Abstract
Background
Higher education has long made efforts to increase underrepresented minority participation in biomedical research and health fields. However, relatively few minority trainees complete advanced degrees or proceed to independent research careers, a loss referred to as the “leaky pipeline.” Minority trainees may take alternate pathways to climbing the academic ladder, exiting to pursue multiple disciplinary or community-serving roles.
Objective
The authors propose a model for understanding minority departures from the education pipeline as a basis for nurturing careers that support community goals for health.
Methods
Concepts of the traditional pipeline training model are compared with a model that aligns with CBPR principles and practices. The article describes an irrigation model that incorporates informal learning from academic and community knowledge bases to prepare trainees for CBPR and interdisciplinary research. Students serve as agents that foster individual, institutional and social change needed to address health problems while attending to root causes of disparities.
Conclusions
Viewing minority students as agents for community engagement allows institutions to reassess the role training can play in diversifying participation in higher education and research. An irrigation model supports development of an infrastructure that optimizes success at all post-secondary levels, and enhances CBPR capacity wherever trainees live, work, and learn. Linking formal education to informal learning in context of community-based participatory research experiences can also reduce community mistrust of research while nurturing productive research partnerships with communities to address health disparities.
Despite an increasingly diverse population, minorities continue to be underrepresented in the U.S. biomedical and research workforce.1 For over forty years, agencies such as the Association of American Medical Colleges and the National Institutes of Health (NIH) have invested significant resources in graduate, post-doctoral, professional, and junior faculty training programs to address this problem.1 As a National Academy of Science (NAS) committee observed, increasing the presence of underrepresented minorities in biomedical fields “broadens scientific inquiry and knowledge, has enhanced potential to solve population-specific health problems, and more fully exploits a valuable human resource.” 2
Although federal programs to boost minority representation have achieved some success, few trainees reach the desired endpoints of health professional or independently-funded researcher careers.1,3 The NAS committee characterized the education pipeline as “understandably leaky” because of the barriers to higher education faced by minority students, yet still defined success in terms of professional career outcomes—trainees who become health care providers, biotechnology employees, academics or science writers.2 Recommendations for improvement focused on measures such as streamlining transfers from community and minority-serving colleges and increasing access to minority faculty mentors.4,5,6
We argue for an expanded definition of success for minority education, in which departures from the pipeline are not simply seen as leaks to be patched, but as an irrigation system that supports productive academic-community partnerships and fosters minority engagement in science education. Minority trainees who exit the pipeline and return to their communities represent potential research partners and can play a key role as ambassadors for higher education and research.
We define community as the places minority students call “home,” including geographic locations and familial, social and professional networks. We incorporate the NIH definition of underrepresented minorities (African American, Hispanic American, Native American/Alaska Native, Hawaiian Native and natives of the Pacific Islands), while recognizing that diversity exists within and among these groups in how they identify and intersect with minority communities. However, these groups share a history of exclusion and reduced access to the societal resources that facilitate success during academic training and beyond.
The current pipeline model focuses on increasing diversity in graduate, professional and post-graduate education. The goal of an irrigation model is to provide all students with positive research experiences, in an interdisciplinary environment spanning minority communities and research institutions. Many minority trainees will exit and re-enter the pipeline over time, and may cross into non-biomedical fields or assume leadership roles in their communities. Regardless of level of college education or discipline, students represent social networks that can nurture community partnerships.4,5,6 If those partnerships are based in the principles of community-based participatory research (CBPR), they provide a vehicle for addressing community priorities. By applying CBPR principles of collaboration to minority training (Table 1), and linking training to participatory research initiatives, academic research centers invest in people who can foster sustainable partnerships with minority communities which can, in turn, promote interest in science and health careers. This approach offers another means to achieving the desired end of increasing diversity in science and research by reframing “losses” from the academic pipeline as potential assets for building community capacity.
Table 1.
CBPR principles applied to characteristics of the Pipeline vs. Irrigation models
| Application of CBPR principles* | Pipeline Model - Barriers | Irrigation System - Solutions | |
|---|---|---|---|
| Goal |
|
|
|
| Student preparedness |
|
|
|
| Student path - Measures of success |
|
|
|
| Directionality – Addressing power differentials |
|
|
|
CBPR principles described herein are from Israel et al.24 These principles were applied to specific rows in the table for simplicity and illustration, acknowledging that they may characterize several qualities of the Irrigation model
Factors contributing to the leaky pipeline
Inadequate preparation is a major limiting factor in efforts to increase the pool of qualified minority applicants for advanced education. Poverty, sub-par resources in minority-serving schools and poor mentorship contribute to losses of minority students at each level of education. For instance, Barr, et. al estimated that out of every 100 African American, Latino, or Native American premed freshmen at Stanford, more than half do not apply to medical school. While tutoring services for foundational classes such as chemistry are important, additional efforts in personal counseling and cultural support for minority students experiencing social isolation on predominantly white college campuses are also critical to assuring academic success.3,7,8
However, competing personal demands are also an important consideration. Attrition from health science pathways can be expected due to competition from other fields,2,8 particularly disciplines that require less time in school or are perceived to have more immediate or greater financial payoff than health and science careers. For example, a computer engineer with a Bachelor’s degree and less than five years experience can earn $60,500 annually while an epidemiologist has a similar average starting salary only after completing a graduate education.9,10 Similarly, many minority students entering college with the intention of pursuing doctoral or medical degrees (endpoints of the pipeline) may exit, permanently or temporarily, after completing technical, Associates, or Bachelors programs that qualify them for wage-earning jobs, so they can meet immediate family or financial obligations. They may move in and out of university to attend to life events, route through community colleges, or work off loans after completing each step on the educational trajectory.4,5,7
Creating roadblocks for trainees who seek education in segments, rather than moving continuously through the pipeline, exacerbates minority exclusion from academic and research systems. We often hear from our trainees that they need a break from the pressures of school to apply what they’ve learned to addressing community priorities, as well as to reassess personal priorities and refocus career goals. In our irrigation model, trainee “leaks” can be reframed and understood as infusing community networks and spheres of influence with skills and relationships from the academy. As such, these departures should be considered both junctures for re-entry and successful outlets that feed the managerial and skilled labor needs of communities.
Acknowledging mistrust
An additional barrier is the mistrust that many minority groups feel toward academic institutions, due to past research misconduct and discrimination in admissions processes. Research findings that come to a community’s attention only when they are publicized can strain relations with the institution. Community partners interested in long-term outcomes may see few rewards from grant-dependent academic research: researchers receive funding, publications and promotion, while communities continue to experience persistent health problems. Academic research paradigms may also be viewed as reinforcing colonial practices that contributed to power imbalances between communities and institutions, and between people of color and non-minority researchers.11,12 For example, funding mechanisms requiring principal investigators to have doctoral-level credentials typically place ultimate decision-making power with the academic partners over community-based research staff.
Addressing mistrust is as important as providing academic program support to minority students. As members of underrepresented groups, student experiences are shaped by perceptions of research institutions in their home communities as well as by interactions on the college campus. Research may be difficult to see as a positive career choice, especially in communities where participation in higher education remains an uncommon event. In addition, years spent in higher education systems can distance students from their home communities, geographically or culturally.4,5 The intentions of minority investigators trained in these environments can be questioned when working in communities who are wary of outside research: “the formidable nature of entering the field and establishing research relationships casts considerable doubt on the notion of minority scholars as ‘privileged’ insiders…women identified with me, not as a model success story but as a Chicana who was also working towards the completion of a degree.”13
Partnerships as the basis for change
Community-based participatory research offers a framework for overcoming mistrust of the research process,11 through sharing of power and resources among communities and academic partners, the development of local capacity, and interdisciplinary research aimed at actionable outcomes for community health.12,14 Translating research to benefit requires teams that can examine environmental and biological interactions and integrate these discoveries with knowledge of the social determinants of health. Collaborative community-university partnerships must also work with a focus on problem solving, as opposed to knowledge generation for its own sake.14
The irrigation model proposes linkages between minority training and projects utilizing CBPR methodology. The approach borrows from the Community Coalition Action Theory (CCAT) and Paulo Freire’s model of Informal Education, and argues for: (1) infrastructures that support minority success in either academic or community career paths; and (2) positive research experiences centered around training connected with community health priorities, as a means to reduce minority community mistrust of academic institutions and research. The CCAT emphasizes action-oriented coalitions that work to assess, analyze, and solve community problems, including academic-community partnerships focused on long-term health issues.15 Freire’s model of informal education16 describes how the self-empowerment of individuals, particularly those representing oppressed sectors of society, can happen through experiences with a diverse group or coalition. An iterative process of structured dialogue and reflection activities leads to a transformative stage of education, where exchange between participants (i.e., teachers, students, providers, community members) moves them toward critical consciousness.16 Reaching this stage of awareness allows them to address feelings of powerlessness and identify steps for personal and social action (e.g., envision success in a PhD program or develop a plan for coalition-building to address a community issue).
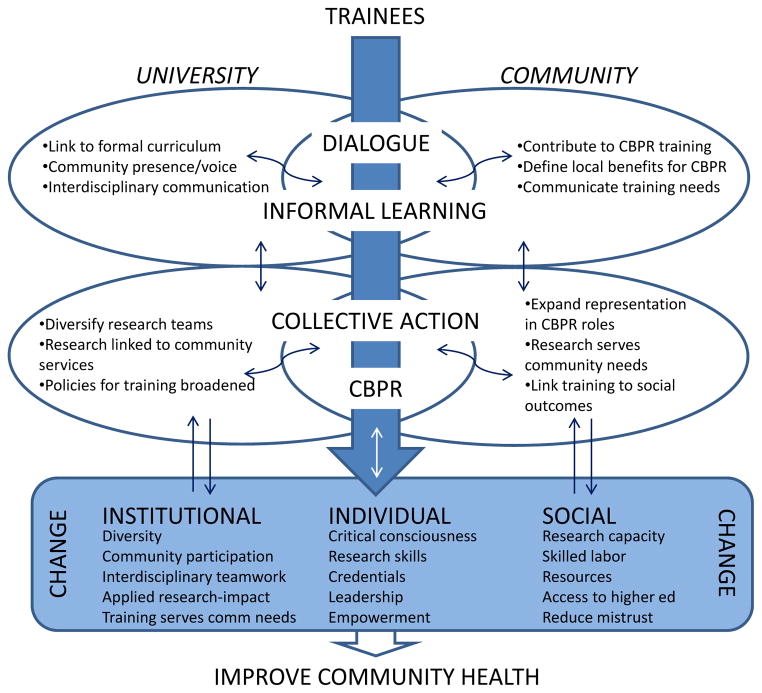
Figure 1 illustrates how minority trainee pathways can incorporate this informal learning process from both academic and community knowledge bases. The overlapping ovals represent spaces where trainees engage in dialogue or coalition-building activities in university, community, or cross-cultural settings. Trainees serve as agents who cross over physical and communication boundaries to foster environments where CBPR partnerships can take root, flourish, and create the potential for institutional and social change.
Figure 1. Trainee pathways to improve community health.
Minority trainee pathways incorporate an informal learning process that draws upon both academic and community knowledge bases. The overlapping ovals represent spaces where trainees engage in dialogue or coalition-building activities in university, community, or cross-cultural settings. As trainees become empowered, they serve as agents that foster environments where collective action and CBPR partnerships can emerge, creating potential for institutional and social change needed to improve community health.
The irrigation model encourages student-centered rather than discipline-driven career guidance. Dialogue and positive CBPR experiences expose minority trainees to multiple ways of succeeding in both the university and in the community. This approach also fosters institutional capacity for CBPR, through informal learning activities that introduce minority students and community worldviews into the academic environment.
Regardless of education level or discipline, students represent a means to bring minority participation into all phases of the research. Although community representation should not be based simply on matched ethnic, racial, or social backgrounds,12 involving students in project planning, funding, implementation, data management, and dissemination builds basic human resources for research roles that typically are held by non-minority academics.11,12 In connection with these research skills, the use of story, art, drama, and other forms of informal learning can provide an accessible platform for trainees to share their own experiences and knowledge on health disparity issues and other matters of concern to minority communities. To facilitate this informal learning and broaden respect for different types of “expert” knowledges, semi-structured exchanges can be integrated into health sciences core curricula as a complement to more traditional academic exchanges such as journal clubs. This type of environment has the potential to counter mistrust and negative community perceptions of the university as an “ivory tower”, creating a safe space for people to explore assumptions that historically privilege academic over local views on health.
Within the context of a robust commitment to improved community health, all types of research can be placed in a translational context. In addition to substantive exposure to CBPR, students benefit from opportunities to see how basic science, technology, clinical research, health services, public health and advocacy are complementary components of efforts to improve population health. Addressing the challenges of interprofessional teamwork are also increasingly important, as universities seek to overcome discipline-specific professional silos.17 An emphasis on cross-cultural collaboration between researchers, health professionals, community leaders and organizers has potential to move science toward true interdisciplinary innovation with real world applications and adoption.17,18 Placing minority training in these kinds of research environments can motivate students to join in a process that links both basic and applied science to medical and public health and a vision of downstream benefit.19,20
Re-evaluating measures of success and addressing power differentials
A proportion of minority students are interested in careers that they envision as addressing social inequities. We have repeatedly witnessed this phenomenon among American Indian college students who have worked and studied with us: “Some Native students are trying to use education to get off the reservation. I’m trying to use mine to come back” and “I wasn’t sure where I was going, but I knew I wanted to be on a track to help my people.” Similarly, Latino participants of a pre-graduate school mentoring program at University of Texas described their commitment to overcome educational challenges and pursue graduate studies as a responsibility to family and community.5 This dedication to underserved populations calls for experiences that allow trainees to see the tools of research, and challenge funders and research programs to develop methods that are more appropriate for addressing community research questions.20 For example, trainees have suggested creating scales that measure concepts of hope or spiritual resources as a way of understanding substance use relapse and framing motivators for behavior change.19 For trainees who value a link between career and action, such experiences may help them to persevere through the rigors of highly competitive programs such as medical school and doctoral training, or when this commitment is not possible, may point them to careers such as community health nursing or health program management, rather than leaving school altogether.
From this perspective, even those who leave before reaching a doctoral degree should be considered worthy of the educational investment rather than framed as a loss to the pipeline. Individuals who return to serve communities where disparities exist have potential to instigate sustainable educational and health efforts in their local surroundings.5,7 A CBPR framework acknowledges and embraces all opportunities for exposure to community knowledge, and recognizes experiences outside of campus as an extension of partnership training.11,18,19 Trainees who take on leadership roles such as managers or directors of community-based organizations, may also serve as partners or brokers of university-community research partnerships. An irrigation model argues for the creation of broader infrastructures that engage this critical workforce to optimize successful program recruitment and retention and further community-academic relations wherever minority trainees choose to live, work, and learn. These individuals are also the ones who may return to school later in their own career trajectories to pursue doctoral training, if a pathway is open to them.
Next steps for academic institutions
Several measures can assist institutions to incorporate the principles of CBPR and the irrigation model into education efforts. First, institutions should assess the status of their research partnerships with communities, ideally with assistance from minority faculty, administrative officials, and current and former students. Appropriate incentives including course credit, continuing education, and service recognition could encourage students, faculty, and personnel to participate in and shape institutional policies that support cross-cultural partnerships, and design training programs to sustain them. Second, explicit connections between minority training and community research partnerships should be developed. Research activities in collaborative and interdisciplinary settings are likely to attract students whether or not they have committed to a career track. Academic institutions can do more outreach work to increase community research capacity, such as sponsoring workshops on preparing federal research grants or helping to understand NIH reporting requirements. Internships or practica in community-based organizations also contribute to student learning while fulfilling needed service gaps. Equally important, programs should be geared to the skills required for CBPR and interdisciplinary teamwork, through research focused on questions of importance to communities.11,19 For example, evaluation methodologies that map the process and outcomes of relationship-building could assist partnerships by providing documentation and feedback on how community advisory boards evolve, address tensions, and develop ground rules for communication or decision-making. An approach to minority education that values action-based research connections provides a basis from which research can serve as a tool for societal benefit. With this infrastructure, academic research institutions can address a critical component of translation: the need for attention to and investment in education and long-term community impact.
Cultural and academic services contribute to a supportive environment for minority students,4,5,6,8 but addition of these services alone is not enough to overcome mistrust of the research enterprise. Participating in coalition-building, community forums that inform human subjects policies, and other informal learning activities that support collaborative health projects should be linked to formal curriculum. Evaluations should include measures of outcomes that illustrate leadership skills in these processes. University and community systems should work together to build CBPR capacity by preparing students to fill gaps in local positions, e.g., creating academic roles that bridge grant management services to communities, or developing joint faculty or administrative positions. Institutions should also create networks for tracking former trainees who leave lengthy or rigid professional or doctorate tracks for more flexible programs, such as a Master’s in public health or social work, that allow them to earn a salary, and to assist them in academic re-entry; e.g., leveraging a community service position toward a thesis project.
Finally, research institutions should embrace their need for capacity development. In addition to core professional competencies, all researchers and health care professionals benefit from multicultural education through experiential learning and the development of critical consciousness.21,22 Criteria for evaluation and promotion of employees should recognize community-engaged scholarship in its various forms of teaching, research, or service.23 Measures of community benefit could include indicators of social or political impact12 such as evidence of youth empowerment, or establishment of community policies to sustain effective interventions. Diversity program outcomes, in addition to pipeline model successes, should be evaluated in light of trainee contributions to strengthening community relations, connecting academic and community leadership, and increasing minority participation in higher education and research.7,23 For example, a trainee who leaves college to direct a community-based organization and in that role serves as a co-investigator in a university-directed health project should represent a successful outcome for the training program. Whether or not such activities are formally designated as CBPR, the values of power sharing, joint planning and attention to community benefit should be encouraged.
Minority trainees experience varied career routes as they weave in and out of education systems, many of which intersect through community contact or service. In this process, they can serve as key informants in efforts to address important community problems, and their expertise and culture should be welcomed on campuses where underserved groups are the focus of research or service. Viewing education as a tool for building community-based partnerships focuses on the strengths of trainees in all sectors of the health and research workforce, lays the foundation for positive academic-community relationships, and expands the reach and success of training efforts.
Acknowledgments
This work was partially supported by the Center for Genomics and Healthcare Equality [P50 HG 3374]
References
- 1.Smith SG, Nsiah-Kumi PA, Jones PR, Pamies RJ. Pipeline programs in the health professions, part 1: Preserving diversity and reducing health disparities. J Natl Med Assoc. 2009;101(9):836–40. doi: 10.1016/s0027-9684(15)31030-0. [DOI] [PubMed] [Google Scholar]
- 2.Committee for the Assessment of NIH Minority Research Training Programs. Assessment of NIH minority research training programs: Phase 3. Washington, DC: National Academies Press; 2005. p. 3. [PubMed] [Google Scholar]
- 3.Barr DA, Gonzalez ME, Wanat SF. The leaky pipeline: Factors associated with early decline in interest in premedical studies among underrepresented minority undergraduate students. Acad Med. 2008;83(5):503–11. doi: 10.1097/ACM.0b013e31816bda16. [DOI] [PubMed] [Google Scholar]
- 4.Guillory RM, Wolverton M. It’s about family: Native American student persistence in higher education. Journal of Higher Educ. 2008;79(1):58–87. [Google Scholar]
- 5.Luna V, Prieto L. Mentoring affirmations and interventions: a bridge to graduate school for Latina/o students. J of Hispanic Higher Educ. 2009:213–24. [Google Scholar]
- 6.Palmer R, Gasman M. “It takes a village to raise a child”: The role of social capital in promoting academic success for African American men at a black college. J College Student Development. 2008;49(1):52–70. [Google Scholar]
- 7.Segrest V, James R, Madrid T, Fernandes R. Launching Native Health Leaders: Students as community-campus ambassadors. Prog Community Health Partnersh. 2009;4(1):81–5. doi: 10.1353/cpr.0.0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Villajero M, Barlow AEL, Kogan D, Veazey BD, Seeney JK. Encouraging minority undergraduates to choose science careers: Career paths survey results. Life Sciences Journal. 2008;7:394–409. doi: 10.1187/cbe.08-04-0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Badenhausen K. Most lucrative college majors. Forbes.com; Jun 18, 2008. Available from http://www.forbes.com/2008/06/18/college-majors-lucrative-lead-cx_kb_0618majors.html. [Google Scholar]
- 10.Chew C. Salaries for epidemiologists with a Ph.D. 2011 May 2; eHow Money. Available from http://www.ehow.com/info_8341185_salaries-epidemiologists-phd.html.
- 11.Cargo M, Mercer SL. The value and challenges of participatory research: Strengthening its practice. Annu Rev Public Health. 2008;29:325–50. doi: 10.1146/annurev.publhealth.29.091307.083824. [DOI] [PubMed] [Google Scholar]
- 12.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312–23. doi: 10.1177/1524839906289376. [DOI] [PubMed] [Google Scholar]
- 13.Zinn MB. Field research in minority communities: ethical, methodological and political observations by an insider. Social Problems. 1979;27(2):209–219. [Google Scholar]
- 14.Wallerstein N. Evidence on effectiveness of empowerment in reducing health disparities. Geneva: Health Evidence Network, World Health Organization; 2006. Available from www.euro.who.int/HEN. [Google Scholar]
- 15.Butterfoss FD, Kegler MC. Toward a comprehensive understanding of community coalitions: Moving from practice to theory. In: DiClemente R, Crosby R, Kegler MC, editors. Emerging theories in health promotion practice and research. 2. San Francisco, CA: Jossey-Bass; 2002. [Google Scholar]
- 16.Freire P. Pedagogy of the Oppressed. New York: Herder and Herder; 1970. [Google Scholar]
- 17.Hall P. Interprofessional teamwork: Professional cultures as barriers. J Interprof Care. 2005;(Supp 1):188–196. doi: 10.1080/13561820500081745. [DOI] [PubMed] [Google Scholar]
- 18.Poole G, Egan JP, Iqbal I. Innovation in collaborative health research training: The role of active learning. J Interprof Care. 2009;23(2):148–155. doi: 10.1080/13561820802634894. [DOI] [PubMed] [Google Scholar]
- 19.Alegria M. Training for research in mental health and HIV/AIDS among racial and ethnic minority populations: Meeting the needs of new investigators. Am J Public Health. 2009;99(suppl 1):S26–30. doi: 10.2105/AJPH.2008.135996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moreno-John G, Fleming C, Ford ME, Mangione CM, Tilley B, Washington OGM, Carrasquillo O. Mentoring in community-based participatory research: The RCMAR experience. Ethn Dis. 2007;17(suppl 1):S33–43. [PubMed] [Google Scholar]
- 21.Basu SJ, Barton AC. A researcher-student-teacher model for democratic science pedagogy: Connections to community, shared authority, and critical science agency. Equity and Excellence in Educ. 2010;43(1):72–87. [Google Scholar]
- 22.Grumbach K, Mendoza R. Disparities in human resources: Addressing the lack of diversity in the health professions. Health Aff. 2008;27(2):413–22. doi: 10.1377/hlthaff.27.2.413. [DOI] [PubMed] [Google Scholar]
- 23.Jones L, Wells K. Strategies for academic and clinician engagement in community-based participatory partnered research. JAMA. 2007;297(4):407–10. doi: 10.1001/jama.297.4.407. [DOI] [PubMed] [Google Scholar]
- 24.Israel BA, Schulz AJ, Parker EA, Becker AB, Allen AJ, Guzman R. Critical issues in developing and following community based participatory research principles. In: Wallerstein MMN, editor. Community based participatory research for health. San Francisco: Jossey-Bass; 2003. [Google Scholar]