One of the challenges in the treatment of plantar fasciitis is that there are very few high-quality studies comparing different treatment modalities to guide evidence-based management. Current literature suggests a change to the way that plantar fasciitis is managed. This article reviews the most current literature on plantar fasciitis and showcases recommended treatment guidelines.
Abstract
One challenge in the treatment of plantar fasciitis is that very few high-quality studies exist comparing different treatment modalities to guide evidence-based management. Current literature suggests a change to the way that plantar fasciitis is managed. This article reviews the most current literature on plantar fasciitis and showcases recommended treatment guidelines. This serves to assist physicians in diagnosing and treating heel pain with plantar fasciitis.
Introduction
Plantar fasciitis is one of the most common causes of heel pain and has been estimated to affect about two million people in the US, resulting in more than one million visits to both primary care physicians and foot specialists.1,2 Plantar fasciitis affects both sedentary and athletic people and is thought to result from chronic overload either from lifestyle or exercise.2 Current literature suggests that plantar fasciitis is more correctly termed fasciosis because of the chronicity of the disease and the evidence of degeneration rather than inflammation.1–6 Treatment is often difficult because of the poorly understood mechanism by which the body heals chronic degeneration as opposed to acute inflammation. This article lays out current recommendations for diagnosis and treatment so as to better guide any physician who encounters a patient with plantar pain.
Case Report
A 48-year-old obese but otherwise healthy woman presents to her primary care physician complaining of bilateral foot pain. She states that she has had the pain daily for months. The pain is located on the bottom of her feet at the heel and is severe, especially on the first step out of bed in the morning and after a long day at work. She works at a warehouse handing out samples to customers and stands for approximately 7 hours a day. The pain does not radiate anywhere, and there is no associated numbness, tingling, leg swelling, or weakness. She denies any history of trauma or falls. She exercises by walking 3 times a week for 30 minutes and is able to complete the walk without problems. In fact, the walking seems to make her feet feel better. She has tried changing shoes and ibuprofen but has had no relief.
On physical examination, her lower legs and feet have no apparent abnormalities. There is no edema, ecchymoses, skin changes, or evidence of cyanosis. She has no tenderness to palpation over the tibia, fibula, malleoli, tarsals, metatarsals, metacarpophalangeal joints, or digits. She has exquisite tenderness to palpation just medial to the midline of her heel just superior to the calcaneal bone. She also has tenderness, but less so, along the plantar aspect of the midfoot. She has normal strength of dorsiflexors and plantar flexors. She has normal range of motion with inversion, eversion, and plantar flexion. She is just able to get to neutral position on dorsiflexion. Sensation is intact and pedal pulses are present and equal bilaterally. When she is standing, it is apparent that she has pes planus. She is able to walk on her toes and heels and has a normal gait with mild pronation.
The patient receives a diagnosis of plantar fasciitis and instructions on conservative management to facilitate recovery, including appropriate footwear at work, stretching, and massage. She is encouraged to start a low-impact exercise program to aid in weight loss.
Discussion
The plantar fascia is a thick fibrous aponeurosis that originates at the medial calcaneal tubercle and helps support the arch of the foot (Figure 1). It is thought that repetitive tensile overload from standing for long periods of time or running causes changes in the aponeurosis that can be either acute or chronic. More recently, the term plantar fasciosis has been introduced to de-emphasize the idea that inflammation is the cause of pain.3 Histopathologic studies have shown that patients with diagnosed plantar fasciitis have more disorganization of fibrous tissue similar to degenerative tendinosis rather than inflammation.4
Figure 1.
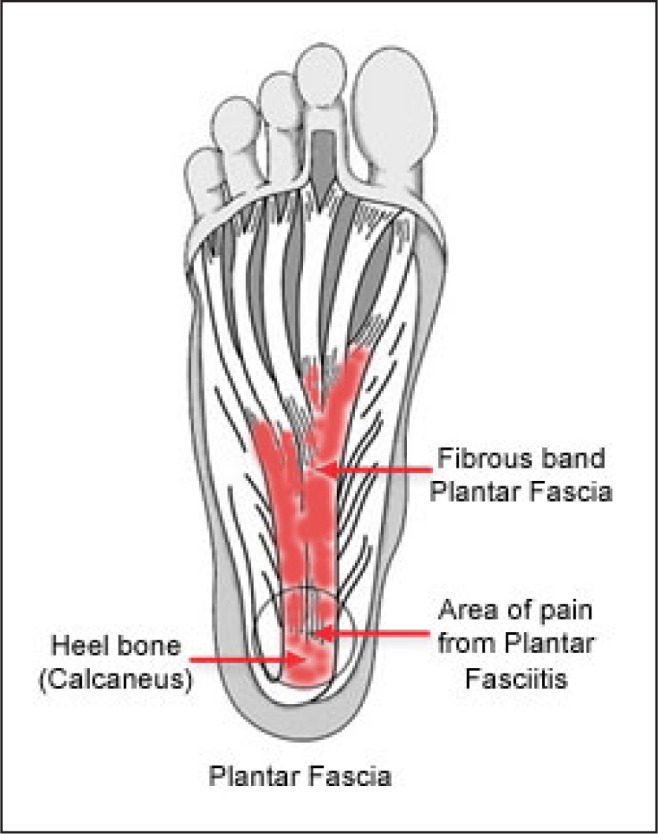
Anatomy of the foot.
Reproduced with permission from OrthoInfo. © American Academy of Orthopaedic Surgeons. http://orthoinfoaaos.org.
Classic symptoms include severe pain in the morning or after a rest period that improves with movement but is aggravated by long periods of weight bearing. Physical examination findings are typically tenderness to palpation over the medical calcaneal tubercle and discomfort with passive dorsiflexion of the first toe.1 Several risk factors, both intrinsic and extrinsic, are listed in Table 1.1–4
Table 1:
| Intrinsic risk factors | |
| Anatomic | Obesity |
| Pes planus (flat feet) | |
| Pes cavus (high-arched feet) | |
| Shortened Achilles tendon | |
| Biomechanic | Overpronation (inward roll) |
| Limited ankle dorsiflexion | |
| Weak intrinsic muscles of the foot | |
| Weak plantar flexor muscles | |
| Extrinsic risk factors | |
| Environmental | Poor biomechanics or alignment |
| Deconditioning | |
| Hard surface | |
| Walking barefoot | |
| Prolonged weight bearing | |
| Inadequate stretching | |
| Poor footwear | |
All of the risk factors can be assessed on the basis of history and physical alone and help to guide appropriate treatment. Imaging is typically not necessary for the diagnosis but may be helpful if there are other likely reasons for heel pain included in the differential diagnosis (Table 2).
Table 2:
Differential diagnosis for heel pain.7
| Type | Diagnosis | Common findings |
|---|---|---|
| Neurologic | Tarsal tunnel syndrome: posterior tibial nerve impingement | Burning sensation in the plantar region worsened by dorsiflexion |
| Neuropathy such as from diabetes | Paresthesias in plantar region | |
| Skeletal | Acute calcaneal fracture | Likely after hard landing on heel |
| Calcaneal stress fracture | Most likely seen in runners | |
| Sever disease: calcaneal apophysitis | Seen in pediatric patients with open physes | |
| Systemic arthritides such as rheumatoid | Expect pain in multiple joints along with heel pain | |
| Soft tissue | Fat pad atrophy | More common in elderly people |
| Fat pad contusion | More likely associated with hard landing on heel | |
| Achilles tendinitis | Posterior calcaneal tenderness and tendon pain | |
| Retrocalcaneal bursitis | Pain in retrocalcaneal bursa | |
| Posterior tibial tendinitis | Pain along posterior tibial tendon and at insertion mid foot at the arch |
Treatment mechanisms have been wide ranging, from ice, nonsteroidal anti-inflammatory medications,1–5,7 stretching,1–4,6–8 formal physical therapy,1–4,7,9 night splints,1–4,7,9–13 custom orthotics,14 over-the-counter heel cups,1–4,14,15 LowDye taping,9,16,17 corticosteroid injections,1–7,18 platelet-rich plasma injections,1,18–21 botulinum toxin injections,22–24 iontophoresis,17 extracorporeal shock wave therapy,24 and fasciotomy.1–4,7,25
It is understood that in general practice, first-line treatment may include a corticosteroid injection. This may relieve symptoms, especially during an acute flare or even with chronic pain, but recent studies are suggesting that less-invasive techniques may be more effective at providing long-term relief.
A current treatment pathway is provided in Figure 2 to aid in the formulation of a treatment plan. All patients should be counseled that with any conservative treatment option, they should not expect to see significant improvement before six to eight weeks.
Figure 2.
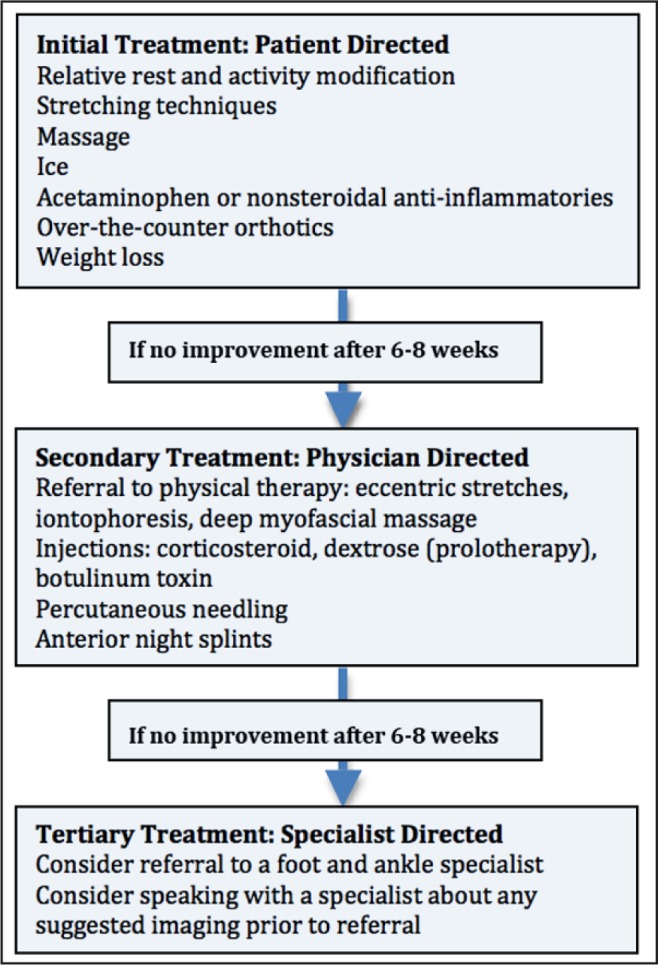
Treatment algorithm
Results of a 2008 query of orthopedic surgeons who are foot-and-ankle specialists showed that for patients with more than 4 months of pain, 74 out of 116 surgeons preferred plantar fascia-specific stretching and supervised physical therapy over anti-inflammatories or corticosteroid injections.25 A 2008 Cochrane Review showed that custom orthotics may not reduce foot pain any more than sham orthotics, over-the-counter orthotics, or night splints and were not any better than stretching alone.9 Night splints are associated with statistically significant improvement, but the cumbersome splints limit patient adherence and, therefore, potential benefits.9,10–13 Fasciotomy may be effective for recalcitrant plantar fasciitis that has not responded to any other conservative treatments. Less well-studied treatments, such as extracorporeal shock wave therapy, iontophoresis, botulinum toxin injections, and platelet-rich plasma injections, have had favorable outcomes but have not yet been tested with randomized, double-blind, placebo-controlled studies.18–25
In all of the literature reviewed, plantar fascia-specific stretching had the best statistically significant long-term results (Figures 3–5). The figures show some of the most widely used and evidence-supported stretches that patients can do at home.
Figure 3.
Calf and arch stretch using a towel. Consider keeping the towel near the bedside and performing before going to sleep and before taking first steps in the morning. Pull back on foot for 30 seconds 3 times with 30 seconds of rest in between.
Figure 5.
Roll plantar fascia with can or ball. Consider keeping at the bedside and performing before going to sleep and before taking first steps in the morning. Roll plantar fascia for 1 minute 3 times with 30 seconds of reset in between.
Figure 4.
Manual plantar fascia stretch with cross-friction massage. Stretch and massage before taking first steps for 1 minute 3 times with 30 seconds of rest in between.
Acknowledgments
Leslie Parker, ELS, provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Young C. In the clinic: plantar fasciitis. Ann Intern Med. 2012 Jan 3;156(1 Pt 1) doi: 10.7326/0003-4819-156-1-201201030-01001. TC1-1, ITC1-2, ITC1-3, ITC1-4, ITC1-5, ITC1-6, ITC1-7, ITC1-8, ITC1-9, ITC1-10, ITC1-11, ITC1-12, ITC1-13, ITC1-14, ITC1-15; quiz ITC1-16. DOI: http://dx.doi.org/10.7326/0003-4819-156-1-201201030-01001. [DOI] [PubMed] [Google Scholar]
- 2.Dyck DD, Jr, Boyajian-O’Neill LA. Plantar fasciitis. Clin J Sport Med. 2004 Sep;14(5):305–9. doi: 10.1097/00042752-200409000-00010. DOI: http://dx.doi.org/10.1097/00042752-200409000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Thomas JL, Christensen JC, Kravitz SR, et al. American College of Foot and Ankle Surgeons heel pain committee. The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. J Foot Ankle Surg. 2010 May-Jun;49(3 Suppl):S1–19. doi: 10.1053/j.jfas.2010.01.001. DOI: http://dx.doi.org/10.1053/j.jfas.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 4.MacAuley D, Best T, editors. Evidence-based sports medicine, Second Edition. London, England: BMJ Books; 2007. [Google Scholar]
- 5.Donley BG, Moore T, Sferra J, Gozdanovic J, Smith R. The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot Ankle Int. 2007 Jan;28(1):20–3. doi: 10.3113/FAI.2007.0004. DOI: http://dx.doi.org/10.3113/FAI.2007.0004. [DOI] [PubMed] [Google Scholar]
- 6.DiGiovanni BF, Nawoczenski DA, Lintal ME, et al. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. J Bone Joint Surg Am. 2003 Jul;85-A(7):1270–7. doi: 10.2106/00004623-200307000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Goff JD, Crawford R. Diagnosis and treatment of plantar fasciitis. Am Fam Physician. 2011 Sep 15;84(6):676–82. [PubMed] [Google Scholar]
- 8.DiGiovanni BF, Nawoczenski DA, Malay DP, et al. Plantar fasica-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up. J Bone Joint Surg Am. 2006 Aug;88(8):1775–81. doi: 10.2106/JBJS.E.01281. DOI: http://dx.doi.org/10.2106/JBJS.E.01281. [DOI] [PubMed] [Google Scholar]
- 9.Crawford F, Thomson C. Interventions for treating plantar heel pain. Cochrane Database Syst Rev. 2003;(3):CD000416. doi: 10.1002/14651858.CD000416. DOI: http://dx.doi.org/10.1002/14651858.CD000416. [DOI] [PubMed] [Google Scholar]
- 10.Powell M, Post WR, Keener J, Wearden S. Effective treatment of chronic plantar fasciitis with dorsiflexion night splints: a crossover prospective randomized outcome study. Foot Ankle Int. 1998 Jan;19(1):10–8. doi: 10.1177/107110079801900103. DOI: http://dx.doi.org/10.1177/107110079801900103. [DOI] [PubMed] [Google Scholar]
- 11.Probe RA, Baca M, Adams R, Preece C. Night splint treatment for plantar fasciitis. A prospective randomized study. Clin Orthop Relat Res. 1999 Nov;(368):190–5. DOI: http://dx.doi.org/10.1097/00003086-199911000-00023. [PubMed] [Google Scholar]
- 12.Berlet GC, Anderson RB, Davis H, Kiebzak GM. A prospective trial of night splinting in the treatment of recalcitrant plantar fasciitis: the Ankle Dorsiflexion Dynasplint. Orthopedics. 2002 Nov;25(11):1273–5. doi: 10.3928/0147-7447-20021101-20. [DOI] [PubMed] [Google Scholar]
- 13.Barry LD, Barry AN, Chen Y. A retrospective study of standing gastrocnemius-soleus stretching versus night splinting in the treatment of planar fasciitis. J Foot Ankle Surg. 2002 Jul-Aug;41(4):221–7. doi: 10.1016/s1067-2516(02)80018-7. [DOI] [PubMed] [Google Scholar]
- 14.Hawke F, Burns J, Radford JA, du Toit V. Custom-made foot orthoses for the treatment of foot pain. Cochrane Database Syst Rev. 2008 Jul;16(3):CD006801. doi: 10.1002/14651858.CD006801.pub2. DOI: http://dx.doi.org/10.1002/14651858.CD006801. [DOI] [PubMed] [Google Scholar]
- 15.Roos E, Engström M, Söderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int. 2006 Aug;27(8):606–11. doi: 10.1177/107110070602700807. DOI: http://dx.doi.org/10.1177/107110070602700807. [DOI] [PubMed] [Google Scholar]
- 16.Hyland MR, Webber-Gaffney A, Cohen L, Lichtman PT. Randomized controlled trial of calcaneal taping, sham taping, and plantar fascia stretching for the short-term management of plantar heel pain. J Orthop Sports Phys Ther. 2006 Jun;36(6):364–71. doi: 10.2519/jospt.2006.2078. DOI: http://dx.doi.org/10.2519/jospt.2006.2078. [DOI] [PubMed] [Google Scholar]
- 17.Osborne HR, Allison GT. Treatment of plantar fasciitis by LowDye taping and iontophoresis: short term results of a double blinded, randomised, placebo controlled clinical trial of dexamethasone and acetic acid. Br J Sports Med. 2006 Jun;40(6):545–9. doi: 10.1136/bjsm.2005.021758. DOI: http://dx.doi.org/10.1136/bjsm.2005.021758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peerbooms JC, van Laar W, Faber F, Schuller HM, van der Hoeven H, Gosens T. Use of platelet rich plasma to treat plantar fasciitis: design of a multi centre randomized controlled trial. BMC Musculoskelet Disord. 2010 Apr;14(11):69. doi: 10.1186/1471-2474-11-69. DOI: http://dx.doi.org/10.1186/1471-2474-11-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sampson S, Gerhardt M, Mandelbaum B. Platelet rich plasma injection grafts for musculoskeletal injuries: a review. Curr Rev Musculoskelet Med. 2008 Dec;1(3–4):165–74. doi: 10.1007/s12178-008-9032-5. DOI: http://dx.doi.org/10.1007/s12178-008-9032-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 2009 Nov;37(11):2259–72. doi: 10.1177/0363546509349921. DOI: http://dx.doi.org/10.1177/0363546509349921. [DOI] [PubMed] [Google Scholar]
- 21.Hall MP, Band PA, Meislin RJ, Jazrawi LM, Cardone DA. Platelet-rich plasma: current concepts and application in sports medicine. J Am Acad Orthop Surg. 2009 Oct;17(10):602–8. doi: 10.5435/00124635-200910000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Placzek R, Deuretzbacher G, Buttgereit F, Meiss AL. Treatment of chronic plantar fasciitis with botulinum toxin A: an open case series with a 1 year follow up. Ann Rheum Dis. 2005 Nov;64(11):1659–61. doi: 10.1136/ard.2005.035840. DOI: http://dx.doi.org/10.1136/ard.2005.035840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang YC, Wei SH, Wang HK, Lieu FK. Ultrasonographic guided botulinum toxin type A for plantar fasciitis: an outcome-based investigation for treating pain and gait changes. J Rehab Med. 2010 Feb;42(2):136–40. doi: 10.2340/16501977-0491. DOI: http://dx.doi.org/10.2340/16501977-0491. [DOI] [PubMed] [Google Scholar]
- 24.Weil LS, Jr, Roukis TS, Weil LS, Borrelli AH. Extracorporeal shock wave therapy for the treatment of chronic plantar fasciitis: indications, protocol, intermediate results, and a comparison of results to fasciotomy. J Foot Ankle Surg. 2002 May-Jun;41(3):166–72. doi: 10.1016/s1067-2516(02)80066-7. DOI: http://dx.doi.org/10.1016/S1067-2516(02)80066-7. [DOI] [PubMed] [Google Scholar]
- 25.DiGiovanni BF, Moore AM, Zlotnicki JP, Pinney SJ. Preferred management of recalcitrant plantar fasciitis among orthopaedic foot and ankle surgeons. Foot Ankle Int. 2012 Jun;33(6):507–12. doi: 10.3113/FAI.2012.0507. DOI: http://dx.doi.org/10.3113/FAI.2012.0507. [DOI] [PubMed] [Google Scholar]





