Abstract
The purpose of the present study was to investigate risk and protective factors for intimate partner violence (IPV) victimization in a high-risk sample of predominantly minority young adults from low-income urban communities. Participants were 1,130 individuals (57.9% women) ages 21 to 26 who participated in a telephone interview assessing IPV victimization, violence-related behaviors, and sexual behaviors. Results indicated that about 20.9% of participants reported experiencing one or more IPV incidents in their lifetime. Based on previous research, we examined lifetime violence, lifetime number of sexual partners, number of children, education, and religious service attendance as predictors of IPV. Results from a multivariate logistic regression showed that lifetime violence-related behaviors, number of lifetime sexual partners, and number of children were significant risk factors for IPV. The link between children and IPV risk: (a) was moderated by education for women and men and (b) was stronger for women (vs. men). These findings suggest that training for coping with stress and anger, endorsement of safe sex practices, and greater support for education may be effective strategies for preventing and reducing IPV among high-risk populations.
Keywords: domestic violence, intervention/treatment, predicting domestic violence, youth violence, alcohol and drugs
Intimate partner violence (IPV)—defined as physical aggression, emotional abuse, and sexual violence (Centers for Disease Control and Prevention [CDC], 2001)—is a widespread issue that affects a nontrivial number of people and couples. According to large population-based surveys, the lifetime prevalence of IPV is between 25% and 30% (Tjaden & Thoennes, 2000). In the United States alone, roughly 50% of couples have reported some incidence of IPV in their lifetime (e.g., Lawrence & Bradbury, 2001; Slep & O’Leary, 2005), and results from national surveys suggest that annual prevalence rates of IPV range from 11% to 39% (e.g., Plichta, Duncan, & Plitcha, 1996; Schaeffer et al., 1998; Straus & Gelles, 1990).
IPV is associated with a host of health and psychosocial issues for individuals, families, and child development. In addition to physical injury, IPV victims report greater psychological distress, substance use, sexually transmitted diseases, HIV/AIDS, and unintended pregnancy (e.g., Bonomi, Anderson, Rivera, & Thompson, 2007; Campbell et al., 2002; Coker et al., 2002). In severe cases, IPV may result in homicide; with women being more likely to be murdered by a male partner (Centers for Disease Control and Prevention [CDC], 2005). IPV is also disruptive to couple functioning, as evidenced by greater dissatisfaction, dissolution, and conflict in couples (Katz, Kuffel, & Coblentz, 2002; Lawrence & Bradbury, 2001). The effects of being exposed to family violence on children are not trivial; higher levels of post-traumatic stress disorder, disruptions in psychosocial functioning, negative peer interactions, substance abuse, and aggressive behaviors are just among a few of the symptoms (e.g., Kilpatrick & Williams, 1997; McCloskey & Walker, 2000; Repetti, Taylor, & Seeman, 2002; Wolfe, Crooks, Chjodo, Hughes, & Ellis, 2011). Over the life span, if not resolved, maladaptive patterns become compounded and often get transmitted to future generations. Certainly, a safe and nurturing early family environment set the foundation for a lifetime of outcomes.
The costs associated with IPV in the U.S. range from US$1.7 billion to US$10 billion annually (Meyer, Scott, & Deal, 1992; Straus, 1986; Straus & Gelles, 1990). These figures are underestimates as many incidents go unreported or underdiagnosed (e.g., Bhargava et al., 2011). The implications of IPV on society and the system are far-reaching. Thus, it is important to identify factors to prevent and protect individuals from IPV and its escalation.
This study examined several risk and protective factors for IPV victimization among racial/ethnic minority young adults from economically disadvantaged communities in New York City. We selected a high-risk sample based on data from national surveys showing that young couples from racial/ethnic minority groups and from low socioeconomic groups are at highest risk for IPV (e.g., Capaldi, Knoble, Shortt, & Kim, 2012; Fox et al., 2002; Halpern, Spriggs, Martin, & Kupper, 2009). National studies suggest that the highest levels of IPV occur among youth, peaking in adolescence and early adulthood (e.g., Capaldi, Shortt, & Kim, 2005; Foshee et al., 2009; Moffitt & Caspi, 1998). Alarmingly, a national study of 4,000 individuals found rates of IPV as high as 80% among adolescents in relationships and 25% in young adults (Halpern et al., 2009). On the brighter side, violence among relationship partners seems to decline with increasing age, beyond one’s 20s as reported in a review of IPV research (Capaldi et al., 2012).
Factors Associated With Intimate Partner Violence
Across systematic reviews of IPV research some consistent trends regarding risk factors have emerged (e.g., Foran & O’Leary, 2008; Schumacher, Feldbau-Kohn, Smith Slep, & Heyman, 2001). For example, individual level factors such as antisocial and aggressive behavior, poor psychosocial adjustment, impulsivity, and risk-taking, are associated with greater IPV (Bettencourt et al., 2006; Capaldi et al., 2012; O’Leary & Slep, 2003; Shorey, Brasfield, Febres, & Stuart, 2011; Smith, White, & Holand, 2003; Vézina, & Hebert, 2007). The links between these factors and IPV may persist over the life span. For example, a longitudinal study with roughly 1,000 middle-school students showed that aggression (e.g., being in a fight, threatening someone with a weapon) measured in the eighth grade predicted IPV at 19 to 20 years of age (O’Donnell, Agronick, Duran, Myint-U, & Stueve, 2009).
Number of sexual partners has also been shown to be significantly related to IPV (e.g., Coker, 2007; Davila & Brackley, 1999; Miller et al., 2010; O’Donnell, Agronick, Duran, Myint-U, & Stueve, 2009; Teitelman, Ratcliffe, Morales-Aleman, & Sullivan, 2007). In fact, studies around the globe have focused on sexual behaviors in association with IPV as it is robustly linked with unintended pregnancy, complications during pregnancy, and sexually transmitted diseases (review, Pallitto, Campbell, & O’Campo, 2005). In the present study we assessed lifetime involvement in violent incidents and the lifetime number of sexual partners as potential risk factors for IPV victimization.
Theory and research have also emphasized a variety of contextual factors in association with IPV. According to dynamic developmental systems perspective (DDS), couple violence is seen as an interactional pattern influenced by the conjoint developmental characteristics and behaviors of each partner, contextual factors (e.g., community, demographic background) and relationship processes (Capaldi et al., 2005). Interdependence theory (Kelley & Thibaut, 1978; Rusbult, 1980) also emphasizes the role of context proposing that greater mutual reliance increases opportunities for disagreements among partners and poses greater constraints to exit relationships. Having children together is a common reported barrier for ending a relationship where IPV may be ongoing (Burch & Gallup, 2004; Gazmararian et al., 1995; Henning & Connor-Smith, 2011; O’Donnell et al., 2006). Children may be a risk factor for IPV for other reasons, such as financial issues and other stressors (e.g., Roberts et al., 2011).
Another factor that seems to be linked with IPV is education level, with some research showing that lower partner education is a risk factor for victimization (Melander, Noel, & Tyler, 2010). Another study showed that education level was a stronger predictor of IPV (compared with employment status), even when controlling for parental IPV, alcohol use, and impulsivity (Cunradi, Caetano, & Schafer, 2002). Therefore, we investigated the extent to which education level may be protective of IPV among a high-risk young adult sample.
Community engagement and social support are also important factors that buffer individuals from IPV (e.g., Huang, Song, & Wang, 2010; Lanier & Maume, 2009). For example, some research shows that religious involvement is associated with lower levels of IPV (e.g., Ellison, Steinfield, & Lampe, 2007); even among adolescents (e.g., Mahoney et al., 1999; Nonnemaker, McNeely, & Blum, 2003
Current Study
The purpose of the present study was to investigate risk and protective factors for IPV victimization among a high-risk sample of predominantly minority young adults living in low-income urban communities. Based on previous research, we examined lifetime violence, lifetime number of sexual partners, number of children, education, and religious involvement as predictors of IPV.
Data were based on telephone surveys from a larger cohort study examining risk behaviors in young adulthood. First, we examined rates of IPV among the sample. Next, we examined the extent to which several key hypothesized individual and contextual factors predicted the likelihood of IPV. Finally, we explored a variety of interaction effects to potentially reveal novel patterns of results for IPV risk.
Method
Procedures
All study procedures were approved by the Institutional Review Board at Weill Cornell Medical College. Participants from this study were from a larger multiwave study investigating the effects of a large, school-based drug abuse and violence prevention trial on risk behaviors in young adults (Botvin, Griffin, & Nichols, 2006). The sample from the present study included individuals that completed a telephone survey. Of the original sample recruited for the study, 79.1% completed the telephone survey. Participants were mailed a study packet which included a description of the study goals along with US$2, and an invitation to participate in a 20 to 40 min phone interview in return for US$40 compensation. Trained study personnel conducted the telephone interviews starting with a description of the study and oral consent procedures, followed by questions about: IPV, sex behaviors, violence-related behaviors, and general demographics (e.g., age, race/ethnicity, household income, relationship status, and education).
Participants
The analysis was constrained to individuals in the untreated control group (as our intention was to examine risk factors among a normative sample) and to those that reported being in a relationship at some point in their life (since the focus of the study was IPV). The resulting sample of participants (N = 1130) included 654 women (57.9%) and 476 men (42.1%) with a mean age of 22.8 years (range 21–26 years). At the time of the study, 38.7% of participants were single, 39.1% had a girlfriend/ boyfriend, 7.8% were engaged, 13.4% were married, or living with a partner, and 1.1% were divorced or separated. Approximately 73.9% reported having no children, 18.5% had one child, 5.5% had two children, and 2.1% had three or more children. Participants had completed a median of 14.0 years of education; about 10.9% reported less than a high school education, 54.6% had attained a high school degree (or equivalent), 14.2% had an associate’s college degree, 18.9% had a bachelor’s college degree, and 0.4% had a master’s degree or higher. The median annual income of the sample was between US$10,000 and US$20,000. Participants reported their race/ethnicity as follows: 60.4% African American/Black, 29.6% Latino/Hispanic, 12.5% White/non-Latino, 7.3% Asian, and 4.5% Native American.
Measures
Intimate Partner Violence
We assessed IPV victimization with one item asking, “In your lifetime, how many times did your partner ever hit, slap, or physically hurt you on purpose?” (Centers for Disease Control and Prevention [CDC], 2009). Participants could select one of the following: 0 times, one to two times, three to five times, six to nine times, 10 to 19 times, 20 to 39 times, 40 to 99 times, and 100 or more times. As expected, the prevalence of IPV was highly skewed, with virtually all respondents reporting either no history of IPV or a number of incidents in the low single digits. Thus, response options were collapsed into a dichotomous variable for ease of interpretation: no IPV (79.1%) or one or more incidences of IPV (20.9%).
Lifetime Violence
Lifetime violence-related behaviors were assessed with a 5-item scale assessing the frequency of carrying a weapon (such as a gun, knife, or club), being threatened or injured with a weapon (such as a gun, knife, or club), threatening or injuring someone with a weapon (such as a gun, knife, or club), being in a physical fight, or being treated medically after a physical fight. Participants could select one of the following: zero times, one to two times, three to five times, six to nine times, 10 to 19 times, 20 to 39 times, 40 to 99 times, and 100 or more times. Prevalence rates were highly skewed, with the vast majority of respondents reporting either no history of violence or a number of incidents in the single digits. Thus, response options were collapsed for ease of interpretation into these categories: “none” (46.4%), “one to two incidents” (22.7%), and “three incidents or more” (30.9%) of lifetime violence-related behaviors.
Lifetime Number of Sexual Partners
Second, to assess the number of lifetime sexual partners participants were asked, “During your life, with how many people have you had sexual intercourse?” Response options were as follows: “No one,” “one to two,” “three to five”, “six to nine”, “10 to 19”, “20 to 39”, “40 to 99” and “100 or more people.” Responses were highly skewed, and for ease of interpretation were recoded into these categories: “one to two” (17.9%), “three to five” (31.2%), and “six or more” (50.8%) lifetime sex partners.
Number of Children
To assess the number of children, participants were asked, “How many children do you have (including stepchildren or adopted children)?” Response options were as follows: “None,” “one,” “two,” and “three or more.” Responses were highly skewed, and for ease of interpretation were recoded into these categories: “none” (73.9%), “one” (18.5%), and “two or more” (7.6%) children.
Level of Education
Participants were asked to select one option among several for the highest degree earned including: less than a high school diploma, high school diploma or equivalent, associate’s degree, bachelor’s degree, master’s degree, and a doctoral degree or equivalent. Education was recoded for ease of interpretation resulting in reference categories for “less than high school” (11.0%), “high school or equivalent” (55.2%), and “some college or more” (33.8%).
Religious Involvement
Participants were asked about the frequency of their religious service attendance and provided the following response options: “Rarely,” “never”, “once or twice per month,” and “about once per week or more.” Responses were collapsed and recoded for ease of interpretation resulting in reference categories for “never” (31.2%), “rarely” (35.8%), and “monthly or more” (33.0%).
Data Analysis
Data were analyzed using SPSS statistical software (Version 13.0, IBM) to examine the association between the risk and protective factors for IPV victimization. First, a series of χ2 analyses were conducted to assess bivariate relationships between predictor variables and IPV. Subsequently, we conducted a multivariate logistic regression in which all predictors were entered simultaneously. Only significant interaction terms were retained in the final multivariate logistic regression model as displayed in Table 1.
Table 1.
Results of Logistic Regression Analyses Predicting Intimate Partner Violence Victimization Among a Multiethnic Urban Sample of Young Adults.
| B | SE | Wald | df | Exp(B) | 95% C.I. for Exp(B) | |
|---|---|---|---|---|---|---|
| Lifetime violence | .78 | .11 | 53.62*** | 1 | 2.19 | 1.78–2.70 |
| Lifetime sexual partners | .70 | .14 | 24.29*** | 1 | 2.01 | 1.52–2.65 |
| Number of children | .79 | .16 | 23.19*** | 1 | 2.21 | 1.60–3.04 |
| Level of education | −.19 | .14 | 1.88 | 1 | .82 | .63–1.09 |
| Religious involvement | −.17 | .11 | 2.62 | 1 | .84 | .68–1.04 |
| Gender | −.86 | .19 | 20.38*** | 1 | .42 | .29–.62 |
| Interactions | ||||||
| Education × Children | −.64 | .25 | 6.38* | 1 | .53 | .32–.87 |
| Gender × Children | .62 | .21 | 8.58** | 1 | 1.85 | 1.23–2.80 |
Note: N = 1130. Exp (B) indicates the predicted odds of having experienced IPV with a one unit increase in the independent variable, controlling for other variables in the model.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Next, because we were interested in exploring whether the impact of risk and protective factors differed among women and men, we entered 2-way interaction terms between all other predictors and gender. We also computed separate multivariate logistic regression models separately for women and men. Lastly, we examined a 2-way interaction between number of children and level of education, as well as a 3-way interaction between these variables and gender. All predictor variables were centered to permit exploration of interaction effects.
Results
Main Effects
Lifetime Violence-Related Behaviors
Participants who reported more lifetime violence-related behaviors were significantly more likely to report IPV, χ2 (2) = 97.73, p < .001. Fifty-three (10.1%) participants who reported no violence-related behaviors also reported LPA, compared to 51 (19.9%) of those with one to two behaviors, and 132 (37.8%) with three or more instances. Lifetime violence-related behaviors remained statistically significant in the multivariate model (Table 1). Controlling for other variables in the model, the odds of IPV increased 2.19 times with each unit increase on the lifetime violence-related behaviors scale. For example, participants that reported 1 to 2 lifetime violence behaviors had 2.19 times greater odds of IPV than participants who reported no lifetime violence behaviors.
Lifetime Sex Partners
Participants with a greater number of lifetime sex partners were also significantly more likely to report IPV, χ2 (2) = 54.88, p < .001. Sixteen (8.3%) participants with one to two partners reported IPV, as did 50 (15.0%) with three to five partners, and 167 (30.7%) with six or more partners. Lifetime sexual partners retained statistical significance in the multivariate model (Table 1). Controlling for other variables in the model, the odds of IPV increased 2.01 times with each unit increase on the lifetime sexual partners scale. For example, participants who reported 6 or more lifetime sexual partners had 2.01 times greater odds of IPV than participants who reported three to five lifetime sexual partners.
Number of Children
Participants with more children were more likely to report IPV, χ2 (1) = 52.46, p < .001. Of the participants without children, 131 (15.7%) reported IPV, compared to 73 (34.9%) with one child, and 32 (37.2%) with two or more children. In the multivariate model, number of children remained statistically significant (Table 1). Controlling for other variables in the model, the odds of IPV increased 2.21 with each unit change in the number of children variable. For example, participants with two or more children were at 2.21 times greater odds of IPV than those with only one child.
Level of Education
Level of education was significantly related to IPV, χ2 (1) = 25.87, p < .001. Forty-one (33.3%) participants with less than a high school education, 143 (23.1%) with a high school degree or equivalent, and 51 (13.5%) with some college or more reported IPV. Education level was not statistically significant in the multivariate model (Table 1).
Religious Involvement
More frequent religious service attendance was significantly related to lower reports of IPV, χ2 (2) = 9.04, p < .05. Ninety-two (26.1%) of the participants who reported never attending services reported IPV, 79 (17.4%) who reported rarely attending services, and 65 (30.8%) who reported attending once time or more. Religious service attendance was not a significant predictor of IPV in the final model (Table 1).
Gender
Rates of intimate partner physical aggression were 21.9% and 19.5% among females and males, respectively. Although the differences were small, logistic regression results showed a significant main effect of gender, with greater likelihood of IPV victimization among women (Table 1).
Interaction Effects
We conducted a series of interactions between predictor variables and report significant effects below.
Education and Children
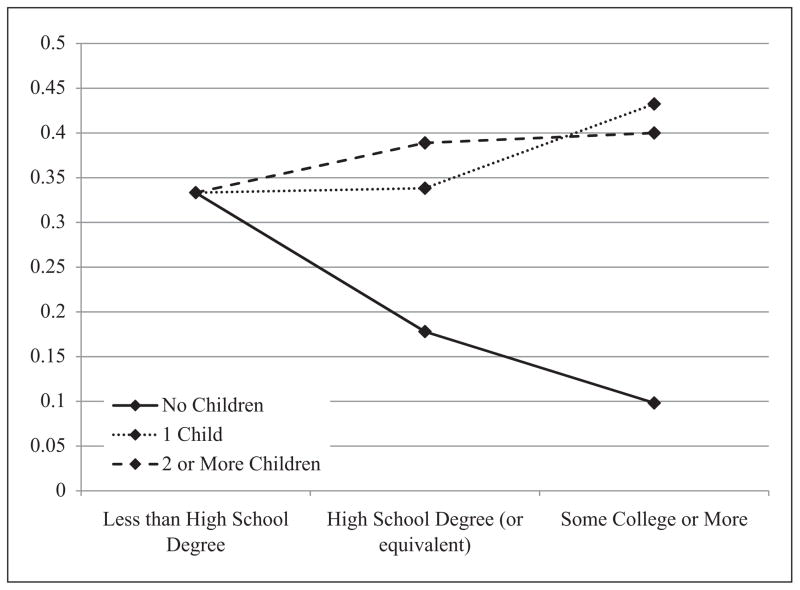
The 2-way interaction between number of children and level of education was statistically significant and retained in the final model (Table 1). As shown in Figure 1, higher education was significantly associated with reduced IPV risk. However, the protective effect of education was eliminated for young adults with children.
Figure 1.
Interaction between number of children and level of education
Note: Y axis represents percentage of participants reporting IPV. Controls for other variables in the model not included.
Gender and Children
The 2-way interaction with gender and number of children was statistically significant and retained in the final multivariate model (Table 1). Closer inspection showed that number of children was a significant predictor of IPV victimization for both women and men, but that having children was more strongly associated with IPV for women (β = .99, SE = .22, Walds χ2 (1) = 20.31, p < .001) compared to men (β = .57, SE = .26, Walds χ2 (1) = 4.66, p < .05).
Discussion
The present research examined risk and protective factors for intimate partner violence (IPV) victimization among a sample of predominantly ethnic minority young adults from low-income urban communities as research suggests they are at a high-risk for IPV (e.g., Foshee et al., 2009; Halpern et al., 2009). Environmental stressors (e.g., violence in the community, crime, and impoverished conditions), common in economically disadvantaged urban communities, may be particularly important in considering violence, including IPV. For example, biological models suggest that chronic stress results in the dysregulation of physiological systems implicated in the threat response (McEwen, 1998; Shonkoff, Boyce, & McEwen, 2009). Thus individuals may overrespond to even mild triggers, and misperceive threats in the environment. Indeed, in a small number of studies that have examined the relationship between IPV and stress (e.g., financial stress) suggest a strong link between the two (e.g., Smith, Murray, & Coker, 2010).
Consistent with research showing robust links between problem behaviors and general aggression/hostility with partner violence (e.g., Capaldi et al., 2012; O’Leary et al., 1989; Shorey et al., 2011) we found that lifetime violence was a major predictor of IPV victimization. Indeed, many studies suggest that risky and externalizing behaviors in adolescents and young adults are significant risk factors for IPV (e.g., Kim & Capaldi, 2004; Moffitt, Krueger, Caspi, & Fagan, 2000).
Number of lifetime sex partners also emerged as a significant risk factor for IPV victimization. This may reflect that having more partners increases the likelihood of experiencing at least one incidence of IPV. It may also be indicative of some underlying factor, such as impulsivity (which is related to risky sex). Although highly speculative, it may also be the case that in some cases sexual infidelity, jealousy, possessiveness may be a trigger for IPV, as reflected by a link between IPV and lifetime sex partners. On the other hand, it may be the case that young adults involved in relationships where IPV is present may choose to exit these relationships, thereby inflating the number of relationships and lifetime sex partners.
Consistent with previous findings, data from the present study showed that young adults with children were at increased risk for IPV. Consistent with a diathesis-stress model, having a child may increase stress and amplify other stressors (financial responsibilities, relationship conflicts) thus increasing the likelihood of IPV. Results from our interaction analyses showed that the association between having children and IPV victimization was stronger for women (vs. men). This is consistent with research showing that more than half of women experiencing IPV live with children under the age of 12 (DeJonghe, Bogat, Levendosky, & von Eye, 2008). Our results are also in line with data showing that economically disadvantaged pregnant women in their 20s are twice as likely to report IPV victimization (e.g., Gazmararian et al., 1996). As suggested in the introduction, having children may impose a constraint to exiting a relationship where IPV may be present. These findings are particularly relevant for interventions and policy as a means to provide focused attention and support to women with children as they may face strong barriers to exit relationships enduring IPV and as a way to reduce intergen-erational transmission of violence.
Although education level was significantly associated with IPV victimization it did not appear to be statistically significant in the multivariate model. Moreover, results from interaction analyses showed that the protective effect of education was eliminated for young adults with children. This interaction may be indicative of a diathesis stress model such that low levels of education limit employment prospects and opportunities (Singh, Darroch, & Frost, 2001), a stressor that is only amplified by the responsibility, financial costs, and barriers to exiting relationships that result from child rearing. Viewed another way, aspirations for higher education seem to be inversely related with decisions to marry and to have children at a young age (e.g., Clarridge, 1985; Hagan & Wheaton, 1993; Hogan & Astone, 1986). Indeed, data from five developed countries (Canada, France, Great Britain, Sweden, and the United States) found strong negative associations between level of education attained and having a child before age 20 (Singh, Darroch, & Frost, 2001). Although interesting, this finding was unexpected and thus replication and further examination is needed.
Religious involvement was significantly associated with IPV risk, with individuals reporting greater service attendance being at reduced risk. This is consistent with research showing that religiosity is significantly associated with lower levels of violence, including relationship violence (e.g., Nonnemaker et al., 2003). It may also reflect the social support afforded by being involved in a religious community, as social isolation is considered a risk factor for IPV (Dutton & Goodman, 2005). Although few studies have examined social support, the data suggest that it may linked with preventing IPV and post-traumatic stress disorder that is typically observed among IPV victims (Coker et al., 2002). These findings require further investigation as religious involvement did not retain significance in the multivariate model. However, they provide a seed for future investigation particularly in terms of the role of social support in buffering and preventing IPV victimization.
Finally, consistent with previous findings rates of IPV victimization were largely similar among males and females in the present sample, with slightly higher rates for females. While IPV is commonly thought of a problem that primarily affects women, the majority of research on IPV suggests about equal rates for males and females, although females incur more serious injuries (even death) as a result of IPV (e.g., Archer, 2000; review see Capaldi et al., 2012; Ehrensaft, Moffitt, & Caspi, 2004). Another notable finding was that the association between having children and IPV was stronger for women (relative to men) in the present study.
Implications
Intimate partner violence is a significant public health issue associated with serious issues for victims, families, and children witnessing family violence (e.g., Bonomi et al., 2007; Lawrence & Bradbury, 2001; Wolfe et al., 2011). The present study identified several risk factors associated with IPV victimization among a high-risk sample of young adults. Lifetime violence-related behaviors, number of sexual partners, and having children emerged as significant predictors of IPV.
Collectively, these results suggest that interventions might focus on violence, anger, and stress reduction as one means to prevent IPV. Some possibilities include providing skills training for coping with stress, anger, and anxiety (such as relaxation training). Research on general risk behaviors suggests that strong self-regulation is a critical factor for preventing IPV as it is robustly linked decreased use of substances and risky sex among adolescents and young adults (e.g., Fishbein et al., 2006; Griffin, Bang, & Botvin, 2010; Lowe, Acevedo, Griffin, & Botvin, 2012; Wills, Walker, Mendoza, & Ainette, 2006). Thus, interventions may also seek to provide individuals with skills to enhance self-regulatory capacities.
Our findings also showed that education level was protective of IPV, but the buffering effect was eliminated for young adults with children. These results suggest that prevention programs and policy-makers might focus on promoting safe sex and planned parenthood in combination with education efforts as a means to prevent IPV among young adults. The cumulative effects of number of children and limited education suggest that taking a multipronged approach to prevent risk behaviors might be fruitful.
Limitations
Although the present study adds to the body of knowledge on risk and protective factors for IPV among a high-risk population there are some limitations worth noting. First, although we specifically selected a sample classified as high risk (young adults of predominantly ethnic minority from low-income urban communities), this limits the extent to which the findings generalize to the larger population. Second, other study limitations concern the nature of data collection. For example, some of our key variables assessed lifetime violence and sex partners, which may result in some inaccuracy due to recollection errors or biases. In addition, due to the sensitive nature of some of the questions (which were assessed via telephone interviews) it is possible that there were some individuals who did not disclose or underreported some incidents. All of our measures were brief in order to reduce the response burden on participants. This may have resulted in oversimplification of our constructs, thus limiting the direct comparability to scale scores from the relevant literature. Another measurement concern is that lifetime violence-related behaviors were assessed with 5 items assessing the frequency of carrying a weapon, being threatened or injured with a weapon, threatening or injuring someone with a weapon, being in a physical fight, or being treated medically after a physical fight. Some of these responses may have included experiences of IPV, therefore inflating the association of lifetime violence with IPV. Although our study had several limitations, results were consistent with previous findings (including reviews and meta-analyses) suggesting a strong link between IPV and problem/violent/antisocial behaviors (e.g., Capaldi et al., 2012; Ehrensaft et al., 2003). Moreover, the present research was one of a few assessing IPV in a high-risk sample, thus providing strong indicators of key factors to be examined in future studies and implemented by program developers and policy-makers.
Conclusion
In the past decade a significant number of studies have examined risk factors associated with intimate partner violence. However, a relatively small number of studies have focused on high-risk populations. The present study represents a step forward in identifying key risk and protective factors among a sample of ethnic minority young adults from low-income urban communities. It is also a step forward in identifying key factors that may guide educators, program developers, and policy-makers to focus their efforts on stress reduction, self-regulation, education, and planned parenthood to prevent IPV in young adults.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by grants R01 DA016106 from the National Institute on Drug Abuse, National Institutes of Health.
Biographies
Bianca P. Acevedo, PhD, is a social psychologist specializing in interpersonal relationships and the neuroscience of love and attachment in humans. She is a researcher in the Department of Psychological and Brain Sciences at the University of California, Santa Barbara.
Sarah R. Lowe, PhD, is a postdoctoral fellow of Psychiatric Epidemiology at Columbia University. Her research focuses on psychological adaptation in the aftermath of traumatic events and over the transition to adulthood.
Kenneth W. Griffin, PhD, MPH, is professor in the Division of Prevention and Health Behavior, Department of Public Health, Weill Cornell Medical College. He has published extensively on the etiology and prevention of risk behaviors including alcohol, tobacco, and other drug use among children, adolescents, and young adults.
Gilbert J. Botvin, PhD, is professor emeritus, Division of Prevention and Health Behavior, Department of Public Health, Weill Cornell Medical College. He is nationally and internationally recognized for his work on drug abuse prevention and has published more than 200 scientific papers.
Footnotes
Reprints and permissions: sagepub.com/journalsPermissions.nav
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Archer J. Sex differences in aggression between heterosexual partners: A meta-analytic review. Psychological Bulletin. 2000;126:651–680. doi: 10.1037/0033-2909.126.5.651. [DOI] [PubMed] [Google Scholar]
- Bettencourt BA, Talley A, Benjamin AJ, Valentine J. Personality and aggressive behavior under provoking and neutral conditions: A meta-analytic review. Psychological Bulletin. 2006;132:751–777. doi: 10.1037/0033-2909.132.5.751. [DOI] [PubMed] [Google Scholar]
- Bhargava R, Temkin TL, Fireman BH, Eaton A, McCaw BR, Kotz KJ, Amaral D. A predictive model to help identify intimate partner violence based on diagnoses and phone calls. American Journal of Preventive Medicine. 2011;41:129–135. doi: 10.1016/j.amepre.2011.04.005. [DOI] [PubMed] [Google Scholar]
- Bonomi M, Anderson M, Rivera F, Thompson R. Health outcomes in women with physical and sexual intimate partner violence exposure. Journal of Women’s Health. 2007;16:987–997. doi: 10.1089/jwh.2006.0239. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Griffin KW, Nichols TR. Preventing youth violence and delinquency through a universal school-based prevention approach. Prevention Science. 2006;7:403–408. doi: 10.1007/s11121-006-0057-y. [DOI] [PubMed] [Google Scholar]
- Burch RL, Gallup GG., Jr Pregnancy as a stimulus for domestic violence. Journal of Family Violence. 2004;19:243–247. [Google Scholar]
- Campbell J, Jones A, Dieneman J, Kub J, Schollenberger J, O’Campo P, Wynne C. Intimate partner violence and physical health consequences. Archives of Internal Medicine. 2002;162:1157–1163. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Shortt JW, Kim HK. A life span developmental systems perspective on aggression toward a partner. In: Pinsof W, Lebow J, editors. Family psychology: The art of the science. New York, NY: Oxford University Press; 2005. pp. 141–167. [Google Scholar]
- Capaldi DM, Knoble NB, Shortt JW, Kim HK. A systematic review of risk factors for intimate partner violence. Partner Abuse. 2012;3:231–280. doi: 10.1891/1946-6560.3.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance—United States, 2001, Surveilance Summaries, 2002. Morbidity & Mortality Weekly Reports. 2001;51(SS04):1–64. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth Risk Behavior Surveilance—United States, 2001, Surveilance Summaries, 2006. Morbidity & Mortality Weekly Reports. 2005;55(SS05):1–108. [Google Scholar]
- Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance—United States, 2009. Surveillance Summaries, 2010. Morbidity & Mortality Weekly Reports. 2009;59(SS-5):1–142. [PubMed] [Google Scholar]
- Clarridge B. School completion and age at first marriage. University of Wisconsin; Madison, WI: 1985. Unpublised manuscript. [Google Scholar]
- Coker A, Davis K, Arias I, Deasai S, Sanderson M, Brandt H, Smith P. Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine. 2002;24:260–268. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- Coker A. Does physical intimate partner violence affect sexual health? A systematic review. Trauma, Violence, & Abuse. 2007;8:149–177. doi: 10.1177/1524838007301162. [DOI] [PubMed] [Google Scholar]
- Cunradi CB, Caetano R, Schafer J. Socioeconomic predictors of intimate partner violence among White, Black, and Hispanic couples in the United States. Journal of Family Violence. 2002;17:377–389. [Google Scholar]
- Davila YR, Brackley MH. Mexican and Mexican American women in a battered women’s shelter: Barriers to condom negotiation for HIV/AIDS prevention. Issues in Mental Health Nursing. 1999;20:333–355. doi: 10.1080/016128499248529. [DOI] [PubMed] [Google Scholar]
- DeJonghe ES, Bogat GA, Levendosky AA, von Eye A. Women survivors of intimate partner violence and post-traumatic stress disorder: Prediction and prevention. Journal of Postgraduate Medicine. 2008;54:294–300. doi: 10.4103/0022-3859.41435. [DOI] [PubMed] [Google Scholar]
- Dutton MA, Goodman LA. Coercion in intimate partner violence: Toward a new conceptualization. Sex Roles: A Journal of Research. 2005;52:743–756. [Google Scholar]
- Ehrensaft MK, Cohen P, Brown J, Smailes E, Chen H, Johnson JG. Intergenerational transmission of partner violence: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2003;71:741–753. doi: 10.1037/0022-006x.71.4.741. [DOI] [PubMed] [Google Scholar]
- Ehrensaft MK, Moffitt TE, Caspi A. Clinically abusive relationships and their developmental antecedents in an unselected birth cohort. Journal of Abnormal Psychology. 2004;113:258–271. doi: 10.1037/0021-843X.113.2.258. [DOI] [PubMed] [Google Scholar]
- Ellison N, Steinfield C, Lampe C. The benefits of Facebook “friends”: Exploring the relationship between college students’ use of online social networks and social capital. Journal of Computer-Mediated Communication. 2007;12:1143–1168. [Google Scholar]
- Fishbein DH, Herman-Stahl M, Eldreth D, Paschall MJ, Hyde C, Hubal R, Ialongo N. Mediators of the stress-substance use relationship in urban male adolescents. Prevention Science. 2006;7:113–126. doi: 10.1007/s11121-006-0027-4. [DOI] [PubMed] [Google Scholar]
- Foran H, O’Leary KD. Problem drinking, jealousy, and anger control: Variables predicting physical aggression against a partner. Journal of Family Violence. 2008;23(3):141–148. [Google Scholar]
- Foshee VA, Benefield T, Suchindran C, Ennett ST, Bauman KE, Karriker-Jaffe KJ, Mathias J. The development of four types of adolescent dating abuse and selected demographic correlates. Journal of Research on Adolescence. 2009;19:380–400. doi: 10.1111/j.1532-7795.2009.00593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox GL, Benson ML, DeMaris A, VanWyk J. Economic distress and intimate partner violence: Testing family stress and resource theories. Journal of Marriage and the Family. 2002;64:793–807. [Google Scholar]
- Gazamararian JA, Adams MM, Saltzman LE, Johnson CH, Bruce FC, Marks JS, Zahniser SC. The relationship between pregnancy intendedness and physical violence in mothers of newborns. The PRAMS Working Group. Obstetrics and Gynecology. 1995;85:1031–1038. doi: 10.1016/0029-7844(95)00057-x. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Lazorick S, Spitz AM, Ballard TJ, Saltzman LE, Marks JS. Prevalence of violence against pregnant women. Journal of the American Medical Association. 1996;275:1915–20. [PubMed] [Google Scholar]
- Griffin KW, Bang H, Botvin GJ. Age of alcohol and marijuana use onset and weekly substance use and related psychosocial problems during young adulthood. Journal of Substance Use. 2010;15:174–183. [Google Scholar]
- Hagan J, Wheaton B. The search for adolescent role exits and the transition to adulthood. Social Forces. 1993;71:955–980. [Google Scholar]
- Halpern CT, Spriggs AL, Martin SL, Kupper L. Patterns of intimate partner violence victimization from adolescence to young adulthood in a nationally representative sample. Journal of Adolescent Health. 2009;45:508–516. doi: 10.1016/j.jadohealth.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henning K, Connor-Smith J. Why doesn’t he leave? Relationship continuity and satisfaction among male domestic violence offenders. Journal of Interpersonal Violence. 2011;26:1366–1387. doi: 10.1177/0886260510369132. [DOI] [PubMed] [Google Scholar]
- Hogan DP, Astone NM. The transition to adulthood. Annual Review of Sociology. 1986;12:109–130. [Google Scholar]
- Huang CC, Son E, Wang LR. Prevalence and factors of domestic violence among unmarried mothers with a young child. Families in Society. 2010;91(2):171–177. [Google Scholar]
- Katz J, Kuffel SW, Coblentz A. Are there gender differences in sustaining dating violence? An examination of frequency and relationship satisfaction. Journal of Family Violence. 2002;17:247–271. [Google Scholar]
- Kelley HH, Thibaut JW. Interpersonal relations: A theory of interdependence. New York, NY: John Wiley & Sons; 1978. [Google Scholar]
- Kilpatrick KL, Williams LM. Post-traumatic stress disorder in child witnesses to domestic violence. American Journal of Orthopsychiatry. 1997;67:639–644. doi: 10.1037/h0080261. [DOI] [PubMed] [Google Scholar]
- Kim HK, Capaldi DM. The association of antisocial behavior and depressive symptoms between partners and risk for aggression in romantic relationships. Journal of Family Psychology. 2004;18:82–96. doi: 10.1037/0893-3200.18.1.82. [DOI] [PubMed] [Google Scholar]
- Lanier C, Maume MO. Intimate partner violence and social isolation across the rural/urban divide. Violence Against Women. 2009;15:1311–1330. doi: 10.1177/1077801209346711. [DOI] [PubMed] [Google Scholar]
- Lawrence E, Bradbury TN. Physical aggression as a predictor of marital dysfunction: A longitudinal analysis. Journal of Family Psychology. 2001;15:135–154. doi: 10.1037//0893-3200.15.1.135. [DOI] [PubMed] [Google Scholar]
- Lowe SR, Acevedo BP, Griffin KW, Botvin GJ. Longitudinal relationships between self-management skills and substance use in an urban sample of predominantly minority adolescents. Journal of Drug Issues. 2012 doi: 10.1177/0022042612462221. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney A, Pargament KI, Jewell T, Swank AB, Scott E, Emery E, Rye M. Marriage and spiritual realm: The role of proximal and distal religious constructs in marital functioning. Journal of Family Psychology. 1999;25:312–338. [Google Scholar]
- McCloskey L, Walker M. Post-traumatic stress in children exposed to family violence and single-event trauma. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(1):108–115. doi: 10.1097/00004583-200001000-00023. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- Melander LA, Noel H, Tyler KA. Bidirectional, unidirectional, and nonviolence: a comparison of the predictors among partnered young adults. Violence and Victims. 2010;25:617–630. doi: 10.1891/0886-6708.25.5.617. [DOI] [PubMed] [Google Scholar]
- Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, Silverman JG. Pregnancy coercion, intimate partner violence, and unintended pregnancy. Contraception. 2010;81:316–22. doi: 10.1016/j.contraception.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A. Annotation: implications of violence between intimate partners for child psychologists and psychiatrists. Journal of Child Psychology & Psychiatry. 1998;39:137–144. [PubMed] [Google Scholar]
- Moffitt TE, Krueger RF, Caspi A, Fagan J. Partner abuse and general crime: How are they the same? How are they different? Criminology. 2000;38:201–235. [Google Scholar]
- Nonnemaker JM, McNeely CA, Blum RW. Public and private domains of religiosity and adolescent health risk behaviors: evidence from the National Longitudinal Study of Adolescent Health. Social Science and Medicine. 2003;57:2049–2054. doi: 10.1016/s0277-9536(03)00096-0. [DOI] [PubMed] [Google Scholar]
- O’Donnell L, Stueve A, Myint-U A, Duran R, Agronick G, Wilson-Simmons R. Middle school aggression and subsequent intimate partner physical violence. Journal of Youth and Adolescence. 2006;35:693–703. [Google Scholar]
- O’Donnell L, Agronick G, Duran R, Myint-U A, Stueve A. Intimate partner violence among economically disadvantaged young adult women: associations with adolescent risk-taking and pregnancy experiences. Perspectives on Sexual and Reproductive Health. 2009;41(2):84–91. doi: 10.1363/4108409. [DOI] [PubMed] [Google Scholar]
- O’Leary KD, Barling J, Arias I, Rosenbaum A, Malone J, Tyree A. Prevalence and stability of physical aggression between spouses: A longitudinal analysis. Journal of Consulting and Clinical Psychology. 1989;57:263–268. doi: 10.1037//0022-006x.57.2.263. [DOI] [PubMed] [Google Scholar]
- O’Leary KD, Slep AM. A dyadic longitudinal model of adolescent dating aggression. Journal of Clinical Child and Adolescent Psychology. 2003;32:314–327. doi: 10.1207/S15374424JCCP3203_01. [DOI] [PubMed] [Google Scholar]
- Pallitto CC, Campbell JC, O’Campo P. Is intimate partner violence associated with unintended pregnancy? A review of the literature. Trauma, Violence, & Abuse. 2005;6:217–235. doi: 10.1177/1524838005277441. [DOI] [PubMed] [Google Scholar]
- Repetti R, Taylor S, Seeman T. Risky families: family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. [PubMed] [Google Scholar]
- Roberts AL, McLaughlin KA, Conron KJ, Koenen KC. Adult stressors, history of childhood adversity, and risk of perpetration of intimate partner violence among men and women. Am J Prev Med. 2011;40:128–138. doi: 10.1016/j.amepre.2010.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusbult CE. Commitment and satisfaction in romantic associations: A Test of The Investment Model. Journal of Experimental Social Psychology. 1980;16:172–186. [Google Scholar]
- Schaeffer HJ, Catling AD, Eblen ST, Collier LS, Krauss A, Weber MJ. MP1: An MEK binding partner that enhances enzymatic activation of the MAP kinase cascade. Science. 1998;281:1668–1671. doi: 10.1126/science.281.5383.1668. [DOI] [PubMed] [Google Scholar]
- Schumacher JA, Feldbau-Kohn S, Smith Slep AMS, Heyman RE. Risk factors for male-to-female partner physical abuse. Aggression and Violent Behavior. 2001;6:281–352. [Google Scholar]
- Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. The Journal of The American Medical Association. 2009;301:2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- Shorey RC, Brasfield H, Febres J, Stuart GL. The association between impulsivity, trait anger, and the perpetration of intimate partner and general violence among women arrested for domestic violence. Journal of Interpersonal Violence. 2011;26:2681–2697. doi: 10.1177/0886260510388289. [DOI] [PubMed] [Google Scholar]
- Singh S, Darroch JE, Frost JJ. Socioeconomic disadvantage and adolescent women’s sexual and reproductive behavior: The case of five developed countries. Family Planning Perspectives. 2001;33:251–289. [PubMed] [Google Scholar]
- Slep AM, O’Leary SG. Parent and partner violence in families with young children: Rates, patterns, and connections. Journal of Consulting and Clinical Psychology. 2005;73:435–444. doi: 10.1037/0022-006X.73.3.435. [DOI] [PubMed] [Google Scholar]
- Smith PH, White JW, Holand LJ. A longitudinal perspective on dating violence among adolescent and college-age women. American Journal of Public Health. 2003;93:1104–1109. doi: 10.2105/ajph.93.7.1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PH, Murray CE, Coker AL. The coping window: A contextual understanding of the methods women use to cope with battering. Violence and Victims. 2010;25(1):18–28. doi: 10.1891/0886-6708.25.1.18. [DOI] [PubMed] [Google Scholar]
- Straus DJ. Strategies in the treatment of Hodgkin’s disease. Seminars in Oncology. 1986;13(4 Suppl 5):26–34. [PubMed] [Google Scholar]
- Straus MA, Gelles RJ. Physical violence in American families. New Brunswick, NJ: Transaction Publishers; 1990. [Google Scholar]
- Teitelman AM, Ratcliffe SJ, Morales-Aleman MM, Sullivan CM. Intimate partner violence, condom use and HIV risk for adolescent girls: Gaps in the literature and future directions for research and intervention. Journal of HIV/ AIDS Prevention in Children and Youth. 2007;8:65–93. [Google Scholar]
- Tjaden P, Thoennes N. Full report of the prevalence, incidence, and consequences of violence against women survey: Research in brief. Washington, DC: National Institute of Justice; 2000. (NCJ18371) [Google Scholar]
- Vézina J, Hébert M. Risk factors for victimization in romantic relationships of young women: A review of empirical studies and implications for prevention. Trauma, Violence, & Abuse. 2007;8:33–66. doi: 10.1177/1524838006297029. [DOI] [PubMed] [Google Scholar]
- Wills TA, Walker C, Mendoza D, Ainette MG. Behavioral and emotional self-control: Relations to substance use in samples of middle and high school students. Psychology of Addictive Behaviors. 2006;20:265–278. doi: 10.1037/0893-164X.20.3.265. [DOI] [PubMed] [Google Scholar]
- Wolfe DA, Crooks CV, Chjodo D, Hughes R, Ellis W. Observations of adolescent peer resistance skills following a classroom-based healthy relationship program: A post-intervention comparison. Prevention Science. 2011;13(2):196–205. doi: 10.1007/s11121-011-0256-z. [DOI] [PubMed] [Google Scholar]