Abstract
Background:
Early detection through screening is the best method to reduce death due to breast cancer. It has been shown, having knowledge and generating positive attitudes, influences the decision of women to participate in the screening programs. The aim of this study was to identify the factors associated with breast cancer screening (BCS) and with an intention to have screening among women in Tehran, Iran.
Methods:
A cross-sectional study was carried out from January to July 2011, among women who had attended to primary health-care centers in West Tehran using multi-stage sampling method. We invited 1,240 women sequentially to complete a self-administered survey questionnaire at the beginning of their visit; and 1,012 (82%) completed the survey. The questionnaire included, items drawn from the Preventive Health Model that assess socio-demographic background and perceptions about BCS. Multiple logistic regression analysis was performed to identify factors associated with screening and intention to do screening in the future.
Results:
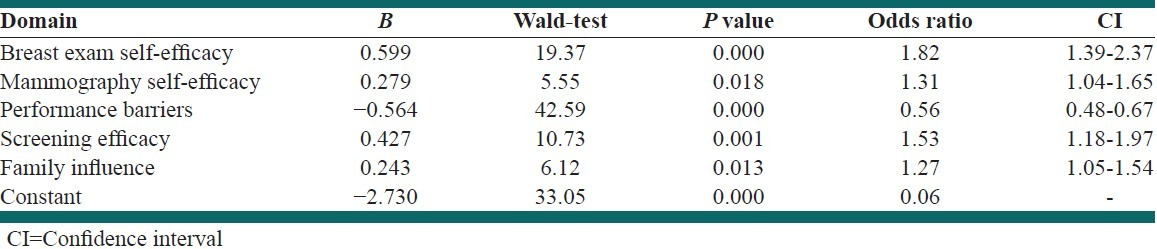
The mean age of subjects was 38.2 years. Women who perceived more screening efficacy (odd ratio [OR] =1.63; confidence interval [CI] 95%: 1.12-2.37) and fewer performance barriers (OR = 0.82; CI 95%: 0.68-0.97) were more likely to perform clinical breast exam in the future. The women who reported higher clinical breast exam self-efficacy (OR = 1.82; CI 95%: 1.39-2.37), mammography self-efficacy (OR = 1.31; CI 95%: 1.04-1.65), screening efficacy (OR = 1.53; CI 95%: 1.18-1.97), and family influence (OR = 1.27; CI 95%: 1.05-1.54), and those who reported fewer screening performance barriers (OR = 0.56; CI 95%: 0.48-0.67) were more likely to decide for carried out mammography in the future. Most respondents indicated that they intended to do clinical breast exam and mammography in the future (75.8% and 72.1% respectively). About 65% of women reported they would do both.
Conclusions:
We found that women's intention to do BCS was very high and a comprehensive national program is needed to guide their intention. Among different demographic factors, the impact of education level on doing BCS was significant.
Keywords: Attitude, breast cancer screening, decision making, knowledge
INTRODUCTION
Breast cancer is the most common cancer among women world-wide and this cancer comprising 16% of all female cancers and it is estimated that 519,000 women died in 2004 because of breast cancer.[1] Although, the incidence of breast cancer in developed countries is more than developing countries, but about 50% of all diagnosis of breast cancer[2] and majority (69%) of all breast cancer deaths occurs in developing countries.[1]
It has been shown that the annual incidence of breast cancer is increasing in developing countries. The incidence rate of breast cancer is as high as 99.4/100,000 in North America while the lowest incidence rate is in African countries.[1] It has been reported that Asia and Africa have a more rapidly rising incidence rate than North America and Europe.[3,4]
The incidence rate of breast cancer is rising in Iran too. Based on a review of published articles from January 1998 to December 2005, the incidence rate of breast cancer was reported as 22/100,000 in Iran.[5] About 72% of the breast cancers diagnosed include, a tumor over 2 cm.[5] Mostly patients present with advanced stage of disease and they are younger than patients in Western countries.[6]
Breast cancer can be detected at early stages and it has been shown that if breast cancer discovered early, it can often be cured. Early detection through screening is the best method to reduce death due to breast cancer.[7] Screening methods for the early detection of breast cancer include: Breast self-examination, clinical breast examination (CBE), and mammography.
The United States Preventive Services Task Force (USPSTF) recommends biennial screening mammography for women aged 50-74 years.[8] Analysis reported by the USPSTF provided an estimated mortality reduction of 16% for women of all ages covered in the screening trials.[9]
Some studies have examined the knowledge and practice of mammography use among women in Iran. One study in Zahedan, Iran showed that only 3.4% of women know about mammography.[2] Based on a population-based survey in Tehran, it was shown the 17% of women reported conducting regular breast self-examination, and 61% stated they knew about methods of breast cancer screening (BCS).[6]
It has been shown having that knowledge and given positive attitudes affects decision of women to participate in screening programs. The importance of this cancer in terms of incidence and mortality in our country, we conducted the present study to identify factors associated with BCS and with intention to have screening among women in Tehran, Iran.
METHODS
Design and participant recruitment
This cross-sectional study was carried out from January to July 2011, among women who had attended to primary health-care centers supported by Shahid-Beheshti University of Medical Sciences in the West Tehran. We selected randomly 10 urban and rural primary health-care centers among 28 centers. These 10 centers provided a good distribution of all 28 centers based on covered population and geographic area. The questionnaire offered to a total of 1240 women, 1012 (82%) questionnaires were returned were included in the final analysis. The women were selected by a sequential sampling method during the study period. At the beginning of the survey, eligible women were recruited sequentially until 6 months. We selected each woman who attended to health centers for any of care. Sample was gathered all days of a week but holidays.
The inclusion criteria were considered literate, being 30-70 years old, and visiting a selected primary health-care center. Women with breast cancer diagnosis were excluded from the study.
This study was approved and granted by research affairs of Tehran University of Medical Sciences. We obtained written informed consent from all participants.
Survey instrument and measures
We used a structured questionnaire, which was used in the study of factors associated with colorectal cancer screening decision stage developed by Sifri et al. by permission.[10] We adapted the instrument by changing items, so that they addressed BCS.
The questionnaire was translated into Persian by two independent public-health professionals fluent in both English and Persian. The translated questionnaire was assessed by a panel of epidemiologists and community medicine specialists for evaluation of any discrepancy. Then, one person back translated the questionnaire into English. The pilot version was made following reviews by all investigators. We asked one hundred eligible women fill out questionnaires and tell us any ambiguity about items. Based on the result of this pilot study, the final version of questionnaire was developed. Pilot study excluded from the main part of the study.
The questionnaire included two main parts and 60 items. The first part was about general and demographic characteristics (i.e., age, marital status, education, previous cancer screening, and general rating of health) using 18 items. The principle part of the questionnaire included 26 items in 8 domains (Breast exam Self-Efficacy (four items), Mammography Self-Efficacy (four items), Performance Barriers (six items), Salience and Coherence (four items), Screening Efficacy (three items), Perceived susceptibility (two items), Worries and concern (two items), and Family influence (one item). These items were the principle items of the questionnaire, and the other items were about the strength of agreement for principle questions. Therefore, each item had a response in two steps: The first one was the main body of question, which asked the agreement of participants (i.e., “Doing the mammography would be difficult for me. Do you agree or disagree?” The second part asked the degree of agreement or disagreement (i.e., “strongly or mildly?”). This part of the question has a 4-point Likert scale (1 = “Strongly Agree”, 2 = “Moderately Agree,” 3 = “Moderately Disagree,” and 4= “Strongly Disagree”). There was a short description of each BCS methods (CBE and Mammography) before decision assessment parts of questionnaire. The trained staff helped participants who needed more description. The main analysis was carried on the principle part of the questionnaire.
The questionnaire was self-administered, which was offered to the women in the waiting rooms of each primary health-care center at the beginning of their visits. In each center, one staff who underwent standardized training helped the participants to fill out the questionnaire.
Statistical analysis
All statistical analyses were performed using SPSS (version 16, SPSS Inc., Chicago, IL). We used independent sample t-test to compare numeric variables across two groups of nominal variables. Chi-square test was used to assess association between nominal or ordinal variables. Analysis of variance was used to compare the mean of numeric variables across more than two groups. An exploratory factor analysis by principal component analysis and Varimax method was used to verify the domains produced from the first analysis in the development of the questionnaire. The criterion to consider loading set as 0.5 or higher. To assess internal consistency of each domain, the co-efficient of Cronbach's α was used. We made two separate models by multiple logistic regression analysis for two key items in the questionnaire. These two items were about “Have you ever carried out CBE as BCS?” And “Do you want to have mammography for BCS in future?” Answers to these two questions were dichotomized as “yes” or “no.” Therefore, dependent variables were answer to these questions, and domains significantly associated with these two questions in bivariate analysis included as independent predictors in the models. Significant level was considered at 0.05.
RESULTS
Among 1240 distributed questionnaires, 1012 completed questionnaires were included in the final analysis. The mean age of subjects was 38.2 years (median = 36, range = 30-70). Majority of women 916 (91%) were married and almost half of them were educated more than primary school.
A total of 896 (92%) subjects did not have benign breast disease. A total of 65 women (6%) reported history of family breast cancer in which 21 (32%) subjects were diagnosed less than 40 years old. CBE and mammography were carried out by 22% and 7% of women respectively. These proportions for decision about doing CBE and mammography were 76% and 72% respectively. The relative frequency of decision on doing both mammography and CBE in future was 65% (655 women). Out of 1012 women, 722 (71%) reported their general health as good and very good [Table 1].
Table 1.
Descriptive profile of participants by items of questionnaire (n=1012)
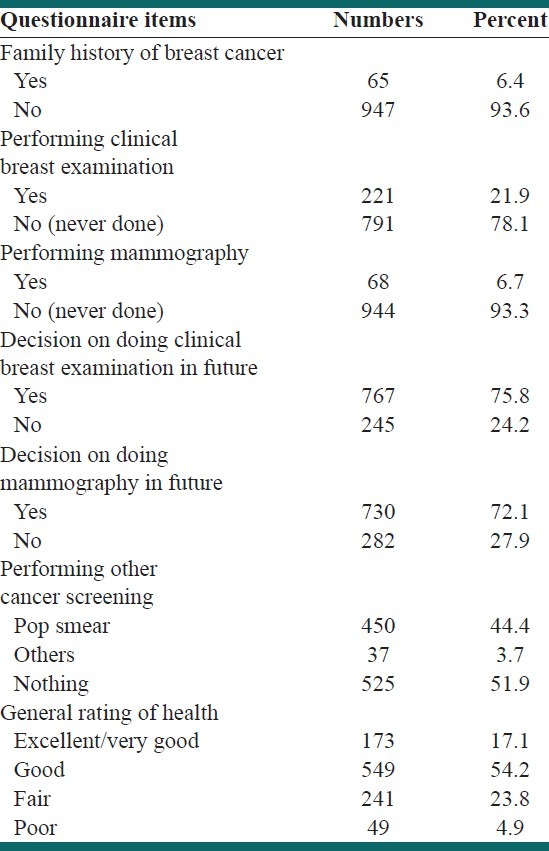
A total of 64% and 65% women respectively knew that CBE and mammography were BCS methods.
Participant's opinion about BCS
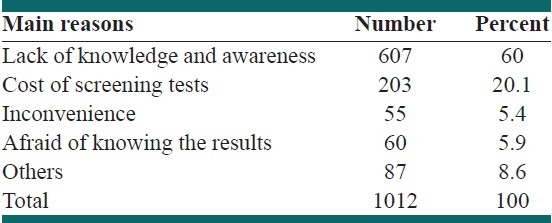
A total of 92% of respondents believed that the benefits of CBE outweigh its difficulty, 90% believed that the benefits of mammography outweigh its difficulty, and 35% had decided to do mammography in the future (less than 12 months). Thirty two percent of the women thought they were not at risk of breast cancer. The main reasons for not doing regular BCS illustrates in Table 2.
Table 2.
The main reasons for not doing regular breast cancer screening
Internal consistency of domains and factor analysis
Internal consistency for all dimensions measured by Cronbach's α was from 0.66 to 0.95. The minimum score was for domain of “mammography Self-Efficacy” (0.66) and maximum score was for domain of “perceived susceptibility” (0.95). In factor analysis with a maximum eight-factor solution all items were loaded on their hypothesized factor.
Description of answers to the domains
Mean score of “breast exam self-efficacy” was 2.21 (±0.63). Eighty percent of participants had a high level of breast exam self-efficacy, and 69% of women reported high level of mammography self-efficacy. Twenty two percent of participants reported high level of performance barriers. Nine hundred and fifty seven subjects (95%) considered BCS as a salient and coherent preventive health behavior. Ninety nine percent of women believed in screening efficacy, 68% believed they were susceptible to breast cancer, 54% were worried and concerned about BCS results, and 83% thought their family supported BCS programs.
Association of domains and demographic characteristics
The mean scores of the performance barrier and family influence in the primary educated group was higher than high school graduated group, while the mean scores of salience and coherence, worries and concern, and perceived susceptibility in the high school graduated group were higher than in primary educated group. All differences were significant at less than 0.05 levels.
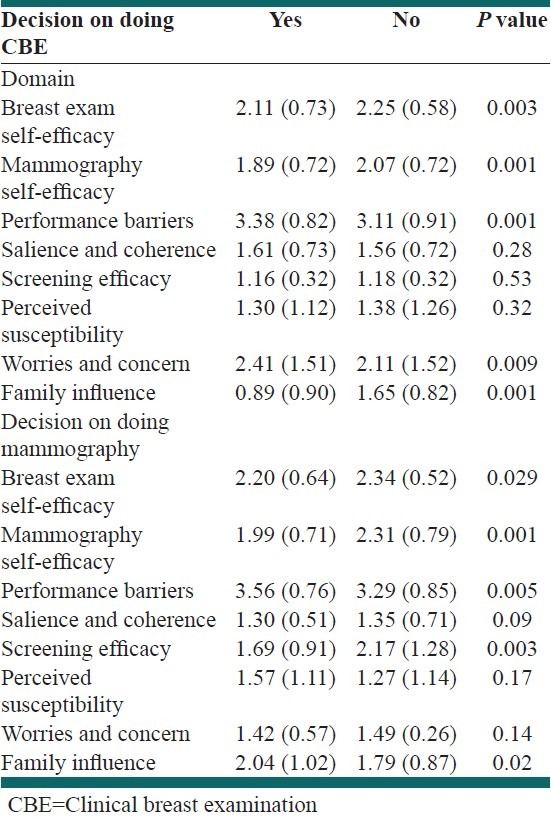
Table 3 illustrates the association between decision to do CBE and mammography in the future by domains' score of the questionnaire.
Table 3.
Decision of doing clinical breast examination and mammography in future by domains
Multivariate analysis
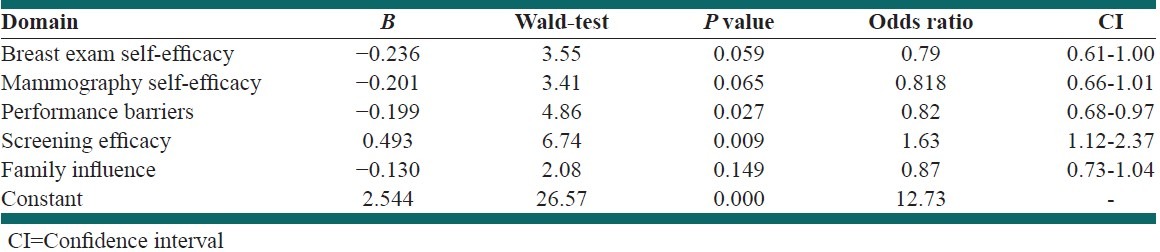
Two multiple logistic regression models were fitted to model the probability of performing CBE and decision on doing mammography in future. The questionnaire's domains, which in the bivariate analyses were associated with these two questions, put in the logistic regression analysis as independent variables.
Logistic regression model of performing CBE in future
After adjustment, the participants who reported higher screening efficacy (odd ratio [OR] =1.63) and fewer performance barriers (OR = 0.82) were more likely to report performing CBE [Table 4].
Table 4.
logistic regression model of domains to predict doing clinical breast examination in future
Logistic regression model of decision on doing mammography in future
After adjustment, all of five entered factors were significantly associated with reported decision to do mammography in future. The subjects who had higher breast exam self-efficacy, Mammography self-efficacy, screening efficacy, Family influence, and who had fewer performance barriers, were more likely to report decision on doing mammography in future [Table 5].
Table 5.
Logistic regression model of domains to predict decision on doing mammography
DISCUSSION
The results of current study demonstrated that prevalence of performing CBE (22%) and mammography (7%) was low among our study participants. however, these proportions for of respondents who had decided to do CBE (76%) and mammography (72%) were high.
Our findings are almost identical to previous studies of BCS in Iran. Some studies in other parts of Iran[2,11,12,13] during last 15 years demonstrated similar findings with the lowest prevalence of BCS in Zahedan (a city in the South East of Iran)[2] and the highest in Tehran.[6] Although, some women of specific population such as health-care workers had high level knowledge about BCS, their BCS practice rates were comparable to the general population. One explanation for the gap between knowledge and practice of BCS could be that BCS is not a social norm. Participation of people in any screening program needs both knowledge and belief that screening is useful.
Countries in the Middle-East have the same situation as Iran considering BCS. A comprehensive Turkish studies on CBE and mammography reported 89.3% of Turkish women had never had mammography and 75% had never had CBE.[14] Some other Turkish studies on West Anatolian sample showed about 50% of participants had at least one CBE but only 4.4% had carried out CBE on regular basis.[15]
Jordanian's women (Amman) study indicated 76% agreement on the benefits of BCS by mammography but they have not reported prevalence of BCS practices.[16]
United Arab Emirates Nurses studies reported 84.4% of performing breast self-examination (BSE) by participants, which was comparable with developed countries such as the US and UK.[17] According to the results of other studies in the Middle-East, beginning of BCS by mammography on 45 years old instead of 50 years old is more useful.[18,19]
Another study on 770 Chinese women showed one-third of participants had never carried out any kind of BCS.[20]
The studies on Asian women (Filipino, Chinese, and Iranian) who had lived in developed countries such as US and Canada reported 40-57% BCS by mammography. The rate of BCS was associated with duration of immigration, insurance, income and level of education.[21] It should be indicated that target rate of mammography screening in Healthy People 2010 was 70%. Health belief model was used in almost all of BCS studies which make these studies comparable.[22,23]
Another main finding in our study was that, participants who had considered screening efficacy and fewer barriers, reported more decision on doing CBE in the future. The logistic regression model to predict decision on doing mammography as a BCS showed believe in “breast exam self-efficacy.” “mammography self-efficacy” and “screening efficacy” are most important independent factors. These findings were supported by other studies .[11,12,16,22,23] The family influence as a mammography predictor was found in our study too. Believe in family influence by women can be critical in screening program progress.
Our findings indicate that educational status has a strong influence on doing BCS. These findings are warranted by other studies.[2,3,4,5,6] Less educated women reported more barriers for doing BCS; and their family influence on doing BCS decision was significant.
Association between education of women with attitude and practice on BCS decision was shown in recent studies in Iran.[6,11,12,13] In current study about half of women were high school or higher educated and in Zahedan study 31% of participants were illiterate.[2] Performing mammography was 7% in our study and 1.3% in Zahedan study (without convenience and economic status adjustment). These findings indicate growing of health behaviors like cancer screening is not as fast as education level of Iranian women. Unfortunately BCS even in Iranian health-care staff, nurses, and specialists (gynecologists) is not optimum.[6,24] Accordance with women intention for doing BCS in our study, a national program on BCS is needed. Although, most breast cancer studies considered breast self-examination as a BCS method, guidelines emphases on CBE and mammography.
Strong aspects of our study were the large sample size, selection of sample size from primary care centers and using of standard and comparable questionnaire. Furthermore, the response rate was high with less than 20% non-responders.
Our study had some limitations. Although, we tried to account important variables, which affect decision on BCS however, the effects of income, insurance, career, and family members were not accounted. It was due to not having a standard measures to account these variables in the questionnaire.
We suggest further studies on finding an appropriate model of behavior change for Iranian women and performing complementary studies for evaluation of these models effects. Future studies considering CBE and mammography in prospective interventional studies to confirm the benefits of these approaches on reducing mortality of breast cancer in Iranian women is recommended.
CONCLUSIONS
We found that women's intention to do BCS is very high and a comprehensive national program is needed to provide women an opportunity to act on their intention.
It may be useful to develop the women's education programs, combined with a national screening program, and to maximize program impact.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Breast cancer: Prevention and control. Breast cancer burden. 2004. [Last accessed 2011 Aug 21]. Available from: http://www.who.int/cancer/detection/breastcancer/en/index1.html .
- 2.Heidari Z, Mahmoudzadeh-Sagheb HR, Sakhavar N. Breast cancer screening knowledge and practice among women in Southeast of Iran. Acta Med Iran. 2008;46:321–8. [Google Scholar]
- 3.Shirazi M, Champeau D, Talebi A. Predictors of breast cancer screening among immigrant Iranian women in California. J Womens Health (Larchmt) 2006;15:485–506. doi: 10.1089/jwh.2006.15.485. [DOI] [PubMed] [Google Scholar]
- 4.Ahmed F, Mahmud S, Hatcher J, Khan SM. Breast cancer risk factor knowledge among nurses in teaching hospitals of Karachi, Pakistan: A cross-sectional study. BMC Nurs. 2006;5:6. doi: 10.1186/1472-6955-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mousavi SM, Montazeri A, Mohagheghi MA, Jarrahi AM, Harirchi I, Najafi M, et al. Breast cancer in Iran: An epidemiological review. Breast J. 2007;13:383–91. doi: 10.1111/j.1524-4741.2007.00446.x. [DOI] [PubMed] [Google Scholar]
- 6.Montazeri A, Vahdaninia M, Harirchi I, Harirchi AM, Sajadian A, Khaleghi F, et al. Breast cancer in Iran: Need for greater women awareness of warning signs and effective screening methods. Asia Pac Fam Med. 2008;7:6. doi: 10.1186/1447-056X-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akhigbe AO, Omuemu VO. Knowledge, attitudes and practice of breast cancer screening among female health workers in a Nigerian urban city. BMC Cancer. 2009;9:203. doi: 10.1186/1471-2407-9-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.USPSTF Guidelines on Mammograms Questioned. 2009. [Last accessed 2011 Aug 21]. Available from: http://www.uspreventiveservicestaskforce.org/uspstf/uspsbrca.htm .
- 9.Humphrey LL, Helfand M, Chan BK, Woolf SH. Breast cancer screening: A summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137:347–60. doi: 10.7326/0003-4819-137-5_part_1-200209030-00012. [DOI] [PubMed] [Google Scholar]
- 10.Sifri R, Rosenthal M, Hyslop T, Andrel J, Wender R, Vernon SW, et al. Factors associated with colorectal cancer screening decision stage. Prev Med. 2010;51:329–31. doi: 10.1016/j.ypmed.2010.06.015. [DOI] [PubMed] [Google Scholar]
- 11.Abedzadeh M, Sadat Z, Saberi F. Knowledge, attitude and performance of women referring health care centersin Kashan towards breast cancer and its screening tests. Feyz. J Kashan University Med Sci Health Services. 2001;4:49–55. [Google Scholar]
- 12.Enjezab B, FarajKhoda T, Mojahed SH, Bokaei M. Barrier and motivators related to cervical and breast cancer screening. J Shahid Sadoughi University Med Sci Health Services. 2004;12:78–84. [Google Scholar]
- 13.Hadi N, Sadeghi-Hassanabadi A, Talei AR, Arasteh MM, Kazerooni T. Assessment of a breast cancer screening programme in Shiraz, Islamic Republic of Iran. East Mediterr Health J. 2002;8:386–92. [PubMed] [Google Scholar]
- 14.Dündar PE, Ozmen D, Oztürk B, Haspolat G, Akyildiz F, Coban S, et al. The knowledge and attitudes of breast self-examination and mammography in a group of women in a rural area in western Turkey. BMC Cancer. 2006;6:43. doi: 10.1186/1471-2407-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Discigil G, Sensoy N, Tekin N, Soylemez A. Attitude and practice on breast health in west Anatolian women sample. Breast J. 2007;13:218–9. doi: 10.1111/j.1524-4741.2007.00411.x. [DOI] [PubMed] [Google Scholar]
- 16.Petro-Nustas W. Young Jordanian women's health beliefs about mammography. J Community Health Nurs. 2001;18:177–94. doi: 10.1207/S15327655JCHN1803_04. [DOI] [PubMed] [Google Scholar]
- 17.Sreedharan J, Muttappallymyalil J, Venkatramana M, Thomas M. Breast self-examination: Knowledge and practice among nurses in United Arab Emirates. Asian Pac J Cancer Prev. 2010;11:651–4. [PubMed] [Google Scholar]
- 18.Soskolne V, Marie S, Manor O. Beliefs, recommendations and intentions are important explanatory factors of mammography screening behavior among Muslim Arab women in Israel. Health Educ Res. 2007;22:665–76. doi: 10.1093/her/cyl132. [DOI] [PubMed] [Google Scholar]
- 19.Klabunde CN, Sancho-Garnier H, Taplin S, Thoresen S, Ohuchi N, Ballard-Barbash R, et al. Quality assurance in follow-up and initial treatment for screening mammography programs in 22 countries. Int J Qual Health Care. 2002;14:449–61. doi: 10.1093/intqhc/14.6.449. [DOI] [PubMed] [Google Scholar]
- 20.Im Kim J, Ok Oh K, YU Li C, Suk Min H, Sung Chang E, Song R. Breast cancer screening practice and health-promoting behavior among chinese women. Asian Nurs Res. 2011;5:157–63. doi: 10.1016/j.anr.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 21.Wu TY, West B, Chen YW, Hergert C. Health beliefs and practices related to breast cancer screening in Filipino, Chinese and Asian-Indian women. Cancer Detect Prev. 2006;30:58–66. doi: 10.1016/j.cdp.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 22.Taymoori P, Berry T. The validity and reliability of Champion's Health Belief Model Scale for breast cancer screening behaviors among Iranian women. Cancer Nurs. 2009;32:465–72. doi: 10.1097/NCC.0b013e3181aaf124. [DOI] [PubMed] [Google Scholar]
- 23.Tavafian SS, Hasani L, Aghamolaei T, Zare S, Gregory D. Prediction of breast self-examination in a sample of Iranian women: An application of the Health Belief Model. BMC Womens Health. 2009;9:37. doi: 10.1186/1472-6874-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harirchi I, Mousavi SM, Mohagheghi MA, Mousavi-Jarrahi A, Ebrahimi M, Montazeri A, et al. Early detection for breast cancer in iran. Asian Pac J Cancer Prev. 2009;1D:849–51. [PubMed] [Google Scholar]


