Abstract
Background:
Application of upper lip catch test (ULCT) for airway evaluation in edentulous patients.
Methods:
This research is an evaluation of a clinical diagnostic test in edentulous patients prior to operation. Five hundred eighty eight edentulous patients in a referral university hospital, between March 2008 and June 2011 scheduled for elective surgery under general anesthesia were enrolled. Those unable to open the mouth and those with pharyngo-laryngeal pathology were excluded. ULCT was assessed and compared with Cormack-Lehane grading as a gold standard for airway evaluation.
Results:
A high negative predictive value of 99.4% was a notable finding for the ULCT. The results also showed a high specificity (89.4%), high sensitivity (75.0%) and a high accuracy (89.3%) in a comparatively higher range for the ULCT.
Conclusion:
The ULCT proved to be a useful predictor for airway assessment in edentulous patients in this setting. Further studies are needed to reconfirm its validity in other ethnic groups.
Keywords: Airway, Cormack-Lehane grade, difficult intubation, modified Mallampati test, upper lip catch test
INTRODUCTION
The foremost responsibility of an Anesthesiologist is to maintain adequate oxygenation and in achieving this end, maintenance of airway becomes an essential goal. Since an unanticipated difficult airway after induction of anesthesia can result in hypoventilation, hypoxemia and death, tests detecting difficult airway become highly important.
The incidence of difficult intubation varies considerably and has been reported between 1% to as high as 18%.[1,2,3,4] Edentulous patients are usually excluded from studies on the assumption that this variable in itself may independently affect the predictability of difficult intubation.[5,6] Eberhart et al.[7] had to exclude 11% of a series of 1425 consecutive patients as the upper lip bite test (ULBT) could not be applied to edentulous patients. The ULBT initially introduced by Khan et al.[5] was intended to evaluate airway class in subjects possessing teeth and excluded edentulous patients as the ULBT was not designed to include and evaluate the edentulous population. The first classification of airway assessment, the ULBT was in fact the harbinger and predecessor of another classification, the upper lip catch test (ULCT), which is explicitly intended and solely designed to evaluate the airway class in edentulous patients. Although, the edentulous state can provide axis alignment easier, but the obstruction of hypopharyngeal structures by the tongue can result in difficult airway management.[8] However, dentition is an important factor in the management of airway, the impacts of its absence on evaluation of airway has not been evaluated in the literature owing perhaps to the non-availability of a specific diagnostic airway test to address this class of patients. The ULCT was introduced for the first time by Khan ZH et al.[9] in response to a letter where in Herschman[10] had raised a concern that the ULBT failed to address the edentulous patients and thus a large number of patients would be disqualified based on their lack of dentition. The ULCT had the essential milestones to provide coverage for the edentulous patients as an airway assessment test.
Since edentulous patients form a major bulk of our patients, Khan ZH et al.[9] proposed a new airway assessment, the ULCT to accommodate these patients in their pilot study.
The present study aims to apply the ULCT for airway evaluation in edentulous patients undergoing elective surgery under general anesthesia and compare the results with Cormack-Lehane grading (CLG) as a gold standard for laryngoscopic view. The modified Mallampati test (MMT) was also evaluated to compare its diagnostic value with ULCT keeping in consideration that the CLG would be the gold standard of laryngoscopic view. The main aim of this study was to test the hypothesis that the ULCT could serve as a standard test with an acceptable diagnostic accuracy of airway evaluation in edentulous patients.
METHODS
An approval was obtained from our Institution's Ethical Committee (… University of Medical Sciences’ Ethical Committee, …, …, February 20, 2008,) and written informed consent from the enrolled patients.
A total of 634 consecutive male or female edentulous patients ≥60 year scheduled to undergo elective surgery under general anesthesia between March 2008 and June 2011 were considered for enrollment. Non-cooperative patients, those unable to open the mouth or with pharyngolaryngeal pathology were excluded from the study. Patients with fixed prosthetic dentures were also excluded and mobile dentures if present were removed to adhere to the true definition of an edentulous case. Forty six patients were excluded and 588 were enrolled.
In order to control reliability two examiners were trained in performing the tests and calibrated by an experienced examiner 2 week before the start of the study. The calibration was performed on a separate group of 20 patients. They were not involved in intubating airways of patients, but only assessed the airway class using the MMT and the ULCT. In the MMT oropharyngeal view was assessed and classified as described by Samsoon and Young:[11] class I = soft palate, fauces, uvula and pillars seen; class II = soft palate, fauces and uvula seen; class III = soft palate and base of uvula seen; class IV = soft palate not visible. The examination was conducted while the patient was seated with the mouth wide open as far as possible and tongue fully protruded without any phonation. In assessing the ULCT class, patient was asked to roll over the lower lip over the upper lip as far as possible and the airway class determined according to the criteria proposed by Khan ZH et al.[9] as below:
Class zero (0): The lower lip gliding or rolling over the upper lip reaching as high as the columella or else positioning itself at any point above midway between the vermilion line and the columella: class I: The lower lip catching the upper lip, completely above the vermilion line fully covering and passing past the vermilion reaching a point midway between the vermilion and the columella; class II: The lower lip catches the upper lip at the level of the vermillion line or positioning itself just above it (2 mm); class III: The lower lip just caresses the upper lip, but falls short of obliterating the vermillion line [Figures 1 and 2].
Figure 1.
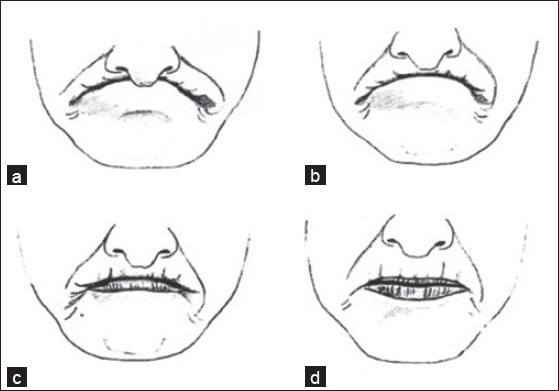
Schematic frontal view of the upper lip catch test. the patient is instructed to protrude his mandible as far as possible so that the lower lip can reach as far near the columella as permitted by mandibular protrusion (Reproduced from Khan et al. Evaluating a patient's airway [in Response]. Anesth Analg 2003;97:915-16 by permission. Copyright 2003 Lippincott Williams & Wilkins)
Figure 2.

Schematic lateral view of the upper lip catch test. Patient is instructed to protrude his mandible as far as possible so that the lower lip can reach as far near the columella as permitted by mandibular protrusion (Reproduced from Khan, et al. evaluating a patient's airway [in Response]. Anesth Analg 2003;97:915-16 by permission. Copyright 2003, Philadelphia, Lippincott Williams & Wilkins)
Anesthesiologists, blinded to the airway class, assessed difficulty of laryngoscopy and intubation, which was performed with patient anesthetized with the standard method and fully relaxed as assessed by an absence of twitch after applying a train-of-four on the operating table. With the patient's head in the sniffing position, laryngoscopy was performed with a Macintosh No. 3 blade or No. 4 if the mandibles appeared to be disproportionately large (Welch Allyn Inc., Skaneateles Falls, NY). If the initial attempt failed to provide a laryngoscopic view, a Miller laryngoscope blade (Welch Allyn) was employed along with external laryngeal pressure and adjustment of head position as the situation dictated. If the second attempt failed, a second Anesthesiologist performed the drill. In case of failure by the second Anesthesiologist, intubation was declared to be difficult and other maneuvers such as gum elastic bougies, video laryngoscope or fiber optic intubation was considered.
The laryngeal view was graded on the first laryngoscopy with Macintosh No. 3 blade according to the method proposed by Cormack and Lehane[12] as grade I: Full view of glottis; grade II: Glottis partly exposed, anterior commissure not seen; grade III: Only epiglottis seen; grade IV: Epiglottis not seen. While reporting the laryngeal view, no external pressure was applied. Grades I and II were considered to represent easy intubations and grades III and IV representing difficult intubations.
Assignment to the ULCT II and III and modified Mallampati class III or IV were earmarked as indicators of difficult intubation.
We used the CLG laryngoscopic view as our gold standard to calculate test parameters including true positive, false positive (FP), true negative, false negative (FN), sensitivity, specificity and accuracy for ULCT and modified Mallampati classification using a standard 2 × 2 table. The data were analyzed using the SPSS version 15 software (SPSS Inc., Chicago, IL, USA). A P value <0.05 was considered to be statistically significant.
RESULTS
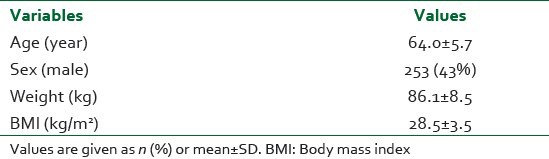
Participant demographics are presented [Table 1]. The mean age of the patients was 64 years (standard deviation = 5.7) and 253 (43%) patients were male.
Table 1.
Characteristics of patients
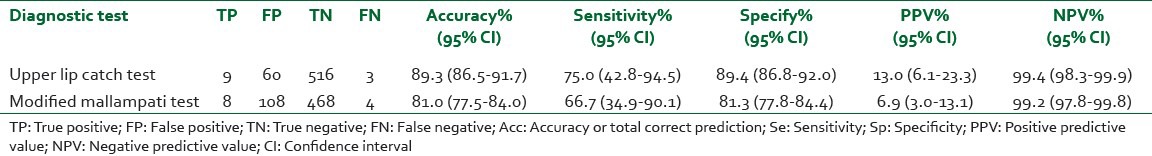
Out of 588 edentulous patients that were enrolled in this study, 12 (2%) of them were found at laryngoscopy to have airways exhibiting laryngoscopy grade III and IV [Table 2]. However, there were no failed intubations. Results for diagnostic test statistics for ULCT and MMT are being depicted [Table 3]. ULCT was 75.0% sensitive (95% confidence interval [CI], 42.8-94.5) and 89.4% specific (95% CI, 86.8-92.0) for laryngoscopy difficulty diagnosis. The sensitivity and specificity for MMT were 66.7% (95% CI, 34.9-90.1) and 81.3% (95% CI, 77.8-84.4), respectively. The accuracy rate was 89.3% for ULCT and 81.0% for MMT. So ULCT is more sensitive, specific and accurate than Mallampati test for laryngoscopy difficulty diagnosis. positive predictive value (PPV) was very low for both ULCT (13.0%) and MMT (6.9%) because of high FP diagnosis. However, negative predictive values (NPV) were very high for both tests (99.4% and 99.2% for ULCT and MMT respectively).
Table 2.
Relationship between the results of two predicting tests and laryngoscopy grades in patients
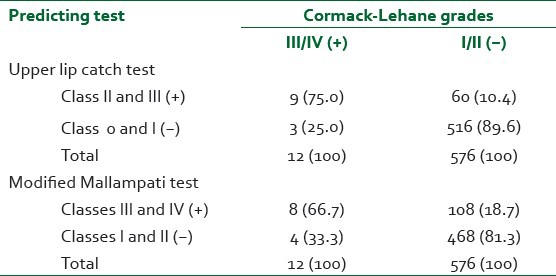
Table 3.
Diagnostic test statistics for upper lip catch test and modified mallampati test as predicting tests of laryngoscopy grades
DISCUSSION
Difficult laryngoscopic intubation is quite uncommon and none of the predictors when studied could reliably yield a high PPV for difficult laryngoscopic intubation.[13] Failure to intubate trachea ranges from 0.05% to 0.35%.[3] In our study, the incidence of difficult intubation was 2% and failure to intubate the trachea was not encountered.
A vacuum exists regarding airway assessment tests in edentulous patients and as such these patients are not subjected to routine preoperative airway assessment protocols. There is a commonly held belief that edentulous patients do not present much of a problem during the laryngoscopy and thus both laryngoscopy and intubation are relatively easy to perform in this set of patients. This assertion is perhaps based on the fact that the presence of teeth in itself may make laryngoscopy difficultly especially if the upper incisors are prominent or else resemble buck teeth. The assertion that edentulous patients are easy to intubate has not been clinically tested and there is no report in the literature documenting the ease of intubation in edentulous patients. To emphasize further, the teeth serve to be of mechanical advantage of leverage during clinical use of the Macintosh or the Miller blade. Thus, the teeth obviously help in supporting a static weight that is applied during the laryngoscopy and their absence as in edentulous patients would pose perhaps some problems. Moreover, the laryngeal structures descend caudally with the increase in age[14,15] and as the edentulous patients are in the old age group, their larynx is low (caudally positioned) and as the tongue, which is mostly contained in the oral cavity thus marking laryngoscopy difficult.
As there is no study in the literature to have evaluated airway assessment in edentulous patients, we sought to assess the potential value of ULCT as our primary goal in this category of patients based on the observations in our pilot study.[9] As most of the edentulous patients are in their old age, a smooth induction of anesthesia and rapid intubation will guarantee no insult to their precarious cardiovascular system, being more vulnerable to acute hemodynamic or heart rate fluctuations. Although a higher FP rate of a test pushes us toward a more cautious handling of the situation thereby helping us in preventing a poor outcome, nevertheless, a high rate of NPV gives us a margin of safety or in other words providing us reassurance of an easy intubation and thus helping us in eliminating cases of difficult intubation.
Bag mask ventilation had been difficult in some cases and it tallies and corroborates with the commonly held belief, which state a difficulty with bag mask ventilation.
Difficult laryngoscopy is a dreaded outcome following loss of consciousness and entails a host of complications; thus, the NPV becomes an important parameter in the evaluation of a test. It helps the Anesthesiologist to know with reasonable certainty that a high negative test allows him to safely anaesthetize the patient without the need for special airway equipment in the room. NPV of ULCT was 99.4% as against 99.2% for that of MMT. To elaborate it further, the chance of a difficult intubation with a negative ULCT is 0.6% versus 0.8% with a negative MMT. Although our primary intent was to test the predictive value of ULCT in edentulous patients and compare it with the gold standard the CLG scale, we also evaluated the MMT's role in detecting difficult intubation in edentulous patients never tested before as our secondary goal. The specificity of MMT was 81.3% in this study. The specificity of ULCT was 89.4%, which further documented that the ULCT had the potential to demarcate those edentulous patients who were subsequently found to have an easy intubation.
We could show that ULCT had a higher accuracy than MMT in the studied population resulting from its lower FP and FN values. In earlier studies, MMT's reliability has been questioned as the degree of prediction ranges widely.[16,17,18] Apparently, to the naïve observer it would appear that catching the upper lip with the lower one can be achieved without moving the mandible thus undermining the validity of the ULCT as an indicator of mandible subluxability. However, the idea in performing the ULCT is stressing on the patient to roll over his lower lip as high as possible over the upper lip so as to catch the columella and this maneuver cannot be achieved if there is a limitation in movement of the temporal mandibular joint (TMJ), thus underscoring the indispensable role and validity of ULCT as an indicator of mandible subluxability. Furthermore, although the lip being a soft-tissue can be easily moved out of the viewing axis during laryngoscopy, the magnitude of its catching and rolling over the upper lip in an effort to reach the columella involves the excursion of the TMJ and is totally inconceivable if there is no mandible subluxability. Immobility of the TMJ may restrict mouth opening and thus increase the ULCT class and the laryngoscopy grade. We however, assume that the ability of the patient to perform ULCT will not be affected if there is a limitation of head extension.
We feel that as the ULCT takes the TMJ and subluxation of the mandible into consideration for its optimal execution to evaluate the airway assessment, a good excursion at the TMJ coupled with subluxation of the mandible helps in achieving a lower score of ULCT thus confirming a wide opening of the mouth and easy glottic exposure owing to a large anterior laryngeal space. These characteristics of the ULCT make the test unique in assessing the airway and providing the observer with a definite clue in delineating cases in whom laryngoscopy and intubation would be easy.
A possible limitation of the study is that patients were not assessed for bag mask ventilation, which could have provided us added information in terms of bag mask ventilation. Furthermore, patients with fixed or partial prosthetic dentures were excluded. What would have been their impact on bag mask ventilation or laryngoscopy is hard to guess.
In conclusion, ULCT had higher accuracy and other diagnostic parameters were found to be comparably better enhancing its value than MMT as a predictor of airway assessment in edentulous patients. It could easily differentiate patients in whom laryngoscopy and intubation were easy owing to its high NPV and specificity. There are ample studies, which document human ethnic craniofacial variation and confirm significant racial variation in mandibular and maxillary morphology and morphometry.[19,20,21] Since this is the first study evaluating the role of ULCT in edentulous patients, its role as a predictive airway test need to be evaluated in different ethnic and racial groups to arrive at more concrete and tangible results to give coverage to this class of patients who are on the rise in our present world owing to the longevity of life span.
Footnotes
Source of Support: Tehran University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Benumof JL. Management of the difficult adult airway. With special emphasis on awake tracheal intubation. Anesthesiology. 1991;75:1087–110. doi: 10.1097/00000542-199112000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: A meta-analysis of bedside screening test performance. Anesthesiology. 2005;103:429–37. doi: 10.1097/00000542-200508000-00027. [DOI] [PubMed] [Google Scholar]
- 3.Tse JC, Rimm EB, Hussain A. Predicting difficult endotracheal intubation in surgical patients scheduled for general anesthesia: A prospective blind study. Anesth Analg. 1995;81:254–8. doi: 10.1097/00000539-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth. 1988;61:211–6. doi: 10.1093/bja/61.2.211. [DOI] [PubMed] [Google Scholar]
- 5.Khan ZH, Kashfi A, Ebrahimkhani E. A comparison of the upper lip bite test (a simple new technique) with modified Mallampati classification in predicting difficulty in endotracheal intubation: A prospective blinded study. Anesth Analg. 2003;96:595–9. doi: 10.1097/00000539-200302000-00053. [DOI] [PubMed] [Google Scholar]
- 6.Krobbuaban B, Diregpoke S, Kumkeaw S, Tanomsat M. The predictive value of the height ratio and thyromental distance: Four predictive tests for difficult laryngoscopy. Anesth Analg. 2005;101:1542–5. doi: 10.1213/01.ANE.0000181000.43971.1E. [DOI] [PubMed] [Google Scholar]
- 7.Eberhart LH, Arndt C, Cierpka T, Schwanekamp J, Wulf H, Putzke C. The reliability and validity of the upper lip bite test compared with the Mallampati classification to predict difficult laryngoscopy: An external prospective evaluation. Anesth Analg. 2005;101:284–9. doi: 10.1213/01.ANE.0000154535.33429.36. table of contents. [DOI] [PubMed] [Google Scholar]
- 8.Gupta S, Rajesh Sharma K, Jain D. Airway assessment: predictors of difficult airway. Indian J Anaesth. 2005;49:257. [Google Scholar]
- 9.Khan ZH, Kashfi A. Evaluating a patient's airway [In response] Anesth Analg. 2003;97:915–16. doi: 10.1213/01.ANE.0000074657.05733.30. [DOI] [PubMed] [Google Scholar]
- 10.Herschman Z. Evaluating a patient's airway[letter] Anesth Analg. 2003;97:915–6. doi: 10.1213/01.ANE.0000074657.05733.30. [DOI] [PubMed] [Google Scholar]
- 11.Samsoon GL, Young JR. Difficult tracheal intubation: A retrospective study. Anesthesia. 1987;42:487–90. doi: 10.1111/j.1365-2044.1987.tb04039.x. [DOI] [PubMed] [Google Scholar]
- 12.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anesthesia. 1984;39:1105–11. [PubMed] [Google Scholar]
- 13.Yentis SM. Predicting difficult intubation - Worthwhile exercise or pointless ritual? Anesthesia. 2002;57:105–9. doi: 10.1046/j.0003-2409.2001.02515.x. [DOI] [PubMed] [Google Scholar]
- 14.Chou HC, Wu TL. Large hypopharyngeal tongue: A shared anatomic abnormality for difficult mask ventilation, difficult intubation, and obstructive sleep apnea? Anesthesiology. 2001;94:936–7. doi: 10.1097/00000542-200105000-00043. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz DS, Keller MS. Maturational descent of the epiglottis. Arch Otolaryngol Head Neck Surg. 1997;123:627–8. doi: 10.1001/archotol.1997.01900060069012. [DOI] [PubMed] [Google Scholar]
- 16.Jacobsen J, Jensen E, Waldau T, Poulsen TD. Preoperative evaluation of intubation conditions in patients scheduled for elective surgery. Acta Anaesthesiol Scand. 1996;40:421–4. doi: 10.1111/j.1399-6576.1996.tb04463.x. [DOI] [PubMed] [Google Scholar]
- 17.Oates JD, Oates PD, Pearsall FJ, McLeod AD, Howie JC. Phonation affects Mallampati class. Anesthesia. 1990;45:984. doi: 10.1111/j.1365-2044.1990.tb14639.x. [DOI] [PubMed] [Google Scholar]
- 18.Wilson ME, John R. Problems with the Mallampati sign. Anesthesia. 1990;45:486–7. doi: 10.1111/j.1365-2044.1990.tb14342.x. [DOI] [PubMed] [Google Scholar]
- 19.Badawi-Fayad J, Cabanis EA. Three-dimensional Procrustes analysis of modern human craniofacial form. Anat Rec (Hoboken) 2007;290:268–76. doi: 10.1002/ar.20442. [DOI] [PubMed] [Google Scholar]
- 20.Hanihara T, Ishida H, Dodo Y. Characterization of biological diversity through analysis of discrete cranial traits. Am J Phys Anthropol. 2003;121:241–51. doi: 10.1002/ajpa.10233. [DOI] [PubMed] [Google Scholar]
- 21.Perez SI, Bernal V, Gonzalez PN. Differences between sliding semi-landmark methods in geometric morphometrics, with an application to human craniofacial and dental variation. J Anat. 2006;208:769–84. doi: 10.1111/j.1469-7580.2006.00576.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


