Abstract
Objectives/Hypothesis
To determine the incidence and risk factors of pharyngocutaneous fistula formation in patients undergoing either primary or salvage laryngectomies and evaluate the role of barium esophagram in these patients.
Study Design
Retrospective cohort study.
Methods
Medical records of 259 patients who underwent total laryngectomy between 2003 and 2009 at our institution were reviewed. Risk factors for fistula formation were analyzed, including primary treatment modality, comorbidities, and operative details, which included use of a free flap for closure, concurrent neck dissections, margin status, and preoperative tracheostomy. The length of time until leak, postoperative swallow study results, and fistula management strategies were also assessed.
Results
Fifty-five patients developed a pharyngocutaneous fistula (overall incidence, 21%) in a median time of 12 days (range, 4–105 days). Twenty of these patients underwent laryngectomy as their initial treatment modality, and 35 had failed previous radiotherapy. Fistula formation was significantly higher in salvage surgery patients (P = .03), particularly those with hypothyroidism (P < .0002). A barium swallow performed at approximately 1 week after laryngectomy demonstrated a sensitivity of 26% with a specificity of 94%. Sixty-two percent of the fistulas healed with conservative measures only.
Conclusions
Our data confirmed that previous radiotherapy and hypothyroidism, particularly in salvage laryngectomy patients, are important significant predictors of postoperative pharyngocutaneous fistula. The use of a postoperative barium swallow in these patients may be useful but was not found to be highly sensitive in predicting who will develop a clinically evident leak and should be used with caution.
Keywords: Laryngectomy, laryngeal cancer, pharyngeal fistula, barium swallow, head and neck squamous cell carcinoma, postoperative complications, free tissue transfer
INTRODUCTION
Pharyngocutaneous fistula (PCF) after total laryngectomy continues to be one of the most common and difficult to manage complications of laryngeal surgery. Development of a PCF is the leading major cause of increased morbidity, delay in adjuvant treatment, prolonged hospital stay, and increased treatment costs in these patients.1,2 The reported incidence of postlaryngectomy fistula is extremely variable and ranges from 5% to 65%.3,4
Numerous studies have identified different variables associated with a statistically significant increased risk of PCF development. These variables include previous radiotherapy,2,5–10 extension of the laryngectomy defect to involve the pharynx,11,12 postoperative hemoglobin lower than 12.5 g/dL,13 chronic congestive heart failure,13 concurrent neck dissection,7,11 positive margins,2,5,14 gastroesophageal reflux disease,15 tumor size,10,16,17 suture material,16 hypoalbuminemia,8 and tumor recurrence.17 Currently, however, there is no consensus on which factors are most significant.2,14 Furthermore, medical management of laryngeal cancer has evolved with the addition of chemotherapy and molecularly targeted agents to radiotherapy, and it is unclear whether this has had an impact on the wound complication rates. Although it is understood that early postoperative detection of fistulae enables early intervention, the optimal method of identifying contained salivary leaks and their clinical significance have not been well studied. To this end, we evaluated the incidence, etiology, and possible risk factors of PCF formation in patients undergoing both primary and salvage laryngectomies and evaluated the role of barium esophagram in these patients at our institution.
MATERIALS AND METHODS
Patients
The records of 259 patients who underwent total laryngectomy between 2003 and 2009 at the University of Alabama at Birmingham were reviewed. Data were collected, including patient age and sex, comorbidities (specifically history of diabetes mellitus and/or hypothyroidism), tumor stage and site, preoperative tracheostomy, prior partial laryngectomy, preoperative radiation, primary closure versus free-flap closure, barium swallow findings, concurrent neck dissection, surgical margin status, cancer recurrence, and development of a PCF. Further details specific to the development of a PCF were recorded for that subset of patients including length of time to fistula, mode of closure, time to closure, and recurrence of fistula.
Median age was 60 years (range, 32–87). There were 49 females (18.9%) and 210 males (81.1%); 46 (17.8%) were hypothyroid, 27 (10.4%) had diabetes mellitus, 82 (31.4%) had a preoperative tracheostomy, 146 (56.4%) had experienced radiation failure, and 163 (62.9%) were closed with a free flap. Forty-nine patients (18.9%) had a failed previous attempt at partial laryngectomy. Two hundred thirty-two patients (89.6%) had advanced stage (III or IV) squamous cell carcinoma, five had chondroradionecrosis of the larynx, three with invasive thyroid carcinoma, and one melanoma of the larynx (Table I).
TABLE I.
Patient Characteristics.
| Characteristic | No. | % |
|---|---|---|
| Sex | ||
| Male | 210 | 81 |
| Female | 49 | 19 |
| Tumor location | ||
| Supraglottis | 72 | 27 |
| Glottis | 113 | 44 |
| Subglottis | 2 | 0.01 |
| Hypopharynx | 57 | 22 |
| Previous radiation therapy | 146 | 56 |
| Preoperative tracheostomy | 82 | 31 |
| Defect closure | ||
| Primary | 96 | 37 |
| Vascularized free tissue | 163 | 63 |
Surgical Technique
Surgery consisted of a standard total laryngectomy in 170 patients (65.6%), laryngopharyngectomy in 70 (27%), and partial/total glossectomy with laryngopharyngectomy in 19 (7.3%). One hundred eighty-eight patients (72.6%) underwent concurrent neck dissections. Ninety-six patients (37%) underwent a two-layer, T-shaped primary closure with a running Connell stitch and interrupted Lembert sutures. The remaining 163 (63%) had closure facilitated by free vascularized tissue or a pedicled flap. The use of a flap was determined by inadequate remaining pharyngeal mucosa and/or in the setting of previous radiation. These included a combination of radial forearm (n = 129), anterolateral thigh (n = 8), rectus (n = 16), jejunal (n = 9), and pectoralis major flaps (n = 1). A watertight seal was confirmed using povidoneiodine–diluted saline placed through the mouth. If gross leakage was noted, it was addressed and corrected at this time with additional sutures. Skin was closed in two layers with absorbable suture over four suction drains.
Statistical Analysis
The prognostic value of age, sex, hypothyroidism, diabetes mellitus, concurrent neck dissection, preoperative tracheostomy, positive surgical margins, cancer recurrence, previous attempt at partial laryngectomy, extension of laryngectomy defect to include pharyngeal mucosa, and use of vascularized tissue for closure was studied in relation to fistula occurrence. All variables were used in the different models as categoric variables. The age variable was coded into two groups (≤60 and >60 years). The sensitivity, specificity, and positive and negative predictive values of a barium esophagram in identifying patients with PCF were calculated.
The relationship between the presence of a fistula and the prognostic variables was analyzed by using a two-tailed Fisher exact test from a 2 × 2 contingency table. Those with a P value less than .05 were considered clinically relevant. The analysis was performed using GraphPad Software (GraphPad, San Diego, CA).
RESULTS
A total of 259 patients underwent laryngectomy during the study period. The study population underwent 113 (43.6%) primary laryngectomies and 146 (56.4%) salvage laryngectomies. Fifty-five patients (21.2%) developed a clinically evident PCF within a median time of 12 days (range, 4–105 days) (Fig. 1). The overall fistula incidence in primary laryngectomy patients was 17.9%, whereas in salvage patients, the incidence was slightly higher at 24% (P = .03). Thirty-three fistulas (62%) healed via conservative measures only. The majority (70%) of the primary laryngectomy patients with fistulas healed via conservative measures in an average of 29 days, whereas only 55% of the salvage laryngectomy patients healed without surgical intervention in an average of 54 days. Occasionally, continuous suction dressings were needed for complete closure in these patients. Surgical closure involved local flaps in two patients, regional flaps in 12 patients (10 pectoralis major and 2 deltopectoral), and free flaps in eight patients (6 radial forearm and 2 anterolateral thigh). Thirteen patients, one primary and 12 salvage, had a recurrent fistula and required two or more surgical procedures for closure.
Fig. 1.
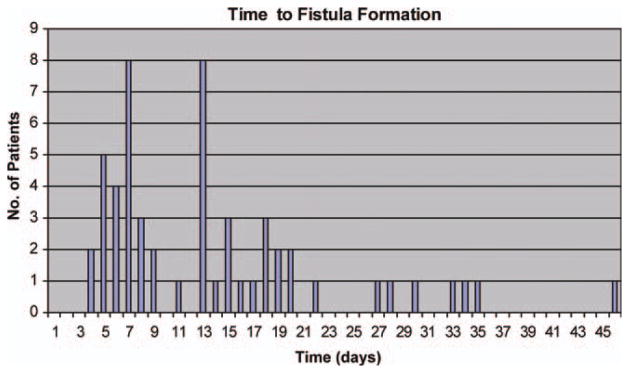
Length of time until fistula. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Two variables had a significant correlation with increased risk of fistula formation. Hypothyroidism, particularly in the setting of a salvage laryngectomy (P < .0002), and previous radiation treatment (P = .03) were found to be significantly associated with fistula formation. Previous chemotherapy, however, did not have a significant effect (P = .4). Concurrent neck dissections in all patients and a preoperative tracheostomy in salvage patients were associated with increased risk for fistulae but did not reach statistical significance (P = .06 for both). The diagnosis of diabetes mellitus, closure utilizing vascularized free tissue (all of which survived), preoperative tracheostomy, previous partial laryngectomy, positive surgical margins, cancer recurrence, male sex, age >60 years, and/or extension of laryngectomy defect to include adjacent subsites did not significantly influence development of PCFs (Table II).
TABLE II.
Relationship Between Clinical Variables and Fistula Occurrence.
| Variable | Incidence of Fistula, No. (%) | P Value |
|---|---|---|
| Age >60 years | 28/135 (21) | .88 |
| Primary | 10/59 (17) | .44 |
| Salvage | 17/76 (22) | .57 |
| Male | 44/200 (22) | .85 |
| Primary | 11/85 (13) | .19 |
| Salvage | 33/115 (29) | .62 |
| Diabetes mellitus | 5/27 (19) | .81 |
| Primary | 2/10 (20) | .65 |
| Salvage | 3/17 (18) | .76 |
| Hypothyroidism | 21/46 (46) | <.0001 |
| Primary | 4/14 (29) | .22 |
| Salvage | 17/32 (53) | .0002 |
| Neck dissection | 34/188 (18) | .06 |
| Primary | 14/105 (13) | .09 |
| Salvage | 20/83 (24) | .57 |
| Free-flap closure | 38/163 (23) | .35 |
| Primary | 5/51 (10) | .12 |
| Salvage | 33/112 (29) | .18 |
| Preoperative tracheostomy | 22/82 (27) | .14 |
| Primary | 5/34 (15) | 1.0 |
| Salvage | 17/48 (35) | .06 |
| Previous partial laryngectomy | 3/29 (10) | .15 |
| Primary | 1/5 (20) | .56 |
| Salvage | 2/24 (8) | .07 |
| Previous radiation | 38/146 (26) | .03 |
| Positive margins | 11/43 (26) | .42 |
| Primary | 2/19 (10) | .73 |
| Salvage | 9/24 (37) | .20 |
| Pharyngeal mucosa involvement | 19/89 (21) | 1.0 |
| Primary | 4/38 (10) | .57 |
| Salvage | 15/51 (29) | .43 |
Two hundred and five patients (79.2%) underwent postoperative radiologic evaluation with a gastrograffin esophagram (followed by a barium esophagram if no leak was seen) between 5 and 12 days (mean, 6 days) after surgery to assess for PCF. As noted, 55 patients developed clinically evident fistulas. The incidence of clinically evident fistulas in those tested was 19%. Of the 29 patients who developed a clinically evident fistula following a negative barium esophagram, 20 (69%) healed without surgical intervention. A similar proportion of patients, 10 of 15 (67%), with a positive barium esophagram healed with conservative measures only.
The sensitivity of the barium esophagram at our institution, when considering all patients combined, was found to be 26%, with a specificity of 94%. The sensitivity of the study in primary laryngectomy patients only was much higher at 55%, with a specificity of 97%. In contrast, the sensitivity in salvage patients was 14%, with a specificity of 91%.
DISCUSSION
This study identified two significant risk factors associated with postlaryngectomy PCF formation, hypothyroidism, and previous radiation therapy. It also served to further classify them according to whether they affected salvage patients, primary surgery patients, or both. To date, this is one of the largest study populations of its kind; this study showed fistula rates in both primary (17.9%) and salvage (24%) patients to be well within the acceptable and expected ranges. The role of a barium esophagram in the evaluation of laryngectomy patients in the early postoperative period remains controversial, but our study helped to clarify its utility by reporting sensitivities and specificities in both primary surgery and salvage surgery patients.
PCFs continue to cause significant morbidity, including salivary leakage, prolonged hospitalization, swallowing difficulty, delayed initiation of adjuvant therapy, and potential fatal complications such as carotid artery rupture.17 It is important to understand the risk factors associated with increased likelihood of PCF formation so that we can be better prepared to provide aggressive perioperative management. This study identified only two significant risk factors out of the numerous variables analyzed. Some of the other well-documented risk factors, such as margin status, pharyngeal mucosa involvement, concurrent neck dissection, and preoperative tracheostomy, were not found to be statistically significant.
Preoperative radiotherapy is a well-documented risk factor for postsurgical complications, including fistula formation.2,5–9,18 Our results were in agreement with the current literature findings. This most likely can be attributed to the diminished healing capacity of the irradiated tissues secondary to obliterative endarteritis, fibrosis, and overall decreased vascularity of the tissues.14,19,20 Several studies have tried to decrease the rate of fistula formation by using vascularized free tissue grafts but thus far have not made a significant impact.17,18
Hypothyroidism is known to increase wound complications and is common in patients with head and neck cancer.9 Our study demonstrated a significantly increased risk of fistula formation in salvage laryngectomy patients with hypothyroidism. It should be noted that the fistula rate was higher in the surgical salvage group, and hypothyroidism was more prevalent in this group; therefore hypothyroidism may not, in itself, be causative for fistulas. A multivariate analysis would more clearly delineate this possibility but was not feasible in this study. The diagnosis of hypothyroidism should not be made after a clinically evident PCF has formed. This can, and should, be an avoidable risk factor if appropriate measures are taken early during treatment. Even patients not known to have hypothyroidism before surgery should have preoperative thyroid function studies performed in the setting of previous radiation. This has now become part of our current practice.
Barium esophagram in the right population can be helpful in the management plan but cannot be relied upon to predict who will develop clinical fistulas and could potentially prolong patient hospital stays unnecessarily. At our institution, barium swallows were found to be highly specific (94%) but not highly sensitive (26%) in predicting which patients would develop a clinically evident PCF. The argument could be made that this is because some of those patients with small leaks seen on preliminary exams are kept without oral nutrition for longer periods of time, given antibiotics, and have drains left in place longer, thereby effectively preventing fistula formation. This is in contrast to a previous study by Krouse and Metson, which found barium swallows to be predictive of, but not preventive of, salivary fistulas.10 It is safe to conclude that having patients at high risk for fistula formation undergo imaging before initiating oral intake is beneficial and may actually lessen potential long-term morbidity.
Fistula management ranges from conservative observation to vascularized free tissue transfer. This study demonstrated closure of 62% of fistulas with simple observation, occasionally utilizing the assistance of continuous suction drainage. This finding is consistent with most current findings reported in the literature.2,13 As expected, a larger percentage of the primary laryngectomy patients healed with conservative management and in less time than the salvage group. Sixty-five percent of the fistula patients requiring surgical management had experienced chemoradiation failure, and 75% of them required a microvascular flap at their initial surgery for closure, which shows the aggressive nature of their disease and poor tissue quality. This information can be useful in predicting which fistula patients will benefit from early surgical closure to speed the recovery process.
CONCLUSION
In conclusion, this study with a large patient population serves to clarify significant risk factors for PCF formation in both primary and salvage laryngectomy patients. It also further elucidates the sensitivity and specificity of the barium esophagram in the evaluation and management of what continues to be a challenging problem for the head and neck surgeon.
Footnotes
Poster presentation at the Triological Society Combined Sections Meeting, Miami Beach, Florida, U.S.A., January 26–28, 2012.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
BIBLIOGRAPHY
- 1.Qureshi SS, Chaturvedi P, Pai PS, et al. A prospective study of pharyngocutaneous fistulas following total laryngectomy. J Cancer Res Ther. 2005;1:51–56. doi: 10.4103/0973-1482.16092. [DOI] [PubMed] [Google Scholar]
- 2.Saki N, Nikakhlagh S, Kazemi M. Pharyngocutaneous fistula after laryngectomy: incidence, predisposing factors, and outcome. Arch Iran Med. 2008;11:314–317. [PubMed] [Google Scholar]
- 3.Sassler AM, Esclamado RM, Wolf GT. Surgery after organ preservation therapy. Analysis of wound complications. Arch Otolaryngol Head Neck Surg. 1995;121:162–165. doi: 10.1001/archotol.1995.01890020024006. [DOI] [PubMed] [Google Scholar]
- 4.Weber RS, Berkey BA, Forastiere A, et al. Outcome of salvage total laryngectomy following organ preservation therapy: the Radiation Therapy Oncology Group trial 91-11. Arch Otolaryngol Head Neck Surg. 2003;129:44–49. doi: 10.1001/archotol.129.1.44. [DOI] [PubMed] [Google Scholar]
- 5.Lundgren J, Olofsson J. Pharyngocutaneous fistulae following total laryngectomy. Clin Otolaryngol Allied Sci. 1979;4:13–23. doi: 10.1111/j.1365-2273.1979.tb01748.x. [DOI] [PubMed] [Google Scholar]
- 6.Hier M, Black MJ, Lafond G. Pharyngocutaneous fistulas after total laryngectomy: incidence, etiology and outcome analysis. J Otolaryngol. 1993;22:164–166. [PubMed] [Google Scholar]
- 7.Galli J, De Corso E, Volante M, Almadori G, Paludetti G. Postlaryngectomy pharyngocutaneous fistula: incidence, predisposing factors, and therapy. Otolaryngol Head Neck Surg. 2005;133:689–694. doi: 10.1016/j.otohns.2005.07.025. [DOI] [PubMed] [Google Scholar]
- 8.Tsou YA, Hua CH, Lin MH, Tseng HC, Tsai MH, Shaha A. Comparison of pharyngocutaneous fistula between patients followed by primary laryngopharyngectomy and salvage laryngopharyngectomy for advanced hypopharyngeal cancer. Head Neck. 32:1494–1500. doi: 10.1002/hed.21352. [DOI] [PubMed] [Google Scholar]
- 9.Hanasono MM, Lin D, Wax MK, Rosenthal EL. Closure of laryngectomy defects in the age of chemoradiation therapy. Head Neck. 2012;34:580–588. doi: 10.1002/hed.21712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krouse JH, Metson R. Barium swallow is a predictor of salivary fistula following laryngectomy. Otolaryngol Head Neck Surg. 1992;106:254–257. doi: 10.1177/019459989210600310. [DOI] [PubMed] [Google Scholar]
- 11.Virtaniemi JA, Kumpulainen EJ, Hirvikoski PP, Johansson RT, Kosma VM. The incidence and etiology of postlaryngectomy pharyngocutaneous fistulae. Head Neck. 2001;23:29–33. [PubMed] [Google Scholar]
- 12.Palomar-Asenjo V, Sarroca Capell E, Tobias Gomez S, Perez Hernandez I, Palomar-Garcia V. Pharyngocutaneous fistula following total laryngectomy. A case-control study of risk factors implicated in its onset [in Spanish] Acta Otorrinolaringol Esp. 2008;59:480–484. [PubMed] [Google Scholar]
- 13.Redaelli de Zinis LO, Ferrari L, Tomenzoli D, Premoli G, Parrinello G, Nicolai P. Postlaryngectomy pharyngocutaneous fistula: incidence, predisposing factors, and therapy. Head Neck. 1999;21:131–138. doi: 10.1002/(sici)1097-0347(199903)21:2<131::aid-hed6>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 14.Markou KD, Vlachtsis KC, Nikolaou AC, Petridis DG, Kouloulas AI, Daniilidis IC. Incidence and predisposing factors of pharyngocutaneous fistula formation after total laryngectomy. Is there a relationship with tumor recurrence? Eur Arch Otorhinolaryngol. 2004;261:61–67. doi: 10.1007/s00405-003-0643-6. [DOI] [PubMed] [Google Scholar]
- 15.Seikaly H, Park P. Gastroesophageal reflux prophylaxis decreases the incidence of pharyngocutaneous fistula after total laryngectomy. Laryngoscope. 1995;105:1220–1222. doi: 10.1288/00005537-199511000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Soylu L, Kiroglu M, Aydogan B, et al. Pharyngocutaneous fistula following laryngectomy. Head Neck. 1998;20:22–25. doi: 10.1002/(sici)1097-0347(199801)20:1<22::aid-hed4>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 17.Andrades P, Pehler SF, Baranano CF, Magnuson JS, Carroll WR, Rosenthal EL. Fistula analysis after radial forearm free flap reconstruction of hypopharyngeal defects. Laryngoscope. 2008;118:1157–1163. doi: 10.1097/MLG.0b013e31816f695a. [DOI] [PubMed] [Google Scholar]
- 18.Fung K, Teknos TN, Vandenberg CD, et al. Prevention of wound complications following salvage laryngectomy using free vascularized tissue. Head Neck. 2007;29:425–430. doi: 10.1002/hed.20492. [DOI] [PubMed] [Google Scholar]
- 19.Moses BL, Eisele DW, Jones B. Radiologic assessment of the early postoperative total-laryngectomy patient. Laryngoscope. 1993;103:1157–1160. doi: 10.1288/00005537-199310000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Teknos TN, Myers LL. Surgical reconstruction after chemotherapy or radiation. Problems and solutions. Hematol Oncol Clin North Am. 1999;13:679–687. doi: 10.1016/s0889-8588(05)70085-x. [DOI] [PubMed] [Google Scholar]


