Abstract
OBJECTIVES
The purpose of this study was to understand the reason for variation in the sensitivity of different methods of detecting right-to-left shunts (RLS).
BACKGROUND
Patent foramen ovale (PFO) is implicated in the pathogenesis of cryptogenic stroke, decompression illness, and migraine headaches. Intravenous agitated saline injections with tomographic imaging (transthoracic, transesophageal, and intracardiac echocardiography) has been used for detecting intracardiac shunts. Some patients with a high clinical suspicion of PFO have inconclusive echocardiographic study results. Transcranial Doppler (TCD) is an alternative method for detecting RLS that is not dependent on tomographic imaging.
METHODS
Thirty-eight consecutive patients who were undergoing PFO closure had simultaneous transcranial Doppler and intracardiac echocardiography performed. Agitated saline injections were performed at rest, with Valsalva maneuver, and with forced expiration into a manometer to 40 mm Hg before and after closure, as well as 3 or more months after closure. Right atrial pressures were measured in the periprocedural period, and RLS were graded according to standard methods during these maneuvers.
RESULTS
Right atrial pressures were significantly higher with Valsalva maneuver compared with rest (before closure 21.6 ± 11.9 mm Hg vs. 6.6 ± 2.6 mm Hg, p < 0.001; after closure 28.4 ± 13.9 mm Hg vs. 6.8 ± 2.6 mm Hg, p < 0.001) and with manometer compared with Valsalva maneuver (before closure 38.7 ± 6.6 mm Hg vs. 21.6 ± 11.9 mm Hg, p < 0.001; after closure 44.0 ± 9.5 mm Hg vs. 28.4 ± 13.9 mm Hg, p < 0.001). Intracardiac echocardiography underestimated shunting in 34% of patients with Valsalva maneuver or manometer after closure compared with TCD.
CONCLUSIONS
Transcranial Doppler with immediate feedback provided by forced expiration against a manometer to 40 mm Hg is more sensitive than echocardiographic imaging for the detection of RLS. These observations have significant implications for determining the incidence of RLS in patients with stroke or migraine.
Keywords: patent foramen ovale, transcranial Doppler, stroke
Patent foramen ovale (PFO) has been implicated in the pathogenesis of several detrimental conditions, such as cryptogenic stroke, decompression illness, and migraine headaches (1–5). It is estimated that 20% to 25% of adults have a PFO (6). Intravenous agitated saline injections with transthoracic echocardiography (TTE) has been used to diagnose the presence of a PFO and to quantitate the right-to-left passage of blood; however, TTE is not as sensitive or as specific as transesophageal echocardiography (TEE) for detecting intracardiac shunts (7). In addition, some patients with a high clinical suspicion of PFO have inconclusive echocardiographic study results, partially from a lack of co-operation with the Valsalva maneuver from sedation. Intracardiac echocardiographic (ICE) imaging also has been used to determine the presence and severity of right-to-left shunting through a PFO. Detection of right-to-left shunts (RLS) using transcranial Doppler (TCD) imaging overcomes the limitation of sedation during TEE while maintaining a high sensitivity rate (8,9). We measured right atrial pressures during Valsalva maneuver and forced expiration through a manometer and compared TCD assessment versus ICE imaging in the cardiac catheterization laboratory to elucidate the mechanism for the differences in sensitivity of these methods for detection of RLS.
METHODS
Study population
Thirty-eight consecutive patients were brought to the adult cardiac catheterization laboratory for PFO closure. Patients were referred who suffered a neurological event indicative of cryptogenic stroke or transient ischemic attack and with a high clinical suspicion of PFO, with 37 of the 38 patients having a positive TTE or TEE before the procedure. The study received prior approval by our Institutional Review Board for Human Research, and all patients signed informed consent.
Procedure
All patients had TCD imaging performed in the catheterization laboratory using a portable Spencer PMD 150 Digital System (Spencer Technologies, Seattle, Washington). Ultrasonic probes were mounted on a head frame, which was positioned on the insonation windows located on the temporal bone. Individual probes were manipulated to locate the middle cerebral artery. Grading of RLS was performed by counting the number of embolic tracks on the power M-mode and Doppler spectrogram in real time as shown in Table 1 (10).
Table 1.
Spencer Grading of Right-to-Left Shunts by Transcranial Doppler
| Grade | Number of Embolic Tracks |
|---|---|
| 0 | 0 |
| I | 1-10 |
| II | 11-30 |
| III | 31-100 |
| IV | 101-300 |
| V | >300 or shower effect |
A Spencer transcranial Doppler grade ≥2 was assumed to represent a significant shunt.
A 6-F multipurpose coronary catheter was used to measure right atrial pressures. The RLS grade was recorded during injection of agitated saline, and right atrial pressures were measured at baseline, during Valsalva maneuver, and during forced exhalation into a manometer to 40 mm Hg. These measurements were repeated after device deployment. Agitated saline was created by using 8 ml saline, 2 ml blood, and 0.5 ml air. The solution was rapidly passed between 2 10-ml syringes connected together through a 3-way stopcock. The stopcock was connected to the sidearm of an 8-F or 10-F sheath placed in the femoral vein that was used for delivery of the device. The agitated saline produced a foam of microbubbles that was injected into the femoral vein. If the bubble study showed a grade 5 shunt at rest, then the injection was not repeated with Valsalva maneuver or with forced expiration into the manometer. Right atrial pressures were obtained during these straining maneuvers, but no more agitated saline was injected if the RLS was already documented to be maximum at rest.
The percutaneous PFO closure techniques have been described previously (11). The PFO was closed using the Helex (Gore Medical, Flagstaff, Arizona) or Amplatzer Cribriform (AGA Medical, Minneapolis, Minnesota) atrial septal occluder device. All patients received intravenous heparin to achieve an activated clotting time >250 s. ICE was performed with an 8-F or 10-F Acuson AcuNav catheter (Acuson, Mountain View, California). We quantified the RLS by ICE using a grading scale based on the number of microbubbles visualized in the left atrium in 1 view during imaging: grade 0 = no microbubbles, grade 1 = 1 to 10, grade 2 = 11 to 20, grade 3 ≥20.
Follow-up TCD studies were performed 3 to 16 months after PFO closure at rest, with Valsalva maneuver and with forced expiration into a manometer to 40 mm Hg. Intravenous agitated saline injections were performed in a similar manner with the patient in a supine position through an upper-extremity antecubital vein.
Statistical analysis
Continuous variables are expressed as mean ± SD or median and interquartile range, as appropriate. Dichotomous variables are expressed as frequency percentage. We used the paired Student t test to compare right atrial pressure between different maneuvers before and after deployment. The Pearson correlation coefficient was calculated to estimate the association between pressures generated by the Valsalva maneuver and those using the manometer. The exact McNemar test was used to compare the rates of detecting significant RLS between ICE and TCD. All tests were 2-sided, and a value of p < 0.05 was considered statistically significant.
RESULTS
PFO closure
Baseline demographics are shown in Table 2. In our study population, TEE had a false-negative rate of 7.9% (3 of 38 patients). Of 38 patients, the majority (63%) were men and the mean age was 49.3 ± 16.5 years. The Helex device was used in 31 (82%) patients, and the Amplatzer cribriform device was used in 7 (18%) patients. All device deployments were successful.
Table 2.
Baseline Characteristics of the Patient Population
| n | % | |
|---|---|---|
| Average age | 49.3 ± 16.5 | |
| Sex | ||
| Male | 24 | 63 |
| Female | 14 | 37 |
| Device | ||
| Amplatzer | 7 | 18 |
| Helex | 31 | 82 |
| TCD shunt grade before closure* | ||
| Grade ≥5 at rest | 19 | 50 |
| Grade ≥5 with Valsalva maneuver | 13 | 34 |
| Grade ≥5 with manometer | 4 | 11 |
The majority of the patient population was male (63%), and the mean age was 49.3 ± 16.5 years.
Bubble studies were sequentially performed at rest, with Valsalva and with the manometer. If a TCD grade 5 shunt was discovered, further agitated saline injections were not repeated. One patient did not have a TCD ≥5 at any state, and PFO was diagnosed by mechanical probe of the septum.
PFO = patent foramen ovale; TCD = transcranial Doppler.
Right atrial pressure measurements
Before device deployment, the average resting right atrial pressure was 6.6 ± 2.6 mm Hg. With the Valsalva maneuver, patients generated a mean pressure of 21.6 ± 11.9 mm Hg, which was significantly increased compared with that at rest (p < 0.001). Using the manometer with forced expiration, the pressure achieved in the right atrium (38.7 ± 6.6 mm Hg, n = 34) was significantly increased compared with that at rest (p < 0.001) or during Valsalva maneuver (p < 0.001). In 25 patients, repeat right atrial pressure measurements were recorded after the deployment of the device during rest, Valsalva maneuver, and manometer conditions. As shown in Table 3, there was no significant difference in the resting (n = 25) right atrial pressure before or after device deployment. There was a trend toward higher pressures with manometer (n = 23), and a statistically significant increase in Valsalva maneuver– generated (n = 24) right atrial pressures after PFO closure (paired Student t test, p = 0.06 with manometer and p = 0.01 with Valsalva maneuver). After device deployment, right atrial pressures using the manometer (44.0 ± 9.5 mm Hg) were significantly increased compared with those using Valsalva maneuver (28.4 ± 13.9 mm Hg, p < 0.001) and at rest (6.8 ± 2.6 mm Hg, p < 0.001).
Table 3.
Right Atrial Pressures Before and After PFO Closure
| Pressure (mm Hg) |
|||
|---|---|---|---|
| Condition | Before Closure | After Closure | p Value |
| At rest | 6.6 ± 2.6 (n = 38) | 6.8 ± 2.6 (n = 25) | 0.65 |
| Valsalva maneuver | 21.6 ± 11.9* (n = 38) | 28.4 ± 13.7* (n = 24) | 0.01 |
| Manometer | 38.7 ± 6.6† (n = 34) | 44.0 ± 9.3† (n = 23) | 0.06 |
There was no significant difference in the resting right atrial pressure before or after device deployment. There was a trend toward higher pressures with manometer and a statistically significant increase in Valsalva maneuver-generated right atrial pressures after patent foramen ovale (PFO) closure (paired Student t test, p = 0.06 with manometer and p = 0.01 with Valsalva maneuver), suggesting a learning effect with repeated Valsalva and manometer maneuvers.
p < 0.001 compared with rest.
p < 0.001 compared with Valsalva maneuver.
Comparison of Valsalva maneuver– and manometer-derived pressures
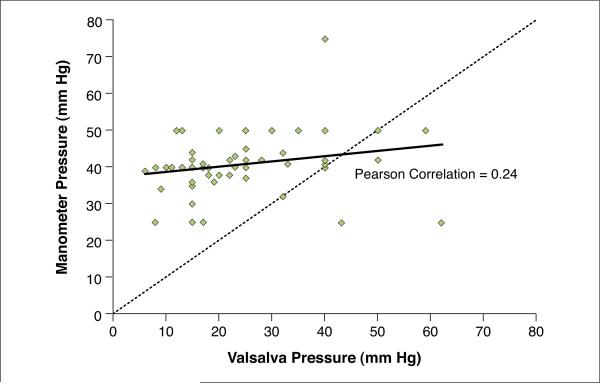
Figure 1 shows the wide variability of pressures generated by the Valsalva maneuver. There was no significant correlation between pressures generated by the Valsalva maneuver and those generated using the manometer (Pearson correlation = 0.24, p = 0.07). The lowest right atrial pressure measurement obtained with the manometer was 25 mm Hg. A total of 33 of 37 patients (89%) had evidence of RLS by TCD at this level of effort immediately after PFO closure. One patient did not have a post-closure bubble study performed and was excluded from this analysis. Thus, using 25 mm Hg as an arbitrary pressure cutoff, 49% of patients were able to generate adequate pressure using a self-induced Valsalva maneuver, in comparison to 100% of patients using the manometer method. The scatter plot shows that the effort of forced expiration against a manometer with visual feedback usually (85% of cases) produced a higher transthoracic pressure compared with the Valsalva maneuver without the manometer.
Figure 1. Comparison of Right Atrial Pressures Measured During Valsalva Maneuver Versus Manometer.
There was no significant correlation between pressures generated by the Valsalva maneuver and those generated using the manometer to 40 mm Hg (Pearson correlation 0.24, p = 0.07). The majority (49 of 56, 87.5%) of patients were able to generate a higher pressure with manometer than with Valsalva maneuver. The dotted line represents line of identity.
Comparison of ICE and TCD
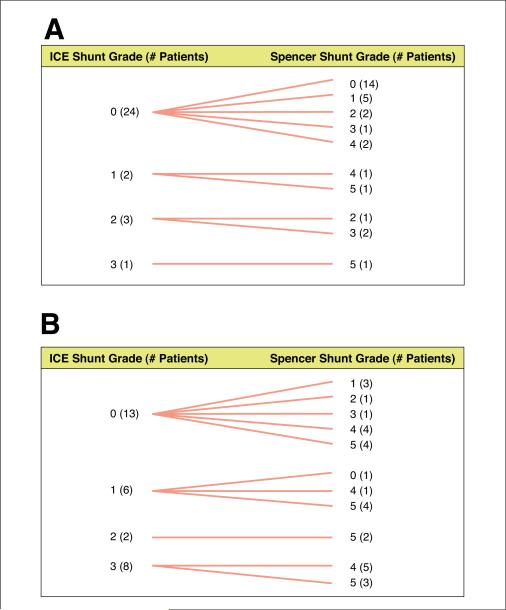
Table 4 summarizes the quantification of RLS by ICE versus TCD before and after deployment of the PFO closure device. Five patients did not have ICE data available for analysis, 1 patient did not have ICE performed, and 1 patient did not have bubble studies performed after PFO closure. These 7 patients were excluded from this analysis. One patient had the procedure performed under general anesthesia, and another patient did not have the ICE images captured with Valsalva maneuver/manometer. These 2 additional patients were excluded from the Valsalva maneuver/manometer analysis. An ICE grade ≥1 or a Spencer TCD grade ≥2 was assumed to represent a significant shunt. Before closing the PFO, when there was a large RLS, ICE and TCD had comparable rates of detecting significant RLS. After device closure, when there was minimal RLS, ICE underestimated the amount of RLS after device deployment in 5 patients (17%) at rest and 10 patients (34%) during the Valsalva or manometer maneuvers. The TCD also had a significantly higher rate of detecting significant RLS during the Valsalva or manometer maneuvers (p = 0.012). Figure 2 shows the individual comparison of ICE versus TCD grading for each patient after PFO closure, both at rest (Fig. 2A) and with Valsalva maneuver or manometer feedback (Fig. 2B). Ten patients (10 of 29, 34%) had an ICE grade 0 despite a TCD Spencer grade ≥2.
Table 4.
Comparison of RLS Quantification With ICE Versus TCD
| Condition | ICE Grade ≥1 | TCD Grade ≥2 | RLS Shunt Underestimated by ICE | RLS Shunt Underestimated by TCD | p Value |
|---|---|---|---|---|---|
| Pre-deployment Valsalva maneuver (n = 31) | 30/31 (97%) | 30/31 (97%) | 1/31 (3%) | 1/31 (3%) | >0.99 |
| Post-deployment rest (n = 30) | 6/30 (20%) | 11/30 (37%) | 5/30 (17%) | 0/30 (0%) | 0.063 |
| Post-deployment Valsalva maneuver/manometer (n = 29) | 16/29 (55%) | 25/29 (86%) | 10/29 (34%) | 1/29 (3%) | 0.012 |
An ICE grade ≥1 or a Spencer TCD grade ≥2 was assumed to represent a significant shunt. Before closure, when there was a large RLS, ICE and TCD had comparable rates of detecting significant RLS. After device closure, when there was diminished RLS, ICE underestimated the amount of RLS after device deployment in 5 patients (17%) at rest and 10 patients (34%) during the Valsalva or manometer maneuvers. The ICE images were not available for analysis on 5 patients, ICE was not performed on 1 patient, and post-closure bubble study was not performed on 1 patient (all excluded from this analysis); post-deployment ICE was not performed on 2 patients, post-deployment provocative maneuvers were not performed on 1 patient. ICE = intracardiac echocardiography; RLS = right-to-left shunt; TCD = transcranial Doppler.
Figure 2. Grade of Shunt Assessed by ICE or TCD After Closure at Rest and After Valsalva Maneuver.
Comparison of RLS quantification by ICE and TCD on a per-patient basis after deployment of patent foramen ovale closure device at rest (A) and using a Valsalva maneuver or manometer (B). There were 30 patients assessed at rest and 29 patients assessed with a Valsalva maneuver or manometer. The Spencer shunt grade tended to be higher than the ICE shunt grade. The TCD detected a Spencer grade ≥2 shunt in 5 patients at rest and 10 patients with Valsalva maneuver or manometer, even when no shunt was observed by ICE. ICE = intracardiac echocardiography; RLS = right-to-left shunt; TCD = transcranial Doppler.
Follow-up TCD
Of the 38 patients, 31 (82%) had a repeat TCD study at 3 or more months (average 6.2 ± 3.61 months, range 3 to 16 months, median 5 months, interquartile range 3 to 8.25 months) after PFO closure. The average resting Spencer shunt grade was 0.4 ± 0.8 (median 0, interquartile range 0 to 1). The average forced manometer shunt grade was 1.2 ± 1.2 (median 1, interquartile range 0 to 2). Using a Spencer TCD grade ≥2 as a positive study, 1 patient (2.6%) at rest and 10 patients (26%) with forced manometer had a positive TCD study result.
DISCUSSION
This study demonstrates that a significantly lower right atrial pressure is achieved during voluntary Valsalva maneuver compared with forced expiration into a manometer. This finding was reproducible before and after device deployment. The lack of a sufficient pressure gradient between the right and left atria has been postulated to contribute to false-negative TEE results in the detection of PFO (12). When patients were asked to voluntarily perform a Valsalva maneuver during our study, inadequate transthoracic pressures were achieved in 50% of cases. As shown in Figure 1, forced expiration with the visual feedback provided by the manometer was more successful in reaching the target level of 40 mm Hg compared with the patient's spontaneous effort with a Valsalva maneuver. This study confirms that false-negative assessment of RLS may occur due to inadequate pressures generated during Valsalva maneuvers despite what seems to be a learning effect with repeated Valsalva and manometer maneuvers as demonstrated by the differences in the before closure and after closure pressures shown in Table 3. The attempt by the patient to produce a high intrathoracic pressure would be even more difficult with TEE probe intubation or after significant sedation.
There are several explanations for the differences in the sensitivities of the methods of identifying an RLS through a PFO. One explanation is the generation of different intrathoracic pressures by the patients in our study. Patients have a variable response in effort after being told to “bear down” or “strain as if you are trying to go to the bathroom.” Using a manometer, patients have a defined goal that can be visualized for immediate feedback and is therefore more likely to be achieved. The end result is a higher and more consistent pressure generated in the thoracic cavity. In addition, our studies were performed by withdrawing blood, which creates a much more efficient form of agitated saline that completely filled the right atrium as documented by ICE imaging. Many echocardiography laboratories perform TEE agitated saline bubble studies without mixing blood in the injectate.
The other major observation of this study is that the sensitivity of TCD was superior to direct imaging of the left atrium for passage of bubbles across the PFO. In comparing ICE and TCD, performed simultaneously for the detection of RLS after PFO closure, ICE did not detect any RLS in 34% of patients. Additionally, 17% of patients at rest and 34% during Valsalva maneuver or manometer conditions had an RLS grade by TCD that was significantly higher than the estimated grade by counting the microbubbles visually seen in the left atrium. Because ICE, TTE, and TEE are tomographic forms of imaging, a significant portion or all of the shunting into the left atrium may be missed by the limited imaging plane.
During the follow-up TCD, there was no shunt during rest and minimal RLS with the manometer. Ten of the shunts at rest and 15 of the RLS observed with the manometer immediately after PFO closure had resolved at follow-up. This is consistent with published studies showing that closure rates increase with percutaneous devices over a period of months (13).
Because of the increased sensitivity of TCD, echocardiography could be negative and yet the TCD could show a significant shunt. This could result in a failure to detect a number of patients with PFOs. This may have implications for epidemiologic studies, which could underestimate the incidence of PFO, depending on the method used to diagnose an RLS. This also raises the question of whether prior studies that separate PFOs with or without atrial septal aneurysms are correct. The methods of detection that were used in those studies could have missed the RLS, and therefore could have misplaced the subjects into the wrong categories (14,15). A TCD evaluation performed while bearing down against a calibrated manometer seems to be more accurate than the other methods to quantitate the size and presence of an RLS. This also would be important in migraine studies, in which a PFO could be treated by a device and yet a small RLS could still exist through the device or the pulmonary circulation and be missed by echocardiography.
A TCD by itself does not reveal the anatomic origin of the shunt. The shunt could be at the pulmonary or cardiac level with a positive TCD. However, the increased sensitivity of TCD suggests that it would be the method of choice if the question asked is: does the patient have an RLS? The optimal assessment of an RLS would be a TCD agitated saline–blood study in addition to an anatomic assessment of the shunt by TEE or ICE.
CONCLUSIONS
Establishing the diagnosis of PFO is important for understanding the mechanisms of certain diseases, such as cryptogenic stroke and migraine. A TEE may not be the optimal initial screening test for the detection of PFO. In addition to avoiding the discomfort of TEE, TCD during forced expiration to 40 mm Hg into a manometer provides immediate feedback so that the patient is more likely to achieve this atrial pressure. The result is that TCD is more sensitive than tomographic imaging modalities such as TTE, TEE, and ICE for detecting significant RLS.
Acknowledgments
This study was funded by an unrestricted grant from AGA Medical, Inc. Dr. Tobis is a consultant to AGA Medical, Inc., and is on the medical advisory board for the PREMIUM trial.
ABBREVIATIONS AND ACRONYMS
- ICE
intracardiac echocardiography
- PFO
patent foramen ovale
- RLS
right-to-left shunt
- TCD
transcranial Doppler
- TEE
transesophageal echocardiography
- TTE
transthoracic echocardiography
REFERENCES
- 1.Lechat P, Mas JL, Lascault G, et al. Prevalence of patent foramen ovale in patients with stroke. N Engl J Med. 1988;318:1148–52. doi: 10.1056/NEJM198805053181802. [DOI] [PubMed] [Google Scholar]
- 2.Overell JR, Bone I, Lees KR. Inter-atrial septal abnormalities and stroke: a meta-analysis of case-control studies. Neurology. 2000;55:1172–9. doi: 10.1212/wnl.55.8.1172. [DOI] [PubMed] [Google Scholar]
- 3.Handke M, Harloff A, Olschewski M, Hetzel A, Geibel A. Patent foramen ovale and cryptogenic stroke in older patients. N Engl J Med. 2007;357:2262–8. doi: 10.1056/NEJMoa071422. [DOI] [PubMed] [Google Scholar]
- 4.Del Sette M, Angeli S, Leandri M, et al. Migraine with aura and right-to-left shunt on transcranial Doppler: a case-control study. Cerebrovasc Dis. 1998;8:327–30. doi: 10.1159/000015875. [DOI] [PubMed] [Google Scholar]
- 5.Sztajzel R, Genoud D, Roth S, Mermillod B, Le Floch-Rohr J. Patent foramen ovale, a possible cause of symptomatic migraine: a study of 74 patients with acute ischemic stroke. Cerebrovasc Dis. 2002;13:102–6. doi: 10.1159/000047758. [DOI] [PubMed] [Google Scholar]
- 6.Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984;59:17–20. doi: 10.1016/s0025-6196(12)60336-x. [DOI] [PubMed] [Google Scholar]
- 7.Pearson AC, Labovitz AJ, Tatineni S, Gomez CR. Superiority of transesophageal echocardiography in detecting cardiac source of embolism in patients with cerebral ischemia of uncertain etiology. J Am Coll Cardiol. 1991;17:66–72. doi: 10.1016/0735-1097(91)90705-e. [DOI] [PubMed] [Google Scholar]
- 8.Teague SM, Sharma MK. Detection of paradoxical cerebral echo contrast embolization by transcranial Doppler ultrasound. Stroke. 1991;22:740–5. doi: 10.1161/01.str.22.6.740. [DOI] [PubMed] [Google Scholar]
- 9.Blersch WK, Draganski BM, Holmer SR, et al. Transcranial duplex sonography in the detection of patent foramen ovale. Radiology. 2002;225:693–9. doi: 10.1148/radiol.2253011572. [DOI] [PubMed] [Google Scholar]
- 10.Spencer MP, Moehring MA, Jesurum J, Gray WA, Olsen JV, Reisman M. Power M-mode transcranial Doppler for diagnosis of patent foramen ovale and assessing transcatheter closure. J Neuroimaging. 2004;14:342–9. doi: 10.1177/1051228404268743. [DOI] [PubMed] [Google Scholar]
- 11.Azarbal B, Tobis J, Suh W, Chan V, Dao C, Gaster R. Association of interatrial shunts and migraine headaches: impact of transcatheter closure. J Am Coll Cardiol. 2005;45:489–92. doi: 10.1016/j.jacc.2004.09.075. [DOI] [PubMed] [Google Scholar]
- 12.Woods TD, Patel A. A critical review of patent foramen ovale detection using saline contrast echocardiography: when bubbles lie. J Am Soc Echocardiogr. 2006;19:215–22. doi: 10.1016/j.echo.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 13.von Bardeleben RS, Richter C, Otto J, et al. Long term follow up after percutaneous closure of PFO in 357 patients with paradoxical embolism: difference in occlusion systems and influence of atrial septal aneurysms. Int J Cardiol. 2009;134:33–41. doi: 10.1016/j.ijcard.2008.02.031. [DOI] [PubMed] [Google Scholar]
- 14.Mas JL, Arquizan C, Lamy C, et al. Recurrent cerebrovascular events associated with patent foramen ovale, atrial septal aneurysm or both. N Engl J Med. 2001;345:1740–6. doi: 10.1056/NEJMoa011503. [DOI] [PubMed] [Google Scholar]
- 15.Rundek T, Elkind MS, Di Tullio MR, et al. Patent foramen ovale and migraine: a cross-sectional study from the Northern Manhattan Study (NOMAS). Circulation. 2008;118:1419–24. doi: 10.1161/CIRCULATIONAHA.108.771303. [DOI] [PMC free article] [PubMed] [Google Scholar]