Abstract
Psychosocial treatments for methamphetamine dependence are of limited effectiveness. Thus, a significant need exists for add-on therapy for this substance user disorder. The aim of this study was to develop and test a novel text messaging intervention for use as an adjunct to cognitive behavioral group therapy for methamphetamine users. Text messaging has the potential to support patients in real-time, around the clock. We convened 2 meetings of an expert panel, held 3 focus groups in current and former users, and conducted 15 semi-structured interviews with in-treatment users in order to develop a fully-automated, cognitive behavioral therapy-based text messaging intervention. We then conducted a randomized, crossover pre-test in 5 users seeking treatment. Participants’ ratings of ease of use and functionality of the system were high. During the pre-test we performed real-time assessments via text messaging on daily methamphetamine use, craving levels, and the perceived usefulness of messages; 79% of scheduled assessments were collected. The odds of messages being rated as “very” or “extremely” useful were 6.6 times [95% CI: 2.2, 19.4] higher in the active vs. placebo periods. The intervention is now ready for testing in randomized clinical trials.
Keywords: methamphetamine, addiction, text messaging, mobile health technology, SMS
INTRODUCTION
Methamphetamine (MA) dependence is endemic worldwide and results in serious public health consequences, including cognitive deficits, increased risk of HIV infection, psychiatric illnesses, and elevated risk of cardiac pathology (Salo et al. 2011; Gonzales, Mooney & Rawson 2010; Brecht et al. 2004; Kalechstein, Newton & Green 2003). The economic impact of MA in 2005, in terms of lost productivity, environmental damage, law enforcement, and health care expenses was estimated to be over $23 billion in the US alone (Rand Corporation 2009).
Group cognitive behavioral therapy (CBT) (Stalcup et al. 2006; Galloway et al. 2000), among other psychosocial treatments, has been shown to improve outcomes in MA dependence (Rawson et al. 2004). However, the effectiveness of these approaches is limited, and patients treated for MA dependence have a high rate of relapse (Rawson et al. 2004). Despite many clinical trials dating back to the 1990s (Galloway et al. 1994), there are no approved medications for MA dependence (Heinzerling et al. 2010; Elkashef et al. 2008; Shoptaw et al. 2008). Thus, a significant need exists for add-on therapy for this substance use disorder.
Outpatient therapy is a more affordable approach than inpatient or residential treatment, but one tradeoff is that support is generally only available for a limited number of hours each day in the outpatient setting. Text messaging has the potential to serve as a real-time adjunctive therapy to outpatient group CBT, when patients are not in the clinic, and craving and risk of use may be high.
CBT relies on a learning component, and even for healthy individuals, repetition of information can improve retention. Methamphetamine users may have significant impairment in a number of neuropsychological domains, including amplified delay discounting, in which users prefer immediate, smaller rewards to delayed larger rewards (Fernandez-Serrano, Perez-Garcia & Verdejo-Garcia 2011; Hoffman et al. 2006); prospective memory (Weinborn et al. 2011); and decision making (Fernandez-Serrano, Perez-Garcia & Verdejo-Garcia 2011; Paulus et al. 2002; Bechara et al. 2001; Rogers et al. 1999). Drug craving itself can further reduce effective use of CBT concepts, as it suppresses forebrain executive functions (Volkow, Fowler & Wang 2003; Bechara & Damasio 2002; Goldstein & Volkow 2002). Text messages sent in real-time could help to compensate for these deficits by, for example, reminding patients of what they have learned in therapy sessions or of negative consequences of using.
Seventy-two percent of cellular phone users send and receive text messages (Purcell et al. 2010). The low cost (Kreps & Neuhauser 2010) and broad adoption of texting have led to rapid development as a health education tool and adjunct to healthcare (Cole-Lewis & Kershaw 2010; Krishna, Boren & Balas 2009; Patrick et al. 2008; Franklin et al. 2006). Patients view texting as easy and confidential (Obermayer et al. 2004; Collins, Kashdan & Gollnisch 2003).
Fully-automated text messaging, if efficacious, would make an inexpensive adjunctive treatment that could be scaled up for use in a large number of MA users.
Previous Studies of Text Messaging for Addiction
Reback et al (2012) conducted a two-week, non-controlled pilot study of an intervention designed to reduce high-risk sexual behaviors and MA use among out-of-treatment men who have sex with men (N=52) (Reback et al. 2012). Messages were sent by research staff manually. MA use outcomes were evaluated at 2-month follow-up (n=48) and compared to the previous 2 months at baseline. Significant decreases in frequency of MA use (p<.01) and unprotected sex while using MA (20.9% vs. 44.2%, p<.01) and a significant increase in MA abstinence based on self-report (13.3% vs. 48.9%, p<.001) and length of time since last use (p<.01) were seen at follow-up.
Eleven randomized controlled trials (RCTs) incorporating text messaging as a component of the intervention for tobacco smoking cessation have been conducted, most in smokers willing to make a quit attempt. Five of these studies (Free et al. 2011; Brendryen, Kraft & Schaalma 2010; Free et al. 2009; Brendryen, Drozd & Kraft 2008; Rodgers et al. 2005) showed significantly higher smoking cessation rates in the active vs. control groups. The other 6 studies, some of which showed trends in favor of the active groups, likely did not have sufficient power (Borland, Balmford & Benda 2013; Ybarra et al. 2013; Naughton et al. 2012; Ybarra et al. 2012; Whittaker et al. 2011; Haug et al. 2009). Aggregate sample size was over 11,000 participants. In all 11 studies, text messaging was fully automated (i.e., sent by a computer). Four studies have demonstrated the feasibility and acceptability of interventions that include a text messaging-based component and are aimed at the reduction of alcohol use (Agyapong et al. 2012; Irvine et al. 2012; McTavish et al. 2012; Suffoletto et al. 2012).
METHODS
This was a single-center study conducted at New Leaf Treatment Center (NLTC), a licensed outpatient addiction treatment facility in Lafayette, California. Institutional Review Boards approved the semi-structured interviews, focus groups, and pre-test and provided oversight of the study. Participants provided informed consent prior to initiation of study procedures.
Confidentiality was a concern with this study, since we were collecting data on illicit drug use. Several steps were implemented to protect patients. We asked participants at screening to password protect their phones, and they had to agree via text message to receive additional messages. In addition, we did not explicitly mention MA in any of the texts, reference to participants’ names in the texts was optional, and data used to personalize test messages were stored on a password-protected server.
Development of Text Messages
We created a CBT-based text messaging intervention to be used in conjunction with NLTC’s standard CBT group therapy, the Craving Identification and Management Model (CIM)(Stalcup et al. 2006). CIM is based on standard CBT principles, with a focus on craving, which we have demonstrated to be predictive of MA use (Galloway, Singleton & The Methamphetamine Treatment Project Corporate Authors 2009; Hartz, Frederick-Osborne & Galloway 2001). Patients are directed to quantify their craving level and, if it is elevated, to identify causes of that elevation, e.g., stress, withdrawal, environmental cues, and increased symptoms of anxiety or depression. Cognitive and behavioral interventions are then suggested to terminate or ameliorate causes of craving, or, if that is not possible, to directly reduce craving (Stalcup et al. 2006). CIM has been shown to have comparable efficacy to the Matrix Model, a prototype for CBT-based therapy in this population (Rawson et al. 2004).
To develop the text messages, we convened 2 meetings of an expert panel and held 3 focus groups (mean n=5 per group) with current and former MA users ≥ 18 years in October and November 2011. We also incorporated findings from 15 semi-structured interviews of MA users ≥ 18 years which occurred in October-December 2011. In order to derive new messages, focus group participants and interviewees were asked open-ended questions about what types of messages might help reduce their craving and/or use of MA. Additionally, focus group participants provided input on messages previously developed by the expert panel. Participants were asked about the utility of personalizing messages on the basis of a screening interview, whether any of the messages could be triggering (i.e., induce craving), and which messages they thought would be most useful, and why.
We also created placebo messages, which were capitals of countries (e.g., “Paris is the capital of France”). The intervention was designed to be fully automated (i.e., sent by a computer), so as to be cost effective and to limit the need for staff resources.
Pre-test
To test procedures and methods, a 23-day pre-test was performed in 5 MA users seeking treatment. Participants were randomized over a 40-day period in April-May 2012 and were required to use their own cellular phones and to have an unlimited text messaging plan. We required that they be experiencing high levels of craving for MA, as defined by having at least 1 time per week in the last 2 weeks in which craving were 3 or higher on a scale of 0–10, where 0 is “no craving” and 10 is “most craving ever experienced for MA.” We collected demographic and cellular telephone use data at baseline via semi-structured interviews.
Messages were personalized on the basis of a screening interview. For example, only participants who indicated they had a 12-step sponsor would be asked to call their sponsor, whereas the intervention of reminding participants that cravings are transient would be delivered to all participants. Text messages were sent at random times 4 times throughout the day on Day 1 (these intervention messages were “pushed”) in a 12-hour period that participants had pre-specified. Participants were also requested to “pull” messages at any time by texting the word “crave” to the system when they were craving MA.
At the end of Day 1, participants were invited via text message to continue for the balance of the trial if they had demonstrated adherence by responding to at least 3 out of 4 requests to rate the utility of the “pushed” messages. If they further demonstrated adherence by responding within 60 minutes that they wanted to continue, they were randomized to either one week of active text messages followed by one week of placebo text messages or vice versa (there was a one-week washout period when no text messages were received between the active and placebo periods in order to minimize the possibility of carryover effects) (Figure 1). Participants continued to receive 4 “pushed” messages per day and were also able to “pull” messages on Days 2–8 and Days 16–22. Participants attended group therapy 3 times per week for 3 weeks between Days 2–23.
Figure 1.
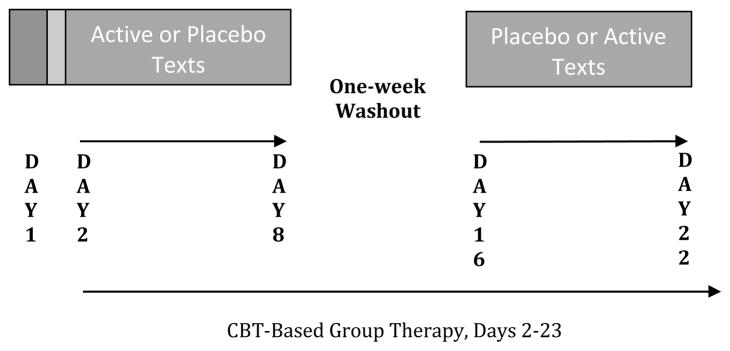
Pre-test Study Schematic
Measurements collected via text message included the following: 60 minutes after each message, participants were instructed to rate on a Likert scale (1= not at all, 2=slightly, 3=moderately, 4=very, 5=extremely) how useful the intervention was. Also, at the end of each day, participants were asked whether they used MA in the past 24 hours, as well as what their peak craving was (on a scale of 0–10, where 0 is “no craving” and 10 is “most craving ever experienced for MA”) in the past 24 hours.
At follow-up participants were asked open-ended questions about the text messages, measurement assessments, the software system, and their overall perceived utility of this intervention. The overall ease of use, acceptability, and effectiveness of the intervention were assessed with Likert scales.
Analyses
Follow-up Visit Assessments: Number and percent of participants providing each Likert score were tabulated. For continuous variables, mean (SD) and/or medians were used. Responses to open-ended questions were summarized.
Text Messaging Assessments: Number of days used in the active vs. placebo groups was described. Logistic regression was used to assess the odds of messages being rated as “very” or “extremely” useful (as opposed to “not at all,” “slightly,” or “moderately”) in the active vs. placebo groups. Similarly, logistic regression was used to calculate the odds of active texts being rated as “very” or “extremely” useful in the personalized vs. non-personalized message groups. Negative binomial regression was used to assess the rate of peak daily craving in the active vs. placebo groups. With all 3 regressions, data were clustered by participant ID to account for the repeated measures in the dataset. Sensitivity analyses were performed in which we removed the participant who discontinued responding to messages prematurely.
Proportions of missing assessments were specified. In addition, since these regressions utilize maximum likelihood estimation, variables that could account for data missing at random in the outcome were considered for addition to the regressions as predictors to help avoid potential bias in the results (Vittinghoff et al. 2011). Specifically, we evaluated high baseline MA use (≥ 15 days out of 30), a marker for severity of disease, as well as MA use that day and the day prior for inclusion as predictors in the models.
Since this was a crossover study, we tested our regressions for period effects (indicating that responses in the 2nd period were influenced by the first period) and sequence effects (whether a difference existed based on whether participants had received active or placebo messages first) by adding these as predictors to our models using a significance cutoff of p<.10. All data were analyzed using Stata 12SE (StataCorp. 2011).
RESULTS
Final CIM-Based Text Messages
We generated 96 active text messages (Table 1). Focus group participants’ and interviewees’ recommendations for text messages were similar. They gave favorable reviews to those that were “positive,” affirmative, succinct, and personalized. They advocated including messages that involved a request to help others, reminders to use concurrent group therapy for support, or 12-step program sayings. They gave negative feedback on messages seen as too demanding or “guilt inducing.” Several methods of individualizing messages were implemented based on participants’ feedback: interviewing participants about their perceived negative consequences of using MA as well as their reasons for entering treatment; and tailoring individual messages to participants with children, those who participate in 12-step program, find exercise helpful, or view prayer as supportive. Participants agreed there should be two different types of messages, those that were “pushed” (i.e., initiated by the computer program at random intervals) and those that were “pulled” (i.e., sent at the request of the participant), and that “pulled” messages should have a greater focus on reducing acute craving.
Table 1.
Sample “Pushed” and “Pulled” Active Text Messages (96 Total)
| PUSHED MESSAGES [71 (74%) Messages*] |
| Non-Personalized [45 (63%) Pushed Messages] |
|
| Personalized [26 (37%) Pushed Messages] |
|
| PULLED MESSAGES [33 (34%) Messages*] |
| Non-Personalized [20 (61%) Pulled Messages] |
|
| Personalized [13 (39%) Pulled Messages] |
|
Eight messages were designed to be both pushed and pulled, so sum of pushed and pulled messages is greater than 96.
Pre-test Findings
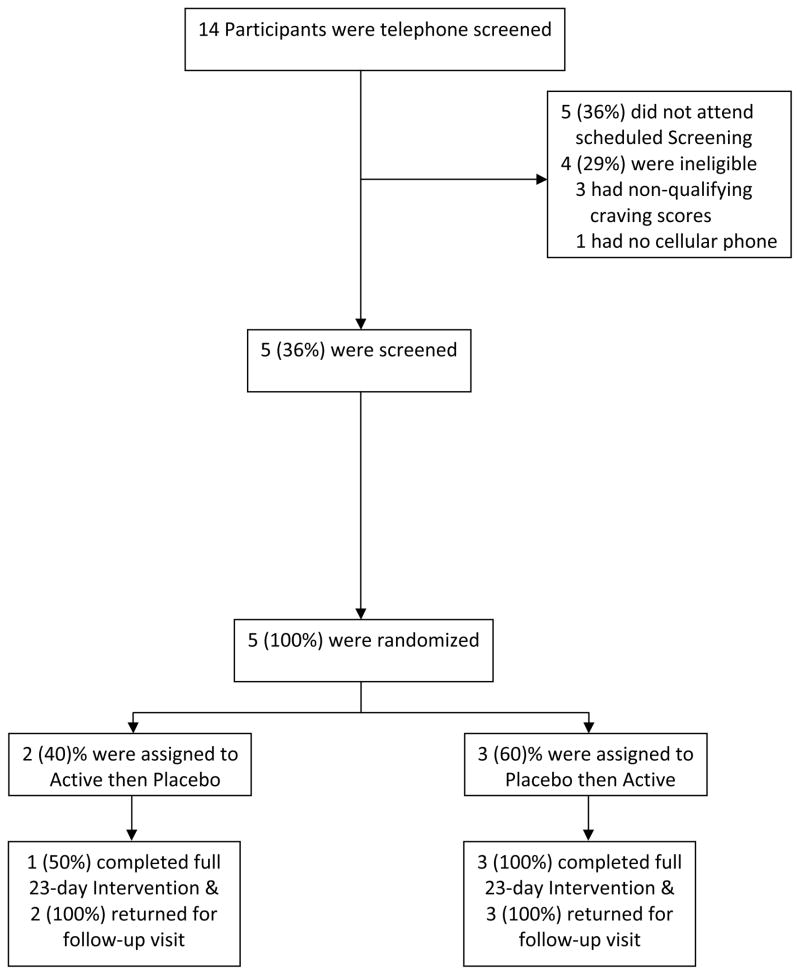
We telephone screened 14 potential participants, and 5 (36%) attended onsite screening visits (see the CONSORT flowchart, Figure 2). All 5 participants met randomization criteria on Day 1. One randomized participant was arrested and discontinued responding to text message assessments on Day 5 (during the active phase); however, he did complete a follow-up visit.
Figure 2.
CONSORT Flowchart of Pre-test Participants
Participants were 80% male, 60% Caucasian, 60% heterosexual, with a mean age of 28.6 (SD 2.1). Median years of education completed was 14. In the 30 days prior to baseline, participants used MA a mean of 9.3 days (SD 12).
At follow-up, all participants agreed or totally agreed (ratings of 4 or 5 on a 5-point scale) that the text messaging system was easy to use. Four out of 5 participants agreed or totally agreed that the system worked well for them to send and receive messages (one participant neither agreed nor disagreed, indicating that he did not like the one hour lag between receiving the intervention and the inquiry about its usefulness). Four out of 5 participants (80%) “totally agreed” that they understood the instructions presented to them at the screening visit, while 1 participant “slightly disagreed.”
Three out of 5 participants thought the number of pushed messages sent to them each day (4) was “just right,” while the other 2 participants thought there were “too many” messages. When asked about the ideal number of pushed messages per day as a continuous outcome, the mean was 3 (SD 0.9). Two participants thought the number of hours per day that they sent and received messages (about 12) was “just right,” while 2 participants thought it was “too long” and 1 indicated it was “too short.” The median ideal number of hours per day that participants would have liked to have sent and received messages was 10.
Three out of 5 participants “pulled” messages (8 times total) during the study.
We were able to collect data for 79% of text messaging assessments (79% of usefulness, 83% of daily use and 74% of daily peak craving data). After removing assessments post discontinuation for the participant who stopped responding after his arrest on Day 5, we successfully collected 92% of data in both the active and placebo periods. In total, 92% of usefulness, 97% of daily use and 87% of daily peak craving data were collected. Table 2 provides a detailed breakdown of data collected in the active and placebo phases.
Table 2.
Responses to Text Message Assessments of Daily Methamphetamine Use, Usefulness of Messages, and Peak Daily Craving
| Text Message Assessments | Active (%) | Placebo (%) | Active* (%) | Placebo* (%) | Efficacy Results | 95% CI |
|---|---|---|---|---|---|---|
| Overall Response Rate (# Responded to/# Sent) | 179/213 (84%) | 160/215 (74%) | 179/195 (92%) | 160/173 (92%) | n/a | |
| Daily Self-Reported Use | 32/35 (91%) | 26/35 (74%) | 32/32 (100%) | 26/28 (93%) | 1 day use (total) in active phase & 2 days use (total) in placebo phase | n/a |
| Usefulness Ratings | 119/143 (83%) | 110/145 (76%) | 119/131 (91%) | 110/117 (94%) | 6.6 OR** | [2.2, 19.4] |
| Daily Peak Craving*** | 28/35 (80%) | 24/35 (69%) | 28/32 (88%) | 24/28 (86%) | Mean 3.3 in placebo phase; 40% higher in the active phase | [2.8, 3.8]; [9%, 80%] |
Excludes from the denominators post Day 5 messages for participant who discontinued responding prematurely due to his arrest.
Odds of messages being rated as “very” or “extremely” useful (versus “not at all,” “slightly” or “moderately”).
On a scale of 0–10, where 0 is “no craving” and 10 is “most ever experienced”
Participants self-reported (via text messaging) using MA 1 time total during the active period and 2 times total during the placebo period. Given the small sample size (n=5) included in the pre-test, we did not expect to find significant differences in self-reported use in the active versus placebo periods. Excluding data because of the participant who was arrested, self-reported use results did not change. Excluding missing data for this participant, there were 0 instances of missing drug use data in the active period and 2 instances in the placebo period; missing data may reflect MA use.
The odds of messages being rated as “very” or “extremely” useful (via text messaging assessments) were 6.6 times [95% CI: 2.2, 19.4] higher in the active vs. placebo periods (Table 2). We examined other cut points for this outcome, but this OR was the most conservative (i.e., lowest). Results of a sensitivity analysis in which we removed the participant who discontinued responding prematurely yielded a similar odds ratio (OR 7.6, [95% CI: 2.2, 26.1]). We had speculated missing usefulness ratings might be a function of use that day or the day prior, but this was not the case, probably because the incidence of MA use reported was low. However, missing data in this outcome was greater (11% vs. 4%) in participants with high baseline MA use (≥ 15 days out of 30). We could not incorporate this dichotomous predictor into our bivariate model (the model would not converge); however, as a univariate predictor, high baseline use showed odds of messages being rated as “very” or “extremely” useful that were 8.8 [95% CI: 2.3, 33.9] times higher than in participants with low baseline use.
Twenty seven percent of active text messages sent had been personalized based upon the results of screening interviews. The odds of active text messages being rated as “very” or “extremely” useful were 52% higher with personalized vs. non-personalized messages; however, this result was not statistically significant (p=.4).
Missing data in the outcome of peak daily craving (assessed via text messaging) was not a function of use that day or the day prior; however, it was greater (18% vs. 7%) in participants with high baseline use. Therefore, we added this predictor to our model. Mean peak daily craving in the placebo period was 3.3 [95% CI: 2.8, 3.8]. Paradoxically, peak daily craving was 40% [95% CI: 9%, 80%] higher in the active vs. placebo periods. Results of a sensitivity analysis in which we removed the participant who discontinued responding prematurely were marginally lower (peak daily craving was 33% higher [95% CI: 4%, 70%] in the active period).
No statistically significant period or sequence effects were observed in the regressions.
DISCUSSION
We have developed a reliable, acceptable text messaging system as an adjunct to CBT group therapy for MA dependence. Our data from 25 semi-structured interviews indicated that 92% of MA users polled owned cellular telephones and, of these, 96% had unlimited texting plans.
Given we were able to collect 79% of data from text messaging assessments (92% of data from participants excluding missing data due to one participant’s premature discontinuation), data collection via this medium is feasible in this population. Although placebo texts (capitals of countries) are fairly repetitive, the fact that we were able to collect the same amount of data (92%) in both the active and placebo periods suggests that participants were not less attentive to them than to CBT-based messages.
At follow-up, participants overall agreed the text messaging system was easy to use and worked well for them to send and receive messages, and they agreed they had understood the instructions explained to them at the screening visit. Preliminary results from the follow-up visit suggest that the ideal number of pushed messages per day is 3–4. When asked about the ideal number of hours a day to send and receive messages, responses were variable, some wanting a longer duration and others preferring shorter. While preliminary efficacy analyses in the 5 pre-test participants showed that the odds of messages being rated as “very” or “extremely” useful were much higher in the active vs. placebo periods, it is possible that these findings may be attributable to the unique characteristics of this small sample.
The finding that peak daily craving was considerably higher in the active vs. placebo periods may dissipate for the same reasons. Alternatively, it may reflect the fact that CIM-based text messages are designed to raise awareness of craving levels. While the possibility that CIM-based messages are triggering exists, daily use data and follow-up interviews did not reflect this, which is reassuring from a safety perspective.
Limitations to this study include its small sample size, brief duration, and lack of biochemical verification of MA use. As the workability of the text messaging system and its acceptability to participants have been established, additional testing of this intervention is warranted.
Acknowledgments
The authors wish to thank Michael Cai for his assistance with programming the intervention, as well as Drs. David V. Glidden and Mark Pletcher, NLTC staff, and our participants. This study was supported by National Institutes of Health (NIH) grant R01DA024714 and a gift from Emily G. Kahn.
Footnotes
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
CONFLICT OF INTEREST: The authors declared no conflict of interest.
Bibliography
- Agyapong VI, Ahern S, McLoughlin DM, Farren CK. Supportive text messaging for depression and comorbid alcohol use disorder: Single-blind randomised trial. Journal of Affective Disorders. 2012 Dec 10;141(2–3):168–76. doi: 10.1016/j.jad.2012.02.040. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H. Decision-making and addiction (part I): Impaired activation of somatic states in substance dependent individuals when pondering decisions with negative future consequences. Neuropsychologia. 2002;40(10):1675–89. doi: 10.1016/s0028-3932(02)00015-5. [DOI] [PubMed] [Google Scholar]
- Bechara A, Dolan S, Denburg N, Hindes A, Anderson SW, Nathan PE. Decision-making deficits, linked to a dysfunctional ventromedial prefrontal cortex, revealed in alcohol and stimulant abusers. Neuropsychologia. 2001;39(4):376–89. doi: 10.1016/s0028-3932(00)00136-6. [DOI] [PubMed] [Google Scholar]
- Borland R, Balmford J, Benda P. Population-level effects of automated smoking cessation help programs: A randomized controlled trial. Addiction (Abingdon, England) 2013 Mar;108(3):618–28. doi: 10.1111/j.1360-0443.2012.04091.x. [DOI] [PubMed] [Google Scholar]
- Brendryen H, Kraft P, Schaalma H. Looking inside the black box: Using intervention mapping to describe the development of the automated smoking cessation intervention ‘happy ending’. Journal of Smoking Cessation. 2010;5(1):29. [Google Scholar]
- Brendryen H, Drozd F, Kraft P. A digital smoking cessation program delivered through internet and cell phone without nicotine replacement (happy ending): Randomized controlled trial. Journal of Medical Internet Research. 2008 Nov 28;10(5):e51. doi: 10.2196/jmir.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiologic Reviews. 2010 Apr;32(1):56–69. doi: 10.1093/epirev/mxq004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins RL, Kashdan TB, Gollnisch G. The feasibility of using cellular phones to collect ecological momentary assessment data: Application to alcohol consumption. Experimental and Clinical Psychopharmacology. 2003 Feb;11(1):73–8. doi: 10.1037//1064-1297.11.1.73. [DOI] [PubMed] [Google Scholar]
- Elkashef AM, Rawson RA, Anderson AL, Li SH, Holmes T, Smith EV, Chiang N, Kahn R, Vocci F, Ling W, Pearce VJ, McCann M, Campbell J, Gorodetzky C, Haning W, et al. Bupropion for the treatment of methamphetamine dependence. Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology. 2008 Apr;33(5):1162–70. doi: 10.1038/sj.npp.1301481. [DOI] [PubMed] [Google Scholar]
- Fernandez-Serrano MJ, Perez-Garcia M, Verdejo-Garcia A. What are the specific vs. generalized effects of drugs of abuse on neuropsychological performance? Neuroscience and Biobehavioral Reviews. 2011 Jan;35(3):377–406. doi: 10.1016/j.neubiorev.2010.04.008. [DOI] [PubMed] [Google Scholar]
- Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of sweet talk, a text-messaging system to support young people with diabetes. Diabetic Medicine: A Journal of the British Diabetic Association. 2006 Dec;23(12):1332–8. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- Free C, Knight R, Robertson S, Whittaker R, Edwards P, Zhou W, Rodgers A, Cairns J, Kenward MG, Roberts I. Smoking cessation support delivered via mobile phone text messaging (txt2stop): A single-blind, randomised trial. Lancet. 2011 Jul 2;378(9785):49–55. doi: 10.1016/S0140-6736(11)60701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Free C, Whittaker R, Knight R, Abramsky T, Rodgers A, Roberts IG. Txt2stop: A pilot randomised controlled trial of mobile phone-based smoking cessation support. Tobacco Control. 2009 Apr;18(2):88–91. doi: 10.1136/tc.2008.026146. [DOI] [PubMed] [Google Scholar]
- Galloway GP, Singleton EG The Methamphetamine Treatment Project Corporate Authors. How long does craving predict use of methamphetamine? assessment of use one to seven weeks after the assessment of craving: Craving and ongoing methamphetamine use. Substance Abuse: ] Research and Treatment. 2009 Aug 26;1:63–79. [PMC free article] [PubMed] [Google Scholar]
- Galloway GP, Marinelli-Casey P, Stalcup J, Lord R, Christian D, Cohen J, Reiber C, Vandersloot D. Treatment-as-usual in the methamphetamine treatment project. Journal of Psychoactive Drugs. 2000 Apr-Jun;32(2):165–75. doi: 10.1080/02791072.2000.10400225. [DOI] [PubMed] [Google Scholar]
- Galloway GP, Newmeyer J, Knapp T, Stalcup SA, Smith D. Imipramine for the treatment of cocaine and methamphetamine dependence. Journal of Addictive Diseases. 1994;13 (4):201–16. doi: 10.1300/j069v13n04_08. [DOI] [PubMed] [Google Scholar]
- Goldstein RZ, Volkow ND. Drug addiction and its underlying neurobiological basis: Neuroimaging evidence for the involvement of the frontal cortex. The American Journal of Psychiatry. 2002 Oct;159(10):1642–52. doi: 10.1176/appi.ajp.159.10.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales R, Mooney L, Rawson RA. The methamphetamine problem in the united states. Annual Review of Public Health. 2010 Apr 21;31 :385–98. doi: 10.1146/annurev.publhealth.012809.103600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartz DT, Frederick-Osborne SL, Galloway GP. Craving predicts use during treatment for methamphetamine dependence: A prospective, repeated-measures, within-subject analysis. Drug and Alcohol Dependence. 2001 Aug 1;63(3):269–76. doi: 10.1016/s0376-8716(00)00217-9. [DOI] [PubMed] [Google Scholar]
- Haug S, Meyer C, Schorr G, Bauer S, John U. Continuous individual support of smoking cessation using text messaging: A pilot experimental study. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 2009 Aug;11(8):915–23. doi: 10.1093/ntr/ntp084. [DOI] [PubMed] [Google Scholar]
- Heinzerling KG, Swanson AN, Kim S, Cederblom L, Moe A, Ling W, Shoptaw S. Randomized, double-blind, placebo-controlled trial of modafinil for the treatment of methamphetamine dependence. Drug and Alcohol Dependence. 2010 Jun 1;109(1–3):20–9. doi: 10.1016/j.drugalcdep.2009.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman WF, Moore M, Templin R, McFarland B, Hitzemann RJ, Mitchell SH. Neuropsychological function and delay discounting in methamphetamine-dependent individuals. Psychopharmacology. 2006 Oct;188(2):162–70. doi: 10.1007/s00213-006-0494-0. [DOI] [PubMed] [Google Scholar]
- Irvine L, Falconer DW, Jones C, Ricketts IW, Williams B, Crombie IK. Can text messages reach the parts other process measures cannot reach: An evaluation of a behavior change intervention delivered by mobile phone? PloS One. 2012;7 (12):e52621. doi: 10.1371/journal.pone.0052621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalechstein AD, Newton TF, Green M. Methamphetamine dependence is associated with neurocognitive impairment in the initial phases of abstinence. The Journal of Neuropsychiatry and Clinical Neurosciences. 2003 Spring;15(2):215–20. doi: 10.1176/jnp.15.2.215. [DOI] [PubMed] [Google Scholar]
- Kreps GL, Neuhauser L. New directions in eHealth communications: Opportunities and challenges. Patient Educ Couns. 2010;78 (3):329–336. doi: 10.1016/j.pec.2010.01.013. [DOI] [PubMed] [Google Scholar]
- Krishna S, Boren SA, Balas EA. Healthcare via cell phones: A systematic review. Telemedicine Journal and e-Health: The Official Journal of the American Telemedicine Association. 2009 Apr;15(3):231–40. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- McTavish FM, Chih MY, Shah D, Gustafson DH. How patients recovering from alcoholism use a smartphone intervention. Journal of Dual Diagnosis. 2012;8 (4):294–304. doi: 10.1080/15504263.2012.723312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naughton F, Prevost AT, Gilbert H, Sutton S. Randomized controlled trial evaluation of a tailored leaflet and SMS text message self-help intervention for pregnant smokers (MiQuit) Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 2012 Feb 6; doi: 10.1093/ntr/ntr254. [DOI] [PubMed] [Google Scholar]
- Obermayer JL, Riley WT, Asif O, Jean-Mary J. College smoking-cessation using cell phone text messaging. Journal of American College Health: J of ACH. 2004 Sep-Oct;53(2):71–8. doi: 10.3200/JACH.53.2.71-78. [DOI] [PubMed] [Google Scholar]
- Patrick K, Griswold WG, Raab F, Intille SS. Health and the mobile phone. American Journal of Preventive Medicine. 2008 Aug;35(2):177–81. doi: 10.1016/j.amepre.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulus MP, Hozack NE, Zauscher BE, Frank L, Brown GG, Braff DL, Schuckit MA. Behavioral and functional neuroimaging evidence for prefrontal dysfunction in methamphetamine-dependent subjects. Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology. 2002 Jan;26(1):53–63. [Google Scholar]
- Purcell K, Rainie L, Mitchell A, Rosenstiel T, Olmstead K. Understanding the participatory news consumer. PEW Research Center; 2010. [Google Scholar]
- Rand Corporation. The economic cost of methamphetamine use in the united states, 2005. 2009 Available from http://www.rand.org/news/press/2009/02/04/meth.html.
- Rawson RA, Marinelli-Casey P, Anglin MD, Dickow A, Frazier Y, Gallagher C, Galloway GP, Herrell J, Huber A, McCann MJ, Obert J, Pennell S, Reiber C, Vandersloot D, Zweben J, et al. A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction (Abingdon, England) 2004 Jun;99(6):708–17. doi: 10.1111/j.1360-0443.2004.00707.x. [DOI] [PubMed] [Google Scholar]
- Reback CJ, Grant DL, Fletcher JB, Branson CM, Shoptaw S, Bowers JR, Charania M, Mansergh G. Text messaging reduces HIV risk behaviors among methamphetamine-using men who have sex with men. AIDS and Behavior. 2012 May 19; doi: 10.1007/s10461-012-0200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers A, Corbett T, Bramley D, Riddell T, Wills M, Lin RB, Jones M. Do u smoke after txt? results of a randomised trial of smoking cessation using mobile phone text messaging. Tobacco Control. 2005 Aug;14(4):255–61. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers RD, Everitt BJ, Baldacchino A, Blackshaw AJ, Swainson R, Wynne K, Baker NB, Hunter J, Carthy T, Booker E, London M, Deakin JF, Sahakian BJ, Robbins TW. Dissociable deficits in the decision-making cognition of chronic amphetamine abusers, opiate abusers, patients with focal damage to prefrontal cortex, and tryptophan-depleted normal volunteers: Evidence for monoaminergic mechanisms. Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology. 1999 Apr;20(4):322–39. doi: 10.1016/S0893-133X(98)00091-8. [DOI] [PubMed] [Google Scholar]
- Salo R, Flower K, Kielstein A, Leamon MH, Nordahl TE, Galloway GP. Psychiatric comorbidity in methamphetamine dependence. Psychiatry Research. 2011 Apr 30;186(2–3):356–61. doi: 10.1016/j.psychres.2010.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoptaw S, Heinzerling KG, Rotheram-Fuller E, Steward T, Wang J, Swanson AN, De La Garza R, Newton T, Ling W. Randomized, placebo-controlled trial of bupropion for the treatment of methamphetamine dependence. Drug and Alcohol Dependence. 2008 Aug 1;96(3):222–32. doi: 10.1016/j.drugalcdep.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stalcup SA, Christian D, Stalcup J, Brown M, Galloway GP. A treatment model for craving identification and management. Journal of Psychoactive Drugs. 2006 Jun;38(2):189–202. doi: 10.1080/02791072.2006.10399843. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Suffoletto B, Callaway C, Kristan J, Kraemer K, Clark DB. Text-message-based drinking assessments and brief interventions for young adults discharged from the emergency department. Alcoholism, Clinical and Experimental Research. 2012 Mar;36(3):552–60. doi: 10.1111/j.1530-0277.2011.01646.x. [DOI] [PubMed] [Google Scholar]
- Vittinghoff E, Glidden D, Shiboski SC, McCulloch CE. Regression methods in biostatistics. 2. Vol. 455. New York: Springer; 2011. Missing data; pp. 458–461. [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ. The addicted human brain: Insights from imaging studies. The Journal of Clinical Investigation. 2003 May;111(10):1444–51. doi: 10.1172/JCI18533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinborn M, Woods SP, O’Toole S, Kellogg EJ, Moyle J. Prospective memory in substance abusers at treatment entry: Associations with education, neuropsychological functioning, and everyday memory lapses. Archives of Clinical Neuropsychology: The Official Journal of the National Academy of Neuropsychologists. 2011 Dec;26(8):746–55. doi: 10.1093/arclin/acr071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittaker R, Dorey E, Bramley D, Bullen C, Denny S, Elley CR, Maddison R, McRobbie H, Parag V, Rodgers A, Salmon P. A theory-based video messaging mobile phone intervention for smoking cessation: Randomized controlled trial. Journal of Medical Internet Research. 2011 Jan 21;13(1):e10. doi: 10.2196/jmir.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ybarra M, Bagci Bosi AT, Korchmaros J, Emri S. A text messaging-based smoking cessation program for adult smokers: Randomized controlled trial. Journal of Medical Internet Research. 2012 Dec 27;14(6):e172. doi: 10.2196/jmir.2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ybarra ML, Holtrop JS, Prescott TL, Rahbar MH, Strong D. Pilot RCT results of stop my smoking USA: A text messaging-based smoking cessation program for young adults. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 2013 Aug;15(8):1388–99. doi: 10.1093/ntr/nts339. [DOI] [PMC free article] [PubMed] [Google Scholar]