Abstract
Background:
Most of the bad outcomes in patients with severe traumatic brain injury (TBI) are related to the presence of a high incidence of pre-hospital secondary brain insults. Therefore, knowledge of these variables and timely management of the disease at the pre-hospital period can significantly improve the outcome and decrease the mortality. The Brain Trauma Foundation guideline on “Prehospital Management” published in 2008 could provide the standardized protocols for the management of patients with TBI; however, this guideline has included the relevant papers up to 2006.
Methods:
A PubMed search for relevant clinical trials and reviews (from 1 January 2007 to 31 March 2013), which specifically discussed about the topic, was conducted.
Results:
Based on the evidence, majority of the management strategies comprise of rapid correction of hypoxemia and hypotension, the two most important predictors for mortality. However, there is still a need to define the goals for the management of hypotension and inclusion of newer difficult airway carts as well as proper monitoring devices for ensuring better intubation and ventilatory management. Isotonic saline should be used as the first choice for fluid resuscitation. The pre-hospital hypothermia has more adverse effects; therefore, this should be avoided.
Conclusion:
Most of the management trials published after 2007 have focused mainly on the treatment as well as the prevention strategies for secondary brain injury. The results of these trials would be certainly adopted by new standardized guidelines and therefore may have a substantial impact on the pre-hospital management in patients with TBI.
Keywords: Evidence, pre-hospital management, secondary brain injury, traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI) is a major burden (approximately 10 million annually victims) on the health care system throughout the world.[1] Moreover, of the patients who survived from the primary insult, some may still have long-term disability. Most of these outcomes are related to the presence of a high incidence of pre-hospital secondary brain insults.[2,3] Therefore, knowledge of these variables and timely management of the disease at the pre-hospital period can significantly improve the outcome and decrease the mortality.[2,3]
Evidence-based clinical practice “Prehospital Management” by the Brain Trauma Foundation (BTF) guidelines have been modified and revised in 2008.[4] These guidelines could provide the standardized protocols for the management of patients with TBI; however, this guideline has included the relevant papers up to 2006. Thereafter, the results of various trials have been published and the major focus of these is mainly to minimize the secondary brain injury following the primary insults. However, the results and conclusions of these trials are yet to be adopted by standard guidelines.
In this article, we have summarized the various aspects of pre-hospital as well as initial management at emergency department in patients with TBI, including the emerging evidence mainly after the BTF 2008.[4]
METHODS
This is a narrative review based on a PubMed search on the terms including “Traumatic brain injury,” “Head injury,” “Head trauma,” “prehospital,” “Resuscitation” and “Management.” This review has involved the relevant clinical trials and reviews (from 1 January 2007 to 31 March 2013) that specifically discussed about the topic. The studies with a minimum of 50 patients are included. The papers in any language have been included; however, pediatric and pregnant patients are not included in this review.
Etiopathogenesis
The most common cause for inciting head injury is motor vehicle accident (MVA).[1,2,3] The other causes of TBI are falls from heights, physical assaults, accidents at home, offices or while playing sports, gunshot and blast injuries. Head injury can be either closed (blunt) or open (penetrating) injury and is further classified into primary injury and secondary injury. This classification is rather more useful while considering the therapeutic and preventive strategies [Table 1].
Table 1.
Classification of brain injury and factors affecting these in patients with TBI
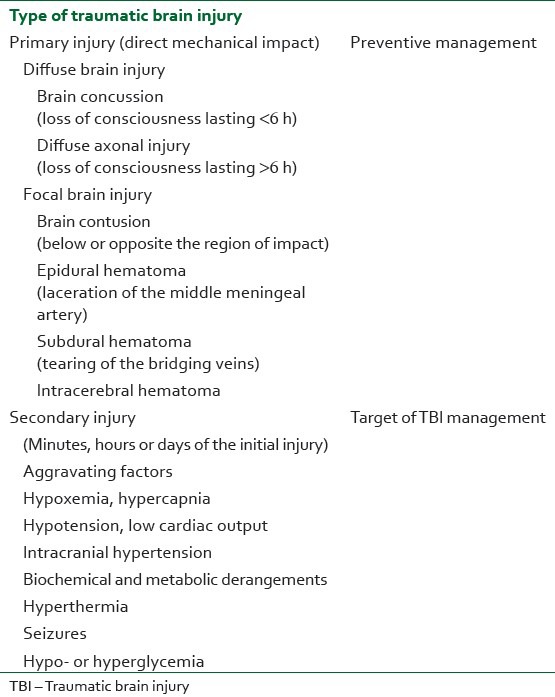
Brain tissue destroyed by the primary impact is very difficult to be salvaged. Secondary brain injury, the sequel of primary insult, is potentially treatable and most of the therapies are targeted to prevent these sequelae. This secondary injury is primarily amplified by various cofactors, including hypoxemia, hypotension, hypercarbia, hypoglycemia, hyperglycemia, hypothermia/hyperthermia, seizures, etc., [Table 1]. The morbidity, mortality and long-term disability are substantially dependent on the management of secondary brain insult. Therefore, functional outcome may be improved by good intensive medical care and by prompt surgical interventions.[2,3,5]
Evaluation
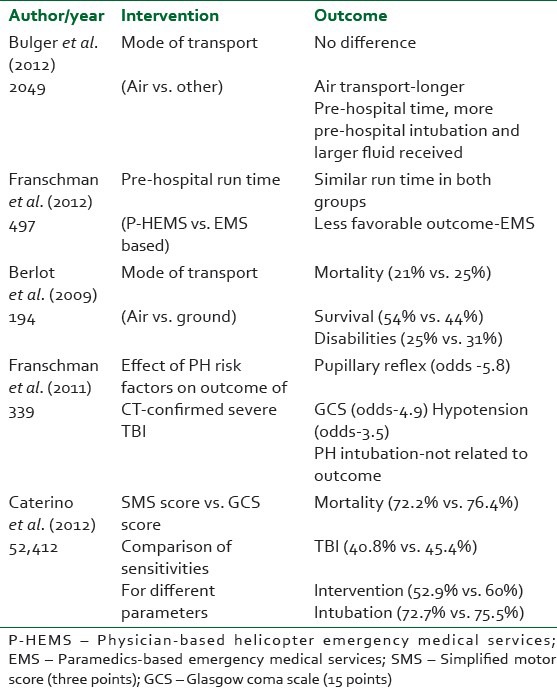
Physiological parameters including Glasgow Coma Scale (GCS) score, systolic blood pressure and respiratory rate are useful predictors for the outcome and can be utilized in the pre-hospital triage of patients with TBI [Table 2].[5] The GCS is a quick, reproducible scoring system that has worldwide acceptance and is used to define the severity of TBI, with severe TBI defined as GCS of ≤ 8. It is based on eye opening, verbal response and the best motor response. An early, non-sedated GCS has been shown to predict prognosis. The lowest total score indicates likely fatal damage, especially if both pupils fail to respond to light and oculovestibular responses are absent. Higher initial scores tend to predict better recovery.[5] The data from the 2007 National Trauma Data Bank (NTDB) National Sample Program showed that after controlling for age, gender, race, Injury Severity Score (ISS) and length of stay in the hospital, patients who had a GCS score ≤13 were 17-times more likely to die than TBI patients who had a higher GCS score.[5] The other scoring system, the simplified motor score (SMS), a three-point measure of TBI severity, is also found to perform equally well as GCS and is validated in many trials. In a retrospective review of 52,412 patients, sensitivity, specificity and area under the receiver – operating characteristic curves were similar between the SMS and GCS for all outcomes.[6] Sensitivity for mortality was 72.2% for SMS and 74.6% for GCS. Sensitivity for TBI was 40.8% for SMS and 45.4% for GCS. Sensitivity for neurosurgical intervention was 52.9% for SMS and 60.0% for GCS.[6] However, the severity and prognosis are predicted more accurately by also considering the computed tomography (CT) scan findings and other clinical factors including a disturbed pupil reflex and arterial hypotension.[5,7,8] Other investigations like X-ray and ultrasound are also helpful to rule out other major injuries.
Table 2.
Evidence on the effect of pre-hospital evaluation/transport methods/personals/duration on outcome
An early non-contrast brain CT is required to guide subsequent therapy. In fact, CT scan facility located in the trauma or emergency room has been found to reduce the time to acquire CT images and improves overall mortality.[8] Once airway, breathing or ventilation and blood pressure is maintained, one should concentrate on the management of intracranial hypertension and evaluate the other associated injuries.
Transportation
The outcome in patients with TBI is also found to be affected by the transport methods, duration and physician or paramedics lead team [Table 2].[9,10] In some systems, air medical crews may provide a higher level of care but may require longer transport times. Based on the analysis of data (2049 patients) from two randomized trials of pre-hospital hypertonic resuscitation, patients transported by air (in comparison with ground transport) had higher rates of pre-hospital intubation (81% vs. 36%), received more intravenous fluids (mean 1.3 L vs. 0.8 L) and had longer pre-hospital times (mean 76.1 min vs. 43.5 min).[9] However, there was no significant impact of mode of transport on survival or 6-month neurologic outcome.[9] Similarly, in a retrospective review of 194 patients, air-based emergency medical services were associated with a lower rate of mortality (21% vs. 25%) as well as neurological disabilities (25% vs. 31%).[11] In addition, a retrospective study of 497 patients with severe TBI showed that in comparison with paramedics, physician-lead helicopter emergency services were found to have a more favorable outcome and mortality scores and there were also similar pre-hospital run times between the two groups.[10] Therefore, there is a need to integrate the most effective transport system through which patients of TBI can be shifted to a specialized trauma center within the minimum possible time. The time is a crucial factor for the occurrence as well as the prevention of secondary brain injury; therefore, the transport vehicle should have all possible drugs/equipment and monitoring devices. Accompanying emergency medical personnels should also have a thorough knowledge of important risk factors and guideline-based management strategies to ensure substantial prevention of secondary brain injury.[9,10,11]
Initial management
The guidelines of Advanced Trauma Life Support (ATLS) provide a standardized protocol for approaching the severely injured patient, with special attention to airway, breathing and circulation.
Hypoxemia
The first most important consideration in TBI is the maintenance of a clear and unobstructed airway [Tables 3, 4]. Hypoxemia is the most important factors related to worse outcome and therefore needs urgent attention.[12] In a multicenter prospective study of 150 patients, the mortality was found to be 20% in patients without secondary insults; however, it increased to 37% during hypoxic episodes.[12] Patients with severe TBI are to be intubated by rapid sequence induction by skilled personnel. The cervical spine must be protected and should always be assumed to be injured until definitively cleared while securing the airway. A randomized controlled trial showed that rapid sequence intubation (RSI) performed by paramedics was associated with an increase in the rate of favorable neurologic outcome at 6 months compared with intubation in the hospital; this highlights the importance of immediate airway control in cases of severe TBI.[13] Similarly, an observational study of 334 patients with pre-hospital hypothermia (PH) intubations and GCS score ≤8 and proven TBI (on CT scan) revealed a higher rate of overall intubations and was associated with no increase in mortality over the emergency department intubation.[14] In addition, the use of RSI with appropriate use of anesthetic agents is of paramount significance to prevent aspiration-related adverse events and simultaneously prevent sympathetic surge incited by airway manipulations; however, avoidance of hypotension should be ensured. The role of lidocaine in cases of RSI is also controversial; however, a recent retrospective cohort of 101 patients showed that lidocaine can be used without producing adverse hemodynamic changes.[15]
Table 3.
Evidence on pre-hospital airway management/monitoring
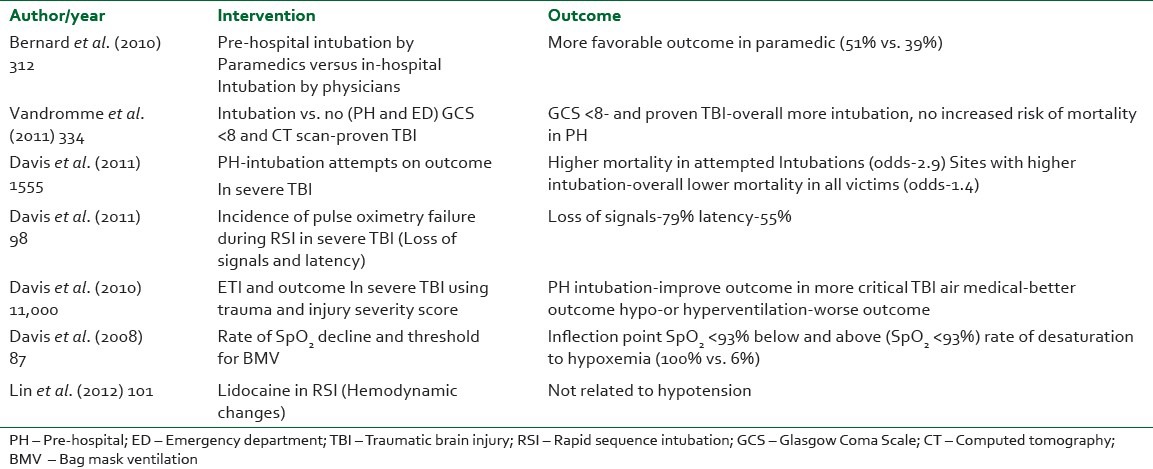
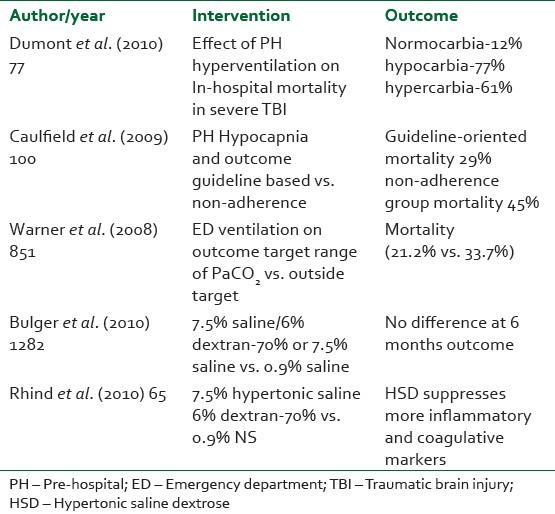
Table 4.
Evidence on pre-hospital ventilation and fluid resuscitation
The technique and equipment are also equally important to manage the pre-hospital intubations, especially by the paramedics. In this regard, the role of video-laryngoscopes and other difficult intubation kits may certainly give better chances for airway management and thus would prevent the secondary brain injuries related to hypoxemia.[16]
In addition, a high incidence of oxygen desaturation during PH intubations warrants standard monitoring such as pulse oximetry. A study on 87 patients with TBI undergoing RSI by pre-hospital providers revealed that the rate of SpO2 decline increases as the SpO2 decreases, with an inflection point occurring around 93%.[17] Intubation attempts below this value are almost always associated with subsequent desaturation.[17] However, a high incidence of pulse oximetry failure was also observed with the use of a digital pulse oximetry probe during pre-hospital RSI.[18] In a retrospective study of 124 patients with severe TBI, 79% of the patients had pulse oximetry failure at the time of RSI. In addition, a latent period appears to exist in the majority of patients (55%) undergoing desaturation.[18] Therefore, caution should be paid to all differential causes of oxygen desaturation, including pulse oximetry related, while attempting RSI.
Hypercarbia/hypocarbia
The intubated patients should be ventilated so as to maintain normocarbia (PaCO2 35 and 40 mmHg). Monitoring of oxygen saturation and capnography is recommended in severely head-injured patients so as to avoid unrecognized hypoxemia or changes in ventilation [Tables 3, 4].[4] This is best assessed by end tidal capnography, and generally corresponds to EtCO2 30-35 mmHg.[4] In analysis of data of 11,000 patients, both hypo- and hypercapnia were associated with worse outcomes in intubated patients.[19] In another retrospective review of 77 patients, both hypocarbia (PaCO2 - <35 mmHg) and hypercarbia (PaCO2 - >45 mmHg) were associated with a substantial increase in in-hospital mortality (77% and 61%, respectively).[20] A study on guideline-based management in pre-hospital ventilation (PaCO2 >29 mmHg) in 100 patients (without herniation signs) showed that the in-hospital mortality was 29% among those in whom guideline levels were achieved and 46% (16 of 35) in those in whom guideline levels were not achieved pre-hospital. Similarly, a retrospective review of 851 patients on targeted ventilation (PaCO2 30-39 mmHg) at the emergency department also found decreased mortality (21.2% vs. 33.7%) in comparison with ventilation achieved outside the target range.[21] Therefore, pre-hospital normoventilation should be ensured. However, in cases with signs of potential brain herniation, transient hyperventilation may be an option. There is strong evidence that capnography can affect the outcome. Therefore, continuous capnography is recommended in all ventilated TBI patients.[21,22] As ETCO2 values may be confounded by low tissue perfusion, long-term ventilation should be guided by the frequent sampling of blood gases.[23] The frequency of blood gas sampling is yet to be quantified.
Oxygenation and ventilation can become difficult if there are other major injuries, particularly chest injuries, aspiration of gastric contents or acute pulmonary edema. Appropriate positive end expiratory pressure (PEEP) should be used. There is no evidence that 10 mmHg PEEP impairs cerebral blood flow or elevates intracranial pressure (ICP) and, indeed, ICP may improve with improved oxygenation.[24]
Hypotension/hypertension
Hypotension is a major secondary brain insult and studies have demonstrated that a single episode of hypotension dramatically worsens the outcome.[5] Hypotension should be treated with fluid resuscitation to euvolaemia and, if necessary, vasopressors are used to maintain optimum blood pressure. According to BTF, prior to the insertion of an ICP monitoring, a MAP ≥ 80 mmHg is recommended. The rationale for a MAP ≥ 80 mmHg is to maintain cerebral perfusion pressure (CPP) ≥ 60 mmHg for a treatment threshold of ICP > 20 mmHg.[25] Following the insertion of an ICP monitoring, the management of MAP will be directed by the ICP/CPP values.
However, recent studies have challenged the lower limit to define hypotension in patients with isolated head injury.[26,27] In a study of 15,733 patients with moderate to severe head injury, the value of systolic blood pressure of 110 mmHg or less is computed as the best fit model for hypotension when mortality was taken as the outcome measure.[26] In another study, maintaining a systolic blood pressure of approximately 120 mmHg has been found to be more efficacious to minimize the secondary brain injury.[27] Therefore, further large clinical trials are needed to support these findings. It is recommended that patients with severe TBI have arterial and central venous lines placed as soon as practical.
Hypertension may be a physiological response produced due to sympathetic surge, and may signify a compromised cerebral perfusion. Hypertension should not be treated unless a cause has been excluded or treated and the systolic blood pressure is >180-200 mmHg or the MAP is >110-120 mmHg.[28] Lowering an increased blood pressure, as a compensatory mechanism to maintain an adequate CPP, exacerbates cerebral ischemia. For the treatment of hypertension to achieve CPP targets, an infusion of short-acting beta blocker is very useful, which maintains blood pressure. These agents do not cause cerebral vasodilatation when compared with nitrates and calcium channel blockers and, therefore, do not increase the cerebral blood volume and ICP.[28]
Fluid resuscitation
Further to this, the prompt resuscitation with fluids is of paramount importance to preserve optimum CPP [Table 4]. However, the choice of fluids is still a matter of great conflict. Some studies have suggested that hypertonic fluids might suppress the biomarkers of TBI and are correlated with better outcome.[29] Many studies have investigated the effect of various fluids on pre-hospital resuscitation. No studies have reported better survival and functional outcomes over the use of isotonic crystalloids.[30] Further to this, a multicenter randomized control trial (RCT) of 1087 patients (15 years or older with blunt trauma who did not meet the criteria for hypovolemic shock) with severe TBI (GCS 8 or less) showed that even the initial resuscitation with hypertonic saline or hypertonic saline/dextran, compared with normal saline, were found to be comparable in terms of 6-month neurologic outcome or survival.[31] However, this study was terminated by the data and safety monitoring board after randomization of 1331 patients. On the other hand, post hoc analysis (460 patients) of a multicenter RCT study titled “Saline Albumin Fluid Resuscitation Trial (SAFE)” highlighted that the use of albumin was associated with the higher mortality data in patients with severe head injury.[32] Among patients with severe brain injury (GCS 3-8), 41.8% patients died in the albumin group as compared with 22.2% patients in the saline group; however, among patients with GCS scores of 9–12, death occurred in eight of 50 patients in the albumin group (16.0%) and eight of 37 patients in the saline group (21.6%).[32] Based on these findings, colloids should not be used as the first choice of fluid, especially in patients with severe TBI, and isotonic crystalloids seem to be a safer choice and are cost-effective as well. The role of colloids in mild to moderate severe head injury is at present inconclusive and therefore needs well-designed RCTs.
PH
Hypothermia has some protective effects in TBI by reducing ICP, cerebral metabolic demands, decreasing disruption of the blood–brain barrier and inhibiting the inflammatory cascade. Induced hypothermia is now an accepted measure to improve outcome following anoxic brain injury associated with cardiac arrest, but its benefits in TBI are inconclusive at present.[33] In a systemic review (12 RCTs), data support the use of early prophylactic mild-to-moderate hypothermia in patients with severe TBI (GCS score ≤8) to decrease mortality and improve the rates of good neurologic recovery.[33] However, this review advocates for early use (emergency department) of therapeutic hypothermia and also recommends a long-term or goal-directed cooling protocol, in which cooling was continued for at least 72 h and/or until stable normalization of ICP for at least 24 h was achieved. On the other hand, in an epidemiological study (level III evidence) of 21,023 patients, 44.6% patients presented with PH.[34] Moreover, hypothermic patients in comparison with normothermic patients required 26% more fluid resuscitation and 17% more total blood products in the emergency department. PH was found to be independently associated with increased adverse events, including need for a transfusion, mortality, incidence of adult respiratory distress syndrome and pneumonia.[34] Similarly, a retrospective review of 1281 patients highlighted that presence of hypothermia (<35°C) on Intensive Care Unit (ICU) admission was found to be an independent factor to increase the mortality. In addition, penetrating injury, Injury Severity Score ≥25 and exploratory laparotomy before admission were found to be independent risk factors for the development of hypothermia on ICU admission.[35] The impact of preventative measures used to avoid the development of hypothermia and the effectiveness of measures for restoring normothermia warrant further investigation.
CONCLUSION
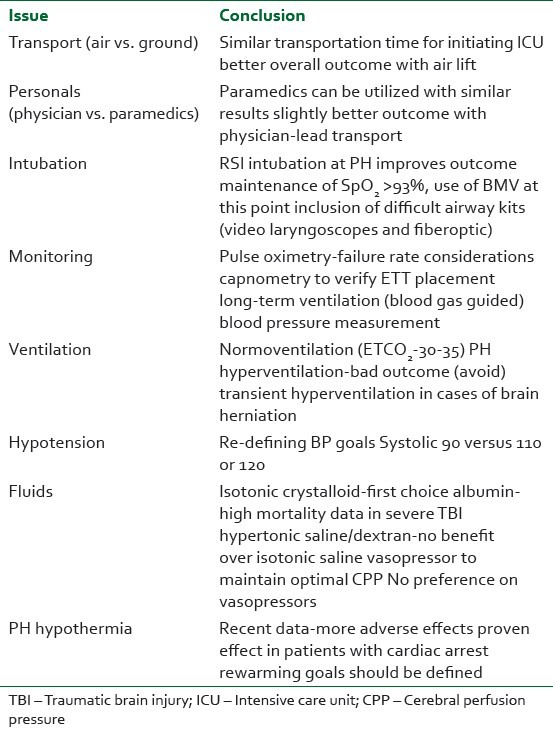
Severe TBI patients impose very high mortality and morbidity and, strikingly, a substantial portion of these bad outcomes can be prevented by prompt evaluation and pre-hospital as well as early emergency management of such cases [Table 5]. Based on the evidence, majority of the management strategies comprise of rapid correction of hypoxemia and hypotension, the two most important predictors for mortality. However, there is still a need to define the goals for the management of hypotension and inclusion of newer difficult airway carts as well as proper monitoring devices for ensuring better intubation and ventilatory management. Isotonic saline should be used as the first choice for fluid resuscitation. The PH has more adverse effects and should therefore be avoided.
Table 5.
Keys issues in the pre-hospital management of TBI patients
Most of the management trials published after 2007 have focused mainly on the treatment as well as the prevention strategies for secondary brain injury. The results of these trials would certainly be adopted by new standardized guidelines and, therefore, may have a substantial impact on the pre-hospital management in patients with TBI.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: A global perspective. Neuro Rehabil. 2007;22:341–53. [PubMed] [Google Scholar]
- 2.Myburgh JA, Cooper DJ, Finfer SR, Venkatesh B, Jones D, Higgins A, et al. Australasian Traumatic Brain Injury Study (ATBIS) Investigators for the Australian; New Zealand Intensive Care Society Clinical Trials Group. Epidemiology and 12-month outcomes from traumatic brain injury in australia and new zealand. J Trauma. 2008;64:854–62. doi: 10.1097/TA.0b013e3180340e77. [DOI] [PubMed] [Google Scholar]
- 3.Wu X, Hu J, Zhuo L, Fu C, Hui G, Wang Y, et al. Epidemiology of traumatic brain injury in eastern China, 2004: A prospective large case study. J Trauma. 2008;64:1313–9. doi: 10.1097/TA.0b013e318165c803. [DOI] [PubMed] [Google Scholar]
- 4.Badjatia N, Carney N, Crocco TJ, Fallat ME, Hennes HM, Jagoda AS, et al. Brain Trauma Foundation; BTF Center for Guidelines Management. Prehosp Emerg Care. 2008;12(Suppl 1):S1–52. doi: 10.1080/10903120701732052. [DOI] [PubMed] [Google Scholar]
- 5.Pearson WS, Ovalle F, Jr, Faul M, Sasser SM. A review of traumatic brain injury trauma center visits meeting physiologic criteria from The American College of Surgeons Committee on Trauma/Centers for Disease Control and Prevention Field Triage Guidelines. Prehosp Emerg Care. 2012;16:323–8. doi: 10.3109/10903127.2012.682701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caterino JM, Raubenolt A. The prehospital simplified motor score is as accurate as the prehospital Glasgow coma scale: Analysis of a statewide trauma registry. Emerg Med J. 2012;29:492–6. doi: 10.1136/emj.2010.110437. [DOI] [PubMed] [Google Scholar]
- 7.Franschman G, Peerdeman SM, Andriessen TM, Greuters S, Toor AE, Vos PE, et al. Amsterdam Lifeliner: Analysis of Results and Methods--Traumatic Brain Injury (ALARM-TBI) Investigators. Effect of secondary prehospital risk factors on outcome in severe traumatic brain injury in the context of fast access to trauma care. J Trauma. 2011;71:826–32. doi: 10.1097/TA.0b013e31820cebf0. [DOI] [PubMed] [Google Scholar]
- 8.Saltzherr TP, Bakker FC, Beenen LF, Dijkgraaf MG, Reitsma JB, Goslings JC REACT Study Group. Randomized clinical trial comparing the effect of computed tomography in the trauma room versus the radiology department on injury outcomes. Br J Surg. 2012;99:105–13. doi: 10.1002/bjs.7705. [DOI] [PubMed] [Google Scholar]
- 9.Bulger EM, Guffey D, Guyette FX, MacDonald RD, Brasel K, Kerby JD, et al. Impact of prehospital mode of transport after severe injury: A multicenter evaluation from the Resuscitation Outcomes Consortium. J Trauma Acute Care Surg. 2012;72:567–73. doi: 10.1097/TA.0b013e31824baddf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Franschman G, Verburg N, Brens-Heldens V, Andriessen TM, Van der Naalt J, Peerdeman SM, et al. Effects of physician- based emergency medical service dispatch in severe traumatic brain injury on prehospital run time. Injury. 2012;43:1838–42. doi: 10.1016/j.injury.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 11.Berlot G, La Fata C, Bacer B, Biancardi B, Viviani M, Lucangelo U, et al. Influence of prehospital treatment on the outcome of patients with severe blunt traumatic brain injury: A single-centre study. Eur J Emerg Med. 2009;16:312–7. doi: 10.1097/MEJ.0b013e32832d3aa1. [DOI] [PubMed] [Google Scholar]
- 12.Chi JH, Knudson MM, Vassar MJ, McCarthy MC, Shapiro MB, Mallet S, et al. Prehospital hypoxia affects outcome in patients with traumatic brain injury: A prospective multicenter study. J Trauma. 2006;61:1134–41. doi: 10.1097/01.ta.0000196644.64653.d8. [DOI] [PubMed] [Google Scholar]
- 13.Bernard SA, Nguyen V, Cameron P, Masci K, Fitzgerald M, Cooper DJ, et al. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: A randomized controlled trial. Ann Surg. 2010;252:959–65. doi: 10.1097/SLA.0b013e3181efc15f. [DOI] [PubMed] [Google Scholar]
- 14.Vandromme MJ, Melton SM, Griffin R, McGwin G, Weinberg JA, Minor M, et al. Intubation patterns and outcomes in patients with computed tomography-verified traumatic brain injury. J Trauma. 2011;71:1615–9. doi: 10.1097/TA.0b013e31822a30a1. [DOI] [PubMed] [Google Scholar]
- 15.Lin CC, Yu JH, Lin CC, Li WC, Weng YM, Chen SY. Postintubation hemodynamic effects of intravenous lidocaine in severe traumatic brain injury. Am J Emerg Med. 2012;30:1782–7. doi: 10.1016/j.ajem.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 16.Bauer K. Prehospital airway management: High tech meets trauma: An air medical perspective. Crit Care Nurs Q. 2012;35:281–91. doi: 10.1097/CNQ.0b013e3182542eb5. [DOI] [PubMed] [Google Scholar]
- 17.Davis DP, Hwang JQ, Dunford JV. Rate of decline in oxygen saturation at various pulse oximetry values with prehospital rapid sequence intubation. Prehosp Emerg Care. 2008;12:46–51. doi: 10.1080/10903120701710470. [DOI] [PubMed] [Google Scholar]
- 18.Davis DP, Aguilar S, Sonnleitner C, Cohen M, Jennings M. Latency and loss of pulse oximetry signal with the use of digital probes during prehospital rapid-sequence intubation. Prehosp Emerg Care. 2011;15:18–22. doi: 10.3109/10903127.2010.514091. [DOI] [PubMed] [Google Scholar]
- 19.Davis DP, Peay J, Sise MJ, Kennedy F, Simon F, Tominaga G, et al. Prehospital airway and ventilation management: A trauma score and injury severity score-based analysis. J Trauma. 2010;69:294–301. doi: 10.1097/TA.0b013e3181dc6c7f. [DOI] [PubMed] [Google Scholar]
- 20.Dumont TM, Visioni AJ, Rughani AI, Tranmer BI, Crookes B. Inappropriate prehospital ventilation in severe traumatic brain injury increases in-hospital mortality. J Neurotrauma. 2010;27:1233–41. doi: 10.1089/neu.2009.1216. [DOI] [PubMed] [Google Scholar]
- 21.Caulfield EV, Dutton RP, Floccare DJ, Stansbury LG, Scalea TM. Prehospital hypocapnia and poor outcome after severe traumatic brain injury. J Trauma. 2009;66:1577–82. doi: 10.1097/TA.0b013e3181a3931d. [DOI] [PubMed] [Google Scholar]
- 22.Holmes J, Peng J, Bair A. Abnormal end-tidal carbon dioxide levels on emergency department arrival in adult and pediatric intubated patients. Prehosp Emerg Care. 2012;16:210–6. doi: 10.3109/10903127.2011.640416. [DOI] [PubMed] [Google Scholar]
- 23.Warner KJ, Cuschieri J, Garland B, Carlbom D, Baker D, Copass MK, J, et al. The utility of early end-tidal capnography in monitoring ventilation status after severe injury. J Trauma. 2009;66:26–31. doi: 10.1097/TA.0b013e3181957a25. [DOI] [PubMed] [Google Scholar]
- 24.Mascia L, Zavala E, Bosma K, Pasero D, Decaroli D, Andrews P, et al. High tidal volume is associated with the development of acute lung injury after severe brain injury: An international observational study. Crit Care Med. 2007;35:1815–20. doi: 10.1097/01.CCM.0000275269.77467.DF. [DOI] [PubMed] [Google Scholar]
- 25.Bullock MR, Povlishock JT, editors. Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons, AANS/CNS Joint Section on Neurotrauma and Critical Care. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. (3rd ed) 2007;24(suppl 1):S1–106. [Google Scholar]
- 26.Berry C, Ley EJ, Bukur M, Malinoski D, Margulies DR, Mirocha J, et al. Redefining hypotension in traumatic brain injury. Injury. 2012;43:1833–7. doi: 10.1016/j.injury.2011.08.014. [DOI] [PubMed] [Google Scholar]
- 27.Brenner M, Stein DM, Hu PF, Aarabi B, Sheth K, Scalea TM. Traditional systolic blood pressure targets underestimate hypotension-induced secondary brain injury. J Trauma Acute Care Surg. 2012;72:1135–9. doi: 10.1097/TA.0b013e31824af90b. [DOI] [PubMed] [Google Scholar]
- 28.Haddad SH, Arabi YM. Critical care management of severe traumatic brain injury in adults. Scand J Trauma Resusc Emerg Med. 2012;20:12. doi: 10.1186/1757-7241-20-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baker AJ, Rhind SG, Morrison LJ, Black S, Crnko NT, Shek PN, et al. Resuscitation with hypertonic saline-dextran reduces serum biomarker levels and correlates with outcome in severe traumatic brain injury patients. J Neurotrauma. 2009;26:1227–40. doi: 10.1089/neu.2008.0868. [DOI] [PubMed] [Google Scholar]
- 30.Tan PG, Cincotta M, Clavisi O, Bragge P, Wasiak J, Pattuwage L, et al. Review article: Prehospital fluid management in traumatic brain injury. Emerg Med Australas. 2011;23:665–76. doi: 10.1111/j.1742-6723.2011.01455.x. [DOI] [PubMed] [Google Scholar]
- 31.Bulger EM, May S, Brasel KJ, Schreiber M, Kerby JD, Tisherman SA, et al. Out-of-hospital hypertonic resuscitation following severe traumatic brain injury: A randomized controlled trial. JAMA. 2010;304:1455–64. doi: 10.1001/jama.2010.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Myburgh J, Cooper DJ, Finfer S, Bellomo R, Norton R, Bishop N, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357:874–84. doi: 10.1056/NEJMoa067514. [DOI] [PubMed] [Google Scholar]
- 33.Fox JL, Vu EN, Doyle-Waters M, Brubacher JR, Abu-Laban R, Hu Z. Prophylactic hypothermia for traumatic brain injury: A quantitative systematic review. CJEM. 2010;12:355–64. doi: 10.1017/s1481803500012471. [DOI] [PubMed] [Google Scholar]
- 34.Bukur M, Hadjibashi AA, Ley EJ, Malinoski D, Singer M, Barmparas G, et al. Impact of prehospital hypothermia on transfusion requirements and outcomes. J Trauma Acute Care Surg. 2012;73:1195–201. doi: 10.1097/TA.0b013e31826fc7d9. [DOI] [PubMed] [Google Scholar]
- 35.Bukur M, Kurtovic S, Berry C, Tanios M, Ley EJ, Salim A. Pre-hospital hypothermia is not associated with increased survival after traumatic brain injury. J Surg Res. 2012;175:24–9. doi: 10.1016/j.jss.2011.07.003. [DOI] [PubMed] [Google Scholar]


