Abstract
Background:
Heparin is one of the most important medication that is used in coronary artery bypass graft (CABG) operations, but some patients demonstrate heparin resistance (HR) during CABG. Heparin resistance was defined as at least one activated clothing time <400 seconds after heparinization and/or the need for purified antithrombin III (AT-III) administration. The goal of this study was the investigation of HR prevalence in our country and relation between HR and post-operative CABG complications.
Materials and Methods:
One hundred patients that candidate for CABG were selected and surveyed for HR and complications. The data entered to computer and analyzed by SPSS soft ware. The Chi-square and student t-tests were used for data analysis.
Results:
The prevalence of heparin resistance in our study was 3%. There was no relation among bleeding, cardiac arrest and HR. Bleeding happened in 13 patients of which 1 person was in HR group (33.3%) and 12 in non HR group (12.4%) (P = 0.34). Cardiac arrest happened in 8 patients, 1 person was in HR group (33.3%) and 7 in non HR group (7.2%) (P = 0.22). According our data there were no relation among HR and gender and ventilator dependency time.
Conclusions:
HR is a nearly prevalent complication among patients that undergone CABG that may led to some complications such as bleeding and cardiac arrest. In our study, we did not find significant relation among them, but in frequency these complications were higher in HR group.
Keywords: Bleeding, coronary artery bypass graft, heparin, heparin complication, heparin resistance
INTRODUCTION
One of the greatest advances in the angina treatment is coronary artery bypass graft (CABG) surgery. The word bypass means by-way, since in the bypass surgery, surgeon removes the legs or chest arteries and use them as a bypass for blocked coronary artery, so the surgery has been named as bypass.[1,2,3] Transfusion of patient blood circulation to heart-lung pump or cardiopulmonary bypass circuit (CPB circuit) in coronary bypass surgery is an essential component of operation. To address this pump, blood is likely to increase coagulation. Heparin has been used to avoid increasing of the coagulability during the surgery. Heparin is a Glykouzamino Glykan Sulfathast that has been used as an injectable anticoagulant drug. Heparin is a natural biological molecule and it also has been made artificially. Heparin has been known as the great negative charge density between the others biological molecules. Heparin plays its blood anticoagulant role by the effect of inhibitory on the blood coagulation factors and increases the domestic anti-thrombin III (AT III). Heparin tolerance has been reported in a lot of patients undergoing CABG and statistics shows that the incidence of this event is increasing.[4,5,6,7,8] Heparin resistance was defined as ACT < 400 seconds after heparinization or need to purified AT III.[9] Complication of heparin tolerance is varied from the effects of sub clinical disorders to severe coagulation and catastrophic in the CPB circuit.[1,7,8] The causes of heparin tolerance can be multi-factorial, such as AT III deficiency due to preoperative use of heparin, thrombocytopenia and increased activity of Factor VIII, and it should be previous history of endocarditic and IABP.[7,8,9,10,11,12] Due to increasing the cardiopulmonary disease and therefore statistical increases of CABG requiring, the importance of heparin tolerance is more visible in CABG. On the other hand by determining the heparin tolerance in a patient, we will be able to be ready for dealing with the consequences of HR. Heparin tolerance outcomes included death, arrhythmias, bleeding, cardiac arrest, requiring intubation, increasing duration of staying in ICU, increasing the duration of mechanical ventilation.[10] The overall objective of this study was to determine the frequency distribution of heparin tolerance during coronary bypass surgery during the year 2011.
MATERIALS AND METHODS
This is a cross sectional study that was done at Chamran hospital in the year 2011. The study population consisted of patient's candidates for CABG (coronary artery bypass graft surgery) who had operated during the year 2011. Entry criteria included the patients who underwent CABG, without aortic balloon pumping before operation and no need emergency surgeries. Exclusion criteria included the patient who died during or before ICU admission. The sample size for this study was estimated to 96 person, for more sure 100 patients undergoing bypass surgery were evaluated. The sampling method was easy and the patients undergoing CABG who had frequently qualified were elected to enter the study sample, so the size number reached sufficient level. After selecting the patients, their age, sex and weight were determined and PT, aPTT, INR and the Plt (platelet) count factors was checked, and then general anesthesia was performe. Before connecting patients to the CPB pump a dose of heparin (400 U/Kg) was injected. Five minutes later, ACT was measured with the device, if ACT was more than 400-ACT >400-the patient was proceeding on CPB pump but if ACT was less than 400- ACT < 400-it was considered as resistant to heparin and second dose of heparin would be injected. Five minutes later, ACT was checked again and if it was less than 400-ACT <400-FFP or purified AT III was used to overcome HR. At the end of the CABG, heparin neutralize with protamine sulfate at a ratio of one to one was done. Patients in the study were studied of other variants such as complications of heparin resistance, mortality, length of stay in ICU and the duration of receiving mechanical ventilation and the obtained information was recorded in a specific checklist that were prepared for this purpose. Finally, the obtained data was entered in the computer and analysis was performed by SPSS18 software. For the information analysis, student t-test and Chi-square test statistic were used.
RESULTS
In this study, 100 patients undergone coronary artery bypass surgery were evaluated. The average age of them was 60.8 ± 9.4 years with the range of 37-79 years, 52 patients were women and 48 of them were men. The average age of women was 60.4 ± 9.7 and for men was 61.2 ± 9.2 years, according to t-test, there was no significant difference between two genders [Table 3]. In this study, the patient's occupations were: 11 workers, one crew, 22 employees, 14 retired and 52 housewives. According to the results in 3 patients heparin tolerance was observed (ACT levels were less than 400), two of them were woman and one in men group (3.8% vs. 2.1%). Furthermore, there was no significant difference between two genders base on the Fisher exact test (P = 0.99) [Table 3]. The results are shown in Table 1. Table 2 shows the frequency of complications in terms of the resistance and no resistance to heparin. According to this table, 31 cases of undergoing studies had arrhythmia and also among two groups, resistant and non-resistant to heparin, respectively, 2 and 29 cases arrhythmia was observed (66.7% vs. 29.9%), but statistical Fisher Test showed no significant relation between arrhythmia and heparin resistance (P = 0.23). The bleeding was occurred in 13 patients and one of them had heparin resistant and 12 of them were from non-resistant heparin group (12.4% vs. 33.3%), and according to the Fisher exact test, there was no significant correlation between resistance to heparin and bleeding (P = 0.34). Cardiopulmonary arrest also occurred in 8 patients, arrest occurred in both resistant and non-resistant to heparin, respectively, there were 1 and 7 (33.3% and 7.2%) and according to the Fisher exact test, there was no significant correlation between the heparin-resistant and arrest incidence, (P = 0.22), although these complications were slightly higher in HR group. The mean total dose of heparin administered to patients was 34899 ± 17108 units. Minimum and maximum injected dose of heparin were 16800 and 120000 units. The mean injected of heparin dose in men 36085 ± 16515 and in women were 33804 ± 17726 unit, and in the test there was no significant difference between sexes (P = 0.51) by t-test. Average dose of heparin used in both resistant and non-resistant to heparin were 52200 ± 23705 and 34363 ± 16747. According t-test, the average dose of heparin-resistant and non-durable consumption in the two groups, had no significant difference (P = 0.08). Mean of ACT in the patients was 599.3 ± 145, respectively. Minimum and maximum amounts of ACT in these patients were 350 and 940, respectively. Also index mean, in the men and women were 617.7 ± 146.7 and 582.3 ± 142.7 and according to t-test, there was no significant differences between sexes (P = 0.23). In the Figure 1, the ACT distribution has been shown to in two sexes.
Table 3.
Patient characteristics
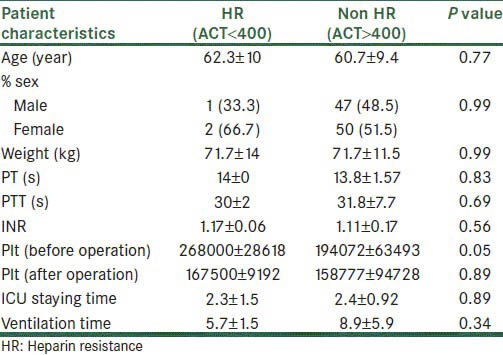
Table 1.
Distribution of resistance to heparin in terms of gender
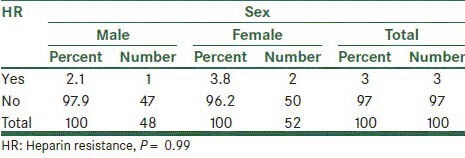
Table 2.
Frequency distribution in terms of gender on the resistance to heparin
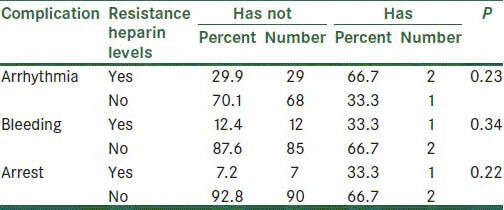
Figure 1.

The median, range, percentile 25% and 75% ACT on sex
During this study, 4 patients died, 4 of which were non-resistant to heparin (0% vs. 4.1%) but according to Fisher's exact test, depending on the frequency of resistance to heparin, there was no significant difference (P = 0.99). The total duration of staying in ICU was 2.4 ± 0.93 days. Minimum and maximum length of staying in ICU respectively was 1 and 8 days. Duration of ICU staying at two groups of resistant and non-resistant to heparin, respectively were 2.33 ± 1.53 and 2.41 ± 0.92 days, according the t-test, no significant differences were observed between groups (P = 0.89) [Figure 2].
Figure 2.
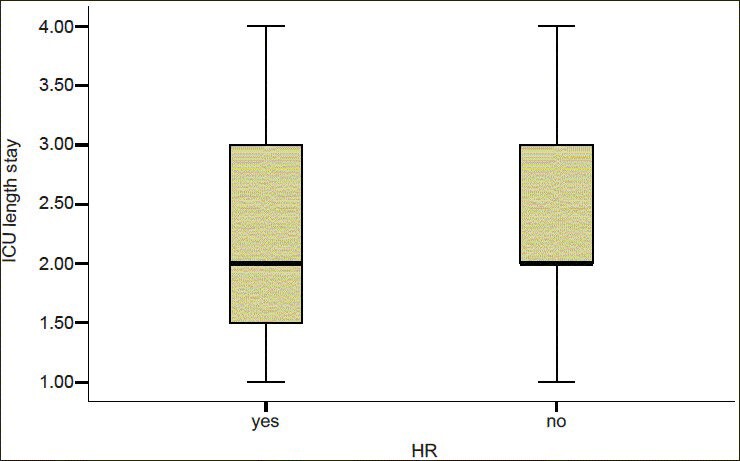
The median, range, percentile 25% and 75 of ICU staying% at two groups
The mean duration of mechanical ventilation in patients under the study was 8.82 ± 5.8 h with a range of 1-50 h. The mean duration of mechanical ventilation in patients with non-resistant and also resistant to heparin, respectively were 8.92 ± 5.9 and 5.67 ± 1.53 h and t-test showed no significant differences between groups (P = 0.34) [Table 3].
DISCUSSIONS
General objective of this study was to determine the frequency distribution of heparin resistance during coronary bypass surgery at Chamran Medical Center during the year 2011. The results of this study among 100 cases of CABG surgery showed were 3% to heparin resistance. However, heparin resistance was investigated at several studies and its incidence has been reported in different studies. At a study conducted in 2003 by Mark, heparin resistance was reported in 22% of patients, this report in compared with our study is much higher.[13] In contrast, another study conducted in 2003 by Esposito, the incidence of heparin-resistant patients has been reported at 8%, which is closer to our study.[14] As it was stated previously, heparin resistance is a problem that exists in all societies and several factors involved in that are hereditary and genetic such as AT III deficiency. Furthermore, disease and other problems such as thrombocytopenia and increased activity of factor 8, and previous history of endocarditic IABP and can also cause resistance to heparin. However, the main issue at this case is that the incidence of heparin resistance to multiple causes, which was mentioned, some of them had been increased[1,2,3,4,5,6,7] and this is important at CABG surgery. Complications associated with heparin resistance, such as arrhythmia, bleeding, arrest and death was items that we examined in our study. In our study, arrhythmias had occurred in 31 cases (31%), that 66.7% patients were in heparin resistant group and 29.9% in non-resistant to heparin group, although there was no difference between the two groups, its occurrence at heparin-resistant patients was more than 2 times vs. non-resistant. Therefore, arrhythmias are considered the most important cases in heparin resistant patients. As it is mentioned above, in Esposito study cardiac arrhythmia had occurred among 19% undergoing CABG patients.[1] The other complication was bleeding that occurred in 13 patients (13%). Its incidence was higher than the heparin resistant to patients, but with not significant differences (33.3% vs. 12.4%), and this is a normal finding in the patients because the incidence of heparin resistance on patients provide coagulation disorders and also if the preventative actions do not happen, bleeding is a common occurrence for such patients.[3] Other complications were the cardiopulmonary arrest, which occurred in 8% of our patients and the difference was no significant in heparin resistant patients and non-resistant to heparin. In our study, 33.3% patients who were in resistant to heparin group suffering from cardiopulmonary arrest, whereas the incidence of this complication was 7.2% in non heparin resistant patients. In a study conducted in 2000 by Soloway 11.5% patients undergoing CABG were suffering from arrest which is close to our study. In that study, the arrhythmia was higher in patients with of heparin resistant.[3] During our study, 4 patients died and all of them were in non-resistant to heparin (0% vs. 1.4%) and the frequency of death, depending on resistance to heparin, had no significant differences. At Dietrich study, the incidence of mortality on undergoing bypass operation patients has been reported about 3%.[6] There are multiple causes of mortality in these patients, and maybe resistance to heparin is one of the factors that either directly or indirectly could cause death in patients. Increasing ICU staying time is also another case that is dependent on resistance to heparin. Although in our study, duration of ICU staying in both group patients had no significant differences. However, most of heparin resistant patients should stay longer in ICU, due to complication incidences and there is a need for more caring.[5] Furthermore, the duration of mechanical ventilation as it is mentioned before is higher in heparin resistance patients as in our study.
General conclusion that can be found of this study is that heparin resistance is an important issue for patients who undergoing CABG and if no precautions and preventative actions have performed, it can lead to serious complication, mortality and increasing duration of staying at hospital for patients. On the other hand, heparin resistance has a relatively high prevalence. This is necessary in CABG surgery centers to provide facilities and required supplies to cope with related complications.
ACKNOWLEDGMENT
The authors wish to sincerely thank the support of all the colleagues in Chamran Hospital Medical Center affiliated to Isfahan University of Medical Sciences in Isfahan, Iran. Furthermore, our special thanks go to the patients, who wholeheartedly and actively assisted us to carry out this research. No conflict of interest existed. This cross sectional study was approved by the Ethics Committee of our university, (Isfahan University of Medical Sciences) and all patients gave written, informed consent.
Footnotes
Source of Support: Anesthesiology and Critical Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
Conflict of Interest: None declared.
REFERENCES
- 1.Garvin S, Fitzgerald D, Muehlschlegel JD, Perry TE, Fox AA, Shernan SK, et al. Heparin dose response is independent of preoperative antithrombin activity in patients undergoing coronary artery bypass graft surgery using low heparin concentrations. Anesth Analg. 2010;111:856–61. doi: 10.1213/ANE.0b013e3181ce1ffa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kamath BS, Fozard JR. Control of heparinization during cardiopulmonary bypass. Experience with the activated clotting time method. Anaesthesia. 1980;35:250–6. doi: 10.1111/j.1365-2044.1980.tb05092.x. [DOI] [PubMed] [Google Scholar]
- 3.Soloway HB, Christiansen TW. Heparin anticoagulation during cardiac surgery in AT-III deficient patients. Am J Clin Pathol. 2000;73:723–5. doi: 10.1093/ajcp/73.5.723. [DOI] [PubMed] [Google Scholar]
- 4.Maurin N. Heparin resistance and antithrombin deficiency. Med Klin (Munich) 2009;104:441–9. doi: 10.1007/s00063-009-1093-8. [DOI] [PubMed] [Google Scholar]
- 5.Singh AK, Stearns G, Maslow A, Feng WC, Schwartz C. Redo sternotomy for cardiac reoperations using peripheral heparin-bonded cardiopulmonary bypass circuits without systemic heparinization: Technique and results. J Cardiothorac Vasc Anesth. 2011;25:347–52. doi: 10.1053/j.jvca.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 6.Dietrich W, Spannagl M, Schramm W, Vogt W, Barankay A, Richter JA. The influence of preoperative anticoagulation on heparin responseduring cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1991;102:505–14. [PubMed] [Google Scholar]
- 7.Bar-Yosef S, Cozart HB, Phillips-Bute B, Mathew JP, Grocott HP. Preoperative low molecular weight heparin reduces heparin responsiveness during cardiac surgery. Can J Anaesth. 2007;54:107–13. doi: 10.1007/BF03022006. [DOI] [PubMed] [Google Scholar]
- 8.Santarpino G, Onorati F, Rubino AS, Abdalla K, Caroleo S, Santangelo E, et al. Preoperative intraaortic balloon pumping improves outcomes for high-risk patients in routine coronary artery bypass graft surgery. Ann Thorac Surg. 2009;87:481–8. doi: 10.1016/j.athoracsur.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Ranucci M, Isgrò G, Cazzaniga A, Soro G, Menicanti L, Frigiola A. Predictors for heparin resistance in patientsundergoing coronary artery bypass grafting. Perfusion. 1999;14:437–42. doi: 10.1177/026765919901400606. [DOI] [PubMed] [Google Scholar]
- 10.Conard J, LeCompte T, Horellou MH, Cazenave B, Sanama M. AT-III in patients treated with subcutaneous or intravenous heparin. Thromb Res. 1981;22:507–11. doi: 10.1016/0049-3848(81)90113-4. [DOI] [PubMed] [Google Scholar]
- 11.Reingardiene D. Heparin-induced thrombocytopenia. Medicina (Kaunas) 2008;44:723–32. [PubMed] [Google Scholar]
- 12.Denson KE. Ratio of Factor VIII-related antigen and Factor VIII biological activity as an index of hypercoagulability and intravascular clotting. Thromb Res. 1977;10:107–19. doi: 10.1016/0049-3848(77)90084-6. [DOI] [PubMed] [Google Scholar]
- 13.Mark H, Robert F, Karl J. Heparin resistance after preoperative heparin therapy or intraaortic balloon pumping. Ann Thorac Surg. 2004;57:1211–6. doi: 10.1016/0003-4975(94)91359-5. [DOI] [PubMed] [Google Scholar]
- 14.Esposito RA, Culliford AT, Colvin SB, Thomas SJ, Lackner H, Spencer FC. Heparin resistance during cardiopulmonary bypass: The role of heparin pretreatment. J Thorac Cardiovasc Surg. 1983;85:346–53. [PubMed] [Google Scholar]


