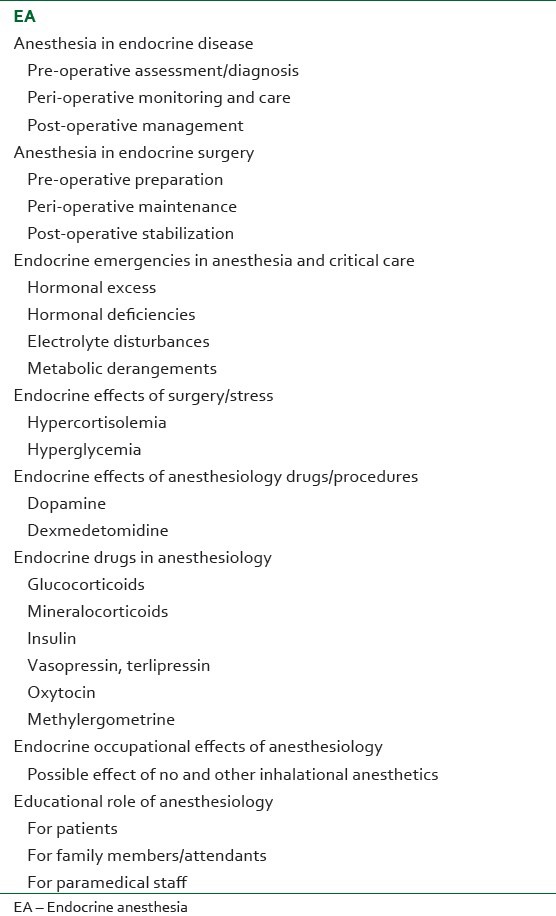
Modern day medicine practice has been fast evolving as a team work among different specialties. Many clinical, practical, and legal reasons have compelled the physicians from various specialties to come together on a common platform to design various management strategies. Guidelines set by various international endocrinology organizations and committees do not address the issues faced by the intensivists and anesthesiologists. Guidelines by the endocrinologists do not highlight the role of intensivists. Anesthesia guidelines do not appreciate the role of endocrinologists. Furthermore, these guidelines have not been completely helpful as they are difficult to apply in totality in resource challenged settings. In spite of this, role of anesthesiologist has grown beyond the four walls of operation theater and ICU. An active participation of anesthesiologist is needed to successfully manage patients with endocrine disorders during pre-operative, intra-operative and post-operative period [Table 1]. Apart from that, motivation of patients to adhere to strict compliance of medication management in various endocrinological disorders can be carried out by anesthesiologist. Such opportunities can be availed during regional anesthesia and surgical cases being performed under monitored anesthesia care. During this period an anesthesiologist can greatly help in disseminating health education and the significance of adherence to strict therapeutic compliance regarding various endocrine disorders such as diabetes and can also convey various other simple preventive and therapeutic strategies. In the operation theater, a patient perceive doctor as next to God and is more likely to imbibe the advice delivered and adhere to various preventive and therapeutic regimens taught during such a crucial period.
Table 1.
Scope of EA
Similarly, the role of an endocrinologist is also underestimated in anesthesiology practice. Whenever feasible, an endocrinologist can be immensely helpful in preparing the patient for any elective or emergency surgery. Endocrinological milieu can be restored to normal before any surgical procedure with the help of an endocrinologist. Overall, such a closely co-ordinated team work can help in achieving a good anesthesia outcome thereby decreasing the overall anesthesia related morbidity and mortality. The increasing incidence and prevalence of various endocrinopathies in patients receiving anesthesia have necessitated that a new sub-speciality of EA be developed and nurtured.
REFERENCES
- 1.Breivik H. Perianesthetic management of patients with endocrine disease. Acta Anaesthesiol Scand. 1996;40:1004–15. doi: 10.1111/j.1399-6576.1996.tb05619.x. [DOI] [PubMed] [Google Scholar]
- 2.Niezgoda J, Morgan PG. Anesthetic considerations in patients with mitochondrial defects. Paediatr Anaesth. 2013;17:228–34. doi: 10.1111/pan.12158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bajwa SS, Sehgal V. Anesthesia and thyroid surgery: The never ending challenges. Indian J Endocrinol Metab. 2013;17:228–34. doi: 10.4103/2230-8210.109671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bajwa SS, Sehgal V. Anesthetic management of primary hyperparathyroidism: A role rarely noticed and appreciated so far. Indian J Endocr Metab. 2013;17:235–9. doi: 10.4103/2230-8210.109679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yong SL, Coulthard P, Wrzosek A. Supplemental perioperative steroids for surgical patients with adrenal insufficiency. Cochrane Database Syst Rev. 2012;12:CD005367. doi: 10.1002/14651858.CD005367.pub3. [DOI] [PubMed] [Google Scholar]
- 6.Bajwa SS, Bajwa SK. Implications and considerations during pheochromocytoma resection: A challenge to the anesthesiologist. Indian J Endocrinol Metab. 2011;15:S337–44. doi: 10.4103/2230-8210.86977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bajwa SS, Bajwa SK. Anesthesia and Intensive care implications for pituitary surgery: Recent trends and advancements. Indian J Endocrinol Metab. 2011;15:S224–32. doi: 10.4103/2230-8210.84872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bajwa SJ, Kalra S. Diabeto-anesthesia: A subspecialty needing endocrine introspection. Indian J Anaesth. 2012;56:513–7. doi: 10.4103/0019-5049.104564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bajwa SJ, Jindal R. Endocrine emergencies in critically ill patients: Challenges in diagnosis and management. Indian J Endocrinol Metab. 2012;16:722–7. doi: 10.4103/2230-8210.100661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalra S, Bajwa SS, Baruah M, Sehgal V. Hypoglycaemia in anesthesiology practice: Diagnostic, preventive, and management strategies. Saudi J Anaesth. 2013;7:447–52. doi: 10.4103/1658-354X.121082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bajwa SJ, Kwatra IS. Reno-endocrinal disorders: A basic understanding of the molecular genetics. Indian J Endocrinol Metab. 2012;16:158–63. doi: 10.4103/2230-8210.93731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bajwa SJ, Kulshrestha A. Renal endocrine manifestations during polytrauma: A cause of concern for the anesthesiologist. Indian J Endocrinol Metab. 2012;16:252–7. doi: 10.4103/2230-8210.93744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vinik AI, Ziegler D. Diabetic cardiovascular autonomic neuropathy. Circulation. 2007;115:387–97. doi: 10.1161/CIRCULATIONAHA.106.634949. [DOI] [PubMed] [Google Scholar]
- 14.Gu W, Pagel PS, Warltier DC, Kersten JR. Modifying cardiovascular risk in diabetes mellitus. Anesthesiology. 2003;98:774–9. doi: 10.1097/00000542-200303000-00029. [DOI] [PubMed] [Google Scholar]
- 15.Scherpereel PA, Tavernier B. Perioperative care of diabetic patients. Eur J Anaesthesiol. 2001;18:277–94. doi: 10.1046/j.0265-0215.2001.00876.x. [DOI] [PubMed] [Google Scholar]
- 16.Vuong C, Van Uum SH, O’Dell LE, Lutfy K, Friedman TC. The effects of opioids and opioid analogs on animal and human endocrine systems. Endocr Rev. 2010;31:98–132. doi: 10.1210/er.2009-0009. [DOI] [PMC free article] [PubMed] [Google Scholar]


