Abstract
Background
Home visits for older adults aim to prevent cognitive and functional impairment, thus reducing institutionalization and mortality. Visitors may provide information, investigate untreated problems, encourage medication compliance, and provide referrals to services.
Methods and Findings
Data Sources: Ten databases including CENTRAL and Medline searched through December 2012. Study Selection: Randomized controlled trials enrolling community-dwelling persons without dementia aged over 65 years. Interventions included visits at home by a health or social care professional that were not related to hospital discharge. Data Extraction and Synthesis: Two authors independently extracted data. Outcomes were pooled using random effects. Main Outcomes and Measures: Mortality, institutionalization, hospitalization, falls, injuries, physical functioning, cognitive functioning, quality of life, and psychiatric illness.
Results
Sixty-four studies with 28642 participants were included. Home visits were not associated with absolute reductions in mortality at longest follow-up, but some programs may have small relative effects (relative risk = 0.93 [0.87 to 0.99]; absolute risk = 0.00 [−0.01 to 0.00]). There was moderate quality evidence of no overall effect on the number of people institutionalized (RR = 1.02 [0.88 to 1.18]) or hospitalized (RR = 0.96 [0.91 to 1.01]). There was high quality evidence for number of people who fell, which is consistent with no effect or a small effect (odds ratio = 0.86 [0.73 to 1.01]), but there was no evidence that these interventions increased independent living. There was low and very low quality evidence of effects for quality of life (standardised mean difference = −0.06 [−0.11 to −0.01]) and physical functioning (SMD = −0.10 [−0.17 to −0.03]) respectively, but these may not be clinically important.
Conclusions
Home visiting is not consistently associated with differences in mortality or independent living, and investigations of heterogeneity did not identify any programs that are associated with consistent benefits. Due to poor reporting of intervention components and delivery, we cannot exclude the possibility that some programs may be effective.
Introduction
About 13% of Americans and 15–20% of Europeans are over 65 years old [1], and most wish to remain in their own homes for as long as possible [2], [3]. However, functional decline increases with age and can lead to loss of independence and early death [4].
Preventive home visits by health professionals aim to increase autonomy through primary, secondary, and tertiary prevention activities. These differ from home care interventions to treat or to rehabilitate people with medical problems. Some programs focus on one risk factor, such as falls. Others include multidimensional geriatric assessment (MGA) to evaluate and to improve medical, functional, psychosocial, and environmental problems and resources. Whilst proximal outcomes differ, these interventions all ultimately aim to prevent negative long-term outcomes like institutionalization and mortality.
Several previous reviews have argued that home visits are associated with clinical and economic benefits [5]–[9]; however, authors have questioned their active ingredients [10], suggested that resource-demanding processes be replaced with more efficient services [11], and argued that they should be discontinued altogether [12].
The United States Preventive Services Task Force does not recommend multifactorial risk assessment for all community-dwelling elderly due to uncertainty of evidence, but this position may be revised as more information becomes available [13]. As previous reviews about home visits are now outdated [14], an updated synthesis of relevant studies is required to inform guidelines and ongoing research.
Methods
Study selection
We conducted a systematic review and meta-analysis of randomized controlled trials to assess the effectiveness of preventive home visits for community-dwelling older adults (65+ years) without dementia. Through pre-specified subgroup analysis, we also investigated factors that may moderate these effects [15]. Studies that evaluated follow-up home visits directly related to recent hospital discharge (e.g., to assess or to attend a recently treated condition), and studies in which more than 50% of participants had dementia, were excluded.
In December 2012, we searched the following databases from inception and without language restriction: British Nursing Index and Archive, C2-SPECTR, CINAHL, CENTRAL, EMBASE, IBSS, Medline, Nursing Full Text Plus, PsycINFO, and Sociological Abstracts (Text S1). Reference lists from previous reviews and from included studies were examined, and trial authors were contacted for unpublished studies and outcomes.
We analyzed effects on mortality, institutionalization, hospitalization, falls, injuries, physical functioning, cognitive functioning, quality of life, and psychiatric illness. To limit the effects of reporting bias, studies were included based on the characteristics of the participants and interventions rather than the outcomes included in published reports.
Data analysis
Following methods recommended by the Campbell Collaboration and the Cochrane Collaborations [16], two authors independently reviewed all citations and extracted data from included studies, such as: context, recruitment strategy, study inclusion criteria, demographics, content and delivery of the intervention, and outcomes. We assessed each study using the Cochrane Risk of Bias Tool; risk of bias was judged ‘high’ for blinding of personnel and blinding of participants per se.
Authors of included studies were contacted to supply any unreported information and to provide information to permit intention-to-treat analyses. Where possible, dichotomous data were entered directly into Review Manager (RevMan) Version 5.2 [17], and relative risks or rate ratios and 95% confidence intervals (CIs) were calculated using Mantel-Haenszel methods. For dichotomous outcomes that were fully reported in all studies, we also calculated the absolute risk difference. Standardized mean differences (SMDs) and 95% CIs were calculated for continuous measures using Hedges g and combined using inverse variance methods. When studies reported more than one measure of a particular outcome (e.g., psychiatric illness measured using two scales), we averaged the results in Comprehensive Meta-Analysis (CMA) Version 2 [18] before entering data in RevMan 5.2. To estimate event rates in studies reporting the number of events but not reporting time at risk, we assumed that (i) all completers were included for the full duration of the study and (ii) dropouts were at risk for 50% of the year in which they died or left the study. Random-effects models were used due to variability in populations and intervention characteristics across studies. In all forest plots, displays extend beyond the range of probable effects (75% reduction to 400% increase; 4 standard deviations difference in means), and studies are ordered by weight.
For critical outcomes included in the Summary of Findings Table (Table S1), we conducted trim-and-fill analyses [19] to investigate the possibility of reporting bias. Overall confidence in the results was assessed using the Grading of Recommendations Assessment, Development and Evaluation Working Group (GRADE) criteria [20], [21].
Investigation of heterogeneity
Differences among included studies were assessed in terms of their participants, interventions, outcomes, and methods. For each meta-analysis, we also visually inspected forest plots to see if the confidence intervals of individual studies had poor overlap, conducted a Chi2 test, and calculated the I2 statistic. We considered meta-analyses to have important heterogeneity when the p value for Chi2 was less than 0.10 and I2 was greater than 25%.
The following subgroups were analyzed when 10 or more studies were available:
Number of visits (1; 2 to 4; 5 or more);
Visitor's professional group
Participant age (≤70, 71–75, 76–80, 81–85, >85);
-
Intervention components:
Falls only (interventions that exclusively targeted falls prevention, e.g., exercise to improve balance and strength);
MGA (a systematic evaluation of at least 3 of these domains—medical, functional, psychosocial, or environmental);
Both falls prevention and MGA;
Neither falls prevention nor MGA.
Meta-regressions were conducted in STATA [22] for key outcomes (mortality, institutionalization, falls, and functioning) and four moderators (number of visits, participant age, risk of mortality in the control group, and percentage female) using restricted maximum likelihood.
Results
Results of the search
We identified 18784 records, and full texts were obtained for 176 records (Figure S1). Thirty papers were secondary reports of a study reported in another paper; thus, 146 studies were assessed for eligibility. Post-hoc, we included two studies (both identified in the search) in which participants were assigned using quasi-random methods that approximated the characteristics of randomization as described below [23], [24]. Sixty-four studies reported in 86 citations were included in the narrative synthesis (Table S2) [23]–[108], but three of these did not report any outcomes that could be included in a meta-analysis [36], [68], [74].
Seventy-six studies (84 citations) [109]–[192] were excluded for reasons that are enumerated (Table S3). We also identified four ongoing studies [193]–[196] and two studies that could not be obtained [197], [198].
Description of studies
Overall, the 64 included studies assigned 28642 participants, ranging from 59 [44], [73] to 3743 [23], with a median sample size of 299 per study. Follow-up periods ranged from 3 months [44] to 60 months [23].
Studies took place between 1981 [74] and 2012 [56] in 13 countries, but most were conducted in the USA (14), UK (14), or Canada (11). Studies used varying eligibility criteria; some included people at high risk of institutionalization while others recruited from the general population. Between 0% and 33% of control subjects died before the last follow-up. Participants were recruited through primary care providers (24), general population registries (11), community and social service organizations (7), emergency rooms (6), health insurance plan registers (5), advertisements (4), veterans' health organizations (1), and various combinations of the above (3); 3 studies did not report how participants were recruited. Studies included participants aged over 65 years (1), 70 years (10), 75 years (28), 80 years (18), and 85 years (3). In others (4), the mean age was over 70 years, but some participants could have been under 65 years. One of these studies included people aged 17 to 99 years; the mean age was 69 years, and 75% of participants were over 65 years [26].
There was heterogeneity across studies in the number, duration, and focus of visits. Participants received an average of 4.9 (SD = 4.55) visits per study. The number of visits varied by participant in 8 studies. Eleven studies provided one visit per participant, and one study averaged 30 visits per participant. Visitors were nurses alone (27); other professionals, including health visitors, physiotherapists, social workers, and occupational therapists (20); or a combination of health professionals, usually a nurse in combination with another professional (17). Visits had different but overlapping goals, including falls prevention (17), multi-dimensional geriatric assessment (25), both of the above (16), or another prevention (6). Exercise was included in 21 studies. Many studies did not systematically report specific aspects of program design, components that staff actually delivered, or participant take-up.
Comparisons included usual care (50), attention-matched controls including social visits (10), and wait-lists (3); 1 study did not describe the comparison condition. We would have considered comparisons separately, but we could not determine reliably what the comparison groups actually received across different locations, times, and service settings.
Quality of the evidence
Most studies adequately described randomization and were at low risk of bias (41), but sequence generation was unclear in 20 (Figure S2). Allocation concealment was also adequate in 33 studies at low risk of bias, but unclear in 27. Two quasi-random studies were included post-hoc and were rated high risk for randomization and allocation concealment per se [23], [24], but we concluded that the methods of assignment had the desirable characteristics of randomization. One study replaced a few intervention participants and was rated high risk for sequence generation and allocation concealment [92].
Many studies did not describe what happened to participants living in the same household (e.g., husband and wife) and may have randomized small clusters. No study reported that effects were adjusted for clustering; however, studies that explicitly assigned households had cluster sizes close to one.
Subjective outcomes were at high risk of bias for provider and participant blinding; however, mortality, institutionalization, and hospitalization are not likely to have been affected by biased reporting or assessment. Outcome assessors were not blind in 12 studies, which were at high risk of bias for some outcomes, and it was unclear if assessors were blind in 6 studies; other studies were at low risk of bias.
Missing data were unlikely to affect estimates of effects for dichotomous outcomes, including mortality, institutionalization, and hospitalization. As a result, 31 studies were at low risk of bias for incomplete outcome data, 16 studies were unclear, and 17 were at high risk of bias, including two that excluded participants from analyses if they refused visits or did not comply with the protocol [60], [79].
Risk of selective outcome reporting was unclear in 43 studies that did not reference a protocol, and there was high risk of bias in 18 studies that omitted measured outcomes. Only 3 studies were clearly free of selective outcome reporting (i.e., outcomes were registered and reported in full).
In trim-and-fill analyses (Figure S3), there was some evidence of small study bias—studies were trimmed for mortality (3), institutionalization (1), falls (2), and hospitalization (5)—but there was little evidence of benefits, and the adjusted effects were not importantly different from the observed effects.
Quantitative synthesis
Mortality
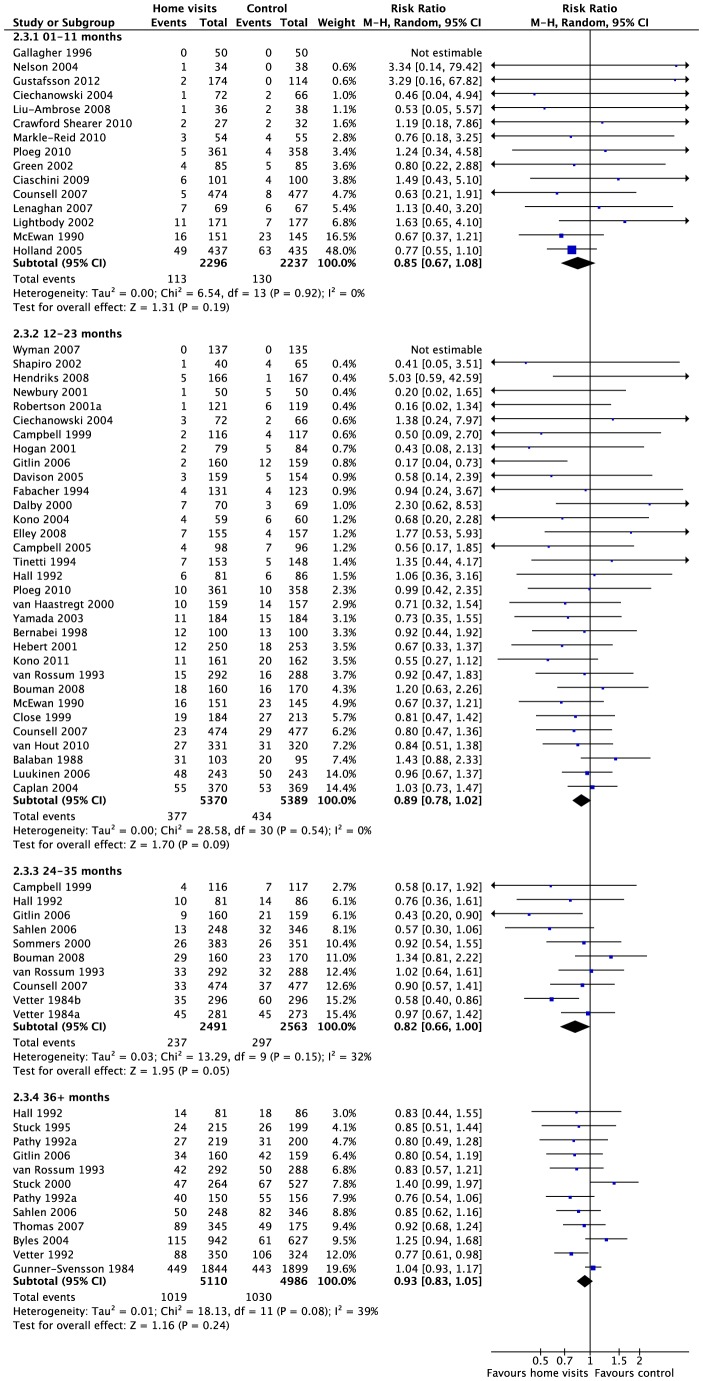
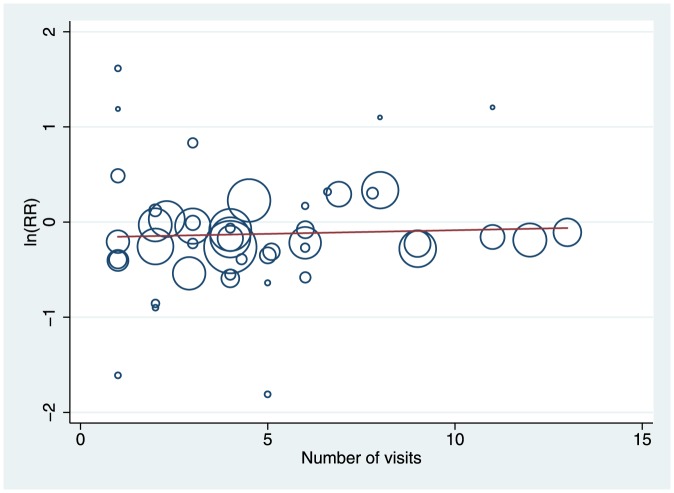
Fifty-three studies (83%) with 23826 participants (83%) reported effects for all-cause mortality. There was high quality evidence of a small relative effect (weighted average) at longest follow-up (Risk ratio = 0.93 [0.87, 0.99]; Chi2 = 54.89, df = 53, p = 0.40; I2 = 3%), but the absolute difference in mortality was close to zero and unlikely to be clinically important (risk difference = 0.00 [−0.01, 0.00]; Chi2 = 64.72, df = 55, p = 0.17; I2 = 15%). Effects for specified follow-up periods were similar to the effect at longest follow-up (Figure 1). Meta-regression did not identify any effects for age (Figure S4) or number of visits (Figure 2); there was a significant relationship with baseline risk of mortality (i.e. annualized risk in the control group), but the relationship was small and unimportant for most studies within the observed range (Figure S4). There was no difference among subgroups when we compared studies by focus of intervention, average age, or number of visits; however, the effect for interventions including both MGA and falls prevention was larger than the effect for either alone. There was some heterogeneity across types of visitors; there was no overall benefit of interventions delivered exclusively by nurses (Figure S5). The data are available as a RevMan 5.2 file (Dataset S1).
Figure 1. Mortality at each follow-up.
All-cause mortality for studies reporting deaths up to 1 year, 2 years, 3 years, and more than 3 years after the start of the trial.
Figure 2. Mortality meta-regression by number of visits.
Circles represent studies (N = 47), size represents weight in the analysis. The slope was not significant (0.008 [95% CI −0.02 to 0.04]; t = 0.53, p = 0.60).
Institutionalization
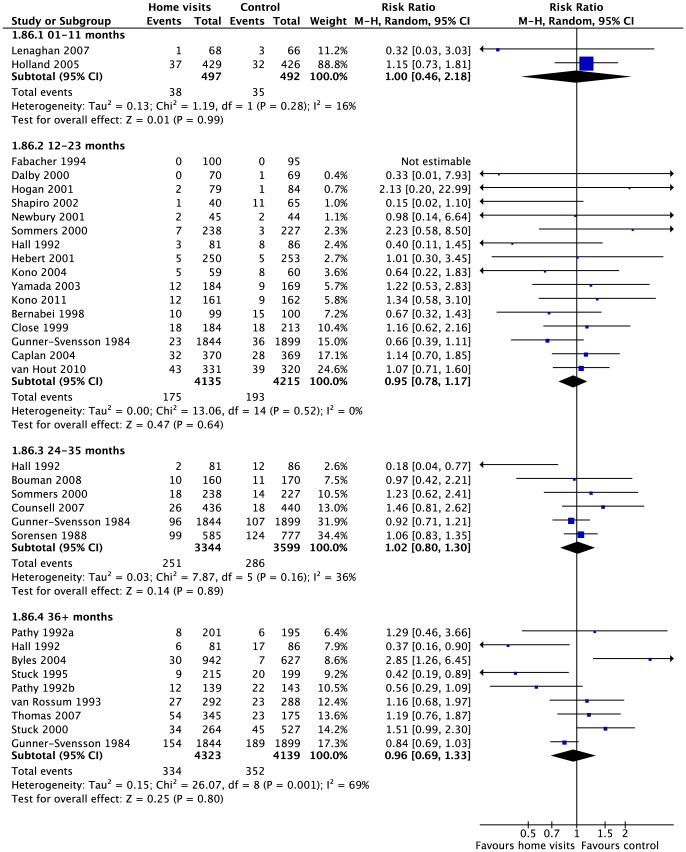
Twenty-six studies (41%) with 16264 participants (57%) reported effects for the number of participants in each group who were admitted to an institution. There was moderate quality evidence of no clinically important difference at longest follow-up in relative effects (risk ratio = 1.02 [0.88, 1.18]; Chi2 = 37.64, df = 26, p = 0.07; I2 = 31%) or absolute effects (risk difference = 0.00 [−0.01, 0.01]; Chi2 = 45.13, df = 27, p = 0.02; I2 = 40%). Effects for specified follow-up periods were similar to the effect at longest follow-up (Figure 3). Meta-regression did not identify any effects for age, number of visits, or risk of mortality. There was no evidence of any differences by time point, focus of visit, age of participants, type of visitor, or number of visits (Table 1).
Figure 3. Institutionalisation at each follow-up.
Number of people living in institution up to 1 year, 2 years, 3 years, and more than 3 years after the start of the trial.
Table 1. Institutionalisation (overall effect and subgroup analyses).
| Home visits | Control | ||||||
| Subgroup | Trials | Events | People | Events | People | Risk Ratio (95% CI), random effects | Heterogeneity I2; Chi2 (p value) |
| All studies | 26 | 667 | 8111 | 700 | 8153 | 1.02 (0.88 to 1.18) | 31%; 37.64 (p = 0.07) |
| Focus of intervention (I2 = 0%; Chi2 = 0.71, p = 0.87) | |||||||
| Falls | 1 | 2 | 79 | 1 | 84 | 2.13 (0.20 to 22.99) | Not applicable |
| MGA | 19 | 552 | 6791 | 596 | 6831 | 0.99 (0.82 to 1.20) | 46%; 35.34 (p = 0.01) |
| Both | 4 | 75 | 844 | 68 | 841 | 1.11 (0.81 to 1.51) | 0%; 0.13 (p = 0.99) |
| Neither | 2 | 38 | 497 | 35 | 492 | 1.00 (0.46 to 2.18) | 16%; 1.19 (p = 0.28) |
| Average age (I2 = 0%; Chi2 = 1.46, p = 0.69) | |||||||
| ≤70 | 1 | 8 | 201 | 6 | 195 | 1.29 (0.46 to 3.66) | Not applicable |
| 71–75 | 1 | 26 | 536 | 18 | 535 | 1.46 (0.81 to 2.62) | Not applicable |
| 76–80 | 15 | 254 | 3450 | 274 | 3377 | 1.03 (0.81 to 1.31) | 30%; 19.90 (p = 0.13) |
| 81–85 | 9 | 225 | 2180 | 213 | 2242 | 1.02 (0.80 to 1.29) | 35%; 12.33 (p = 0.14) |
| Type of visitor (I2 = 49.2%; Chi2 = 3.94, p = 0.14) | |||||||
| Nurse | 15 | 394 | 4550 | 431 | 4693 | 0.95 (0.77 to 1.16) | 36%; 21.93 (p = 0.08) |
| Other | 5 | 86 | 1120 | 96 | 1143 | 0.92 (0.68 to 1.24) | 9%; 5.48 (p = 0.36) |
| Combined | 6 | 187 | 2541 | 173 | 2412 | 1.29 (0.99 to 1.69) | 18%; 6.13 (p = 0.29) |
| Number of visits (I2 = 0%; Chi2 = 0.05, p = 0.98) | |||||||
| 1 | 4 | 124 | 1064 | 149 | 1287 | 1.07 (0.86 to 1.33) | 0%; 0.08 (p = 0.99) |
| 2–4 | 9 | 186 | 2012 | 144 | 1826 | 1.10 (0.90 to 1.36) | 0%; 3.44 (p = 0.90) |
| 5 or more | 10 | 196 | 3170 | 190 | 3085 | 1.08 (0.80 to 1.45) | 51%; 20.46 (p = 0.03) |
Legend: Overall effect on institutionalisation, effects for each subgroup, and tests for differences among subgroups.
Hospitalization
Fifteen studies (23%) including 6288 participants (22%) reported the number of people admitted to hospital in each group (Table 2). At longest follow-up, there was moderate quality evidence of a small relative effect (risk ratio = 0.96 [0.91, 1.01]; Chi2 = 13.70, df = 14, p = 0.47; I2 = 0%) that may not be clinically important (risk difference = −0.01 [−0.03, 0.00]; Chi2 = 13.89, df = 14, p = 0.46; I2 = 0%). There was no evidence of any differences among subgroups, except a statistically significant difference among types of visitors that was consistent with the results for mortality.
Table 2. Outcomes at longest follow-up.
| Participants (events) | |||||
| Outcomes | Trials | Home visits | Control | ES (95% CI), random effects | Heterogeneity I2; Chi2 (p value) |
| Mortality | 53 | 12008 (1589) | 11818 (1672) | Risk = 0.93 (0.87 to 0.99) | 3%; 54.89 (p = 0.40) |
| Institutionalization | |||||
| People admitted | 26 | 8111 (667) | 8153 (700) | Risk = 1.02 (0.88 to 1.18) | 31%; 37.64 (p = 0.07) |
| Days in institution | 4 | 766 | 757 | Rate = 0.78 (0.76 to 0.80) | 100%; 2198.79 (p<0.001) |
| Hospitalization | |||||
| People admitted | 15 | 3167 | 3121 | Risk = 0.96 (0.91 to 1.01) | 0%; 13.70 (p = 0.47) |
| Admissions | 11 | 2476 | 2467 | Rate = 0.93 (0.81 to 1.06) | 61%; 28.07 (p = 0.003) |
| Days in hospital | 12 | 2303 | 2270 | Rate = 0.85 (0.71 to 1.02) | 99%; 909.84 (p<0.001) |
| People attending ER | 12 | 2180 | 2141 | Risk = 0.91 (0.81 to 1.03) | 32%; 16.29 (p = 0.13) |
| ER visits | 10 | 2632 | 3238 | Rate = 0.92 (0.81 to 1.04) | 75%; 35.81 (p<0.001) |
| Falls | |||||
| People who fell | 23 | 3407 | 4048 | Odds = 0.86 (0.73 to 1.01) | 50%; 43.59 (p = 0.004) |
| Number of falls | 15 | 2344 | 2975 | Rate = 0.74 (0.63 to 0.86) | 88%; 113.04 (p<0.001) |
| Fear of falling | 14 | 1349 | 1225 | SMD = −0.16 (−0.26 to −0.07) | 29%; 18.26 (p = 0.15) |
| Injuries | |||||
| People injured | 10 | 1524 | 1531 | Risk = 0.77 (0.63 to 0.95) | 0%; 7.24 (p = 0.61) |
| Number of injuries | 7 | 1558 | 2160 | Rate = 0.98 (0.87 to 1.11) | 0%; 4.32 (p = 0.63) |
| Physical functioning | 27 | 4296 | 4473 | SMD = −0.10 (−0.17 to −0.03) | 53%; 55.40 (p<0.001) |
| Cognitive functioning | 8 | 852 | 756 | SMD = −0.06 (−0.21 to 0.09) | 44%; 12.49 (p = 0.09) |
| Quality of life | 29 | 5136 | 4756 | SMD = −0.06 (−0.11 to −0.01) | 22%; 35.69 (p = 0.15) |
| Psychiatric illness | 15 | 1676 | 1642 | SMD = −0.10 (−0.18 to −0.02) | 22%; 18.06 (p = 0.20) |
Legend: Overall effects at longest follow-up. Rate ratio (Rate); Risk ratio (Risk); Odds Ratio (Odds); Standardised Mean Difference (SMD).
Eleven studies (17%) including 4943 participants (17%) reported the number of admissions to hospital. There was low quality evidence at longest follow-up, which would be consistent with no effect or a small effect (rate ratio = 0.93 [0.81, 1.06]; Chi2 = 28.07, df = 11, p = 0.003; I2 = 61%). There was no evidence of any differences among subgroups except a significant difference among types of visitors that was not consistent with the results for people admitted to hospital or mortality.
Twelve studies (19%) including 4321 participants (15%) reported the number of people who visited an emergency room in each group. There was moderate quality evidence at longest follow-up, which would be consistent with no effect or a small relative effect (risk ratio = 0.91 [0.81, 1.03]; Chi2 = 16.29, df = 11, p = 0.13; I2 = 32%). There was no evidence of any differences among subgroups.
Ten studies (16%) including 5870 participants (20%) reported the number of emergency room visits. There was low quality evidence at longest follow-up, which would be consistent with no effect or a small effect (rate ratio = 0.92 [0.81, 1.04]; Chi2 = 35.81, df = 9, p<0.0001; I2 = 75%). Several differences across subgroups were statistically significant because one group in several analyses included only one study that was inconsistent with others; there were no meaningful differences.
Falls
Twenty-three studies (36%) including 7455 (26%) participants reported the number of people who fell. One study reported an adjusted effect that could not be combined with other measures to estimate a relative risk, so an overall odds ratio was calculated [96]. There was moderate quality evidence of a small effect at longest follow-up, but it was not statistically significant (odds ratio = 0.86 [0.73, 1.01]; Chi2 = 43.59, df = 22, p = 0.004; I2 = 50%). Most effects were measured after about 12 months; two studies reporting longer follow-up found no evidence of extended benefits. Meta-regression did not identify any effects for age, number of visits, or risk of mortality. There was no evidence of any differences among subgroups, though only one study reported falls but did not explicitly target falls prevention.
Fifteen studies (23%) including 5319 (19%) participants reported the number of falls. There was low quality evidence of a small effect at longest follow-up (rate ratio = 0.74 [0.58, 0.93]), but as with days in hospital or days in institution, the results were extremely inconsistent (Chi2 = 4574.87, df = 14, p<0.00001; I2 = 100%). Some subgroups analyses suggested statistical differences among groups, but studies within these groups were also highly heterogeneous; that is, differences between subgroups did not appear to explain the observed heterogeneity.
Physical and cognitive functioning
Twenty-seven studies (42%) including 8769 (31%) participants reported a measure of functioning activities of daily living (ADL) or instrumental activities of daily living (IADL). Several studies reported the number of people dependent or independent (or having difficulty) in specific activities (e.g., eating or dressing), but did not report an estimate of overall functioning [79]. There was very low quality evidence of a small effect on ADLs and IADLs at longest follow-up (SMD = −0.10 [−0.17, −0.03]; Chi2 = 55.40, df = 26, p<0.001; I2 = 53%). Meta-regression did not identify any effects for age, number of visits, or risk of mortality. There was no evidence of any differences among subgroups.
Eight studies (13%) including 1608 (6%) of participants reported a measure of cognitive functioning. There was low quality evidence of no clinically important difference at longest follow-up (SMD = −0.06 [−0.21, 0.09]; Chi2 = 12.49, df = 7, p = 0.09; I2 = 44%). We did not compare subgroups due to a lack of studies.
Quality of life
Twenty-nine studies (45%) including 9892 participants (35%) reported any measure of health-related quality of life. There was low quality evidence of no clinically important difference at longest follow-up (SMD = −0.06 [−0.11, −0.01], Chi2 = 35.69, df = 28, p = 0.15; I2 = 22%). There was no evidence of any significant differences among subgroups.
Psychiatric illness (anxiety and depression)
Fifteen studies (23%) including 3318 participants (12%) reported psychiatric illness (anxiety or depression). There was low quality evidence of a small effect at longest follow-up (SMD = −0.10 [−0.18, 0.02]; Chi2 = 18.06, df = 14, p = 0.20; I2 = 22%). There was no evidence of any differences among subgroups.
Additional analyses
Additional analyses identified no evidence of important benefits for: days in institution, days in hospital, fear of falling, people injured, and number of injuries. These outcomes were infrequently reported and many were heterogeneous (Table 2); subgroup analyses did not reveal any patterns that were inconsistent with the results above (Figure S5).
Discussion
Over the past 20 years, many reviews have investigated the effects of preventive home visiting. Some analyses conclude that comprehensive geriatric assessment may have several benefits [14], [199], but other reviews have come to conflicting conclusions [6], [7], [9], [12], [200], [201] guidelines reflect this uncertainty [13], but this review finds high quality evidence that preventive home visits do not have important effects on mortality or on independent living overall (Table S1). Future guidelines might recommend against these interventions as they do not have proven effects.
Including 64 randomized trials conducted over the three decades, this review is the most comprehensive in scope, and it identified several studies not included in previous analyses. The results include a wide range of outcomes, the main results are statistically precise with little evidence of statistical heterogeneity, and broad inclusion criteria facilitated several pre-specified subgroup analyses. The quality of evidence was high for mortality and moderate for other critical outcomes, and we conclude that these interventions are ineffective overall; however, we cannot exclude the possibility that some programs may be associated with benefits.
Some home visits are part of larger programs that might have positive effects, including exercise, improved assessment by medical professionals, or falls prevention. However, no specific components appeared to distinguish effective programs from ineffective programs for mortality and institutionalization. Consistent with a recent review of interventions to prevent falls [7], we find some evidence that home visits may reduce risk of falling; however, many studies did not have a pre-defined primary outcome, and most studies were not prospectively registered. We interpret these results cautiously because other included studies may have measured proximal outcomes and failed to report them. Furthermore, there was no evidence of effects on distal outcomes among those studies that reported reductions in falls.
An overview of reviews identified a need for further analyses to investigate differences related to the focus of visits, number of visits, characteristics of participants, and characteristics of providers [202]. To the extent possible, this review investigated these variables and failed to identify any patterns across outcomes that would be consistent with benefits overall or consistent with benefits for any defined subgroup. Limited reporting of intervention implementation prevented further investigation into potential mediators and moderators (Figure S6). It is possible that some combination of components in particular populations and settings could yield benefits; however, most studies failed to describe a clear program theory [10]. Some interventions included mostly assessment and recommendations; the efficacy of such interventions depends on adherence to these recommendations (e.g., removing fall hazards, exercising, changing medications) and complementary care. Included trials rarely reported participant compliance and use of other services during the trial. As many of the programs required contacts with local health services, it is impossible to assess effects without a description of usual care for each site at each point in time.
Poorly reported trials waste scare resources [203], [204] and can exacerbate difficulties in systematic reviews of complex interventions [203], [204], yet under-reporting of intervention content and delivery is common [205]–[207]. This review cannot demonstrate if home visits delivered as intended will have insignificant effects; null effects could be related to implementation failure. To produce useful evidence about the effects of complex interventions, researchers must adhere to CONSORT guidelines for reporting trials [204], [208]; report all outcomes measured [209]; and clearly describe program design, delivery, and uptake so that intervention components can be fully considered in systematic reviews [210].
Given the size of this review and the number of previous reviews on this topic, further small studies comparing multi-component preventive home visits to usual care will add very little to the knowledge base. Only a very large trial—or a program of research leading to one—could be justified at this time. Funders should not support further trials unless researchers can explain how new studies would change conclusions drawn from a large body of existing evidence.
Conclusion
Home visiting is not consistently associated with differences in mortality or independent living, and investigations of heterogeneity did not identify any subset of programs that are associated with consistent benefits. Due to poor reporting of intervention components and delivery, we cannot exclude the possibility that some programs may be effective. If researchers continue to evaluate these types of interventions, they should begin with clear theories of change, clearly describe programmes and their implementation, and report all outcomes measured [202], [211], [212].
Supporting Information
PRISMA Chart.
(TIFF)
Risk of bias.
(TIFF)
Main outcomes and tests for reporting bias.
(TIFF)
Meta-regression analyses.
(TIFF)
Results for each follow-up interval, longest follow-up, and subgroup analyses.
(PDF)
Extended table of included studies.
(PDF)
Summary of findings table.
(DOCX)
Table of included studies.
(DOCX)
Table of excluded studies.
(DOCX)
Complete search strategies.
(DOCX)
RevMan 5.2 file.
(RM5)
(DOC)
Acknowledgments
We thank Camilla Thorgaard (Danish National Centre for Social Research) and Karianne Thune Hammerstrom (Norwegian Knowledge Centre for the Health Services) for assistance with the first searches, and G.J. Melendez-Torres (MPhil) at the Centre for Evidence-Based Intervention, University of Oxford, for assistance with generating the meta-regression figures. Thanks also to Terri Pigott (PhD), Jeff Valentine (PhD) from the Campbell Methods Group, and to Nick Huband (PhD), Julia Littell (PhD), Jane Dennis (PhD) from the Campbell Social Welfare Group, and Katherine Hicks (MA) from the Cochrane Dementia and Cognitive Improvement Group, for comments on the protocol and manuscript.
Funding Statement
This work was sponsored by a grant from the Nordic Campbell Centre (Denmark). The authors received internal support from the Centre for Evidence Based Intervention, Department of Social Policy and Intervention, University of Oxford (UK). EMW received internal support from the Centre for Outcomes Research and Effectiveness (CORE), Research Department of Clinical, Educational & Health Psychology, University College London (UK). SG is supported by a linked Clarendon Fund & Green Templeton College Annual Fund Scholarship. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.United Nations (2011) World Population Prospects: The 2010 Revision. New York: United Nations Department of Economic and Social Affairs, Population Division. [Google Scholar]
- 2.Department of Health (2001) National Service Framework for Older People. London: HMSO. [Google Scholar]
- 3.Rostgaard T, Friedberg T (1998) Caring for Children and Older People - A Comparison of European Policies and Practices. Copenhagen: The Danish National Institute of Social Research. [Google Scholar]
- 4. Guralnik J, Ferrucci L (2002) Underestimation of disability occurrence in epidemiological studies of older people: Is research on disability still alive? J Am Geriatr Soc 50: 1599–1601. [DOI] [PubMed] [Google Scholar]
- 5. Beswick AD, Rees K, Dieppe P, Ayis S, Gooberman-Hill R, et al. (2008) Complex interventions to improve physical function and maintain independent living in elderly people: A systematic review and meta-analysis. Lancet 371: 725–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Elkan R, Kendrick D, Dewey M, Hewitt M, Robinson J, et al. (2001) Effectiveness of home based support for older people: Systematic review and meta-analysis. BMJ 323: 719–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, et al. (2009) Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2: CD007146. [DOI] [PubMed] [Google Scholar]
- 8. Michael YL, Whitlock EP, Lin JS, Fu R, O'Connor EA, et al. (2010) Primary care–relevant interventions to prevent falling in older adults: A systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med 153: 815–825. [DOI] [PubMed] [Google Scholar]
- 9. Stuck AE, Egger M, Hammer A, Minder CE, Beck JC (2002) Home visits to prevent nursing home admission and functional decline in elderly people: Systematic review and meta-regression analysis. JAMA 287: 1022–1028. [DOI] [PubMed] [Google Scholar]
- 10. Markle-Reid M, Browne G, Weir R, Gafni A, Roberts J, et al. (2006) The effectiveness and efficiency of home-based nursing health promotion for older people: A review of the literature. Med Care Res Rev 63: 531–569. [DOI] [PubMed] [Google Scholar]
- 11. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381: 752–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. van Haastregt JC, Diederiks JP, van Rossum E, de Witte LP, Crebolder HF (2000) Effects of preventive home visits to elderly people living in the community: Systematic review. BMJ 320: 754–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moyer VA (2012) on behalf of the U.S. Preventive Services Task Force (2012) Prevention of falls in community-dwelling older adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 157: 1–8. [DOI] [PubMed] [Google Scholar]
- 14. Huss A, Stuck AE, Rubenstein LZ, Egger M, Clough-Gorr KM (2008) Multidimensional preventive home visit programs for community-dwelling older adults: A systematic review and meta-analysis of randomized controlled trials. J Gerontol A Biol Sci Med Sci 63A: 298–307. [DOI] [PubMed] [Google Scholar]
- 15. Burton J, Montgomery P, Mayo-Wilson E, Underhill K, Thorgaard C (2009) Protocol for a systematic review: Home visits for prevention of impairment and death in elderly people. Campbell Systematic Reviews 5 (Accessed 21 August 2013). [Google Scholar]
- 16.Higgins J, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: John Wiley & Sons Ltd. [Google Scholar]
- 17.Cochrane Collaboration (2011) Review Manager (RevMan), Version 5.2. Copenhagen: The Nordic Cochrane Centre. [Google Scholar]
- 18.Borenstein M, Hedges L, Higgins J, Rothstein H (2005) Comprehensive Meta-analysis, Version 2. Englewood, NJ: Biostat. [Google Scholar]
- 19. Duval S, Tweedie R (2000) Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56: 455–463. [DOI] [PubMed] [Google Scholar]
- 20. Guyatt G, Oxman A, Schünemann H, Tugwell P, Knotterus A (2010) GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol 64: 380–382. [DOI] [PubMed] [Google Scholar]
- 21. Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, et al. (2011) GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology 64: 401–406. [DOI] [PubMed] [Google Scholar]
- 22.StataCorp (2009) Stata Statistical Software: Release 11.2. College Station, TX: StataCorp LP. [Google Scholar]
- 23. Gunner-Svensson F, Ipsen J, Olsen J, Waldstrom B (1984) Prevention of relocation of the aged in nursing homes. Scand J Prim Health Care 2: 49–56. [DOI] [PubMed] [Google Scholar]
- 24. Sahlen KG, Dahlgren L, Hellner BM, Stenlund H, Lindholm L (2006) Preventive home visits postpone mortality–A controlled trial with time-limited results. BMC Public Health 6: 220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Alessi CA, Stuck AE, Aronow HU, Yuhas KE, Bula CJ, et al. (1997) The process of care in preventive in-home comprehensive geriatric assessment. J Am Geriatr Soc 45: 1044–1050. [DOI] [PubMed] [Google Scholar]
- 26. Balaban DJ, Goldfarb NI, Perkel RL, Carlson BL (1988) Follow-up study of an urban family medicine home visit program. J Fam Pract 26: 307–312. [PubMed] [Google Scholar]
- 27. Bernabei R, Landi F, Gambassi G, Sgadari A, Zuccala G, et al. (1998) Randomised trial of impact of model of integrated care and case management for older people living in the community. BMJ 316: 1348–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bouman A, Van Rossum E, Ambergen T, Kempen G, Knipschild P (2008) Effects of a home visiting program for older people with poor health status: A randomized, clinical trial in the Netherlands. J Am Geriatr Soc 56: 397–404. [DOI] [PubMed] [Google Scholar]
- 29. Bouman A, Van Rossum E, Evers SM, Ambergen T, Kempen G, et al. (2008) Effects on health care use and associated cost of a home visiting program for older people with poor health status: A randomized clinical trial in the Netherlands. J Gerontol A Biol Sci Med Sci 63A: 291–297. [DOI] [PubMed] [Google Scholar]
- 30. Büla CJ, Alessi CA, Aronow HU, Yubas K, Gold M, et al. (1995) Community physicians' co-operation with a program of in-home comprehensive geriatric assessment. J Am Geriatr Soc 43: 1016–1020. [DOI] [PubMed] [Google Scholar]
- 31. Byles JE, Tavener M, O'Connell RL, Nair BR, Higginbotham NH, et al. (2004) Randomised controlled trial of health assessments for older Australian veterans and war widows. Med J Aust 181: 186–190. [DOI] [PubMed] [Google Scholar]
- 32. Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM (1999) Falls prevention over 2 years: A randomized controlled trial in women 80 years and older. Age Ageing 28: 513–518. [DOI] [PubMed] [Google Scholar]
- 33. Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, et al. (1997) Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 315: 1065–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Campbell AJ, Robertson MC, La Grow SJ, Kerse NM, Sanderson GF, et al. (2005) Randomised controlled trial of prevention of falls in people aged > or = 75 with severe visual impairment: The VIP trial. BMJ 331: 817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Caplan GA, Williams AJ, Daly B, Abraham K (2004) A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department–The DEED II Study. J Am Geriatr Soc 52: 1417–1423. [DOI] [PubMed] [Google Scholar]
- 36. Chandler JM, Duncan PW, Kochersberger G, Studenski S (1998) Is lower extremity strength gain associated with improvement in physical performance and disability in frail, community-dwelling elders? Arch Phys Med Rehabil 79: 24–30. [DOI] [PubMed] [Google Scholar]
- 37. Ciaschini PM, Straus SE, Dolovich LR, Goeree RA, Leung KM, et al. (2008) Community-based randomised controlled trial evaluating falls and osteoporosis risk management strategies. Trials 9: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ciaschini PM, Straus SE, Dolovich LR, Goeree RA, Leung KM, et al. (2009) Community-based intervention to optimise falls risk management: A randomised controlled trial. Age Ageing 38: 724–730. [DOI] [PubMed] [Google Scholar]
- 39. Ciechanowski P, Wagner E, Schmaling K, Schwartz S, Williams B, et al. (2004) Community-integrated home-based depression treatment in older adults: A randomized controlled trial. JAMA 291: 1569–1577. [DOI] [PubMed] [Google Scholar]
- 40. Close J, Ellis M, Hooper R, Glucksman E, Jackson S, et al. (1999) Prevention of falls in the elderly trial (PROFET): A randomised controlled trial. Lancet 353: 93–97. [DOI] [PubMed] [Google Scholar]
- 41. Counsell SR, Callahan CM, Buttar AB, Clark DO, Frank KI (2006) Geriatric Resources for Assessment and Care of Elders (GRACE): A new model of primary care for low-income seniors. J Am Geriatr Soc 54: 1136–1141. [DOI] [PubMed] [Google Scholar]
- 42. Counsell SR, Callahan CM, Clark D, Tu W, Buttar AB, et al. (2007) Geriatric care management for low-income seniors: A randomized controlled trial. JAMA 298: 2623–2633. [DOI] [PubMed] [Google Scholar]
- 43. Counsell SR, Callahan CM, Tu W, Stump TE, Arling GW (2009) Cost analysis of the geriatric resources for assessment and care of elders care management intervention. J Am Geriatr Soc 57: 1420–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Crawford Shearer NB, Fleury JD, Belyea M (2010) Randomized control trial of the Health Empowerment Intervention: Feasibility and impact. Nurs Res 59: 203–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Dahlin-Ivanoff S, Gosman–Hedström G, Edberg AK, Wilhelmson K, Eklund K, et al. (2010) Elderly persons in the risk zone. Design of amultidimensional, health-promoting, randomised three-armed controlled trial for “prefrail” people of 80+ years living at home. BMC Geriatr 10: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dalby DM, Sellors JW, Fraser FD, Fraser C, van Ineveld C, et al. (2000) Effect of preventive home visits by a nurse on the outcomes of frail elderly people in the community: A randomized controlled trial. CMAJ 162: 497–500. [PMC free article] [PubMed] [Google Scholar]
- 47. Davison J, Bond J, Dawson P, Steen IN, Kenny RA (2005) Patients with recurrent falls attending Accident & Emergency benefit from multifactorial intervention - a randomised controlled trial. Age Ageing 34: 162–168. [DOI] [PubMed] [Google Scholar]
- 48. Elley CR, Robertson MC, Garrett S, Kerse NM, McKinlay E, et al. (2008) Effectiveness of a falls-and-fracture nurse coordinator to reduce falls: A randomized, controlled trial of at-risk older adults. J Am Geriatr Soc 56: 1383–1389. [DOI] [PubMed] [Google Scholar]
- 49. Elley CR, Robertson MC, Kerse NM, Garrett S, McKinlay E, et al. (2007) Falls Assessment Clinical Trial (FACT): Design, interventions, recruitment strategies and participant characteristics. BMC Public Health 7: 185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Fabacher D, Josephson K, Pietruszka F, Linderborn K, Morley JE, et al. (1994) An in-home preventive assessment program for independent older adults: A randomized controlled trial. J Am Geriatr Soc 42: 630–638. [DOI] [PubMed] [Google Scholar]
- 51. Gallagher E, Brunt H (1996) Head over heels: Impact of a health promotion program to reduce falls in the elderly. Can J Aging 15: 84–96. [Google Scholar]
- 52. Gitlin LN, Hauck WW, Dennis MP, Winter L, Hodgson N, et al. (2009) Long-term effect on mortality of a home intervention that reduces functional difficulties in older adults: Results from a randomized trial. J Am Geriatr Soc 57: 476–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gitlin LN, Hauck WW, Winter L, Dennis MP, Schulz R (2006) Effect of an in-home occupational and physical therapy intervention on reducing mortality in functionally vulnerable older people: Preliminary findings. J Am Geriatr Soc 54: 950–955. [DOI] [PubMed] [Google Scholar]
- 54. Gitlin LN, Winter L, Dennis MP, Corcoran M, Schinfeld S, et al. (2006) A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc 54: 809–816. [DOI] [PubMed] [Google Scholar]
- 55. Green J, Forster A, Bogle S, Young J (2002) Physiotherapy for patients with mobility problems more than l year after stroke: A randomised controlled trial. Lancet 359: 199–203. [DOI] [PubMed] [Google Scholar]
- 56. Gustafsson S, Wilhelmson K, Eklund K, Gosman-Hedström G, Zidén L, et al. (2012) Health-promoting interventions for persons aged 80 and older are successful in the short term—Results from the randomized and three-armed elderly persons in the risk zone study. J Am Geriatr Soc 60: 447–454. [DOI] [PubMed] [Google Scholar]
- 57. Hall N, De BP, Johnson D, Mackinnon K, Gutman G, et al. (1992) Randomized trial of a health promotion program for frail elders. Can J Aging 11: 72–91. [Google Scholar]
- 58. Hebert R, Robichaud L, Roy PM, Bravo G, Voyer L (2001) Efficacy of a nurse-led multidimensional preventive programme for older people at risk of functional decline. A randomized controlled trial. Age Ageing 30: 147–153. [DOI] [PubMed] [Google Scholar]
- 59. Hendriks MR, Bleijlevens MH, van Haastreght JC, Crebolder HF, Diederiks JP, et al. (2008) Lack of effectiveness of a multidisciplinary fall-prevention program in elderly people at risk: A randomized, controlled trial. J Am Geriatr Soc 56: 1390–1397. [DOI] [PubMed] [Google Scholar]
- 60. Hogan DB, MacDonald FA, Betts J, Bricker S, Ebly EM, et al. (2001) A randomized controlled trial of a community-based consultation service to prevent falls. CMAJ 165: 537–543. [PMC free article] [PubMed] [Google Scholar]
- 61. Holland R, Lenaghan E, Harvey I, Smith R, Shepstone L, et al. (2005) Does home based medication review keep older people out of hospital? The HOMER randomised controlled trial. BMJ 330: 393–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Holland R, Lenaghan E, Smith R, Lipp A, Christou M, et al. (2006) Delivering a home- based medication review, process measures from the HOMER randomised controlled trial. Int J Pharm Pract 14: 71–79. [Google Scholar]
- 63. Huang T, Acton GJ (2004) Effectiveness of home visit falls prevention strategy for Taiwanese community-dwelling elders: Randomized trial. Public Health Nurs 21: 247–256. [DOI] [PubMed] [Google Scholar]
- 64. Kingston P, Jones M, Lally F, Crome P (2001) Older people and falls: A randomized controlled trial of a health visitor (HV) intervention. Rev Clin Gerontol 11: 209–214. [Google Scholar]
- 65. Kono A, Fujita T, Tsumura C, Kondo T, Kushiyama K, et al. (2009) Preventive home visit model targeted to specific care needs of ambulatory frail elders: Preliminary report of a randomized trial design. Aging Clin Exp Res 21: 167–173. [DOI] [PubMed] [Google Scholar]
- 66. Kono A, Kai I, Sakato C, Harker JO, Rubenstein LZ (2004) Effect of preventive home visits for ambulatory housebound elders in Japan: A pilot study. Aging Clin Exp Res 16: 293–299. [DOI] [PubMed] [Google Scholar]
- 67. Kono A, Kanaya Y, Fujita T, Tsumura C, Kondo T, et al. (2011) Effects of a preventive home visit program in ambulatory frail older people: A randomized controlled trial. J Gerontol A Biol Sci Med Sci 67A: 302–309. [DOI] [PubMed] [Google Scholar]
- 68. Krebs DE, Jette AM, Assmann SF (1998) Moderate exercise improves gait stability in disabled elders. Arch Phys Med Rehabil 79: 1489–1495. [DOI] [PubMed] [Google Scholar]
- 69. La Grow SJ, Robertson MC, Campbell AJ, Clarke GA, Kerse NM (2006) Reducing hazard related falls in people 75 years and older with significant visual impairment: How did a successful program work? Inj Prev 12: 296–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Lenaghan E, Holland R, Brooks A (2007) Home-based medication review in a high risk elderly population in primary care–The POLYMED randomised controlled trial. Age Ageing 36: 292–297. [DOI] [PubMed] [Google Scholar]
- 71. Lightbody E, Watkins C, Leathley M, Sharma A, Lye M (2002) Evaluation of a nurse-led fallsprevention programme versus usual care: A randomized controlled trial. Age Ageing 31: 203–210. [DOI] [PubMed] [Google Scholar]
- 72. Lin MR, Wolf SL, Hwang HF, Gong SY, Chen CY (2007) A randomized, controlled trial of fall prevention programs and quality of life in older fallers. J Am Geriatr Soc 55: 499–506. [DOI] [PubMed] [Google Scholar]
- 73. Liu-Ambrose T, Donaldson MG, Ahamed Y, Graf P, Cook WL, et al. (2008) Otago home-based strength and balance retraining improves executive functioning in older fallers: A randomized controlled trial. J Am Geriatr Soc 56: 1821–1830. [DOI] [PubMed] [Google Scholar]
- 74. Luker KA (1981) Health visiting and the elderly. Nurs Times 77: 137–140. [Google Scholar]
- 75. Luukinen H, Lehtola S, Jokelainen J, Väänänen-Sainio R, Lotvonen S, et al. (2006) Prevention of disability by exercise among the elderly: A population-based, randomized, controlled trial. Scand J Prim Health Care 24: 199–205. [DOI] [PubMed] [Google Scholar]
- 76. Luukinen H, Lehtola S, Jokelainen J, Väänänen-Sainio R, Lotvonen S, et al. (2007) Pragmatic exercise-oriented prevention of falls among the elderly: A population-based, randomized, controlled trial. Preventive Medicine 44: 265–271. [DOI] [PubMed] [Google Scholar]
- 77. Markle-Reid M, Browne G, Gafni A, Roberts J, Weir R, et al. (2010) The effects and costs of a multifactorial and interdisciplinary team approach to falls prevention for older home care clients ‘at risk’ for falling: A randomized controlled trial. Can J Aging 29: 139–161. [DOI] [PubMed] [Google Scholar]
- 78. Markle-Reid M, Weir R, Browne G, Roberts J, Gafni A, et al. (2006) Health promotion for frail older home care clients. J Adv Nurs 54: 381–395. [DOI] [PubMed] [Google Scholar]
- 79. McEwan RT, Davison N, Forster DP, Pearson P, Stirling E (1990) Screening elderly people in primary care: A randomized controlled trial. Br J Gen Pract 40: 94–97. [PMC free article] [PubMed] [Google Scholar]
- 80. Nelson ME, Layne JE, Bernstein MJ, Nuernberger A, Castaneda C, et al. (2004) The effects of multidimensional home-based exercise on functional performance in elderly people. J Gerontol A Biol Sci Med Sci 59A: 154–160. [DOI] [PubMed] [Google Scholar]
- 81.Newbury J (2001) 75+ health assessments: A randomised controlled trial: Adelaide University.
- 82. Newbury JW, Marley JE, Beilby JJ (2001) A randomised controlled trial of the outcome of health assessment of people aged 75 years and over. Med J Aust 175: 104–107. [DOI] [PubMed] [Google Scholar]
- 83. Nicolaides-Bouman A, van Rossum E, Habets H, Kempen GI, Knipschild P (2007) Home visiting programme for older people with health problems: Process evaluation. J Adv Nurs 58: 425–435. [DOI] [PubMed] [Google Scholar]
- 84. Nicolaides-Bouman A, van Rossum E, Kempen GI, Knipschild P (2004) Effects of home visits by home nurses to elderly people with health problems: Design of a randomised clinical trial in the Netherlands. BMC Health Serv Res 4: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Pacini M, Smith RD, Wilson EC, Holland R (2007) Home-based medication review in older people: Is it cost effective? Pharmacoeconomics 25: 171–180. [DOI] [PubMed] [Google Scholar]
- 86. Pathy MS, Bayer A, Harding K, Dibble A (1992) Randomised trial of case finding and surveillance of elderly people at home. Lancet 340: 890–893. [DOI] [PubMed] [Google Scholar]
- 87. Pighills AC, Torgerson DJ, Sheldon TA, Drummond AE, Bland JM (2011) Environmental assessment and modification to prevent falls in older people. J Am Geriatr Soc 59: 26–33. [DOI] [PubMed] [Google Scholar]
- 88. Ploeg J, Brazil K, Hutchison B, Kaczorowski J, Dalby DM, et al. (2010) Effect of preventive primary care outreach on health related quality of life among older adults at risk of functional decline: Randomised controlled trial. BMJ 340: c1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Robertson MC, Devlin N, Gardner MM, Campbell AJ (2001) Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: Randomised controlled trial. BMJ 322: 697–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Robertson MC, Devlin N, Scuffham P, Gardner MM, Buchner DM, et al. (2001) Economic evaluation of a community based exercie programme to prevent falls. J Epidemiol Community Health 55: 600–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Rubenstein LZ, Aronow HU, Schloe M, Steiner A, Alessi CA, et al. (1994) A home-based geriatric assessment, follow-up and health promotion program: Design, methods, and baseline findings from a 3-year randomized clinical trial. Aging Clin Exp Res 6: 105–120. [DOI] [PubMed] [Google Scholar]
- 92. Shapiro A, Taylor K (2002) Effects of a community-based early intervention program on the subjective well-being, institutionalization, and mortality of low-income elders. Gerontologist 42: 334–341. [DOI] [PubMed] [Google Scholar]
- 93. Sommers LS, Marton KI, Barbaccia JC, Randolph J (2000) Physician, nurse, and social worker collaboration in primary care for chronically ill seniors. Arch Intern Med 1825–1833. [DOI] [PubMed] [Google Scholar]
- 94. Sorensen KH, Silvertsen J (1988) Follow-up three years after intervention to relieve unmet medical and social needs of old people. Compr Gerontol B 2: 85–89. [PubMed] [Google Scholar]
- 95. Stevens M, Holman CDA, Bennett N (2001) Preventing falls in older people: Impact of an intervention to reduce environmental hazards in the home. J Am Geriatr Soc 49: 1442–1447. [DOI] [PubMed] [Google Scholar]
- 96. Stevens M, Holman CDA, Bennett N, de Klerk N (2001) Preventing falls in older people: Outcome evaluation of a randomized controlled trial. J Am Geriatr Soc 49: 1455. [DOI] [PubMed] [Google Scholar]
- 97. Stuck AE, Aronow HU, Steiner A, Alessi CA, Büla CJ, et al. (1995) A trial of annual in-home comprehensive geriatric assessments for elderly people living in the community. N Engl J Med 333: 1184–1189. [DOI] [PubMed] [Google Scholar]
- 98. Stuck AE, Minder CE, Peter-Wuest I, Gillmann G, Egli C, et al. (2000) A randomized trial of in-home visits for disability prevention in community-dwelling older people at low and high risk for nursing home admission. Arch Intern Med 160: 977–986. [DOI] [PubMed] [Google Scholar]
- 99. Thomas R, Worrall G, Elgar F, Knight J (2007) Can they keep going on their own? A four-year randomized trial of functional assessments of community residents. Can J Aging 26: 379–389. [DOI] [PubMed] [Google Scholar]
- 100. Tinetti ME, Baker DI, Garrett PA, Gottschalk M, Koch ML, et al. (1993) Yale FICSIT: Risk factor abatement strategy for fall prevention. J Am Geriatr Soc 41: 315–320. [DOI] [PubMed] [Google Scholar]
- 101. Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, et al. (1994) A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med 331: 821–827. [DOI] [PubMed] [Google Scholar]
- 102. van Haastregt JC, Diederiks JP, van Rossum E, de Witte LP, Voorhoeve PM, et al. (2000) Effects of a programme of multifactorial home visits on falls and mobility impairments in elderly people at risk: Randomised controlled trial. BMJ 321: 994–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. van Hout HP, Jansen AP, van Marwijk HW, Pronk M, Frijters DF, et al. (2010) Prevention of adverse health trajectories in a vulnerable elderly population through nurse home visits: A randomized controlled trial. J Gerontol A Biol Sci Med Sci 65: 734–742. [DOI] [PubMed] [Google Scholar]
- 104. van Rossum E, Frederiks CM, Philipsen H, Portengen K, Wiskerke J, et al. (1993) Effects of preventive home visits to elderly people. BMJ 307: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Vetter NJ, Jones DA, Victor CR (1984) Effect of health visitors working with elderly patients in general practice: A randomised controlled trial. BMJ 288: 369–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Vetter NJ, Lewis PA, Ford D (1992) Can health visitors prevent fractures in elderly people? BMJ 304: 888–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Wyman JF, Croghan CF, Nachreiner NM, Gross CR, Stock HH, et al. (2007) Effectiveness of education and individualized counseling in reducing environmental hazards in the homes of community-dwelling older women. J Am Geriatr Soc 55: 1548–1556. [DOI] [PubMed] [Google Scholar]
- 108. Yamada Y, Ikegami N (2003) Preventive home visits for community-dwelling frail elderly people based on Minimum Data Set-Home Care: Randomised controlled trial. Geriatr Gerontol Int 3: 236–242. [Google Scholar]
- 109. Archbold PG, Stewart BJ, Miller LL, Harvath TA, Greenlick MR, et al. (1995) The PREP system of nursing interventions: A pilot test with families caring for older members. Res Nurs Health 18: 3–16. [DOI] [PubMed] [Google Scholar]
- 110. Carpenter GI, Demopoulos GR (1990) Screening the elderly in the community: Controlled trial of dependency surveillance using a questionnaire administered by volunteers. BMJ 300: 1253–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Clarke M, Clarke SJ, Jagger C (1992) Social intervention and the elderly: A randomized controlled trial. Am J Epidemiol 136: 1517–1523. [DOI] [PubMed] [Google Scholar]
- 112. Clemson L, Cumming RG, Kendig H, Swann M, Heard R, et al. (2004) The effectiveness of a community-based program for reducing the incidence of falls in the elderly: A randomized trial. J Am Geriatr Soc 52: 1487–1494. [DOI] [PubMed] [Google Scholar]
- 113. Comans TA, Brauer SG, Haines TP (2010) Randomized trial of domiciliary versus center-based rehabilitation: Which is more effective in reducing falls and improving quality of life in older fallers? J Gerontol A Biol Sci Med Sci 65: 672–679. [DOI] [PubMed] [Google Scholar]
- 114. Dapp U, Anders J, von Renteln-Kruse W, Meier-Baumgartner HP (2005) Active health promotion in old age: Methodology of a preventive intervention programme provided by an interdisciplinary health advisory team for independent older people. J Public Health (Oxf) 13: 122–127. [Google Scholar]
- 115. Dapp U, Anders JAM, von Renteln-Kruse W, Minder CE, Meier-Baumgartner HP, et al. (2011) A randomized trial of effects of health risk appraisal combined with group sessions or home visits on preventive behaviors in older adults. J Gerontol A Biol Sci Med Sci 66A: 591–598. [DOI] [PubMed] [Google Scholar]
- 116. Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, et al. (2002) Randomised factorial trial of falls prevention among older people living in their own homes. BMJ 325: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. de Vries OJ, Peeters GM, Elders PJ, Muller M, Knol DL, et al. (2010) Multifactorial intervention to reduce falls in older people at high risk of recurrent falls: A randomized controlled trial. Arch Intern Med 170: 1110–1117. [DOI] [PubMed] [Google Scholar]
- 118. Dunn RB, Lewis PA, Vetter NJ, Guy PM, Hardman CS, et al. (1994) Health visitor intervention to reduce days of unplanned hospital re-admission in patients recently discharged from geriatric wards: The results of a randomised controlled study. Arch Gerontol Geriatr 18: 15–23. [DOI] [PubMed] [Google Scholar]
- 119. Engelhardt JB, Toseland RW, O'Donnell JC, Richie JT, Jue D, et al. (1996) The effectiveness and efficiency of outpatient geriatric evaluation and management. J Am Geriatr Soc 44: 847–856. [DOI] [PubMed] [Google Scholar]
- 120. Epstein AM, Hall JA, Fretwell M, Feldstein M, DeCiantis ML, et al. (1990) Consultative geriatric assessment for ambulatory patients. A randomized trial in a health maintenance organization. JAMA 263: 538–544. [PubMed] [Google Scholar]
- 121. Ettinger WH, Burns R, Messier SP, Applegate W, Rejeski WJ, et al. (1997) A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST). JAMA 277: 25–31. [PubMed] [Google Scholar]
- 122. Fairhall N, Aggar C, Kurrle SE, Sherrington C, Lord S, et al. (2008) Frailty intervention trial (FIT). BMC Geriatr 8: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Fletcher AE, Price GM, Ng ESW, Stirling SL, Bulpitt CJ, et al. (2004) Population-based multidimensional assessment of older people in UK general practice: A cluster-randomised factorial trial. Lancet 364: 1667–1677. [DOI] [PubMed] [Google Scholar]
- 124. Flood C, Mugford M, Stewart S, Harvey I, Poland F, et al. (2005) Occupational therapy compared with social work assessment for older people. An economic evaluation alongside the CAMELOT randomised controlled trial. Age Ageing 34: 47–52. [DOI] [PubMed] [Google Scholar]
- 125. Fordyce M, Bardole D, Romer L, Soghikian K, Fireman B (1997) Senior Team Assessment and Referral Program–STAR. J Am Board Fam Pract 10: 398–406. [PubMed] [Google Scholar]
- 126. Fox PJ, Vazquez L, Tonner C, Stevens JA, Fineman N, et al. (2010) A randomized trial of a multifaceted intervention to reduce falls among community-dwelling adults. Health Educ Behav 37: 831–848. [DOI] [PubMed] [Google Scholar]
- 127. German PS, Burton LC, Shapiro S, Steinwachs DM, Tsuji I, et al. (1995) Extended coverage for preventive services for the elderly: Response and results in a demonstration population. Am J Public Health 85: 379–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Gill TM, Baker DI, Gottschalk M, Peduzzi PN, Allore H, et al. (2002) A program to prevent functional decline in physically frail, elderly persons who live at home. N Engl J Med 347: 1068–1074. [DOI] [PubMed] [Google Scholar]
- 129. Gill TM, Baker DI, Gottschalk M, Peduzzi PN, Allore H, et al. (2004) A prehabilitation program for the prevention of functional decline: Effect on higher-level physical function. Arch Phys Med Rehabil 85: 1043–1049. [DOI] [PubMed] [Google Scholar]
- 130.Graham SA (2006) Effects of a home-based physical activity program implemented by a trained caregiver on the physical function of community-dwelling older adults: The University of Texas.
- 131. Hansen FR, Spedtsberg K, Schroll M (1992) Geriatric follow-up by home visits after discharge from hospital: A randomized controlled trial. Age Ageing 21: 445–450. [DOI] [PubMed] [Google Scholar]
- 132. Hay WI, Van Ineveld C, Browne G, Roberts J, Bell B, et al. (1998) Prospective care of elderly patients in family practice. Is screening effective? Can Fam Physician 44: 2677–2687. [PMC free article] [PubMed] [Google Scholar]
- 133. Hendriksen C, Lund E, Stromgard E (1984) Consequences of assessment and intervention among elderly people: A three year randomised controlled trial. BMJ 289: 1522–1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Hornbrook MC, Stevens VJ, Wingfield DJ, Hollis JF, Greenlick MR, et al. (1994) Preventing falls among community-dwelling older persons: Results from a randomized trial. Gerontologist 34: 16–23. [DOI] [PubMed] [Google Scholar]
- 135. June KJ, Lee JY, Yoon JL (2009) Effects of case management using Resident Assessment Instrument-Home Care (RAI-HC) in home health services for older people. J Korean Acad Nurs 39: 366–375. [DOI] [PubMed] [Google Scholar]
- 136. Karatay G, Akkus Y (2012) Effectiveness of a multistimulant home-based program on cognitive function of older adults. West J Nurs Res 34: 883–901. [DOI] [PubMed] [Google Scholar]
- 137. Kerse NM, Flicker L, Jolley D, Arroll B, Young D (1999) Improving the health behaviours of elderly people: Randomised controlled trial of a general practice education programme. BMJ 319: 683–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Kronborg C, Vass M, Lauridsen J, Avlund K (2006) Cost effectiveness of preventive home visits to the elderly: Economic evaluation alongside randomized controlled study. Eur J Health Econ 7: 238–246. [DOI] [PubMed] [Google Scholar]
- 139. Legault C, Jennings JM, Katula JA, Dagenbach D, Gaussoin SA, et al. (2011) Designing clinical trials for assessing the effectsof cognitive training and physical activityinterventions on cognitive outcomes: The Seniors Health and Activity Research Program Pilot (SHARP-P) Study, a randomized controlled trial. BMC Geriatr 11: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Leveille SG, Wagner EH, Davis C, Grothaus L, Wallace J, et al. (1998) Preventing disability and managing chronic illness in frail older adults: A randomized trial of a community-based partnership with primary care. J Am Geriatr Soc 46: 1191–1198. [DOI] [PubMed] [Google Scholar]
- 141. Mahoney JE, Shea TA, Przybelski R, Jaros L, Gangnon R, et al. (2007) Kenosha County falls prevention study: A randomized, controlled trial of an intermediate-intensity, community-based multifactorial falls intervention. J Am Geriatr Soc 55: 489–498. [DOI] [PubMed] [Google Scholar]
- 142. Mann WC, Ottenbacher KJ, Fraas L, Tomita M, Granger CV (1999) Effectiveness of assistive technology and environmental interventions in maintaining independence and reducing home care costs for the frail elderly. Arch Fam Med 8: 210–217. [DOI] [PubMed] [Google Scholar]
- 143. Matzen LE, Foged L, Pedersen P, Wengle K, Andersen-Ranberg K (2007) Geriatric home visits can prevent hospitalisation of subacute patients but is timeconsuming–A randomised study. [Geriatrisk teambesog kan forebygge indlaeggelse af subakut henvistepatienter, men er et tidskraevende tilbud: En randomiseret undersogelse]. Ugeskr Laeger 169: 2113–2118. [PubMed] [Google Scholar]
- 144. Matzen LE, Foged L, Pedersen P, Wengler K, Andersen-Ranberg K (2007) Primary visitation of elective referred geriatric patients–a randomised study of home visits compared to day hospital visits. [Primaer visitation af elektive geriatriske patienter. Enrandomiseret undersogelse af hjemmebesog kontra ambulantbesog]. Ugeskr Laeger 169: 2109–2113. [PubMed] [Google Scholar]
- 145. McMurdo MET, Johnstone R (1995) A randomized controlled trial of a home exercise programme for elderly people with poor mobility. Age Ageing 24: 425–428. [DOI] [PubMed] [Google Scholar]
- 146. Melin AL, Bygren LO (1992) Efficacy of the rehabilitation of elderly primary health care patients after short-stay hospital treatment. Med Care 30: 1004–1015. [DOI] [PubMed] [Google Scholar]
- 147. Melis RJ, van Eijken MI, Borm GF, Wensing M, Adang E, et al. (2005) The design of the Dutch EASYcare study: A randomised controlled trial on the effectiveness of a problem-based community intervention model for frail elderly people. BMC Health Serv Res 5: 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Melis RJ, van Eijken MI, Teerenstra S, van Achterberg T, Parker SG, et al. (2008) A randomized study of a multidisciplinary program to intervene on geriatric syndromes in vulnerable older people who live at home (Dutch EASYcare Study). J Gerontol 63A: 283–290. [DOI] [PubMed] [Google Scholar]
- 149. Messier SP, Royer TD, Craven TE, O'Toole ML, Burns R, et al. (2000) Long-term exercise and its effect on balance in older, osteoarthritic adults: Results from the Fitness, Arthritis, and Senior Trial (FAST). J Am Geriatr Soc 48: 131–138. [DOI] [PubMed] [Google Scholar]
- 150. Miller DK, Lewis LM, Nork MJ (1996) Controlled trial of a geriatric case-finding and liaison service in an emergency department. J Am Geriatr Soc 44: 513–520. [DOI] [PubMed] [Google Scholar]
- 151. Moore AA, Siu AL, Partridge JM, Hays RD, Adams J (1997) A randomized trial of office-based screening for common problems in older persons. Am J Med 102: 371–378. [DOI] [PubMed] [Google Scholar]
- 152. Newcomer R, Maravilla V, Faculjak P, Graves M (2004) Outcomes of preventive case management among high-risk elderly in three medical groups. Eval Health Prof 27: 323–348. [DOI] [PubMed] [Google Scholar]
- 153. Oktay JS, Volland PJ (1990) Post-hospital support program for the frail elderly and their caregivers: A quasi-experimental evaluation. Am J Public Health 80: 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Parsons J, Rouse P, Robinson EM, Sheridan N, Connolly MJ (2012) Goal setting as a feature of homecare services for older people: Does it make a difference? Age Ageing 41: 24–29. [DOI] [PubMed] [Google Scholar]
- 155. Peeters GM, de Vries OJ, Elders PJ, Pluijm SM, Bouter LM, et al. (2007) Prevention of fall incidents in patients with a high risk of falling: Design of a randomised controlled trial with an economic evaluation of the effect of multidisciplinary transmural care. BMC Geriatr 7: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Penninx BW, Rejeski WJ, Pandya J, Miller ME, Di Bari M, et al. (2002) Exercise and depressive symptoms: a comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. J Gerontol B Psychol Sci Soc Sci 57: 124–132. [DOI] [PubMed] [Google Scholar]
- 157. Poulsen T, Elkjaer E, Vass M, Hendriksen C, Avlund K (2007) Promoting physical activity in older adults by education of home visitors. Eur J Ageing 4: 115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Poulstrup A, Jeune B (2000) Prevention of fall injuries requiring hospital treatment among community-dwelling elderly. Eur J Public Health 10: 45–50. [Google Scholar]
- 159. Rejeski WJ, Brawley LR, Ettinger W, Morgan T, Thompson C (1997) Compliance to exercise therapy in older participants with knee osteoarthritis: Implications for treating disability. Med Sci Sports Exerc 29: 977–985. [DOI] [PubMed] [Google Scholar]
- 160. Robertson MC, Gardner MM, Devlin N, McGee R, Campbell AJ (2001) Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 2: Controlled trial in multiple centres. BMJ 322: 701–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Robichaud L, Hebert R, Roy P, Roy C (2000) A preventive program for community-dwelling elderly at risk of functional decline: A pilot study. Arch Gerontol Geriatr 30: 73–84. [DOI] [PubMed] [Google Scholar]
- 162. Rosie J, Taylor D (2007) Sit-to-stand as home exercise for mobility-limited adults over 80 years of age—GrandStand System may keep you standing? Age Ageing 36: 555–562. [DOI] [PubMed] [Google Scholar]
- 163. Salminen M, Vahlberg T, Sihvonen S, Piirtola M, Isoaho R, et al. (2008) Effects of risk-based multifactorial fall prevention program on maximal isometric muscle strength in community-dwelling aged: A randomized controlled trial. Aging Clin Exp Res 20: 487–493. [DOI] [PubMed] [Google Scholar]
- 164. Salminen M, Vahlberg T, Sihvonen S, Sjösten N, Piirtola M, et al. (2009) Effects of risk-based multifactorial fall prevention on postural balance in the community-dwelling aged: A randomized controlled trial. Arch Gerontol Geriatr 48: 22–27. [DOI] [PubMed] [Google Scholar]
- 165. Salminen MJ, Vahlberg TJ, Salonoja MT, Aarnio PTT, Kivela SL (2009) Effect of a risk-based multifactorial fall prevention program on the incidence of falls. J Am Geriatr Soc 57: 612–619. [DOI] [PubMed] [Google Scholar]
- 166. Schraeder C, Shelton P, Sager M (2001) The effects of a collaborative model of primary care on the mortality and hospital use of community-dwelling older adults. J Gerontol A Biol Sci Med Sci 56A: M106–M112. [DOI] [PubMed] [Google Scholar]
- 167. Scogin F, Morthland M, Kaufman A, Burgio L, Chaplin W, et al. (2007) Improving quality of life in diverse rural older adults: A randomized trial of a psychological treatment. Psychol Aging 22: 657–665. [DOI] [PubMed] [Google Scholar]
- 168. Sevick MA, Bradham DD, Muender M, Chen GJ, Enarson C, et al. (2000) Cost-effectiveness of aerobic and resistance exercise in seniors with knee osteoarthritis. Med Sci Sports Exerc 32: 1534–1540. [DOI] [PubMed] [Google Scholar]
- 169. Silverman M, Musa D, Martin DC, Lave JR, Adams J, et al. (1995) Evaluation of outpatient geriatric assessment: A randomized multi-site trial. J Am Geriatr Soc 43: 733–740. [DOI] [PubMed] [Google Scholar]
- 170. Sjosten NM, Salonoja M, Piirtola M, Vahlberg TJ, Isoaho R, et al. (2007) A multifactorial fall prevention programme in the community-dwelling aged: Predictors of adherence. Eur J Public Health 17: 464–470. [DOI] [PubMed] [Google Scholar]
- 171. Sjosten NM, Salonoja M, Piirtola M, Vahlberg T, Isoaho R, et al. (2007) A multifactorial fall prevention programme in home-dwelling elderly people: A randomized-controlled trial. Public Health 121: 308–318. [DOI] [PubMed] [Google Scholar]
- 172. Sjosten NM, Vahlberg TJ, Kivela SL (2008) The effects of multifactorial fall prevention on depressive symptoms among the aged at increased risk of falling. Int J Geriatr Psychiatry 23: 504–510. [DOI] [PubMed] [Google Scholar]
- 173. Spice CL, Morotti W, George S, Dent TH, Rose J, et al. (2009) The Winchester falls project: A randomised controlled trial of secondary prevention of falls in older people. Age Ageing 38. [DOI] [PubMed] [Google Scholar]
- 174. Steinberg M, Cartwright C, Peel N, Williams G (2000) A sustainable programme to prevent falls and near falls in community dwelling older people: Results of a randomised trial. J Epidemiol Community Health 54: 227–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Stewart S, Harvey I, Poland F, Lloyd-Smith W, Mugford M, et al. (2005) Are occupational therapists more effectvie than social workers when assessing frail older people? Results of CAMELOT, a randomised controlled trial. Age Ageing 34: 41–46. [DOI] [PubMed] [Google Scholar]
- 176. Stuck AE, Kharicha K, Dapp U, Anders J, von Renteln-Kruse W, et al. (2007) The PRO-AGE study: An international randomised controlled study of health risk appraisal for older persons based in general practice. BMC Med Res Methodol 7: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Theander E, Edberg AK (2005) Preventive home visits to older people in Southern Sweden. Scand J Prim Health Care 33: 392–400. [DOI] [PubMed] [Google Scholar]
- 178. Toseland RW, O'Donnell JC, Engelhardt JB, Hendler J, Thomley J, et al. (1996) Outpatient geriatric evaluation and management: Results of a randomized trial. Med Care 34: 624–640. [DOI] [PubMed] [Google Scholar]
- 179. Townsend J, Piper M, Frank AO, Dyer S, North WR, et al. (1988) Reduction in hospital readmission stay of elderly patients by a community based hospital discharge scheme: A randomised controlled trial. BMJ 297: 544–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Tulloch AJ, Moore V (1979) A randomized controlled trial of geriatric screening and surveillance in general practice. J R Coll Gen Pract 29: 733–742. [PMC free article] [PubMed] [Google Scholar]
- 181. Vaapio S, Salminen M, Vahlberg T, Sjösten N, Isoaho R, et al. (2007) Effects of risk-based multifactorial fall prevention on health-related quality of life among the community-dwelling aged: A randomized controlled trial. Health Qual Life Outcomes 5: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Vass M, Avlund K, Lauridsen J, Hendriksen C (2005) Feasible model for prevention of functional decline in older people: Municipality-randomized, controlled trial. J Am Geriatr Soc 53: 568. [DOI] [PubMed] [Google Scholar]
- 183. von Renteln KW, Anders J, Dapp U, Meier-Baumgartner HP (2003) Preventative home visits by a specially trained nurse for 60-year olds and elderly in Hamburg. Z Gerontol Geriatr 36: 378–391. [DOI] [PubMed] [Google Scholar]
- 184. Wagner EH, LaCroix AZ, Grothaus L, Leveille SG, Hecht JA, et al. (1994) Preventing disability and falls in older adults: A population-based randomized trial. Am J Public Health 84: 1800–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Wallace JI, Buchner DM, Grothaus L, Leveille S, Tyll L, et al. (1998) Implementation and effectiveness of a community-based health promotion program for older adults. J Gerontol A Biol Sci Med Sci 53: M301–M306. [DOI] [PubMed] [Google Scholar]
- 186. Wasson JH, Stukel TA, Weiss JE (1999) A randomized trial of the use of patient self-assessment data to improve community practices. Eff Clin Pract 2: 1–10. [PubMed] [Google Scholar]
- 187. Whitehead C, Wundke R, Crotty M, Finucane P (2003) Evidence-based clinical practice in falls prevention: A randomised controlled trial of a falls prevention service. Aust Health Rev 26: 88–97. [DOI] [PubMed] [Google Scholar]
- 188. Williams EI, Greenwell J, Groom LM (1992) The care of people over 75 years old after discharge from hospital: An evaluation of timetabled visiting by Health Visitor Assistants. J Public Health Med 14: 138–144. [PubMed] [Google Scholar]
- 189. Williams K, Mustian K, Kovacs C (2002) A home-based intervention to improve balance, gait and self-confidence in older adults. Act Adapt Aging 27: 1–16. [Google Scholar]
- 190. Wolf B, Feys H, De Weerdt W, van der Meer J, Aufdemkampe G (2001) Effect of a physical therapeutic intervention for balance problems in the elderly: A single-blind, randomized controlled multicentre trial. Clin Rehabil 15: 624–636. [DOI] [PubMed] [Google Scholar]
- 191. Yates SM, Dunnagan TA (2001) Evaluating the effectiveness of a home-based fall risk reduction program for rural community-dwelling older adults. J Gerontol A Biol Sci Med Sci 56A: M226–M230. [DOI] [PubMed] [Google Scholar]
- 192. Zimmer JG, Groth-Juncker A, McKusker J (1985) A randomized controlled study of a home health care team. Am J Public Health 75: 134–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Cutchin MP, Coppola S, Talley V, Svihula J, Catellier D, et al. (2009) Feasibility and effects of preventive home visits for at-risk older people: Design of a randomized controlled trial. BMC Geriatr 9: 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Ferrer A, Badia T, Formiga F, Gil A, Padrós G, et al. (2010) A randomized clinical trial of falls and malnutrition prevention in community-dwelling elders aged 85 years old. The OCTABAIX study. [Ensayo clinico aleatorizdo de prevencion de caidas y malnutricion en personas de 85 anos en la comunidad]. Revista Espanola de Geriatria y Gerontologia 45: 79–85. [DOI] [PubMed] [Google Scholar]
- 195. Fleischer S, Roling G, Beutner K, Hanns S, Behrens J, et al. (2008) Growing old at home–A randomized controlled trial to investigate the effectiveness and cost-effectiveness of preventive home visits to reduce nursing home admissions: Study protocol. BMC Public Health 8: 185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Hinrichs T, Bucchi C, Brach M, Wilm S, Endres HG, et al. (2009) Feasibility of a multidimensional home-based exercise programme for the elderly with structured support given by the general practitioner's surgery: Study protocol of a single arm trial preparing an RCT. BMC Geriatr 9: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Jingna Y, Liqun C, Shoumei J (2012) Influence of community nurse-led multidisciplinary team home visiting services on psychological state of old age of home elderly. Chinese Nursing Research 26: 975–978. [Google Scholar]
- 198. Jitapunkul S (1998) A randomised controlled trial of regular surveillance in Thai elderly using a simple questionnaire administered by non-professional personnel. J Med Assoc Thai 81: 352–356. [PubMed] [Google Scholar]
- 199. Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ (1993) Comprehensive geriatric assessment: A meta-analysis of controlled trials. Lancet 342: 1032–1036. [DOI] [PubMed] [Google Scholar]
- 200. Bouman A, van Rossum E, Nelemans P, Kempen GIJM, Knipschild P (2008) Effects of intensive home visiting programs for older people with poor health status: A systematic review. BMC Health Serv Res 8: 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Turner SAG, Lyons RA, Weightman AL, Mann MK, et al. (2011) Modification of the home environment for the reduction of injuries. Cochrane Database Syst Rev 2: CD003600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Elkan R, Kendrick D (2004) What is the effectiveness of home visiting or homebased support for older people? Copenhagen: WHO Regional Office for Europe (Accessed 21 August 2013). [Google Scholar]
- 203. Altman DG (2013) Transparent reporting of trials is essential. Am J Gastroenterol 108: 1231–1235. [DOI] [PubMed] [Google Scholar]
- 204. Mayo-Wilson E, Grant S, Hopewell S, Macdonald G, Moher D, et al. (2013) Developing a reporting guideline for social and psychological intervention trials. Trials 14: 242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Grant SP, Mayo-Wilson E, Melendez-Torres GJ, Montgomery P (2013) Reporting quality of social and psychological intervention trials: a systematic review of reporting guidelines and trial publications. PLoS One 8: e65442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Underhill K, Operario D, Montgomery P (2007) Reporting deficiencies in trials of abstinence-only programmes for HIV prevention. AIDS 21: 266–267. [DOI] [PubMed] [Google Scholar]
- 207. Mayo-Wilson E (2007) Reporting implementation in randomized trials: proposed additions to the consolidated standards of reporting trials statement. Am J Public Health 97: 630–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Schulz KF, Altman DG, Moher D (2010) for the CONSORT Group (2010) CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ 340: 698–702. [DOI] [PubMed] [Google Scholar]
- 209. Hart B, Lundh A, Bero L (2012) Effect of reporting bias on meta-analyses of drug trials: Reanalysis of meta-analyses. BMJ 344: d7202. [DOI] [PubMed] [Google Scholar]
- 210. Montgomery P, Underhill K, Operario D, Gardner F, Mayo-Wilson E (2013) The Oxford Implementation Index: A new tool for incorporating implementation data into systematic reviews and meta-analyses. J Clin Epidemiol 66: 874–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Eldridge S, Spencer A, Cryer C, Parsons S, Underwood M, et al. (2005) Why modelling a complex intervention is an important precursor to trial design: Lessons from studying an intervention to reduce falls-related injuries in older people. J Health Serv Res Policy 10: 133–142. [DOI] [PubMed] [Google Scholar]
- 212. Clark J (2001) Preventive home visits to elderly people. BMJ 323: 708. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Chart.
(TIFF)
Risk of bias.
(TIFF)
Main outcomes and tests for reporting bias.
(TIFF)
Meta-regression analyses.
(TIFF)
Results for each follow-up interval, longest follow-up, and subgroup analyses.
(PDF)
Extended table of included studies.
(PDF)
Summary of findings table.
(DOCX)
Table of included studies.
(DOCX)
Table of excluded studies.
(DOCX)
Complete search strategies.
(DOCX)
RevMan 5.2 file.
(RM5)
(DOC)