Abstract
Background:
The incidence of pain reported in literature after IV administration of rocuronium is 50-80%. The aim of our study was to determine whether pre-treatment with intravenous granisetron and nitroglycerine would reduce rocuronium-induced pain.
Methods:
One hundred fifty patients of either sex, aged 18-65 years, American society of Anaesthesiologist grading (ASA) I-II, scheduled for various surgeries under general anesthesia were randomly assigned to one of the groups. Group G: received 2 granisetron (1mg/ml) diluted with 3 ml of 0.9% normal saline) while the Group C: received 5 ml of 0.9% normal saline. Group N: received 200΅g of nitroglycerine diluted to a total of 5 ml(with 0.9% normal saline). It was accompanied by manual venous occlusion for 20 seconds. Then 0.06mg/kg of rocuronium was injected through same cannula over 10-15 sec. Patients were asked by a blinded investigator to score the pain on injection of rocuronium using visual analogue scale (0-10) with 0-no pain,1-3 mild pain, 4-6 moderate and >=7 severe pain. At the same time discomfort in the form of patient's movement, such as no movement (grade 0), movement only wrist (grade 1), movement to the upper arm and shoulder of injected arm (grade 2) or generalized movements (grade3) was observed. Statistical analysis using independent t test, Mann-Whitney test and reverse ANOVA was done.
Results:
1. At 0 seconds, in group G number of patients who experienced withdrawl score of 0-1 were 92%,group N were 82% while only 26% of patients in group C had favourable withdrawl score.74% of patients in group C had score of 2-3 at same time. 2. At 0 sec, in group G number of patients who experienced VAS score of 0-3 were 96%, group N 72%. At same time Group C 48 % of patients had VAS score of 2-3.
Conclusion:
We conclude that pre-treatment with granisetron or nitroglycerine both are highly effective in attenuation of rocuronium induced pain.
Keywords: Granisetron, nitroglycerine, pain, rocuronium
INTRODUCTION
Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage.[1] It is now considered as the fifth vital sign. It is believed that pain is inevitable but suffering is optional.
Rocuronium an aminosteroidal nondepolarizing muscle relaxant has replaced suxamethonium in all most all modern day operating suites.[2,3] There are several reports of burning pain from injection of aminosteroidal nondepolarizing muscle relaxants such as rocuronium that can be severe and distressing. The incidence of pain reported in the literature after IV administration of rocuronium is 50-80%.[4] A sudden withdrawal of upper limb has been noted in patients after induction. A variety of pre-treatment drugs like fentanyl, lignocaine, tramadol, sodium bicarbonate, magnesium have been administered and proved to decrease rocuronium pain.[5,6]
Granisetron is an antiemetic drug introduced into practice. Its pro drug ondansetron has demonstrated a local analgesic property.[7] A study conducted on rats has proved that ondansetron blocks sodium channels in rat brain neurons; it can be used as an analgesic. Nitroglycerine (NTG) causes an increase in concentration of cyclic guanosine monophosphate, which induces pain modulation in central and peripheral nervous systems.[8]
The primary aim of the present study was to do a subjective analysis and measure the intensity of pain in awake patients, just before induction by using sub-anesthetic doses of rocuronium. We compared granisetron, NTG, and placebo group for attenuation of rocuronium injection pain.
METHODS
After approval of hospital research and ethical committee, an informed consent was taken from patients. The study was conducted on 150 patients from ASA I-II, aged 18-65 years scheduled for various surgeries under general anesthesia. Exclusion criteria included ASA III-V, age <18 >65 years, allergic to any of the study drug, patients with any cardiovascular, neurological and respiratory comorbid conditions, vascular disease, and weak thin dorsal veins.
Patients were randomized according to computer-generated numbers placed in a sealed opaque envelope. Drugs were prepared in identical syringes according to the list by the same anesthesiologist who was not involved in the analysis of the study. Group G: received 2 mg granisetron (1 mg/ml) diluted with 3 ml of 0.9% normal saline to a total of 5 ml, Group N: received 200 μg of NTG diluted to a total of 5 ml (with 0.9% normal saline) and Group C: received 5 ml of 0.9% normal saline at ambient operating room temperature (20-22°C)
Patients were informed that they would receive a drug at the beginning of their anesthesia that might cause a burning pain in their arm. They were told that they would be asked to score the severity of pain, if any occurred, after the drug had been injected. The patients were also informed that they could experience side effects such as heavy eye lids, blurred vision, or difficulty in swallowing and breathing after injection of the drug. They instructed to report if any side effects occurred.
The unpremedicated patients were then taken to operating room, a 18-gauge catheter inserted in the dorsum of right hand. Patients were given ringer lactate 100 ml/hour and the mean arterial pressure, SpO2, electrocardiograph, end tidal carbon dioxide, urine output, and heart rate will be monitored. With the aim of keeping the drug within the vein, the forearm was squeezed manually for 20 seconds. The occlusion was released after 20 seconds and a sub-anesthetic dose of 0.06 mg/kg of rocuronium was injected through the same cannula over a period of 10-15 seconds. Patients were asked by a blinded investigator to score the pain on injection immediately, at 5 seconds, at 10 seconds, at 15 seconds, and at 20 seconds using the following criteria.[9,10,11]
Withdrawal score was taken as 0-No discomfort reported; negative response to questioning, 1-withdrawl of wrist, 2-movement of upper arm and shoulder of injected arm, 3-generalized movement of whole upper limb, and VAS was interpreted as 0= no pain, 1-3 = mild pain, 4-6= moderate pain, and ≥7 as severe pain.
Because the administration of intravenous rocuronium may cause unpleasant effects, an IV hypnotic drug in the form of injection fentanyl (2 μg/kg) was given immediately thereafter and anesthesia proceeded as planned. Any complications in the form of venous induration, residual pain, edema, wheal or flare response at the site of injection were noted for period of 24 hours. Also, any choking sensation, blurring of vision, difficulty in swallowing, or light headedness at any time from start of the study till 24 hours postoperatively was noted.
For this pilot project, we reviewed previous studies and found that 50 patients in each group to a total of 150 patients would be appropriate. Statistical analysis was done using an independent t test for demographic data, Mann-Whitney test for withdrawal, and VAS score and reverse ANOVA for heart rate. A P value of <0.05 was taken as significant values.
RESULTS
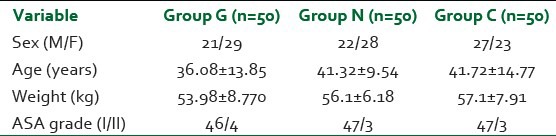
No significant differences were observed in terms of demographic criteria [Table 1].
Table 1.
Patient's characteristics values are mean (SD) where appropriate
At 0 seconds, in Group G 92%, Group N 82% of patients had withdrawal scores of 0-1, while only 26% of patients in Group C had favorable withdrawal score of 0-1. 74% of Group C patients experienced moderate to severe discomfort (score 2-3) at the same time. At 5 seconds, in Group G 92% and in Group N 98% of patients had no to mild discomfort. (0-1) On the other hand, at the same time, as many as 70% of Group C patients still had severe discomfort (2-3). Similar results were seen at 10, 15, and 20 seconds with a statistical significance observed both within the groups at various intervals and between the three groups (P < 0.00) [Figure 1].
Figure 1.
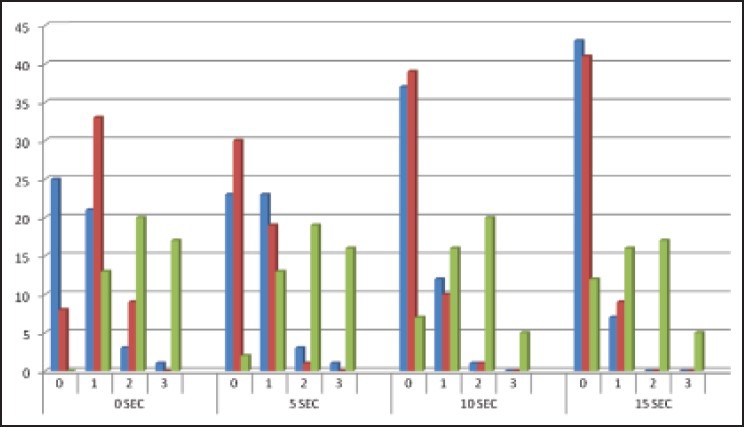
Withdrawl score of various groups at different time intervals
For VAS scores, at 0 seconds 96% of Group G and 72% of Group N patients had no to mild pain (VAS 0-3), while as many as 48% of Group C had moderate to severe pain (VAS 4-10). Similar results were seen at 10, 15, and 20 seconds with 44%, 40%, and 26% of Group C patients having pain, respectively (VAS 4-10). On the other hand, 100% of Group G, 95-98% of Group N had no to mild pain at same time intervals (VAS 0-3, P < 0.00). Also, the number of patients in Group C, having pain decreased with time [Figure 2].
Figure 2.
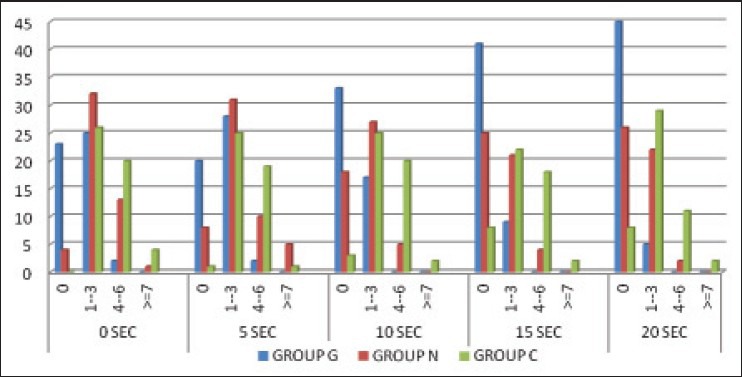
VAS score of various groups at different time intervals
No statistical significance was found in hemodynamic data in between the three groups. Twenty-four hours later, there was no venous induration, residual pain, edema, wheal, or flare response at the site of injection. At the end of surgical procedure, patients recalled of pain but no patient had any memory of respiratory difficulty. No side effects like choking sensation, blurring of vision, difficulty in swallowing, or light headedness was reported just after injection or within 24 hours postoperatively. Clinically significant hypotension was observed in 5/50 patients in the NTG group.
DISCUSSION
n the present day anesthesia regimen suxamethonium has been replaced by rocuronium. A vast array of side effects and complications of suxamethonium have been studied and proved time and again.[2,3] Rocuronium has emerged as a muscle relaxant of choice for all routine procedures. It has gradually replaced suxamethonium even in scenarios where rapid sequence induction is required.[12]
Rocuronium pain with an incident of 50-80% has been proved to be distressing and unwanted. Even the subject anaesthetized with induction agent may experience intense burning pain along with sudden flexion of wrist and arm lasting for 20 seconds after injection of rocuronium.[13] Pain caused by this drug has been linked to endothelial irritation, osmolality difference, unphysiological pH, and activation of pain mediators.[14] Release of various neurotransmitters like bradykinin, serotonin, and histamine has been postulated to cause local vasodilatation and hyperpermeability.[5,15]
Granisetron is a 5HT3 receptor antagonist and is more efficacious with longer duration of action. It has almost similar pharmacological properties to ondansetron. Ondansetron is routinely administered as premedication for postoperative nausea and vomiting in patients following general anesthesia. It has been shown to relieve pain by sodium channel blocking and μ opioid agonist property. Its 5HT3 receptor-blocking property is also involved in inhibiting the nociceptive pathway and causing preemptive analgesia[7,16] Ambesh et al administered 2 ml (4 mg) of ondansetron to successfully prevent injection pain.[9] Reddy et al found that pain from rocuronium and propofol was significantly reduced in the ondansetron (4 mg) and lignocaine (50 mg) groups compared with placebo and that pain was significantly less with lidocaine than with ondansetron.[17] So this study was designed to ascertain whether pretreatment with granisetron could alleviate pain produced by rocuronium injection.
NTG is a nitric oxide (NO) generator which causes peripheral vasodilatation. NO derived from NTG causes an increase in the concentration of cyclic guanosine monophosphate, which induces pain modulation in central and peripheral nervous system.[8,18] NO can also induce an antinociceptive effect through direct stimulation of peripheral fibers mimicking the action of locally applied acetylcholine.[8] NTG 200 μg added to lidocaine for intravenous regional anesthesia (IVRA) was reported to improve sensory and motor block, tourniquet pain, and postoperative analgesia, without side effects.[19] Therefore, NTG 200 μg was chosen for the present study.
Venous retention with a tourniquet is a technique often used for pretreatment of propofol injection pain.[15,20,21] Occlusion with a tourniquet was also used by Memis et al who used it for rocuronium pain.[22] The venous occlusion technique is suitable for studying the peripheral action of pretreatment drugs with local anesthetic property such as lidocaine, ondansetron, or tramadol but is not useful for drugs that are postulated to act centrally such as morphine or fentanyl, as it prevents the delivery of drugs to the effect sites.[22,23] Total duration of venous occlusion is also a factor influencing the analgesic potency of study drug, especially with a peripheral mechanism of action. Similarly, in drugs like opioid with a central mode of action, timing of administration of pretreatment drug plays important role.[22,24] We used the standard method of manual occlusion of vein on dorsum of hand for 20 seconds, prior to administration of rocuronium.
The grading of pain done in previous studies is VAS or other pain scores in the form of discomfort felt by patient.[9,10,11] We used both VAS and withdrawal scores. These were judged at 0, 5, 10, 15, and 20 seconds. VAS gave a more subjective analysis and withdrawal score an expert observation by a blinded anesthesiologist. By doing a comparative analysis at various time intervals, the intensity of pain could be graded more precisely.
Various pretreatment methods and drugs have been used in the past. Tunale et al used various dilutions of rocuronium (10 mg/kg, 1 mg/kg, and 0.5 mg/kg) and studied pain reported by patient. They found that percentage of patients with pain decreased from 80% (10 mg/kg) to 38% (1 mg/kg) which further reduced to 0% (0.5 mg/kg) in awake patients.[25] Chiarella et al mixed 10 mg rocuronium with sodium bicarbonate (8.4%) 2 ml, fentanyl 100 μg, lidocaine 2%, or normal saline. They concluded that sodium bicarbonate reduced pain by 18.4 times, followed by 3.6 times by lidocaine and 1.9 times by fentanyl.[26] Spontaneous movements associated with rocuronium have been reported in the past. Borgeat et al compared group I (10 mg of rocuronium) with group II (2 successive doses of 10 mg at 30 seconds interval) and group III (1 ml 0.9% NS). They concluded that the first group had sudden flexion of elbow and wrist, while the third group had no pain at all. The second group had markedly decreased pain intensity.[15] Jeon et al used a combination of NTG 0.1 μg/kg and lidocaine 20 mg for attenuation of propofol pain. They summed up that this combination is more effective than lidocaine used alone as a preemptive analgesic.[7]
Our results demonstrated an unacceptable high incidence of pain or discomfort with rocuronium, which decreased significantly with pretreatment with granisetron and NTG. Granisetron was found to be more effective than NTG as a preemptive analgesic. Patients in the control group had severe pain along with sudden withdrawal of upper limb. Our results showed that rocuronium caused moderate to severe pain in 48% of patients which decreased to 26% by 20 seconds. Patients who received injection granisetron, only 4% had moderate to severe pain at beginning which decreased to 0% after 10 seconds and thereafter. Similarly, in the NTG group as many as 28% of patients had moderate to severe pain which decreased to 2-5% after 20 seconds. Thus, both granisetron and NTG markedly decreased the intensity of pain caused by rocuronium. Also, pain caused by rocuronium decreased over the period of time.
CONCLUSION
Rocuronium causes pain even when given after induction in the form of withdrawal movements. So steps should be taken to alleviate pain. Granisetron and NTG both decrease this pain with former (2 mg) being more efficacious than the latter (200 μg).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.International Association for the Study of Pain: Pain Definitions; Derived from Bonica JJ. The need of a taxonomy. Pain. 1979;6:247–8. [Google Scholar]
- 2.Singh A, Bhatia PK, Tulsiana KL. Comparison of onset time intubating conditions achieved with suxamethonium and rocuronium. Indian J Anaesth. 2004;48:129–33. [Google Scholar]
- 3.Durant NN, Katz RL. Suxamethonium. Br J Anaesth. 1982;54:195–208. doi: 10.1093/bja/54.2.195. [DOI] [PubMed] [Google Scholar]
- 4.Steegers MA, Robertson EN. Pain on injection of rocuronium bromide. Anesth Analg. 1996;83:193–205. doi: 10.1097/00000539-199607000-00065. [DOI] [PubMed] [Google Scholar]
- 5.Lockey D, Coleman P. Pain during injection of rocuronium bromide. Anesthesia. 1995;50:474. doi: 10.1111/j.1365-2044.1995.tb06019.x. [DOI] [PubMed] [Google Scholar]
- 6.Moorthy SS, Dierdorf SF. Pain on injection of rocuronium bromide. Anesth Analg. 1995;80:1067. doi: 10.1097/00000539-199505000-00057. [DOI] [PubMed] [Google Scholar]
- 7.Ye JH, Mui WC, Ren J, Hunt TE, Wu WH, Zbuzek VK. Ondansetron exhibits the properties of a local anesthetic. Anesth Analg. 1997;85:1116–21. doi: 10.1097/00000539-199711000-00029. [DOI] [PubMed] [Google Scholar]
- 8.Duarte ID, Lorenzetti BB, Ferreira SH. Acetylcholine induces peripheral analgesia by the release of nitric oxide from l-arginine. In: Moncada S, Higgs EA, editors. A bioregulatory system. Amsterdam: Elsevier; 1990. pp. 165–70. [Google Scholar]
- 9.Ambesh SP, Dubey PK, Sinha PK. Ondansetron pretreatment to alleviate pain on propofol injection: A randomized, controlled, double-blinded study. Anesth Analg. 1999;89:197–9. doi: 10.1097/00000539-199907000-00035. [DOI] [PubMed] [Google Scholar]
- 10.McCrirrick A, Hunter S. Pain on injection of propofol: The effect of injectate temperature. Anesthesia. 1990;45:443–4. doi: 10.1111/j.1365-2044.1990.tb14329.x. [DOI] [PubMed] [Google Scholar]
- 11.Agarwal A, Ansari MF, Gupta D, Pandey R, Raza M, Singh PK, et al. Pretreatment with thiopental for prevention of pain associated with propofol injection. Anesth Analg. 2004;98:683–6. doi: 10.1213/01.ane.0000103266.73568.18. [DOI] [PubMed] [Google Scholar]
- 12.Marsch SC, Steiner L, Bucher E, Pargger H, Schumann M, Aebi T, et al. Suxamethonium versus rocuronium for rapid sequence induction in intensive care. Crit Care. 2011;15:R199. doi: 10.1186/cc10367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joshi GP, Whitten CW. Pain on injection of rocuronium bromide. Anesth Analg. 1997;84:228–36. doi: 10.1097/00000539-199701000-00044. [DOI] [PubMed] [Google Scholar]
- 14.Klement W, Arndt JO. Pain on intravenous injection of some anesthetic agents is evoked by the unphysiological osmolality or pH of their formulations. Br J Anaesth. 1991;66:189–95. doi: 10.1093/bja/66.2.189. [DOI] [PubMed] [Google Scholar]
- 15.Borgeat A, Kwiatkowski D. Spontaneous movements associated with rocuronium: Is pain on injection the cause? Br J Anaesth. 1997;79:382–3. doi: 10.1093/bja/79.3.382. [DOI] [PubMed] [Google Scholar]
- 16.Gregory RE, Ettinger DS. 5-HT3 receptor antagonists for the prevention chemotherapy-induced nausea and vomiting: A comparison of their pharmacology and clinical efficacy. Drugs. 1998;55:173–89. doi: 10.2165/00003495-199855020-00002. [DOI] [PubMed] [Google Scholar]
- 17.Reddy MS, Chen FG, Ng HP. Effect of ondansetron pretreatment on pain after rocuronium and propofol injection: A randomised, double-blind controlled comparison with lidocaine. Anesthesia. 2001;56:902–5. doi: 10.1046/j.1365-2044.2001.02059-6.x. [DOI] [PubMed] [Google Scholar]
- 18.Zhuo M, Meller ST, Gebhart GF. Endogenous nitric oxide is required for tonic cholinergic inhibition of mechanical transmission. Pain. 1993;54:71–8. doi: 10.1016/0304-3959(93)90101-T. [DOI] [PubMed] [Google Scholar]
- 19.Abbasivash R, Hassani E, Aghdashi MM. The effect of nitroglycerine as an adjuvant to lidocaine in intravenous regional anesthesia. Middle East J Anaesthesiol. 2009;20:2. [PubMed] [Google Scholar]
- 20.Pang WW, Huang S, Chung YT, Chang DP, Lin SS, Hong MH. Comparison of intravenous retention of fentanyl and lidocaine on local analgesia in propofol injection pain. Acta Anaesthesiol Sin. 1997;35:217–21. [PubMed] [Google Scholar]
- 21.Pang WW, Mok MS, Huang S, Hwang MH. The analgesic effect of fentanyl, morphine, meperidine, and lidocaine in the peripheral veins: A comparative study. Anesth Analg. 1998;86:382–6. doi: 10.1097/00000539-199802000-00031. [DOI] [PubMed] [Google Scholar]
- 22.Memis D, Turan A, Karamanhoglu B, Süt N, Pamukçu Z. The prevention of pain from injection of rocuronium by ondansetron, lidocaine, tramadol and fentanyl. Anesth Analg. 2002;94:1517–20. doi: 10.1097/00000539-200206000-00026. [DOI] [PubMed] [Google Scholar]
- 23.Shevchenko Y, Jocson JC, McRae VA, Stayer SA, Schwartz RE, Rehman M, et al. The use of lidocaine for preventing the withdrawal associated with the injection of rocuronium in children and adolescents. Anesth Analg. 1999;88:746–8. doi: 10.1097/00000539-199904000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Ahmad N, Choy CY, Balan S. Preventing the withdrawal response associated with rocuronium injection: A comparison of fentanyl with lidocaine. Anesth Anaig. 2005;100:987–90. doi: 10.1213/01.ANE.0000147790.76114.3A. [DOI] [PubMed] [Google Scholar]
- 25.Tuncali B, Karci A, Tuncali BE, Mavioglu O, Olguner CG, Ayhan S, et al. Dilution of rocuronium to 0.5% mg/ml with 0.9% NaCl eliminates the pain during intravenous injection in awake patients. Anesth Analg. 2004;99:740–3. doi: 10.1213/01.ANE.0000130005.94395.B2. [DOI] [PubMed] [Google Scholar]
- 26.Chiarella AB, Jolly DT, Huston CM, CLanachan AS. Comparison of four strategies to reduce the pain associated with intravenous administration of rocuronium. Br J Anaesth. 2003;90:377–9. doi: 10.1093/bja/aeg054. [DOI] [PubMed] [Google Scholar]


