Abstract
Background
A common problem among patients with chronic diseases is poor adherence with prescribed medication. Studies have shown that certain interventions can improve adherence and clinical outcomes.
Methods
We selectively searched the PubMed database for publications on the treatment of hypertension that contained the terms “adherence,” “drug,” “treatment, “outcome,” “hypertension,” and “randomized controlled trial.”
Results
The interventions studied were highly varied, ranging from the use of calendar blister packs to complex patient education programs. 62% of the studies that we identified documented an improvement in adherence after an intervention (median Cohen’s d = 0.52). In 92% of cases, improved adherence was associated with a significant improvement in clinical end points (median Cohen’s d = 0.34).
Conclusion
The promotion of adherence to prescribed medication is clearly desirable. Studies on the treatment of hypertension have shown that attempts to improve adherence often fail. In most studies, however, improved adherence led to better clinical outcomes. Simplification of drug regimens (e.g., reducing the number of pills taken per day) is the single most effective way to promote adherence. Moreover, the findings of studies on the treatment of hypertension and other diseases suggest that shared decision-making should be the basis of physician-patient discussions about medication. Suitable medications can also be chosen in order to maximize safety and efficacy even if adherence is incomplete. It would also be desirable for studies on the promotion of adherence to be carried out in Germany, under the specific conditions that prevail in our national health-care system.
The term “compliance,” which was used most often in the past, is often understood from a perspective of a paternalistic or maternalistic role of the treating health professional, in the sense of not following the drug regimen prescribed by the doctor. The term “adherence,” which is the preferred term today, is based on the therapeutic alliance between patient and treating physician and thus explicitly refers to responsibilities on both sides. The concept of shared decision making can be considered as accepted in this setting (Box 1) (1, e1– e3). It is also consistent with the definition of adherence as proposed by the World Health Organization (WHO): “The extent to which a person’s behavior—taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider” (2). Adherence in the wider sense describes the extent to which a patient follows a treatment plan. In industrialized countries, medication adherence for chronic diseases is often only around 50% (2). The forms and patterns of adherence (or non-adherence) with medication and the parameters for measuring these are varied. The measure used most often is determining the proportion of drug doses that are prescribed and then actually taken. According to Dunbar, adherence and its measurement can be placed in one of three categories (3). The first category is that of the quantity of medication, and further differentiation comes under that category—for example, between the proportion of medical drugs taken relative to the doses laid out in the treatment plan (the prescribed doses), the proportion of medications taken in the correct dosage, or the taking of the medication doses at the time stipulated in the treatment plan (4– 6). The term “persistence” describes the proportion of patients who (still) follow the prescribed drug treatment at all, or “the duration of time from initiation to discontinuation of therapy” (4, 5). Depending on the observation period, it is difficult to distinguish between non-persistence and temporary drug holidays. Relative to the overall prevalence of non-persistence, primary non-persistence—that is, a situation in which a prescribed medication regimen is not even started—represents a lower proportion of patients, at 5%, but still a relevant proportion (4, e4– e6). Dunbar’s second category attempts a qualitative evaluation of adherence as “good” or “poor” (non-adherence) (3). However, the definition of what is considered “good” adherence varies notably in different studies—for example, with threshold values of = 80% to = 95% regarding the ingestion of prescribed doses (6). The third category comprises combined adherence indices that associate different behaviors (for example, taking medication, turning up for doctor’s appointments, abstaining from nicotine) and/or awareness/knowledge (for example, about the treatment or disorder).
Box 1. Shared decision making in the therapeutic setting (1).
The interaction between doctor and patient aims to identify the appropriate therapy by reaching a decision jointly by means of communication
This entails explaining the current scientific evidence on the background of a doctor–patient partnership orientation.
The best possible decision about therapy should be reached according to clinical demands and by recognizing the patient’s preferences.
Studies have shown that low adherence is associated with a reduction or total absence of therapeutic success, reduced quality of life, and higher treatment costs, among others; good adherence, by contrast, is associated with lower mortality in clinical studies (2, 7, 8). Many studies have been conducted of the question of which factors can influence adherence with medication and of which measures can increase compliance with regard to medication therapy (2, 6, 9, e7– e10). In this article, we provide an overview of studies that investigated whether measures to promote adherence influenced compliance on the one hand and clinical end points on the other hand. Our focus was on studies of arterial hypertension, since hypertension is a clinically relevant example of a common disorder with serious consequences, which can be treated effectively, but whose therapy in all experience has been associated with unsatisfactory adherence (2, 10, e11, e12).
Methods
We conducted a PubMed search using the search terms “adherence,” “drug,” “treatment,” “outcome,” “hypertension,” and “randomized controlled trial,” without any restrictions on date of publication. We identified in the search results the prospective, randomized, controlled studies of antihypertensive therapy, in which effects were reported for end points regarding adherence to medication as well as lowering of blood pressure. Further inclusion criteria were: a rate of participants dropping out of the study of <20% and an observation period of at least six months. Our research results were compared with and augmented by a meta-analysis by Kripalani et al. and a review article by Haynes et al. (11, 12). See eBox for the effect size calculation.
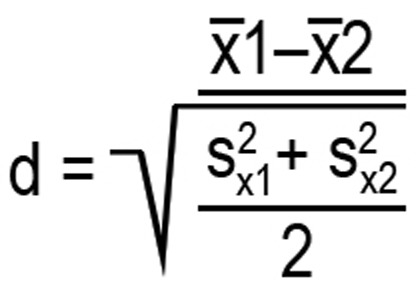
eBOX. Effect size.
The effect sizes were estimated according to Cohen’s d by using the following formula:
Results
The PubMed search yielded 88 hits for the search terms used; the number was reduced further by 16 by restricting the selection to the article type “clinical trial.” The remaining publications included 21 randomized clinical intervention studies of end points regarding hypertension and adherence. Two of these studies were excluded as the results regarding adherence were not shown (e13, e14). Five of the remaining 19 studies did not meet the inclusion criteria rate of study dropouts <20% or a minimum observation period of six months (e15– e19). Seven further studies that met the requirements were taken from the articles by Kripalani et al. and Haynes et al. (11, 12).
As expected, very different measures aiming to promote adherence were studied, ranging from the use of calendar blister packs to combination preparations to comprehensive educational events, regular personal encounters, or the use of telephone based computer systems (Table 1). Many studies combined several measures (complex interventions). The adherence end points were similarly heterogeneous and ranged from patients’ self assessments on the basis of validated scores to the proportion of drug prescriptions actually filled to electronic registration of frequency and timing of medication intake. Clinical end points comprised systolic and/or diastolic blood pressure measurements, their decrease during the study period, or achieving the target blood pressure. Blood pressure measurements were partly taken on an outpatient basis, partly in hospitals or doctors’ offices.
Table 1a. Randomized controlled studies of therapy with antihypertensive drugs, in which the intervention under study had positive effects on adherence as well as on clinical end points.
| Study | Type of intervention/case numbers (control vs intervention) | Effects on adherence and clinical end points |
|---|---|---|
| (13) |
|
After 6 months:
|
| (14) |
|
After 6 months:
|
| (15) |
|
After 6 months:
|
| (16) |
|
After 6 months:
|
| (17) |
|
After 6 months:
|
| (18) |
|
After 6 months:
|
| (19) |
|
After 9 months:
|
| (20) |
|
After 36 months:
|
| (22) |
|
Over 6 months:
|
| (23) |
|
After 6 months:
|
| (24) |
|
Over 12 months:
|
| (25) |
|
After 6 months:
|
* Statistically significant effects in favor of the intervention group (as a rule p<0.05);
n.s.: non-significant, ES: effect size, estimated as Cohen’s d.
13 of the 21 studies (62%) showed a positive effect of the intervention under study on adherence compared with a control group (Table 1a, b) (13– 25); eight studies did not (Table 1c, eTable) (26– 33). In 12 of the 13 studies showing a positive effect on adherence, at least one end point regarding antihypertensive therapy improved (Table 1a), in one study this was not the case (21). One study showed a significant improvement in clinical end points, but not of the collected adherence parameters (Table 1c) (31). The effect sizes estimated by using Cohen’s d varied regarding the adherence end points from small to large (0.29–2.89), with a median of 0.52. Regarding the hypertension end points, the effect sizes were mostly small (0.16–0.80, median 0.34).
Table 1b. Randomized controlled study of antihypertension therapy, in which the intervention under study had a positive effect on adherence but not on clinical end points.
| Study | Type of intervention / case numbers (control vs intervention) | Effects on adherence and clinical end points |
|---|---|---|
| (21) |
|
After 12 months:
|
* Statistically significant effects in favor of the intervention group (as a rule p<0.05);
n.s.: non-significant
Tabelle 1c. Randomized controlled study of antihypertension therapy, in which the intervention under study had no positive effect on adherence but on clinical end points.
| Study | Type of intervention / case numbers (control vs intervention) | Effects on adherence and clinical end points |
|---|---|---|
| (31) |
|
|
*Statistically significant effects in favor of the intervention group (as a rule p<0.05); n.s.: non-significant statistically when comparing the groups with one another; # p = 0.07
eTable. Randomized controlled studies of therapy with antihypertensive drugs, in which neither adherence nor clinical end points were affected in favor of the intervention under study.
| Study | Type of intervention / case numbers (control vs intervention) | Effects on adherence and clinical end points |
|---|---|---|
| (26) |
|
After 3 months:
|
| (27) |
|
After 6 months:
|
| (28) |
|
After 6 months:
|
| (29) |
|
After 1, 3, and 6 months:
|
| (30) |
|
After 12 months:
|
| (32) |
|
After 6 months:
|
| (33) |
|
After 6 months:
|
n.s.: statistically not significant when comparing groups with one another
Discussion
Using the example of antihypertensive medication, we found that of 21 randomized controlled studies of the effect of adherence-promoting measures on clinical end points, only 13 affected therapeutic compliance positively. The finding is consistent with other reviews and meta-analyses of various diseases, where 30–50% of studies did not show that the measures under study improved adherence (10– 12, 34). On the other hand, it should be noted that 12 out of 13 studies (92%) in which compliance was affected positively showed additional significant effects on antihypertensive treatment end points in the intervention groups. Kripalani et al. conducted a meta-analysis of intervention studies for different diseases (12). For those studies that improved adherence as well as clinical end points, these authors found rather remarkable effect sizes compared with control groups (here: Cohen’s d): 0.27–0.89 (median 0.55) for adherence and 0.29–1.58 (median 0.66) for clinical end points. In the studies on hypertension treatment that were analyzed for the present work, the effects sizes for the clinical end points were markedly lower. In terms of limitations, one has to note that in the studies considered by Kripalani et al. and by us that found positive effects regarding adherence, often only a proportion of the end points that had been defined a priori were significantly affected.
In some studies included in our review it seems easy to explain why they did not yield positive results. One study was successful in terms of the hypertension end points, but the effect on adherence did not reach significance (p = 0.07) (31). The calculated statistical power regarding the adherence end point was not reached, because the number of included patients was notably below the intended number (111 and 112, instead of two groups of 250 each). In another study, adherence at baseline was as high as 98%, blood pressure regulation was initially also already good, at <140/80 mm Hg (29). Even if an improvement in adherence could have been noted in this setting it is highly questionable whether this would have sufficed for a clinically relevant effect on blood pressure.
A comparison of the studies we identified did not clearly show what makes an intervention effective, or more effective than others. One reason, among others, is that most studies combined several individual measures. Kripalani et al. in their meta-analysis concluded that individual measures that target medication intake behavior directly, are most likely to be successful regarding adherence and are most effective, primarily those that aim to simplify therapeutic schemes (for example, a reduction in the daily number of medication intakes, or packaging medications in calendar blister packs; Cohen’s d as effect size [ES]: 0.89–1.20) (12). In the hypertension studies we identified, using calendar blister packs in one case improved both adherence and blood-pressure control; in another study, the outcome was unsuccessful for compliance as well as antihypertension treatment. A study investigating the use of fixed combinations of antihypertensive drugs was unsuccessful, which seems to be due to the baseline conditions (29). The data are not sufficient to assess the use of the much discussed polypill, which contains substances to treat different disorders and diseases, even though indications are that adherence is improved compared with the use of monopreparations (e20, e21). The reasons for a lack of adherence are multifarious and comprise the diversest of factors (Box 2) (2, 9, 10, 35, 36). The list of factors with a negative impact can be contrasted with a list of adherence-promoting factors that mirrors it in many instances (Box 2) (9, 35, 36). Accordingly, Kripalani et al. found improved adherence for other measures too. These included, for example, improved information for patients (for example, individual training sessions or group training, printed information materials; ES 0.35–1.13), testing patients’ knowledge and awareness (for example, during personal conversation or via computer communication; ES 0.27–0.81), or a close observation period (including the use of reminders; ES 0.43–0.86) and adherence monitoring (ES 0.27–1.20) (12). The latter two items are among the successful educational interventions that many studies have consistently indicated (10– 12). Of note is the fact that the effect sizes of the more complex interventions range between weak and strong (ES 0.43–1.2) and that the combination of different approaches does not necessarily bring about any further improvement of the effect on adherence (12). Many of the studied interventions are part of strategies that can be used to pursue the concept of shared decision making (1, e22). Indeed, promoting shared decision making can, in suitable patients, improve therapeutic success, as has been shown by a study of hypertension treatment (37). However, data on this issue from clinical studies are insufficient so far.
Box 2. Factors that influence adherence.
-
Factors that improve adherence (2, 10, 35, 36):
Long term medication intake (>5 years) (35)
Awareness of the necessity of long term treatment
Low number of daily drug intakes
Older age (for example, >60 years for anticonvulsive or antihypertensive drugs) (2, e23)
Marital status: married
Social support
Satisfied with the therapy
Experience of effectiveness
Systematic, close follow-up
Good awareness and knowledge of therapy
hort waiting times when visiting the doctor and between visits
-
Factors that impair adherence (2, 35, 36):
Chronic disorder
Few or no symptoms
Long duration of treatment
Several doses required every day (from only >2/d) (9)
Complex treatment schemes
Adverse effects or fear of such effects
Measures that impair everyday life
Younger age (for example, <60 years for antihypertensive medication) (e23, e24)
Male, single
Low level of education
Lack of support
Lack of communication between doctor and patient
No or insufficient information
Ignoring the problems with adherence
It seems obvious to conclude that the selection of the drug can contribute to improving adherence if one considers that the reasons for non-adherence include adverse drug effects (possibly specific to the effective substance). The side effect profiles are thus being discussed in association with data on current hypertensive drugs of choice, according to which adherence seems best for therapy with angiotensin 1 receptor blockers (38). Furthermore it seems plausible that pharmacotherapy should be planned while fully expecting unsatisfactory compliance. A concept that may be useful in this setting is that of “forgiving” drugs. The extent to which a medical drug “forgives” if it is taken irregularly depends, among others, on the rate at which its effect wears off (“off-rate”) and the time taken until its effect sets in (again). An analysis of simulated treatments over a time period of 256 days showed that for many hypertensive drugs, a mean intake of 75% of prescribed doses means that a significantly impaired mean blood pressure reduction is to be expected (39). According to the study, however, no loss of systolic blood pressure reduction would be expected for amlodipine (off-rate <1 mm Hg/d), whereas for enalapril (off-rate 12 mm Hg/d) the reduction is only about 10 mm Hg with an otherwise equally effective dose. It should be noted, however, that to our knowledge, no clinical end point studies of the concept of forgiving antihypertensive drugs exist so far.
Summary and conclusion
Attempts to improve medical adherence have often failed, which is confirmed by the available studies of hypertension treatment. If improvement of adherence is successful, however, positive effects for clinical end points can also be expected for many of the patients. Studies of different diseases have shown that measures to simplify medication therapy schemes, such as reducing the number of tablets and the frequency of intake, are the most effective single measures to improve adherence, and they are rather easy to implement. Further effective measures include, for example, patient information about their disease and treatment (positive and negative aspects), active integration of patients, and consideration of factors affecting adherence in general (Box 2) as well as of individual possibilities and needs. This supports the recommendation of making shared decision making (Box 1) the basic principle of the prescribing consultation (2, 40). In case individual measures are not sufficiently effective, complex interventions may be considered, such as are available in the context of “patient education on hypertension” and rehabilitation measures, for example. The individual selection of suitable medications should consider the adherence that is to be expected and, if needed, it can be shaped in such a way that the medication therapy is as effective and safe as possible, even in case of unsatisfactory compliance.
Key Messages.
Adherence with medication is unsatisfactory for chronic disorders such as arterial hypertension.
Randomized controlled studies of promoting adherence in antihypertensive therapy have shown an improvement in adherence in 60% of patients, which in the majority of studies was associated with improvement in at least one clinical end point.
The most effective single measures to promote adherence are based on simplifying therapeutic schemes.
Many adherence-promoting measures entail the active integration of the patient in the therapy, so that for example shared decision making as the basis of the consultation seems worth recommending.
By selecting suitable medication, adherence promotion can be supported while at the same time counteracting unsatisfactory adherence.
Acknowledgments
Translated from the original German by Dr Birte Twisselmann.
Footnotes
Conflict of interest statement
Professor Albus has received honoraria for consulting from UCB Pharma. He has received honoraria from Berlin Chemie and Actelion Pharmaceuticals for preparing continuing medical education events.
Dr Matthes declares that no conflict of interest exists.
References
- 1.General Medical Council. 2008. Consent: patients and doctors making decisions together. [Google Scholar]
- 2.Sabaté E. Geneva, Switzerland: World Health Organization; 2003. Adherence to long-term therapies: evidence for action. [Google Scholar]
- 3.Dunbar J. Adherence measures and their utility. Control Clin Trials. 1984;5:515–521. doi: 10.1016/0197-2456(84)90012-6. [DOI] [PubMed] [Google Scholar]
- 4.Blaschke TF, Osterberg L, Vrijens B, Urquhart J. Adherence to medications: insights arising from studies on the unreliable link between prescribed and actual drug dosing histories. Annu Rev Pharmacol Toxicol. 2012;52:275–301. doi: 10.1146/annurev-pharmtox-011711-113247. [DOI] [PubMed] [Google Scholar]
- 5.Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11:44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- 6.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 7.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 8.Simpson SH, Eurich DT, Majumdar SR, et al. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ. 2006;333 doi: 10.1136/bmj.38875.675486.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Möbes J. Compliance: Neue Positionen am Beispiel des Diabetes mellitus. Z Allg Med. 2003;79:238–243. [Google Scholar]
- 10.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028–3035. doi: 10.1161/CIRCULATIONAHA.108.768986. [DOI] [PubMed] [Google Scholar]
- 11.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD000011.pub3. CD000011. [DOI] [PubMed] [Google Scholar]
- 12.Kripalani S, Yao X, Haynes RB. Interventions to enhance medication adherence in chronic medical conditions: a systematic review. Arch Intern Med. 2007;167:540–550. doi: 10.1001/archinte.167.6.540. [DOI] [PubMed] [Google Scholar]
- 13.Friedman RH, Kazis LE, Jette A, et al. A telecommunications system for monitoring and counseling patients with hypertension. Impact on medication adherence and blood pressure control. Am J Hypertens. 1996;9:285–292. doi: 10.1016/0895-7061(95)00353-3. [DOI] [PubMed] [Google Scholar]
- 14.Haynes RB, Sackett DL, Gibson ES, et al. Improvement of medication compliance in uncontrolled hypertension. Lancet. 1976;1:1265–1268. doi: 10.1016/s0140-6736(76)91737-2. [DOI] [PubMed] [Google Scholar]
- 15.Jarab AS, Alqudah SG, Mukattash TL, Shattat G, Al-Qirim T. Randomized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J Manag Care Pharm. 2012;18:516–526. doi: 10.18553/jmcp.2012.18.7.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA. 2006;296:2563–2571. doi: 10.1001/jama.296.21.joc60162. [DOI] [PubMed] [Google Scholar]
- 17.Marquez Contreras E, Vegazo Garcia O, Claros NM, et al. Efficacy of telephone and mail intervention in patient compliance with antihypertensive drugs in hypertension. ETECUM-HTA study. Blood Press. 2005;14:151–158. doi: 10.1080/08037050510008977. [DOI] [PubMed] [Google Scholar]
- 18.Marquez-Contreras E, Martell-Claros N, Gil-Guillen V, et al. Efficacy of a home blood pressure monitoring programme on therapeutic compliance in hypertension: the EAPACUM-HTA study. J Hypertens. 2006;24:169–175. doi: 10.1097/01.hjh.0000198023.53859.a2. [DOI] [PubMed] [Google Scholar]
- 19.Morgado M, Rolo S, Castelo-Branco M. Pharmacist intervention program to enhance hypertension control: a randomised controlled trial. Int J Clin Pharm. 2011;33:132–140. doi: 10.1007/s11096-010-9474-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Obreli-Neto PR, Guidoni CM, de Oliveira Baldoni A, et al. Effect of a 36-month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patients. Int J Clin Pharm. 2011;33:642–649. doi: 10.1007/s11096-011-9518-x. [DOI] [PubMed] [Google Scholar]
- 21.Ogedegbe GO, Boutin-Foster C, Wells MT, et al. A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive African Americans. Arch Intern Med. 2012;172:322–326. doi: 10.1001/archinternmed.2011.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pladevall M, Brotons C, Gabriel R, et al. Multicenter cluster-randomized trial of a multifactorial intervention to improve antihypertensive medication adherence and blood pressure control among patients at high cardiovascular risk (the COM99 study) Circulation. 2010;122:1183–1191. doi: 10.1161/CIRCULATIONAHA.109.892778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rudd P, Miller NH, Kaufman J, et al. Nurse management for hypertension. A systems approach. Am J Hypertens. 2004;17:921–927. doi: 10.1016/j.amjhyper.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 24.Schneider PJ, Murphy JE, Pedersen CA. Impact of medication packaging on adherence and treatment outcomes in older ambulatory patients. J Am Pharm Assoc (2003) 2008;48:58–63. doi: 10.1331/JAPhA.2008.07040. [DOI] [PubMed] [Google Scholar]
- 25.Sookaneknun P, Richards RM, Sanguansermsri J, Teerasut C. Pharmacist involvement in primary care improves hypertensive patient clinical outcomes. Ann Pharmacother. 2004;38:2023–2028. doi: 10.1345/aph.1D605. [DOI] [PubMed] [Google Scholar]
- 26.Becker LA, Glanz K, Sobel E, Mossey J, Zinn SL, Knott KA. A randomized trial of special packaging of antihypertensive medications. J Fam Pract. 1986;22:357–361. [PubMed] [Google Scholar]
- 27.de Castro MS, Fuchs FD, Santos MC, et al. Pharmaceutical care program for patients with uncontrolled hypertension. Report of a double-blind clinical trial with ambulatory blood pressure monitoring. Am J Hypertens. 2006;19:528–533. doi: 10.1016/j.amjhyper.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 28.Johnson AL, Taylor DW, Sackett DL, Dunnett CW, Shimizu AG. Self-recording of blood pressure in the management of hypertension. Can Med Assoc J. 1978;119:1034–1039. [PMC free article] [PubMed] [Google Scholar]
- 29.Matsumura K, Arima H, Tominaga M, et al. Does a combination pill of antihypertensive drugs improve medication adherence in Japanese? A randomized controlled trial. Circ J. 2012;76:1415–1422. doi: 10.1253/circj.cj-11-1481. [DOI] [PubMed] [Google Scholar]
- 30.Ogedegbe G, Chaplin W, Schoenthaler A, et al. A practice-based trial of motivational interviewing and adherence in hypertensive African Americans. Am J Hypertens. 2008;21:1137–1143. doi: 10.1038/ajh.2008.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rinfret S, Lussier MT, Peirce A, et al. The impact of a multidisciplinary information technology-supported program on blood pressure control in primary care. Circ Cardiovasc Qual Outcomes. 2009;2:170–177. doi: 10.1161/CIRCOUTCOMES.108.823765. [DOI] [PubMed] [Google Scholar]
- 32.Sackett DL, Haynes RB, Gibson ES, et al. Randomised clinical trial of strategies for improving medication compliance in primary hypertension. Lancet. 1975;1:1205–1207. doi: 10.1016/s0140-6736(75)92192-3. [DOI] [PubMed] [Google Scholar]
- 33.Schroeder K, Fahey T, Hollinghurst S, Peters TJ. Nurse-led adherence support in hypertension: a randomized controlled trial. Fam Pract. 2005;22:144–151. doi: 10.1093/fampra/cmh717. [DOI] [PubMed] [Google Scholar]
- 34.McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA. 2002;288:2868–2879. doi: 10.1001/jama.288.22.2868. [DOI] [PubMed] [Google Scholar]
- 35.Kjellgren KI, Ahlner J, Saljo R. Taking antihypertensive medication-controlling or co-operating with patients? Int J Cardiol. 1995;47:257–268. doi: 10.1016/0167-5273(94)02203-u. [DOI] [PubMed] [Google Scholar]
- 36.Melnikow J, Kiefe C. Patient compliance and medical research: issues in methodology. J Gen Intern Med. 1994;9:96–105. doi: 10.1007/BF02600211. [DOI] [PubMed] [Google Scholar]
- 37.Deinzer A, Babel H, Veelken R, Kohnen R, Schmieder RE. [Shared decision-making with hypertensive patients. Results of an implementation in Germany] Dtsch Med Wochenschr. 2006;131:2592–2596. doi: 10.1055/s-2006-956254. [DOI] [PubMed] [Google Scholar]
- 38.Kronish IM, Woodward M, Sergie Z, Ogedegbe G, Falzon L, Mann DM. Meta-analysis: impact of drug class on adherence to antihypertensives. Circulation. 2011;123:1611–1621. doi: 10.1161/CIRCULATIONAHA.110.983874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lowy A, Munk VC, Ong SH, et al. Effects on blood pressure and cardiovascular risk of variations in patients’ adherence to prescribed antihypertensive drugs: role of duration of drug action. Int J Clin Pract. 2011;65:41–53. doi: 10.1111/j.1742-1241.2010.02569.x. [DOI] [PubMed] [Google Scholar]
- 40.Perk J, De Backer G, Gohlke H, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) Eur Heart J. 2012;33:1635–1701. doi: 10.1093/eurheartj/ehs092. [DOI] [PubMed] [Google Scholar]
- e1.Dwamena F, Holmes-Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev. 2012;12 doi: 10.1002/14651858.CD003267.pub2. CD003267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e2.Legare F, Ratte S, Stacey D, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD006732.pub2. CD006732. [DOI] [PubMed] [Google Scholar]
- e3.Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD001431.pub3. CD001431. [DOI] [PubMed] [Google Scholar]
- e4.Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25:284–290. doi: 10.1007/s11606-010-1253-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e5.Karter AJ, Parker MM, Moffet HH, Ahmed AT, Schmittdiel JA, Selby JV. New prescription medication gaps: a comprehensive measure of adherence to new prescriptions. Health Serv Res. 2009;44(5 Pt 1):1640–1661. doi: 10.1111/j.1475-6773.2009.00989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e6.Raebel MA, Ellis JL, Carroll NM, et al. Characteristics of patients with primary non-adherence to medications for hypertension, diabetes, and lipid disorders. J Gen Intern Med. 2012;27:57–64. doi: 10.1007/s11606-011-1829-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e7.Krueger KP, Berger BA, Felkey B. Medication adherence and persistence: a comprehensive review. Adv Ther. 2005;22:313–356. doi: 10.1007/BF02850081. [DOI] [PubMed] [Google Scholar]
- e8.Mahtani KR, Heneghan CJ, Glasziou PP, Perera R. Reminder packaging for improving adherence to self-administered long-term medications. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD005025.pub3. CD005025. [DOI] [PubMed] [Google Scholar]
- e9.McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA. 2002;288:2868–2879. doi: 10.1001/jama.288.22.2868. [DOI] [PubMed] [Google Scholar]
- e10.Schedlbauer A, Davies P, Fahey T. Interventions to improve adherence to lipid lowering medication. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD004371.pub3. CD004371. [DOI] [PubMed] [Google Scholar]
- e11.Burke TA, Sturkenboom MC, Lu SE, Wentworth CE, Lin Y, Rhoads GG. Discontinuation of antihypertensive drugs among newly diagnosed hypertensive patients in UK general practice. J Hypertens. 2006;24:1193–1200. doi: 10.1097/01.hjh.0000226211.95936.f5. [DOI] [PubMed] [Google Scholar]
- e12.Sackett DL, Haynes RB, Gibson ES, Taylor DW, Roberts RS, Johnson AL. Patient compliance with antihypertensive regimens. Patient Couns Health Educ. 1978;1:18–21. doi: 10.1016/s0738-3991(78)80033-0. [DOI] [PubMed] [Google Scholar]
- e13.Heisler M, Hofer TP, Schmittdiel JA, et al. Improving blood pressure control through a clinical pharmacist outreach program in patients with diabetes mellitus in 2 high-performing health systems: the adherence and intensification of medications cluster randomized, controlled pragmatic trial. Circulation. 2012;125:2863–2872. doi: 10.1161/CIRCULATIONAHA.111.089169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e14.Wakefield BJ, Holman JE, Ray A, et al. Effectiveness of home telehealth in comorbid diabetes and hypertension: a randomized, controlled trial. Telemed J E Health. 2011;17:254–261. doi: 10.1089/tmj.2010.0176. [DOI] [PubMed] [Google Scholar]
- e15.Christensen A, Christrup LL, Fabricius PE, et al. The impact of an electronic monitoring and reminder device on patient compliance with antihypertensive therapy: a randomized controlled trial. J Hypertens. 2010;28:194–200. doi: 10.1097/HJH.0b013e328331b718. [DOI] [PubMed] [Google Scholar]
- e16.Planas LG, Crosby KM, Mitchell KD, Farmer KC. Evaluation of a hypertension medication therapy management program in patients with diabetes. J Am Pharm Assoc (2003) 2009;49:164–170. doi: 10.1331/JAPhA.2009.08164. [DOI] [PubMed] [Google Scholar]
- e17.Wetzels GE, Nelemans PJ, Schouten JS, et al. Electronic monitoring of adherence as a tool to improve blood pressure control. A randomized controlled trial. Am J Hypertens. 2007;20:119–125. doi: 10.1016/j.amjhyper.2006.07.018. [DOI] [PubMed] [Google Scholar]
- e18.Bogner HR, de Vries HF. Integration of depression and hypertension treatment: a pilot, randomized controlled trial. Ann Fam Med. 2008;6:295–301. doi: 10.1370/afm.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e19.Alhalaiqa F, Deane KH, Nawafleh AH, Clark A, Gray R. Adherence therapy for medication non-compliant patients with hypertension: a randomised controlled trial. J Hum Hypertens. 2012;26:117–126. doi: 10.1038/jhh.2010.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e20.Endres M, Heuschmann PU, Laufs U, Hakim AM. Primary prevention of stroke: blood pressure, lipids, and heart failure. Eur Heart J. 2011;32:545–552. doi: 10.1093/eurheartj/ehq472. [DOI] [PubMed] [Google Scholar]
- e21.Gaziano TA, Opie LH, Weinstein MC. Cardiovascular disease prevention with a multidrug regimen in the developing world: a cost-effectiveness analysis. Lancet. 2006;368:679–686. doi: 10.1016/S0140-6736(06)69252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e22.Elwyn G, Edwards A, Mowle S, et al. Measuring the involvement of patients in shared decision-making: a systematic review of instruments. Patient Educ Couns. 2001;43:5–22. doi: 10.1016/s0738-3991(00)00149-x. [DOI] [PubMed] [Google Scholar]
- e23.Hyre AD, Krousel-Wood MA, Muntner P, Kawasaki L, DeSalvo KB. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertens (Greenwich) 2007;9:179–186. doi: 10.1111/j.1524-6175.2007.06372.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e24.Caldwell JR, Cobb S, Dowling MD, de Jongh D. The dropout problem in antihypertensive treatment. A pilot study of social and emotional factors influencing a patient’s ability to follow antihypertensive treatment. J Chronic Dis. 1970;22:579–592. doi: 10.1016/0021-9681(70)90034-2. [DOI] [PubMed] [Google Scholar]


