INTRODUCTION
For centuries, the microbial world has been the biggest threat to public health. Infectious diseases were the main causes of death world-wide. Life expectancy was short and epidemics raged. The gradual improvements in standards of living, hygiene and the vaccines, the miracle cures, helped eliminate the diseases of filth. However then came the inexorable rise of non-infectious diseases. Ischemic heart disease and Cancers became the scourges of the West together with the chronic pulmonary diseases and cerebrovascular disease.
“Modernization” that contributes to the rise of these diseases is being accompanied by a growing need for chronic care. In reality the net gain of the benefits of modernization and economic growth are nullified out by the costs of care, lost productivity and premature death, of a preventable disease and also leads to disruption of social fiber of the society.
While sitting for an artist's portrait and signing papers at the “The Little White House” in Warm Springs, Georgia, on April 12, 1945, Roosevelt suddenly lost consciousness after complaining of a severe headache. Examining the patient 15 min later, Bruenn recorded the president's blood pressure (BP) at >300/190 mm Hg. Roosevelt died at the “young” age of 63. No autopsy was performed. Bruenn certified the cause of death as a cerebral hemorrhage. Bruenn wrote later in the Annals of Internal Medicine, “I have often wondered what turn the subsequent course of history might not have taken if the methods for the prevention and control of hypertension (HT) had been available.[1]
Even this modern era is full of stress and life is so fast that there is no time to take care of our health. This stressed up mind may also lead to increase of adrenaline in blood stream that eventually leads to increase in BP. It is termed as silent killer as sometimes it does not present any symptoms, but eventually effects heart and may cause heart attack.
This year World Health Day, i.e., on 7th April, publicized the increasing prevalence of HT by choosing “High BP” as the theme of 2013's celebration.
GLOBAL AND INDIAN OVERVIEW
Of the latest (2008) data available on mortality statistics, out of 57 million global deaths, 36 million or 63% were due to non-communicable diseases (NCDs). The burden of these diseases is rising disproportionately among lower income countries and populations. For the same year, nearly 80% of NCD deaths - 29 million - occurred in low- and middle-income countries with about 29% of deaths occurring before the age of 60.[2] The leading causes of NCD deaths in 2008 were cardiovascular diseases (CVD) (17 million deaths, or 48% of all NCD deaths), cancers (7.6 million, or 21% of all NCD deaths) and diabetes caused another 1.3 million deaths.[2] Nearly 70% of the NCDs are contributed by CVD, cancer and diabetes alone.
In terms of attributable deaths, the leading NCD risk factors globally are raised BP. (To which 13% of the global deaths are attributed), followed by tobacco (9%), high blood glucose (6%), physical inactivity (6%) and overweight and obesity (5%).[2]
HT is currently the leading risk resulting in considerable death and disability world-wide and accounted for 9.4 million deaths and 7% of disability adjusted life years in 2010.[3]
In India CVD cause 1.5 million deaths annually.[4] HT is directly responsible for 57% of all stroke deaths and 24% of all coronary heart disease (CHD) deaths. This fact is important because HT is a controllable disease and a 2 mm Hg population wide decrease in BP can prevent 151,000 stroke and 153,000 CHD deaths.[5]
Statistics are staggering considering India accounting for 21% of the Worlds global burden of disease. Adult HT prevalence has risen dramatically over the past three decades from 5% to between 20-40% in urban areas and 12-17% in rural areas.[6]
A community based survey was carried out in 7 states under Integrated Disease Surveillance Project with Indian Council of Medical Research as the implementing agency during 2007-2008, the prevalence of HT was varying from 19 to 24% in the states with marginal rural - urban difference.[7]
Apart from health implications it has huge societal, developmental and economic costs. There is a remarkable income loss to the families affected by HT not only due to illness, but because of hospital admissions and premature deaths. The annual income loss (calculated in 2004) was Rs 43 billion and accounts for 64% of out of pocket expense. A month's treatment with just one antihypertensive medication costs 1.8 day's wages and becomes unaffordable if more than one drug is prescribed or more than one person is hypertensive in the family.[8]
PREVENTION AND CONTROL
The preclinical substrates for CVD (e.g., fatty streaks and atherosclerosis) begin early in life and are influenced over time by potentially modifiable risk factors, behaviors and environmental exposures. Favorable risk factor levels in middle age are associated with a lower lifetime risk for CVD mortality, increased survival and improved quality-of-life.
Population-based and clinical studies highlight the importance of primordial prevention, defined herein as prevention of the development of risk factors in the first place and primary prevention, defined as interventions designed to modify adverse levels of risk factors once present with the goal of preventing HT.
The low prevalence of HT in some communities indicates that HT is potentially preventable. HT can be prevented by complementary application of strategies that target the general population and individuals and groups at higher risk for high BP. Life-style interventions are more likely to be successful and the absolute reduction in risks of HT are likely to be greater when targeted in persons who are older and those who have a higher risk of developing HT compared with their counterparts who are younger or have a lower risk.
The World Health Organization (WHO) has recommended the following approaches in the prevention of HT:
Primary prevention: Population and high risk strategy
Prevention paradox
According to Geoffrey Rose, nature presents us with a processor continuum, not a dichotomy for the vast majority of diseases. The risk typically increases across the spectrum of a risk factor. Use of dichotomous labels such as “hypertensive” and “normotensive” is therefore for operational convenience. Hence, the “deviant minority” (hypertensive) are only part of a risk continuum, rather than a distinct group. This leads to one of the most fundamental axioms in preventive medicine: “A large number of people exposed to a small risk may generate many more cases than a small number exposed to high risk.” A preventive strategy focusing on high-risk individuals will thus deal only with the margin of the problem and will not have any impact on the large proportion of disease occurring in the large proportion of people who are at moderate risk, for example, people with slightly raised BP suffer more cardiovascular events than the hypertensive minority.[9]
The goal of the population approach is to shift the community distribution of BP toward lower levels or biological normality. This involves a multi factorial approach, dietary approaches are of paramount importance, reduction of salt intake, avoidance of a high alcohol intake, moderate fat intake, exercise promotion, and last but not the least behavioral changes. The whole community must be mobilized and made aware of the possibility of primary prevention. In an analysis based on Framingham Heart Study experience, Cook et al. concluded that a 2 mm Hg reduction in the population average of diastolic BP for white U.S. residents 35-64 years of age would result in a 17% decrease in the prevalence of HT, a 14% of reduction in the risk of stroke and transient ischemic attacks and a 6% reduction in the risk of CHD.[10]
The population strategy offers only a small benefit to each individual, since most of them were going to be all right anyway, at least for many years. This leads to the prevention paradox: “A preventive measure which brings much benefit to the population offers little to each participating individual” and thus there is poor motivation for the subject. In mass prevention each individual has usually only a small expectation of benefit and this small benefit can easily be outweighed by a small risk.
Dietary approaches to stop HT eating plan includes whole grain products, fish, poultry and nuts. It is reduced in lean red meat, sweets, added sugars and sugar-containing beverages compared with the typical American diet. It is rich in potassium (4700 mg), magnesium (500 mg) and calcium (1250 mg), as well as protein (18% of total calories) and fiber (30 g).[11]
Limited available data point to high salt intake (9-12 g/day), which exceeds current WHO recommended levels.[12] The recent global burden of disease study reports excess salt intake to be the 7th leading cause of mortality in South East Asia Region, which is much higher than in rest of the world (11th globally), highlighting the adverse impact of high intake in countries like India.[3]
SECONDARY PREVENTION AND RESISTANT HYPERTENSION
Secondary prevention stands at the boundary between prevention and treatment. Many cardiologists consider secondary prevention to be treatment of coronary artery disease; others see it as prevention of recurrent coronary events. Predisposing risk factors consist of obesity, physical inactivity, family history of premature CHD, male sex and possibly behavioral, socio-economic and ethnic factors. Their association with CHD is complex.
Mainstay of the the treatment is four classes of drugs, i.e., diuretics followed by angiotension receptor blockers, beta blockers and calcium channel blockers, but they all vary according to the heath status and co-morbidities.
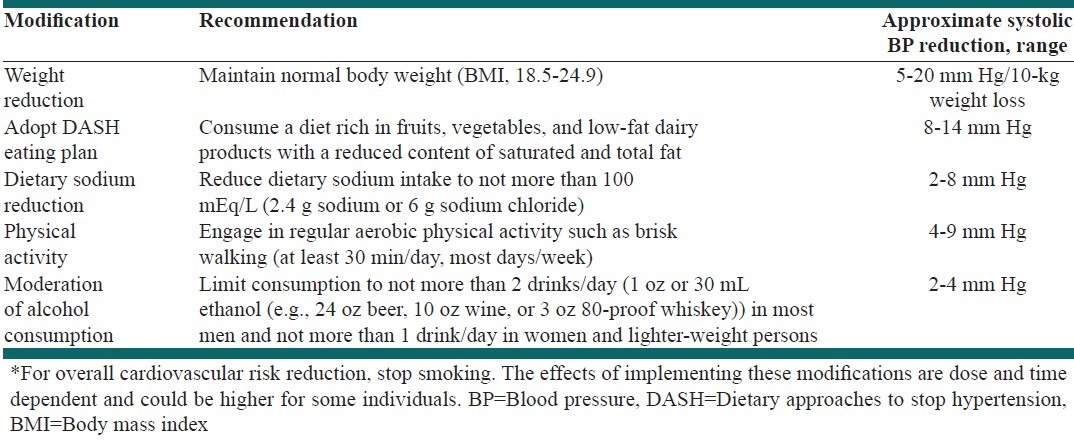
HT is a major independent risk factor for CAD, stroke and renal failure. The concept that CHD can be prevented has increasingly become a driving force in cardiovascular medicine. Widespread acceptance of the benefits of prevention came first in the area of secondary prevention, i.e., preventing recurrent coronary events in patients with established CHD [Table 1].[13,14]
Table 1.
Lifestyle modifications to manage hypertension*
One of the facets of the HT epidemic that has come to the forefront is “RH”. RH is defined as BP above goal (usually 140/90 mm Hg) despite adherence to a combination of at least 3 optimally dosed antihypertensive medications of different classes, one of which ideally is a diuretic.
Patients requiring ≥4 antihypertensive medications (even if controlled) are classified as having RH. The prevalence of RH has been estimated to be 20-30%.[15]
An another fact in recent results of studies describing associations between habitual smoking and BP and/or newly developed HT are inconsistent and vary from modest positive effects (Halperin RQ, Gaziano JM, Sesso HD. Smoking and the risk of incident HT in middle aged- and older men. Am J Hypertens 2008; 21: 148-152), through no observed effect to protective effects. Habitually smoking men had significantly negative correlation on the development of HT, but the same effect was not seen among women.[16]
THE ROAD AHEAD
India cannot afford the resource intensive model of health-care to address HT and NCDs and should, therefore, prioritize population based prevention approaches requiring multi-sectoral actions across non-health sectors to minimize population risk factor exposure in tandem with evidence based clinical approaches focussed on early detection and treatment, which can maximize the gains for population health.
India is experiencing a rapid health transition with large and rising burden of chronic NCDs. HT is easily diagnosable and treatable with life-style modifications and effective medicines. Thus, HT control provides an entry point to deal with other NCDs as any intervention will help concomitantly address other NCDs as well. This has been taken into cognizance in the newly launched National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS), which has HT and diabetes as the main focus areas.[17]
The NPCDCS aims at integration of NCD interventions in the National Rural Health Mission (NRHM) framework for optimization of scarce resources and provision of seamless services to the end customer/patients as also for ensuring long term sustainability of interventions. Thus, the institutionalization of NPCDCS at district level within the District Health Society, sharing administrative and financial structure of NRHM becomes a crucial program strategy for NPCDCS. The NCD cell at various levels will ensure implementation and supervision of the programme activities related to health promotion, early diagnosis, treatment and referral, and further facilitates partnership with laboratories for early diagnosis in the private sector.
Strategy for early diagnosis of chronic NCDs will consist of opportunistic screening of persons above the age of 30 years at the point of primary contact with any health-care facility, be it the village, CHC, District hospital, tertiary care hospital etc.
“NCD clinic” will be established at CHC and District Hospital (NCD here refers to cancer diabetes, HT, CVD and stroke) where comprehensive examination of patients referred by lower health facility/health worker as well as of those reporting directly will be conducted for ruling out complications or advanced stages of common NCDs. Screening, diagnosis and management (including diet counseling, life-style management) and home based care will be the key functions.
The rising burden of HT, associated CVD and NCDs in India needs to be addressed as a public health priority employing an optimal context specific resource sensitive combination of the population and the clinical approach.[18]
The foremost modifiable risk factors are overweight (and obesity) and physical inactivity. These conditions occur commonly in our society and predispose to multiple risk factors, both causal and conditional. Because the latter risk factors accompanying obesity and physical inactivity result from metabolic aberration and often cluster in individuals, their clustering has been called the metabolic syndrome. The success of recent secondary prevention trials of statin therapy mandates more emphasis on high-risk primary prevention.
The landmark decision at the World Health Assembly (65 [6]) to adopt the global target of a 25% reduction in premature NCD mortality by 2025 has already made significant progress. Now, all UN Member States need to agree on a comprehensive set of targets and indicators that will drive progress towards the “25 by 25” goal. As WHO Director General Margaret Chan previously stated, “what gets measured, gets done.”[19]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bruenn HG. Clinical notes on the illness and death of President Franklin D. Roosevelt. Ann Intern Med. 1970;72:579–91. doi: 10.7326/0003-4819-72-4-579. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Global Health Observatory. Geneva: WHO; 2011. NCD Mortality and Morbidity. [Google Scholar]
- 3.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaziano TA, Reddy KS, Paccaud F, Horton S, Chaturvedi V. Cardiovascular disease. In: Jamison DT, Breman JG, Measham MR, Alleyne G, Claeson M, Evans DB, editors. Disease Control Priorities in Developing Countries. 2nd ed. New York, NY: Oxford University, Press; 2006. pp. 645–62. [Google Scholar]
- 5.Rodgers A, Lawes C, MacMahon S. Reducing the global burden of blood pressure-related cardiovascular disease. J Hypertens Suppl. 2000;18:S3–6. [PubMed] [Google Scholar]
- 6.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004;18:73–8. doi: 10.1038/sj.jhh.1001633. [DOI] [PubMed] [Google Scholar]
- 7.Integrated Disease Surveillance Project. Ministry of Health and Family Welfare, Government of India. New Delhi: MoHFW; 2007-08. Non-communicable Disease Risk Factors Survey Phase-1. [Google Scholar]
- 8.Mahal A, Karan A, Engelgau M. Health Nutrition and Population (HNP) Discussion Paper. Washington: The World Bank; 2010. The Economic Implications of Non-Communicable Disease for India. [Google Scholar]
- 9.Dobe M. Hypertension: The prevention paradox. Indian J Public Health. 2013;57:1–3. doi: 10.4103/0019-557X.111354. [DOI] [PubMed] [Google Scholar]
- 10.Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–9. [PubMed] [Google Scholar]
- 11.NHLBI. Your Guide to Lowering Your Blood Pressure with DASH. Washington: National Institutes of Health National Heart, Lung, and Blood Institute; 2006. NIH Publication No. 06-4082. [Google Scholar]
- 12.Mohan S, Prabhakaran D. Background Paper for the Expert Meeting on Population Sodium Reduction Strategies for Prevention and Control of Noncommunicable Diseases in the South-East Asia Region. New Delhi: WHO, SEARO; 2012. Review of Salt and Health: Situation in South-east Asia Region. [Google Scholar]
- 13.Chobanian AV, Hill M. National Heart, Lung, and Blood Institute Workshop on Sodium and Blood Pressure: A critical review of current scientific evidence. Hypertension. 2000;35:858–63. doi: 10.1161/01.hyp.35.4.858. [DOI] [PubMed] [Google Scholar]
- 14.Smith SC, Jr, Blair SN, Criqui MH, Fletcher GF, Fuster V, Gersh BJ, et al. Preventing heart attack and death in patients with coronary disease. Circulation. 1995;92:2–4. [PubMed] [Google Scholar]
- 15.Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: Diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–19. doi: 10.1161/HYPERTENSIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 16.Wang W, Lee ET, Fabsitz RR, Devereux R, Best L, Welty TK, et al. A longitudinal study of hypertension risk factors and their relation to cardiovascular disease: The Strong Heart Study. Hypertension. 2006;47:403–9. doi: 10.1161/01.HYP.0000200710.29498.80. [DOI] [PubMed] [Google Scholar]
- 17.Operational Guidelines. New Delhi: Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India; 2011. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke. [Google Scholar]
- 18.Mohan S, Campbell N, Chockalingam A. Time to effectively address hypertension in India. Indian J Med Res. 2013;137:627–31. [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. 65 (6)th World Health Assembly. Geneva: WHO; 2011. Prevention and Control of Non-communicable Diseases. [Google Scholar]


