Sir,
Ultrasound inter-scalene brachial plexus block (ISBPB) is one of the most common procedures carried out for upper limb surgery. However, anatomical variations in brachial plexus anatomy with respect to scalene muscles are common.[1] With ultrasound guided inter-scalene block, the commonly described anatomical position of the brachial plexus lying between the anterior and middle scalene muscle is seen in 60% of cases only. These variations may pose a problem for nerve stimulation-based approaches to brachial plexus blocks above the clavicle. We report a brachial plexus anomaly at inter-scalene level that was uncommon in our experience.
A 55-year-old male who presented to our operation theater at Jai Prakash Narayan Apex Trauma Center, All India Institute of Medical Sciences with fracture radius was scheduled for open reduction and internal fixation. After patient's consent, we planned to give ultrasound guided supraclavicular brachial plexus block. Since the brachial plexus imaging is most consistent in supraclavicular region, we routinely practice to scan supraclavicular region first and trace the plexus to inter-scalene groove. In our patient, brachial plexus anatomy at the level of supraclavicular region was near normal, but as we traced the plexus cranially toward inter-scalene groove, we noticed that the plexus was missing from inter-scalene groove. All ventral rami were seen stacked medial to the anterior scalene muscle (ASM) and lateral to internal jugular vein [Figure 1]. We confirmed these roots by stimulating with nerve stimulator. We gave supraclavicular nerve block to patient and surgery was uneventful with no complications and complete paresthesia with motor blockade. Sonography of the opposite side of the brachial plexus revealed no such anomaly and the ventral rami were all stacked between the two scalene muscles.
Figure 1.
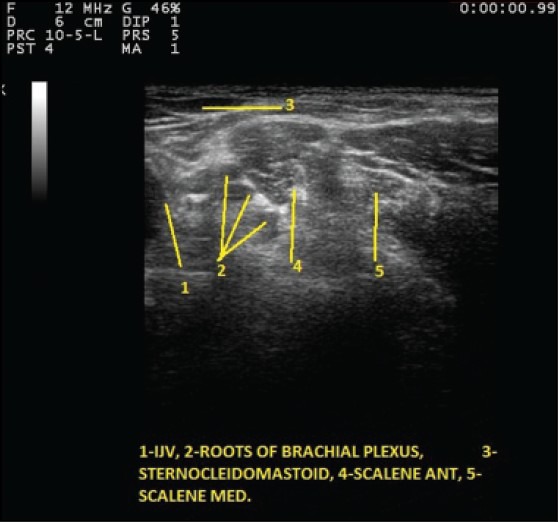
Inter-scalene brachial plexus anomaly (1) Internal jugular vein, (2) roots of brachial plexus, (3) sternocleidomastoid, (4) scalene ant, (5) scalene med
The upper nerve roots of the brachial plexus in the inter-scalene region have been reported with 13-35% anomalies involving their relation to the ASM. The C5 and C6 nerve roots either course through or anterior to the ASM before assuming a normal position in the inter-scalene groove posterolateral to the subclavian artery.[1,2,3]
There have been not many studies and a few case reports only on scalene muscle anomaly.
In a study performed on cadavers by Harry et al., it was found that the most common variation was the penetration of the ASM by the C5 and/or C6 ventral rami.[1]
Chin et al. also reported an anomalous course of the C5 roots located just medial to the ASM. The C6 root lay slightly more lateral, but still inferomedial to the ASM.[4]
In our patient, it seemed that most of the roots originating from ventral rami were medial to the ASM. In none of our cases we had encountered an anatomical variation like this. The clinical implications of these anomalies were more when only nerve stimulator is used for ISBPB. These anomalies lead to restriction of the distribution of the local anesthetic injection resulting in inadequate analgesia. The clinical significance of this anomaly is that in landmark guided technique there would have been sparing of the block in this patient. Therefore, in view of such high anatomical anomaly we recommend that ultrasound should be used in ISBPB. Since the anatomical anomaly in supraclavicular region is fewer; therefore, anesthetist should be prefer it in patients. In addition, sonographic assessment of more volunteers is needed so that frequency of this kind of anatomical variation may be assessed in the general population.
REFERENCES
- 1.Harry WG, Bennett JD, Guha SC. Scalene muscles and the brachial plexus: Anatomical variations and their clinical significance. Clin Anat. 1997;10:250–2. doi: 10.1002/(SICI)1098-2353(1997)10:4<250::AID-CA6>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 2.Kessler J, Gray AT. Sonography of scalene muscle anomalies for brachial plexus block. Reg Anesth Pain Med. 2007;32:172–3. doi: 10.1016/j.rapm.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 3.Natsis K, Totlis T, Tsikaras P, Anastasopoulos N, Skandalakis P, Koebke J. Variations of the course of the upper trunk of the brachial plexus and their clinical significance for the thoracic outlet syndrome: A study on 93 cadavers. Am Surg. 2006;72:188–92. [PubMed] [Google Scholar]
- 4.Chin KJ, Niazi A, Chan V. Anomalous brachial plexus anatomy in the supraclavicular region detected by ultrasound. Anesth Analg. 2008;107:729–31. doi: 10.1213/ane.0b013e31817dc887. [DOI] [PubMed] [Google Scholar]


