Abstract
Clonidine, an alpha-2 adrenergic receptor agonist, has well-established role in acute perioperative pain management. However, recently it has found increasing use in chronic pain conditions as well. In this review, we systematically searched and analyzed the clinical studies from “PubMed,” “PubMed central” and “Scopus” database for use of clonidine in the chronic pain. Quantitative meta-analysis was not possible as clonidine has been used in various patient populations through different routes. However, qualitative analysis of nearly thirty clinical studies provides some evidence that clonidine administered through epidural, intrathecal and local/topical route may be effective in chronic pain conditions where neuropathy is a predominant component. It may also be effective where opioids are of limited use due to inadequate pain relief or adverse effects.
Keywords: Chronic pain, clonidine, neuropathy
INTRODUCTION
Clonidine, the first congener of alpha-2 adrenergic receptor agonist, is mainly used as antihypertensive in the clinical medicine.[1] However, it has also been used for drug detoxification,[2] pain relief and sedation.[3,4] The role of systemic[5] and intrathecal[6] clonidine in acute post-operative pain has recently been well-established. However, there is an increasing evidences from animal[7] and the human studies[8,9] that clonidine may be effective in the prevention and management of chronic pain as well. Chronic pain is continuous, long-term pain of more than 12 weeks or after the time when healing would have been thought to have occurred in pain after trauma or surgery.[10] It includes, but not limited to complex regional pain syndrome, neuropathic pain, trigger points/myofascial pain, osteoarthritis, chronic persistent pain and chronic non-specific pain syndrome. However, the results of the clinical studies on the effect of clonidine in chronic pain have not been systematically reviewed so far. In this brief systematic review, role of clonidine administered through various routes in prevention and management of chronic painful conditions has been analyzed.
METHODS
All the authors independently did an electronic search with the keywords: “clonidine” and “chronic pain” in the PubMed, PubMed Central and Scopus on 3rd April, 2013. The PubMed search strategy has been mentioned in Appendix 1. We manually searched for the published human clinical trials and case series where clonidine has been used as sole agent or along with other drugs for prophylaxis or management of chronic pain. A quantitative meta-analysis was not possible on this topic as clonidine has been used in different patient population through different routes.
RESULTS
A total of 30 clinical trials were found in initial electronic data base search. Most of the clinical trials have used intrathecal clonidine with or without other drugs for prevention or management of chronic pain. Some studies have used epidural or other routes of drug administration.
Intrathecal clonidine
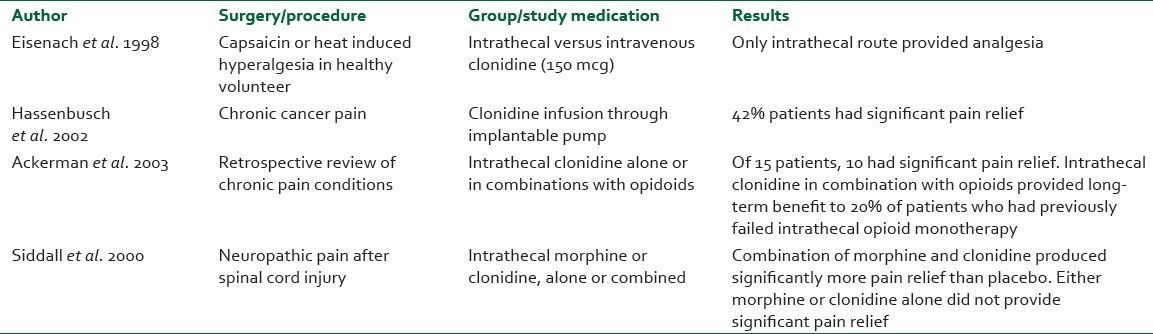
Eisenach et al.[11] in 1998 found that intrathecal clonidine at a dose of 150 mcg may reduce capsaicin or heat induced hyperalgesia in normal healthy volunteers and intravenous clonidine is ineffective in this regard.
Hassenbusch et al.[12] in 2002 studied the effects of infusion of intrathecal clonidine through an implantable pump in chronic cancer pain patients whose pain was not relieved by oral opioids. They found that 13 patients (42%) were considered long-term successes with a mean follow-up of 16.7 months (range = 6.3-44 months). Nine patients failed to achieve adequate pain relief due to side-effects or lack of efficacy.
Ackerman et al.[13] did a retrospective chart review of 15 patients where intrathecal clonidine alone or in combinations with other opioid was used in a variety of chronic pain patients. All patients received trial of single-shot with or without short-term infusion of clonidine. They found that 10 of 15 patients reported a significant pain relief (>50% decrease in visual analog scale (VAS) scores) with the initial trial and received long-term therapy. Initially 70% patients responded to clonidine alone (75-950 μg/day) before requiring a second drug. Intrathecal clonidine in combination with intrathecal opioids provided long-term benefit lasting up to 24 months in 20% of patients who had previously failed intrathecal opioid monotherapy.
Siddall et al.[14] concluded that intrathecal administration of a combination of 0.2-1 mg of morphine and 50-100 mcg of clonidine is more effective than either drug administered alone in the treatment of neuropathic pain after spinal cord injury.
Rudich et al.[15] concluded that clonidine, when mixed with hydromorphone, is stable and can be delivered by implantable intrathecal pump for long-term use. Ruan et al.[16] reported a case where clonidine 67 mcg/day with baclofen 100 mcg/day was used in a patient of failed back surgery syndrome resulting in significant improvement of back and leg pain (2-4/10 on VAS), which did not initially resolve with morphine. Table 1 summarizes the findings of the above mentioned studies.
Table 1.
Intrathecal clonidine in chronic pain conditions
Epidural clonidine
Glynn et al.[8] in 1988 first reported the use of epidural clonidine for the management of chronic low back pain, arachnoiditis and surgical scar pain. They found that clonidine at a dose of 150 mcg provides similar pain relief to 5 mg morphine with a much longer duration (6 h-1 month in clonidine vs. 6-24 h in morphine). However, it was a small study with only 20 patients and all patients had a significant hypotension and sedation. Epidural clonidine, at a dose of 300 mcg and 700 mcg bolus followed by long-term epidural infusion may be useful for refractory reflex sympathetic dystrophy. It caused similar pain relief, hypotension and bradycardia in either dosage; however, sedation was more with higher dosage.[9] Subsequently in 1996 Glynn et al.[17] in a double-blind crossover trial studied the effect of lumbar epidural clonidine 150 mcg, lignocaine 40 mg and the combination of clonidine 150 mcg and lignocaine 40 mg in 20 patients with the chronic pain who previously had obtained analgesia from epidural clonidine and lignocaine. The author found a significant difference between lignocaine and lignocaine-clonidine combinations. They concluded epidural clonidine had a supra-additive effect and behaved more like a co-analgesic than a pure analgesic.
However, whether epidural clonidine does actually have any added advantage over intravenous route was questioned by Carroll et al.[18] They found that intravenous clonidine produced significantly greater analgesia than epidural clonidine and both the routes were associated with significant side-effects. In a phase I trial,[19] it was found that epidural clonidine provides pain relief in intractable cancer pain for up to 6 h with an acceptable side-effect profile. Following this study, seven patients from the study population received long-term clonidine-morphine home infusion that provided pain relief for up to 5 months. Eisenach et al.[20] in 1995 reported that epidural clonidine may provide pain relief in intractable cancer pain patients particularly those who have neuropathic pain.
Lavand’homme and De Kock evaluated the modulatory effect of intraoperative neuraxial analgesia on objective changes (i.e., mechanical hyperalgesia) reflecting central sensitization. They found that epidural or intrathecal clonidine added to local anesthetic may also prevent the development of chronic post-surgical pain and hyperalgesia after major abdominal surgery.[21] Gabriella et al.[22] compared the efficacy of epidural clonidine with ketamine in chronic neuropathic pain patients. They reported similar efficacy of epidural clonidine and ketamine in chronic cancer pain and epidural administration of ketamine or clonidine in combination with 1% lignocaine resulted in analgesia during the epidural catheter maintenance (initial VAS 8-10 cm vs. final VAS 0-3 cm; P < 0.002). VAS scores remained maintained between 0 cm and 3 cm from 2 to 5 weeks following epidural catheter removal. Recently, Ayad and El Masry[23] in a pilot study reported that a combination of epidural steroid and clonidine may provide pain relief in chronic post-thoracotomy pain. The findings of afore mentioned studies have been summarized in Table 2.
Table 2.
Epidural clonidine in chronic pain
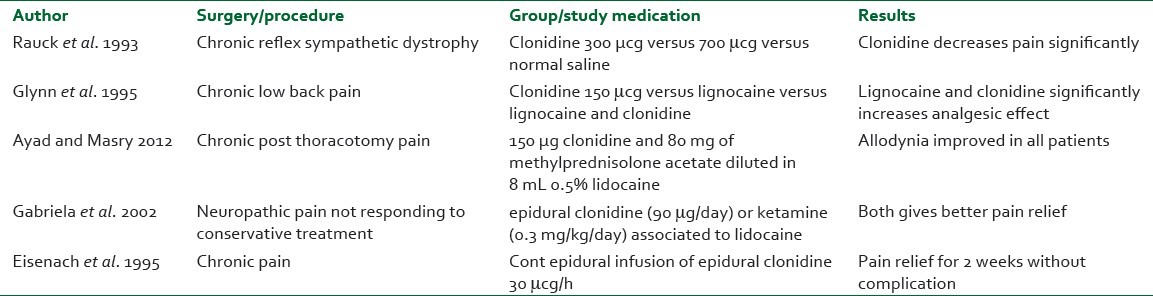
All studies reported that hypotension is the most common and at times serious side-effect of epidural clonidine. However, in most of the cases, hypotension was managed by fluid administration and only a few required vasopressor. Dose related bradycardia and sedation may also be associated with the epidural clonidine.
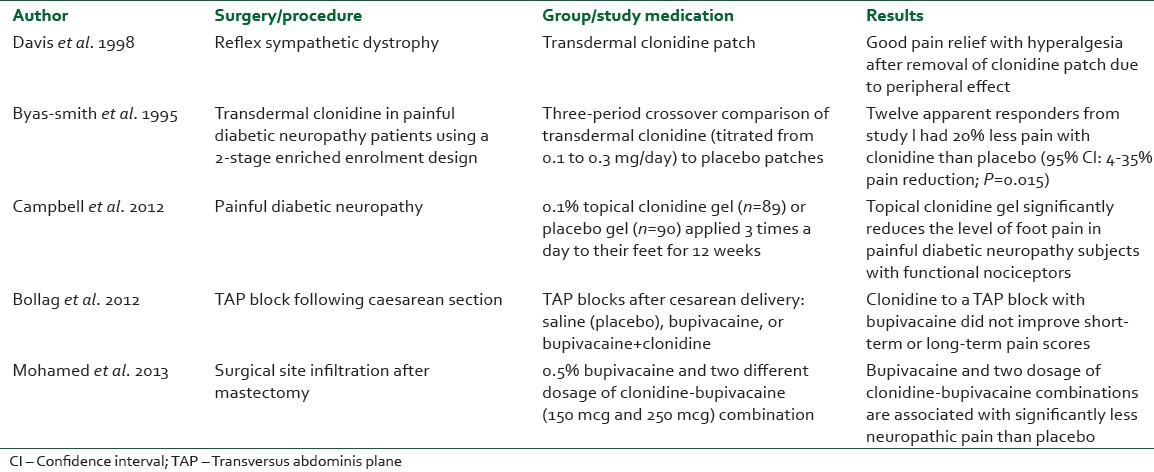
Clonidine: Other routes of administration
Topical application (i.e., clonidine patch) has been the most studied mode of delivery other than neuraxial route. Neuropathic peripheral nerves generate ectopic impulses, which are sensitive to adrenergic agonist. These nerve terminals are inhibited from releasing norepinephrine upon adrenergic agonist binding.[24]
Davis et al.[25] showed that use of clonidine patch delivering 30 mcg/cm2/day, either 7 cm2 or 10.5 cm2 in size for 7 days gives a good pain relief with hyperalgesia after removal of the patch. Byas-Smith[26] showed that use of clonidine patch gives a significant pain relief in patients of diabetic neuropathy. Campbell et al.[27] did a randomized, double-blind, placebo-controlled, parallel-group, multicenter trial on 182 patients. They used 0.1% topical clonidine to a maximum of 3.9 mg/day in patients who were suffering from diabetic neuropathy. This study concluded that topical clonidine gel significantly reduced pain intensity in subjects with diabetic neuropathy in whom there are functional (and possibly sensitized) nociceptors in the affected skin. Bollag et al. in 2102 found that clonidine added to bupivacaine in transversus abdominis plane (TAP) block is ineffective in preventing long-term pain in women following a cesarean section.[28] However, the authors themselves mentioned that the dosage of clonidine (75 mcg/site) they used may be insufficient for TAP block. Recently, 0.5% bupivacaine in combination with two different dosages of clonidine (150 mcg and 250 mcg) have been used in surgical site infiltration following mastectomy to delineate their effects on chronic neuropathic pain.[29] The authors found that two dosage of clonidine-bupivacaine combination was associated with significantly less neuropathic pain than placebo. However, there is no difference among the study groups. These findings have been summarized in Table 3.
Table 3.
Local and topical clonidine in chronic pain
DISCUSSION
Clonidine has been used in various routes in different cancer and non-cancer painful conditions with varying degree of success. Intrathecal clonidine has been found to be effective in both cancer and non-cancer pain. Long-term use of intrathecal clonidine is also reported with the use of an implantable pump. One study reported that a combination of clonidine and morphine is superior to either drug alone in post-spinal cord injury related pain.
In epidural route, clonidine has been used in a wide range of dosage ranging from 90 mcg to 700 mcg. It has been found to be effective in reflex sympathetic dystrophy, chronic low back pain, post-thoracotomy pain and neuropathic pain not responding to conventional management. It may have a role in prevention of the chronic post-surgical pain when used along with local anesthetics.
Transdermal clonidine patch and topical clonidine gel has been used with good success rate in painful diabetic neuropathy. Surgical site infiltration with bupivacaine clonidine combination is recently found to be effective in preventing chronic pain following mastectomy, but found to be ineffective when used in TAP block flowing cesarean section.
CONCLUSION
There are some clinical evidence, which support the notion that clonidine may be effective in chronic painful conditions particularly where neuropathy is a significant component such as chronic post-surgical pain due to nerve entrapment, post radiation neuropathy etc. It may also be effective where opioids are of limited use due to inadequate pain relief or adverse effects. However, large well-designed randomized controlled trials are required to firmly establish its role in chronic pain. However, conducting clinical trials in chronic pain states is difficult because, chronic pain is multifactorial and contribution of each factor may be different in different population. Hence, targeting a single factor may not result in significant pain relief in a study group. Until such trials are available, we can only recommend clonidine in very selective patients where neuropathy may be a significant component.
Appendix 1
(“clonidine”[MeSH Terms] OR “clonidine”[All Fields]) AND (“chronic pain”[MeSH Terms] OR (“chronic”[All Fields] AND “pain”[All Fields]) OR “chronic pain”[All Fields]).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ferder L, Inserra F, Medina F. Safety aspects of long-term antihypertensive therapy (10 years) with clonidine. J Cardiovasc Pharmacol. 1987;10(Suppl 12):S104–8. [PubMed] [Google Scholar]
- 2.Gold MS, Redmond DE, Jr, Kleber HD. Clonidine blocks acute opiate-withdrawal symptoms. Lancet. 1978;2:599–602. doi: 10.1016/s0140-6736(78)92823-4. [DOI] [PubMed] [Google Scholar]
- 3.Maze M, Tranquilli W. Alpha-2 adrenoceptor agonists: Defining the role in clinical anesthesia. Anesthesiology. 1991;74:581–605. [PubMed] [Google Scholar]
- 4.Scholz J, Tonner PH. Alpha2-adrenoceptor agonists in anesthesia: A new paradigm. Curr Opin Anaesthesiol. 2000;13:437–42. doi: 10.1097/00001503-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Blaudszun G, Lysakowski C, Elia N, Tramèr MR. Effect of perioperative systemic α2 agonists on postoperative morphine consumption and pain intensity: Systematic review and meta-analysis of randomized controlled trials. Anesthesiology. 2012;116:1312–22. doi: 10.1097/ALN.0b013e31825681cb. [DOI] [PubMed] [Google Scholar]
- 6.Engelman E, Marsala C. Efficacy of adding clonidine to intrathecal morphine in acute postoperative pain: Metaanalysis. Br J Anaesth. 2013;110:21–7. doi: 10.1093/bja/aes344. [DOI] [PubMed] [Google Scholar]
- 7.Roh DH, Kim HW, Yoon SY, Seo HS, Kwon YB, Han HJ, et al. Intrathecal clonidine suppresses phosphorylation of the N-methyl-D-aspartate receptor NR1 subunit in spinal dorsal horn neurons of rats with neuropathic pain. Anesth Analg. 2008;107:693–700. doi: 10.1213/ane.0b013e31817e7319. [DOI] [PubMed] [Google Scholar]
- 8.Glynn C, Dawson D, Sanders R. A double-blind comparison between epidural morphine and epidural clonidine in patients with chronic non-cancer pain. Pain. 1988;34:123–8. doi: 10.1016/0304-3959(88)90157-1. [DOI] [PubMed] [Google Scholar]
- 9.Rauck RL, Eisenach JC, Jackson K, Young LD, Southern J. Epidural clonidine treatment for refractory reflex sympathetic dystrophy. Anesthesiology. 1993;79:1163–9. [PubMed] [Google Scholar]
- 10.Morgan GE, Mikhail MS, Murray MJ. 3rd ed. Philadelphia: McGraw-Hill; 2006. Clinical Anesthesiology; pp. 283–4. [Google Scholar]
- 11.Eisenach JC, Hood DD, Curry R. Intrathecal, but not intravenous, clonidine reduces experimental thermal or capsaicin-induced pain and hyperalgesia in normal volunteers. Anesth Analg. 1998;87:591–6. doi: 10.1097/00000539-199809000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Hassenbusch SJ, Gunes S, Wachsman S, Willis KD. Intrathecal clonidine in the treatment of intractable pain: A phase I/II study. Pain Med. 2002;3:85–91. doi: 10.1046/j.1526-4637.2002.02014.x. [DOI] [PubMed] [Google Scholar]
- 13.Ackerman LL, Follett KA, Rosenquist RW. Long-term outcomes during treatment of chronic pain with intrathecal clonidine or clonidine/opioid combinations. J Pain Symptom Manage. 2003;26:668–77. doi: 10.1016/s0885-3924(03)00144-1. [DOI] [PubMed] [Google Scholar]
- 14.Siddall PJ, Molloy AR, Walker S, Mather LE, Rutkowski SB, Cousins MJ. The efficacy of intrathecal morphine and clonidine in the treatment of pain after spinal cord injury. Anesth Analg. 2000;91:1493–8. doi: 10.1097/00000539-200012000-00037. [DOI] [PubMed] [Google Scholar]
- 15.Rudich Z, Peng P, Dunn E, McCartney C. Stability of clonidine in clonidine-hydromorphone mixture from implanted intrathecal infusion pumps in chronic pain patients. J Pain Symptom Manage. 2004;28:599–602. doi: 10.1016/j.jpainsymman.2004.02.018. [DOI] [PubMed] [Google Scholar]
- 16.Ruan X, Liu H, Couch JP, Wang F, Chiravuri S. Recurrent cellulitis associated with long-term intrathecal opioid infusion therapy: A case report and review of the literature. Pain Med. 2010;11:972–6. doi: 10.1111/j.1526-4637.2010.00854.x. [DOI] [PubMed] [Google Scholar]
- 17.Glynn C, O’Sullivan K. A double-blind randomised comparison of the effects of epidural clonidine, lignocaine and the combination of clonidine and lignocaine in patients with chronic pain. Pain. 1996;64:337–43. doi: 10.1016/0304-3959(95)00119-0. [DOI] [PubMed] [Google Scholar]
- 18.Carroll D, Jadad A, King V, Wiffen P, Glynn C, McQuay H. Single-dose, randomized, double-blind, double-dummy cross-over comparison of extradural and i.v. clonidine in chronic pain. Br J Anaesth. 1993;71:665–9. doi: 10.1093/bja/71.5.665. [DOI] [PubMed] [Google Scholar]
- 19.Eisenach JC, Rauck RL, Buzzanell C, Lysak SZ. Epidural clonidine analgesia for intractable cancer pain: Phase I. Anesthesiology. 1989;71:647–52. doi: 10.1097/00000542-198911000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Eisenach JC, DuPen S, Dubois M, Miguel R, Allin D. Epidural clonidine analgesia for intractable cancer pain. The epidural clonidine study group. Pain. 1995;61:391–9. doi: 10.1016/0304-3959(94)00209-W. [DOI] [PubMed] [Google Scholar]
- 21.Lavand’homme P, De Kock M. The use of intraoperative epidural or spinal analgesia modulates postoperative hyperalgesia and reduces residual pain after major abdominal surgery. Acta Anaesthesiol Belg. 2006;57:373–9. [PubMed] [Google Scholar]
- 22.Gabriella LR, Menezes de A, Alves JM, Paulino dos M. Epidural ketamine versus epidural clonidine as therapeutic for refractory neuropathic chronic pain. Rev Bras Anestesiol. 2002;52:34–40. [Google Scholar]
- 23.Ayad AE, El Masry A. Epidural steroid and clonidine for chronic intractable post-thoracotomy pain: A pilot study. Pain Pract. 2012;12:7–13. doi: 10.1111/j.1533-2500.2011.00469.x. [DOI] [PubMed] [Google Scholar]
- 24.Galer BS. Topical medications. In: Loeser JD, Butter SH, Chapman CR, Turk DC, editors. Bonica's Management of Pain. 3rd ed. Philadelphia, PA: Lipincott William & Wilkins; 2001. pp. 1736–42. [Google Scholar]
- 25.Davis KD, Treede RD, Raja SN, Meyer RA, Campbell JN. Topical application of clonidine relieves hyperalgesia in patients with sympathetically maintained pain. Pain. 1991;47:309–17. doi: 10.1016/0304-3959(91)90221-I. [DOI] [PubMed] [Google Scholar]
- 26.Byas-Smith MG, Max MB, Muir J, Kingman A. Transdermal clonidine compared to placebo in painful diabetic neuropathy using a two-stage ‘enriched enrollment’ design. Pain. 1995;60:267–74. doi: 10.1016/0304-3959(94)00121-t. [DOI] [PubMed] [Google Scholar]
- 27.Campbell CM, Kipnes MS, Stouch BC, Brady KL, Kelly M, Schmidt WK, et al. Randomized control trial of topical clonidine for treatment of painful diabetic neuropathy. Pain. 2012;153:1815–23. doi: 10.1016/j.pain.2012.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bollag L, Richebe P, Siaulys M, Ortner CM, Gofeld M, Landau R. Effect of transversus abdominis plane block with and without clonidine on post-cesarean delivery wound hyperalgesia and pain. Reg Anesth Pain Med. 2012;37:508–14. doi: 10.1097/AAP.0b013e318259ce35. [DOI] [PubMed] [Google Scholar]
- 29.Mohamed SA, Abdel-Ghaffar HS. Effect of the addition of clonidine to locally administered bupivacaine on acute and chronic postmastectomy pain. J Clin Anesth. 2013;25:20–7. doi: 10.1016/j.jclinane.2012.05.006. [DOI] [PubMed] [Google Scholar]


