Abstract
China has experienced a transition from a history of undernutrition to a rapid increase in obesity. The China Health and Nutrition Survey, an ongoing longitudinal, household-based survey of urban and rural residents of nine provinces, documents these changes using measured height and weight across 53,298 observations from 18,059 participants collected from 1991 to 2011. Adult overweight (body mass index [BMI] ≥ 25 kilograms per square meter [kg/m2]) prevalence nearly tripled from 1991 (11.7%) to 2009 (29.2%), with significant cohort and age-related effects (stronger in males). Among youth, quantile regression reveals changes across the BMI distribution. By 2009 approximately 12% of children and adolescents were overweight, and 3% of 7–11 years old and 1% of 12–17 years old were obese (International Obesity Taskforce [IOTF] BMI 25 and 30 kg/m2 equivalents, respectively). In 1991–2000 urbanicity was strongly and positively associated with BMI, but in 2000–2011 trends were more similar across rural and urban areas. Among women, the burden has shifted to lower-educated women (the reverse is true for males, as overweight was higher in higher-educated men). Our findings highlight the importance of preventive measures early in the life cycle to reduce weight gain.
Keywords: China, obesity, adult, children, urbanicity, gender
INTRODUCTION
China presents a unique model for weight change, as the country has experienced a transition from a history of undernutrition to a very rapid increase in obesity.1, 2 While researchers have documented increases in body mass index (BMI) and overweight across China,3–6 there is considerable geographic and temporal heterogeneity in the timing of the transition from underweight to overweight across the country, thus providing variation in weight change by age, by area, and over time.7–11 Incidence of obesity-related noncommunicable diseases, such as diabetes, have recently increased, and those diseases are now the leading causes of morbidity, disability, and mortality in China.1, 12 For example, the prevalence of type 2 diabetes in China has more than doubled over the past two decades from approximately 3% in 1994 to 7–10% in 2008.13, 14 A recent meta-analysis suggests a stronger association between BMI and diabetes in younger versus older cohorts in Asia.15
Chinese modernization over the past 20 years has changed the economic landscape dramatically, with major increases in economic development and wealth.16 Patterns of adult and pediatric obesity in China now closely mirror similar patterns in the United States. As has been seen in low- and middle-income countries around the globe, economic development is soon followed by obesity, Pedwith disparities by socioeconomic status (SES).17, 18 This is true for China, where over one-fifth of adults are overweight and inactive and consume high quantities of caloric sweeteners, animal-source foods, and edible oils, with the poor shouldering the greatest burden of recent obesity.1, 19–25
For Chinese children, modernization has resulted in improvement in nutritional status with declines in underweight and stunting4, 26, 27 and a comparatively higher reduction in underweight relative to adults.4 Similar to the adult population, the Chinese pediatric population has experienced an increase in overweight, with younger cohorts experiencing comparatively higher BMIs at earlier ages than ever before. For example, in children aged 6 to 9 years the ninety-fifth cohort percentile increased BMI by 5 units from 1997 to 2006.28 Barry M. Popkin et al.29 showed that in the period from 1989 to 2004 absolute increases in overweight were higher among adults than children, yet when taking baseline weight into account, relative increases in overweight were higher among children than adults.
While overweight is clearly important, abdominal obesity is a particular issue for Asians, who are at higher cardiometabolic risk at lower BMI thresholds than other populations.30, 31 There is considerable evidence that abdominal obesity is an independent indicator of cardiometabolic risk, especially in individuals with normal BMI values.32–36 This is particularly true for Chinese adults, for whom abdominal obesity is a stronger predictor of coronary heart disease, diabetes, and metabolic syndrome than general obesity.31, 37–40 A recent study suggests screening for coronary heart disease, diabetes, and metabolic syndrome risk in China, where screening using BMI alone is estimated to miss a large proportion of the population at risk due to abdominal obesity but not general obesity.41
In this paper we use 20 years of longitudinal anthropometric data from the China Health and Nutrition Survey (CHNS) on more than 34,000 individuals in 288 communities throughout China across eight surveys from 1991 to 2011 to examine trends in BMI, overweight, and waist circumference (WC) over time. We give an example of age-period-cohort changes in BMIs using the CHNS data. We examine changes in WC relative to BMI to provide a sense of the changes in body shape over time. We provide examples of the differential patterning in change by SES and urbanicity to give a sense of how these changes relate to the wider social and economic changes accompanying modernization in China.
METHODS
As described in Bing Zhang et al.,42 the original survey in 1989 used a multistage, random cluster design to select a stratified probability sample with primary sampling units that were politically and geographically classified based on state statistical office definitions.43 Within each province, cities and counties were selected based on income, then communities were selected based on urbanicity, and then households were randomly selected for participation.44 In 2011 sampling in three Chinese megacities (Beijing, Shangai, and Chongqing) was added to the CHNS to enhance representation of the larger cities that have developed. Because these cities are only present at 2011, we present data on them separately and do not include them in trends analyses.
We present data on subsets of the total sample based on specific research questions. In general we limited eligibility to children between the ages of and 2 and 18 and adults between the ages of 18 and 66 to avoid age-related declines in weight due to sarcopenia.45 In addition participants had to have anthropometric data at each point for cross-sectional analyses or multiple measurement occasions for longitudinal analyses. At each visit height was measured without shoes to the nearest 0.2 centimeter (cm) using a portable Seca stadiometer, weight was measured without shoes and in light clothing to the nearest 0.1 kilogram (kg) on a calibrated beam scale, and WC was measured with a Seca tape measure. We use three sets of BMI cut points for adults to present overweight statistics using contrasting reference data for comparative purposes: (1) the World Health Organization (WHO) overweight BMI cut point, BMI ≥ 25 kilograms per square meter (kg/m2),46 (2) the Asian overweight BMI cut point, BMI ≥ 23 kg/m2,47 and (3) the Chinese overweight BMI cut point, BMI ≥ 24 kg/m2.48 For the presentation of pediatric overweight, we use the International Obesity Task Force (IOTF) cut points,49 which provide age- and sex-specific overweight classification at the BMI ≥ 25 kg/m2 equivalent and thus provide comparability with overweight classified using the adult BMI ≥ 25 kg/m2 cut point. In addition we use the Chinese age- and sex-specific BMI cut points for overweight, which are only produced for those 6 to 18 years old.50
Control variables
We present findings for BMI and WC by urbanicity status using a multicomponent continuous scale developed specifically for the CHNS (Jones-Smith and Popkin 2010). The urbanicity measure is described in detail elsewhere in this issue.42 In addition we present findings for BMI and WC by sex, age, household income, and attained educational status.
Statistical analyses
Descriptive and model-based analyses are described below relative to each set of results. All descriptive findings are age standardized using the Chinese 1990 census age distribution.
TRENDS OVER TIME
General descriptive statistics for the sample are shown in Table 1. Household income rose steadily over time. Urbanicity, as measured by the multicomponent urbanicity index, also increased over time.
Table 1.
Sample description, adults aged 18–65 in the CHNS cohort across survey years
| Survey year
|
||||||||
|---|---|---|---|---|---|---|---|---|
| 1991 | 1993 | 1997 | 2000 | 2004 | 2006 | 2009 | 2011* | |
| All Participants | ||||||||
| n | 7,804 | 7,349 | 7,621 | 8,296 | 7,710 | 7,520 | 7,779 | 7,269 |
| Male, % (SE)** | 47.6 ± 0.6 | 47.6 ± 0.6 | 48.5 ± 0.6 | 47.7 ± 0.5 | 47.8 ± 0.6 | 47.4 ± 0.6 | 47.3 ± 0.6 | 46.8 ± 0.6 |
| Age (years), mean (SE) | 38.1 ± 0.1 | 38.9 ± 0.1 | 40.0 ± 0.1 | 41.3 ± 0.1 | 43.7 ± 0.1 | 44.7 ± 0.1 | 45.4 ± 0.1 | 46.5 ± 0.1 |
| Household income (2009 yuan), mean (SE) | 16,587 ± 212 | 18,727 ± 247 | 20,998 ± 210 | 24,839 ± 275 | 2,993 ± 343 | 35,084 ± 542 | 49,821 ± 792 | 55,252 ± 738 |
| Community urbanicity,‡ mean (SE) | 46.1 ± 0.2 | 47.8 ± 0.2 | 52.6 ± 0.2 | 58.6 ± 0.2 | 62.2 ± 0.2 | 64.1 ± 0.2 | 66.9 ± 0.2 | 69.4 ± 0.2 |
Table does not include the three megacities added in 2011.
Standard error.
Urbanicity based on a 12-component urbanicity index (possible range 0–120) formed specifically for the CHNS 60.
While changes in mean BMI for adults aged 18 to 65 years were relatively small, ranging from 21.5 kg/m2 in 1991 to 22.9 kg/m2 in 2011, mean WC increased dramatically from 74.5 cm in 1993 to 78.3 cm in 2006 and to 80.5 cm in 2011 (Table 2). The increase in WC was particularly large in men, who gained on average 7.7 cm in WC from 1993 to 2006 compared to 4.5 cm among women. Mean annualized BMI gain was < 0.5 kg/m2/year across all years, with a sharp increase to 0.8 kg/m2/year in 2011.
Table 2.
Age-standardized* cross-sectional summary statistics, BMI, WC, and overweight, adults aged 18–65 in the CHNS cohort across survey years
| Survey year
|
||||||||
|---|---|---|---|---|---|---|---|---|
| 1991 | 1993 | 1997 | 2000 | 2004 | 2006 | 2009 | 2011† | |
| All Participants | ||||||||
| n | 7,804 | 7,349 | 7,621 | 8,296 | 7,710 | 7,520 | 7,779 | 7,269 |
| WC (cm) | — | 74.5 ± 0.1 | 76.0 ± 0.1 | 77.3 ± 0.1 | 78.3 ± 0.2 | 78.6 ± 0.2 | 79.7 ± 0.2 | 80.5 ± 0.2 |
| BMI (kg/m2) | 21.5 ± 0.0 | 21.6 ± 0.0 | 22.0 ± 0.0 | 22.3 ± 0.0 | 22.4 ± 0.0 | 22.5 ± 0.1 | 22.5 ± 0.1 | 22.9 ± 0.1 |
| BMI increase per year (BMI/yr) | — | 0.4 ± 0.0 | 0.3 ± 0.0 | 0.5 ± 0.0 | 0.3 ± 0.0 | 0.4 ± 0.1 | 0.5 ± 0.0 | 0.8 ± 0.2 |
| Overweight, WHO** | 10.4 ± 0.3 | 11.1 ± 0.1 | 14.9 ± 0.4 | 18.1 ± 0.4 | 19.2 ± 0.5 | 20.8 ± 0.6 | 22.4 ± 0.6 | 26.0 ± 0.1 |
| Overweight, Asia‡ | 16.0 ± 0.4 | 17.4 ± 0.4 | 21.8 ± 0.5 | 25.5 ± 0.5 | 27.1 ± 0.6 | 29.0 ± 0.7 | 31.0 ± 0.7 | 33.9 ± 0.1 |
| Overweight, China§ | 24.7 ± 0.5 | 25.7 ± 0.5 | 30.6 ± 0.6 | 36.1 ± 0.6 | 36.9 ± 0.7 | 39.4 ± 0.8 | 39.5 ± 0.8 | 44.0 ± 0.1 |
| Males | ||||||||
| n | 3,711 | 3,499 | 3,695 | 3,958 | 3,684 | 3,561 | 3,681 | 3,399 |
| WC (cm) | — | 75.5 ± 0.1 | 77.6 ± 0.2 | 79.4 ± 0.2 | 80.6 ± 0.2 | 81.3 ± 0.2 | 82.2 ± 0.3 | 83.2 ± 0.3 |
| BMI (kg/m2) | 21.3 ± 0.0 | 21.5 ± 0.0 | 21.8 ± 0.0 | 22.3 ± 0.1 | 22.4 ± 0.1 | 22.8 ± 0.1 | 22.8 ± 0.1 | 23.3 ± 0.1 |
| BMI increase per year (BMI/yr) | — | 0.2 ± 0.0 | 0.1 ± 0.0 | 0.2 ± 0.0 | 0.1 ± 0.0 | 0.2 ± 0.1 | 0.2 ± 0.0 | 0.5 ± 0.0 |
| Overweight, WHO** | 8.0 ± 0.4 | 9.3 ± 0.5 | 13.3 ± 0.6 | 17.9 ± 0.6 | 19.4 ± 0.8 | 23.4 ± 0.9 | 25.4 ± 1.0 | 30.2 ± 1.2 |
| Overweight, Asia‡ | 12.7 ± 0.5 | 14.5 ± 0.5 | 19.8 ± 0.7 | 25.2 ± 0.7 | 28.2 ± 0.9 | 32.2 ± 1.0 | 34.6 ± 1.1 | 39.4 ± 1.3 |
| Overweight, China§ | 20.9 ± 0.6 | 22.6 ± 0.7 | 28.9 ± 0.8 | 35.1 ± 0.8 | 38.7 ± 1.0 | 43.3 ± 1.1 | 43.4 ± 1.2 | 50.1 ± 1.4 |
| Females | ||||||||
| n | 4,093 | 3,850 | 3,926 | 4,338 | 4,026 | 3,959 | 4,098 | 3,870 |
| Age (years) | 37.9 ± 0.2 | 38.8 ± 0.2 | 40.3 ± 0.2 | 41.4 ± 0.2 | 43.7 ± 0.2 | 44.7 ± 0.2 | 45.4 ± 0.2 | 46.5 ± 0.2 |
| WC (cm) | — | 73.6 ± 0.1 | 74.5 ± 0.1 | 75.3 ± 0.2 | 76.1 ± 0.2 | 75.9 ± 0.2 | 77.3 ± 0.2 | 78.1 ± 0.3 |
| BMI (kg/m2) | 21.7 ± 0.0 | 21.7 ± 0.0 | 22.1 ± 0.1 | 22.3 ± 0.1 | 22.2 ± 0.1 | 22.2 ± 0.1 | 22.3 ± 0.1 | 22.6 ± 0.1 |
| BMI increase per year (BMI/yr) | — | 0.1 ± 0.0 | 0.1 ± 0.0 | 0.1 ± 0.0 | 0.1 ± 0.0 | 0.0 ± 0.0 | 0.1 ± 0.0 | 0.2 ± 0.0 |
| Overweight, WHO** | 12.5 ± 0.5 | 12.8 ± 0.5 | 16.4 ± 0.6 | 18.4 ± 0.6 | 18.9 ± 0.7 | 18.3 ± 0.7 | 20.0 ± 0.8 | 22.2 ± 0.9 |
| Overweight, Asia‡ | 19.0 ± 0.6 | 20.0 ± 0.6 | 23.7 ± 0.7 | 25.8 ± 0.7 | 25.9 ± 0.8 | 25.9 ± 0.9 | 27.7 ± 0.9 | 29.0 ± 0.9 |
| Overweight, China§ | 28.2 ± 0.7 | 28.7 ± 0.7 | 32.3 ± 0.8 | 37.2 ± 0.9 | 34.9 ± 1.0 | 35.8 ± 1.1 | 35.8 ± 1.0 | 38.6 ± 1.1 |
The age-standardized prevalence of overweight and obesity increased steadily among adults aged 18 to 65 from 1991 to 2011 regardless of whether the WHO, Asia, or Chinese reference was used (table 2). For example, using the WHO reference,46 overweight prevalence rose from 10.4% in 1991 to 18.1% in 2000 and to 26.0% in 2011. Using the China-specific reference,48 comparable overweight prevalence was 24.7% in 1991, 36.1% in 2000, and 44.0% in 2011. Overweight prevalence was higher in women than men in early survey years (e.g., using the WHO reference,46 12.5% for women versus 8.0% for men in 1991; 18.4% for women versus 17.9% for men in 2000), but after 2000 overweight prevalence was higher for men than women (e.g., 23.4% for men versus 18.3% for women in 2006; 30.2% for men versus 22.2% for women in 2011).
Similarly overweight rose steadily for children in the CHNS whether defined using the IOTF or the Chinese-specific cut points for overweight (Table 3). Looking at the full pediatric cohort, overweight prevalence according to the IOTF among children aged 2 to 18 years increased from 6.2% in 1991 to 8.5% in 2000 and to 15.4% in 2011. Using the Chinese-specific cut points, overweight rose from 6.3% in 1991 to 8.8% in 2000 and to 17.1% in 2011 among children aged 6 to 18 years. Among boys, overweight prevalence was comparatively higher in the younger age groups (2–6 and 6–11 years) in the earlier study years (1991 and 1993) and then became more comparable in 2011. Among girls, overweight was consistently higher in the younger age groups (2–6 and 6–11 years) than in the older age group (11–18 years). While overweight prevalence was similar in boys and girls 2 to 18 years old at baseline, prevalence by sex started to diverge in 1993, with boys having continuously higher prevalence at all follow-up exams. By 2011, according to the IOTF, overweight prevalence was 15.4% in girls and 17.1% in boys aged 2 to 18 years. Overweight for boys and girls aged 2 to 18 was lower in the three autonomous cities (the megacities) than in the nine provinces (table 3).
Table 3.
Age-standardized* cross-sectional summary statistics, BMI, WC, and overweight, children aged 2–18 years in the CHNS cohort across survey years
| Survey year
|
||||||||
|---|---|---|---|---|---|---|---|---|
| 1991 | 1993 | 1997 | 2000 | 2004 | 2006 | 2009 | 2011† | |
| Males | ||||||||
| 2–6 years old | n = 554 | n = 405 | n = 238 | n = 206 | n = 186 | n = 185 | n = 201 | n = 211 |
| WC (cm)* | — | 50.5 ± 0.4 | 51.0 ± 0.3 | 51.0 ± 0.4 | 50.7 ± 0.4 | — | — | — |
| BMI (kg/m2)* | 15.7 ± 0.1 | 15.9 ± 0.1 | 15.7 ± 0.1 | 15.7 ± 0.1 | 16.1 ± 0.2 | 15.9 ± 0.2 | 15.6 ± 0.1 | 16.9 ± 0.4 |
| Overweight, IOTF*‡ | 8.9 ± 1.3 | 16.1 ± 2.0 | 9.8 ± 2.1 | 10.9 ± 2.3 | 18.3 ± 3.3 | 14.9 ± 3.2 | 6.7 ± 1.7 | 15.5 ± 2.9 |
| 6–11 years old | n = 593 | n = 636 | n = 587 | n = 403 | n = 281 | n = 290 | n = 286 | n = 273 |
| WC (cm)* | — | 56.2 ± 0.5 | 56.9 ± 0.3 | 57.4 ± 0.3 | 58.3 ± 0.5 | 57.2 ± 0.6 | 59.1 ± 0.6 | 60.1 ± 0.9 |
| BMI (kg/m2)* | 15.8 ± 0.1 | 15.8 ± 0.1 | 16.2 ± 0.1 | 16.5 ± 0.1 | 16.6 ± 0.2 | 16.6 ± 0.2 | 16.7 ± 0.2 | 17.2 ± 0.3 |
| Overweight, IOTF*‡ | 6.4 ± 1.2 | 6.7 ± 1.2 | 8.5 ± 1.2 | 10.2 ± 1.7 | 13.6 ± 2.5 | 16.1 ± 2.6 | 17.0 ± 2.6 | 18.2 ± 3.1 |
| Overweight, China*§ | 7.9 ± 1.3 | 8.6 ± 1.3 | 10.7 ± 1.4 | 13.9 ± 1.9 | 16.5 ± 2.7 | 19.7 ± 2.8 | 19.8 ± 2.7 | 20.5 ± 3.2 |
| 11–18 years old | n = 800 | n = 724 | n = 724 | n = 854 | n = 537 | n = 358 | n = 336 | n = 279 |
| WC (cm)* | — | 65.5 ± 0.3 | 66.1 ± 0.3 | 67.3 ± 0.3 | 68.4 ± 0.4 | 69.6 ± 0.5 | 69.1 ± 0.5 | 71.3 ± 0.7 |
| BMI (kg/m2)* | 18.2 ± 0.0 | 18.4 ± 0.1 | 18.5 ± 0.1 | 18.7 ± 0.1 | 18.9 ± 0.1 | 19.0 ± 0.1 | 19.1 ± 0.2 | 19.7 ± 0.2 |
| Overweight, IOTF*‡ | 3.1 ± 0.6 | 4.5 ± 0.8 | 4.2 ± 0.8 | 6.5 ± 0.9 | 7.4 ± 1.1 | 8.2 ± 1.5 | 11.4 ± 1.7 | 15.8 ± 2.4 |
| Overweight, China*§ | 3.6 ± 0.7 | 5.5 ± 0.9 | 6.5 ± 0.9 | 7.6 ± 1.0 | 8.9 ± 1.2 | 9.8 ± 1.6 | 12.6 ± 1.8 | 19.3 ± 2.5 |
| Females | ||||||||
| 2–6 years old | n = 473 | n = 354 | n = 176 | n = 191 | n = 142 | n = 152 | n = 168 | n = 181 |
| WC (cm)* | — | 49.4 ± 0.6 | 49.7 ± 0.5 | 49.6 ± 0.5 | 49.4 ± 0.7 | — | — | — |
| BMI (kg/m2)* | 15.4 ± 0.1 | 15.6 ± 0.1 | 15.6 ± 0.1 | 15.3 ± 0.1 | 15.6 ± 0.1 | 15.3 ± 0.2 | 15.9 ± 0.2 | 16.4 ± 0.4 |
| Overweight, IOTF*‡ | 9.6 ± 1.6 | 12.4 ± 1.9 | 11.3 ± 2.7 | 11.8 ± 2.6 | 13.7 ± 3.3 | 8.9 ± 2.1 | 20.6 ± 3.6 | 19.0 ± 3.6 |
| 6–11 years old | n = 534 | n = 542 | n = 521 | n = 379 | n = 259 | n = 235 | n = 211 | n = 248 |
| WC (cm)* | — | 54.9 ± 0.5 | 55.5 ± 0.3 | 56.0 ± 0.3 | 55.7 ± 0.5 | 55.2 ± 0.6 | 56.2 ± 0.6 | 56.9 ± 0.8 |
| BMI (kg/m2)* | 15.4 ± 0.1 | 15.6 ± 0.1 | 15.8 ± 0.1 | 16.0 ± 0.1 | 16.2 ± 0.2 | 16.3 ± 0.2 | 16.2 ± 0.3 | 16.0 ± 0.3 |
| Overweight, IOTF*‡ | 4.9 ± 1.0 | 6.5 ± 1.3 | 7.7 ± 1.4 | 9.4 ± 1.7 | 14.4 ± 2.6 | 13.1 ± 2.7 | 15.1 ± 3.1 | 10.4 ±1.9 |
| Overweight, China*§ | 7.2 ± 1.2 | 7.7 ± 1.3 | 10.7 ± 1.6 | 11.7 ± 1.8 | 16.8 ± 2.7 | 16.8 ± 2.9 | 16.3 ± 3.1 | 12.5 ± 2.0 |
| 11–18 years old | n = 785 | n = 678 | n = 663 | n = 723 | n = 468 | n = 339 | n = 282 | n = 254 |
| WC (cm)* | — | 64.6 ± 0.3 | 65.0 ± 0.3 | 65.3 ± 0.3 | 66.0 ± 0.4 | 65.4 ± 0.4 | 66.3 ± 0.5 | 68.2 ± 0.6 |
| BMI (kg/m2)* | 18.7 ± 0.1 | 18.5 ± 0.1 | 18.7 ± 0.1 | 18.7 ± 0.1 | 18.9 ± 0.1 | 18.6 ± 0.1 | 19.1 ± 0.2 | 19.3 ± 0.2 |
| Overweight, IOTF*‡ | 3.5 ±1.0 | 3.1 ± 1.0 | 3.5 ± 0.7 | 3.5 ± 0.7 | 4.5 ± 1.0 | 5.3 ± 1.3 | 7.8 ± 1.7 | 9.3 ± 1.9 |
| Overweight, China*§ | 5.3 ± 0.8 | 3.9 ± 0.8 | 5.0 ± 0.9 | 4.5 ± 0.8 | 7.1 ± 1.2 | 6.3 ± 1.3 | 8.5 ± 1.8 | 11.7 ± 2.1 |
| All participants, total sample, aged 2–18, IOTF‡ | ||||||||
| Male | n = 1,947 | n = 1,765 | n = 1,549 | n = 1,463 | n = 1,004 | n = 833 | n = 823 | n = 763 |
| Overweight, IOTF*‡ | 6.2 ± 0.5 | 8.7 ± 0.7 | 7.9 ± 0.7 | 9.6 ± 0.9 | 11.6 ± 1.0 | 12.3 ± 1.1 | 12.1 ± 1.2 | 17.1 ± 1.5 |
| Female | n = 1,792 | n = 1,574 | n = 1,360 | n = 1,293 | n = 869 | n = 726 | n = 661 | n = 683 |
| Overweight, IOTF*‡ | 6.2 ± 0.6 | 7.4 ± 0.7 | 6.7 ± 0.8 | 7.2 ± 0.8 | 10.9 ± 1.1 | 9.4 ± 1.1 | 12.2 ± 1.3 | 13.7 ± 1.4 |
| Total | n = 3,739 | n = 3,339 | n = 2,909 | n = 2,756 | n = 1,873 | n = 1,559 | n = 1,484 | n = 1,446 |
| Overweight, IOTF*‡ | 6.2 ± 0.4 | 8.1 ± 0.5 | 7.3 ± 0.5 | 8.5 ± 0.6 | 11.3 ± 0.8 | 10.9 ± 0.8 | 12.1 ± 0.9 | 15.4 ± 1.0 |
| All participants, total sample, aged 6–18, China§ | ||||||||
| Male | n = 1,393 | n = 1,360 | n = 1,311 | n = 1,257 | n = 818 | n = 648 | n = 622 | n = 552 |
| Overweight, China*§ | 5.5 ± 0.6 | 7.4 ± 0.7 | 9.1 ± 0.8 | 9.9 ± 0.9 | 12.6 ± 1.2 | 13.8 ± 1.4 | 15.0 ± 1.5 | 19.8 ± 1.9 |
| Female | n = 1,319 | n = 1,220 | n = 1,184 | n = 1,102 | n = 727 | n = 574 | n = 493 | n = 502 |
| Overweight, China*§ | 7.0 ± 0.7 | 6.3 ± 0.7 | 7.6 ± 0.8 | 7.5 ± 0.9 | 12.3 ± 1.3 | 10.4 ± 1.3 | 12.1 ± 1.6 | 14.2 ± 1.7 |
| Total | n = 2,712 | n = 2,580 | n = 2,495 | n = 2,359 | n = 1,545 | n = 1,222 | n = 1,115 | n = 1,054 |
| Overweight, China*§ | 6.3 ± 0.5 | 6.9 ± 0.5 | 8.4 ± 0.6 | 8.8 ± 0.6 | 12.4 ± 0.9 | 12.2 ± 0.9 | 13.7 ± 1.0 | 17.1 ± 1.3 |
Age standardized to the 1990 Chinese population.
Table does not include the three megacities added in 2011.
Overweight classified using the IOTF age- and sex-specific BMI ≥ 25 kg/m2 equivalent 49.
Overweight classified using the Chinese age- and sex-specific cut points for Chinese children aged 6–18 years 50. Note: Chinese cut points are not produced for children < 6 years of age.
We contrast overweight incidence between 1991 and 2000 relative to that between 2000 and 2011 by age and sex in Table 4. In this table we present the number of new unique cases of overweight between 1991 and 2000 and between 2000 and 2011. Among adults, 15.3% of the cohort became overweight between 1991 and 2000, whereas 25.4% became overweight between 2000 and 2011. The increase in new overweight cases between 2000 and 2011 in the pediatric cohort was dramatic. Among children, 5.1% of the pediatric cohort became overweight between 1991 and 2000, whereas 14.5% became overweight between 2000 and 2011. Overweight incidence was considerably higher in boys than in girls across all age groups.
Table 4.
Age-standardized* incident overweight (new cases between 1991 and 2000 and between 2000 and 2011) across two decades in the CHNS
| 1991–2000 | 2000–2011† | |
|---|---|---|
| Adults aged 18–65‡ | ||
| Men | 14.7 ± 1.1 | 27.4 ± 2.8 |
| Women | 15.2 ± 1.2 | 21.3 ± 5.7 |
| Total | 15.3 ± 0.8 | 25.4 ± 2.5 |
| Children aged 2–6§ | ||
| Boys | 3.0 ± 0.7 | 9.4 ± 4.0 |
| Girls | 1.4 ± 0.5 | 7.3 ± 3.5 |
| Total | 2.3 ± 0.4 | 8.3 ± 2.7 |
| Children aged 6–11§ | ||
| Boys | 0.6 ± 0.3 | 16.6 ± 6.1 |
| Girls | 1.0 ± 0.4 | 4.1 ± 4.0 |
| Total | 0.8 ± 0.2 | 11.5 ± 3.9 |
| Children aged 11–18§ | ||
| Boys | 4.2 ± 1.0 | 23.8 ± 3.5 |
| Girls | 9.2 ± 3.4 | 8.2 ± 3.5 |
| Total | 4.5 ± 0.0 | 19.2 ± 2.7 |
| All Children aged 2–18§ | ||
| Boys | 4.9 ± 0.9 | 18.7 ± 2.5 |
| Girls | 6.6 ± 2.0 | 6.7 ± 2.1 |
| Total | 5.1 ± 0.8 | 14.5 ± 1.7 |
Age standardized to the 1990 Chinese population.
Table does not include the three megacities added in 2011.
WHO overweight BMI cut point, BMI ≥ 25 kg/m2 46.
Overweight classified using the IOTF age- and sex-specific BMI ≥ 25 kg/m2 equivalent 49. Incident cases defined as nonoverweight at baseline and became overweight in the two decades 1991–2000 and 2000–2011.
It is of great interest to compare overweight in the megacities added in 2011 relative to the rest of the CHNS 2011 sample. In these three autonomous cities, cross-sectional overweight prevalence was comparatively higher than the rest of the 2011 CHNS cohort (Table 5). Among adults, overweight was highest in men from Beijing (44%) and was higher in men than women in Beijing and Shanghai but was higher in women than men in Chongqing. Similarly pediatric overweight was comparatively higher in Beijing than in Shanghai and Chongqing. However, male-female differences were greater in Beijing and Chongqing.
Table 5.
Age-standardized* overweight prevalence in the megacities, CHNS 2011
| Beijing | Shanghai | Chongqing | Total | |
|---|---|---|---|---|
| n = 1,190 | n = 1,295 | n = 1,183 | n = 3,668 | |
| Adult men‡ | 44.0 ± 5.3 | 34.8 ± 3.1 | 20.6 ± 2.9 | 34.3 ± 2.0 |
| Adult women‡ | 29.3 ± 2.0 | 20.7 ± 3.1 | 29.4 ± 4.3 | 26.0 ± 1.8 |
| Total adults‡ | 34.6 ± 2.4 | 27.1 ± 2.1 | 25.0 ± 2.4 | 29.6 ± 1.3 |
| Boys aged 2–18§ | 12.3 ± 3.3 | 5.4 ± 2.2 | 9.8 ± 2.9 | 9.3 ± 1.6 |
| Girls aged 2–18§ | 8.5 ± 3.3 | 5.2 ± 2.1 | 2.6 ± 1.1 | 5.1 ± 1.2 |
| Total aged 2–18§ | 10.5 ± 2.3 | 5.2 ± 1.5 | 6.2 ± 1.5 | 7.2 ± 1.0 |
AGE, PERIOD, COHORT EFFECTS
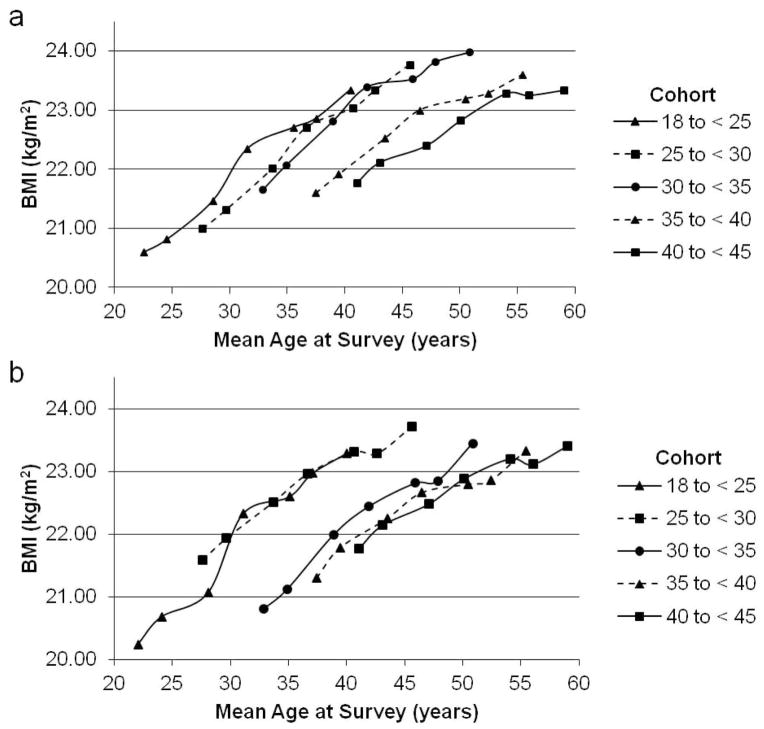
While the cross-sectional trends in BMI and overweight by CHNS survey year clearly show a dramatic increase in weight over time, the cohort is also aging. Thus it is essential to disentangle the aging and period effects over time to fully understand these temporal trends. Lindsay. M. Jaacks et al.51 examined age-period-cohort effects to determine whether increases in BMI over time related to changes across cohorts and periods were independent of age. To do so the authors used a series of mixed effects models with fixed and random individual-level effects and random slopes to assess differences in BMI in individuals over time (age effect) and population-wide differences in BMI over time (period effect) whether differences in the period effect varied across age cohorts in a complete-case subgroup analysis (n = 1,269) seen at all survey years. Jaacks et al.51 found a nonlinear increase in BMI with age and evidence of a strong cohort effect (Figure 1). For example, at any given age later birth cohorts (e.g., baseline age 18 to < 25 years) had higher mean BMIs than earlier birth cohorts (e.g., 40 to < 45 years at baseline). In other words, at age 40 men and women from later birth cohorts were over 1.5 BMI units heavier than men and women from earlier birth cohorts. This translates to a difference of 7 kg in men and 6 kg in women for the 40-year-old of average height (men 169 cm; women 159 cm). This cohort effect is troublesome given that Chinese children are at even higher BMIs than the adults discussed here.
Figure 1.
BMI across all seven surveys stratified by baseline age group (cohort) in males (top panel) and females (bottom panel)
BODY MASS INDEX TRAJECTORIES
Most research on temporal trends in BMI uses repeated cross-sectional or longitudinal BMI data rather than summary measures of trajectories over time that can be used to identify differential tempo and timing of weight gain. While there are many methods for identifying trajectories, latent class trajectory analysis (LCTA) has only recently been used in epidemiological data52 to classify individuals into distinct groups with similar underlying trajectories.53–55 We used LCTA modeling in SAS version 9.2 (SAS Institute, Cary, NC) with the TRAJ procedure using the censored normal model (CNORM)56, 57 to derive weight change trajectories, allowing for a variety of different order polynomials to determine the best fit. The best-fitting models were chosen based on lowest Bayesian information criteria, a goodness of fit criterion for comparing model fit and parsimony across models regardless of their underlying distribution, and at least 2% of the sample size within each trajectory class. Figure 2 shows the shape of the latent class weight trajectory curves by sex, with separate colors indicating each weight trajectory class.
Figure 2.
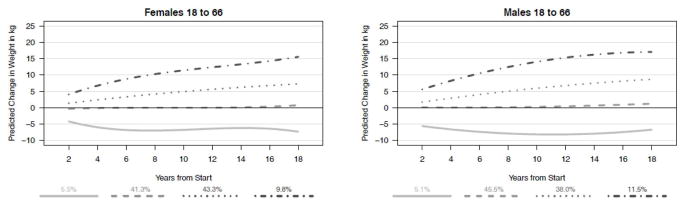
Weight gain trajectories for adults aged 18–66 years, 1991 to 2009, CHNS, derived using latent class trajectory analysis
There were four weight trajectory classes for males and females, two weight gain classes (the top two curves), one weight stable class (the dashed line), and one smaller class for individuals with maintenance of weight loss (the solid line). For females, the largest classes were the weight stable and moderate weight gain classes, approximately 40% each, and a smaller proportion was in the high weight gain and maintenance of weight loss classes. For males, the largest class was the weight stable class, but large proportions were in both weight gain classes: 11.5% in the high weight gain class and 38.0% in the moderate weight gain class. Thus overall approximately half of males and females fell into weight gain classes.
Using generalized linear mixed models, Lauren Paynter et al.58 examined baseline predictors of weight trajectories and found that baseline weight status was highly predictive of weight trajectory class membership for men and women. Baseline urbanicity was negatively associated with membership in the slower weight gain trajectory for women. However, baseline urbanicity was not statistically associated with the upward weight gain trajectories in women (and was associated with none of the classes in men), suggesting lack of differences in weight gain across the full scope of urbanicity.
CHANGES IN WAIST CIRCUMFERENCE RELATIVE TO BODY MASS INDEX
Dalia Stern et al.59 examined the proportional increase in WC relative to BMI from 1993 to 2009, finding that each unit increase in BMI was associated with a 3.22 cm (95% confidence interval [CI]: 2.91, 3.54, p < 0.05) and a 2.05 cm (95% CI: 1.76, 2.35, p < 0.05) higher WC between 1993 and 2009 for males and female, respectively. Thus even at equivalent BMIs, on average the more recent CHNS participants had higher WCs than their counterparts from 1993. Furthermore, as shown in Figure 3, the proportional increase in WC was higher in obese versus lean participants. For example, at BMI = 18.5 kg/m2 in 1993 and 2009, males had a 2.8 cm (and females a 1.5 cm) larger WC than their counterparts at the 2009 visit. However, at BMI = 28 kg/m2 in 1993 and 2009, males had a 3.9 cm (and females a 2.9 cm) larger WC than their counterparts at the 2009 visit.
Figure 3.
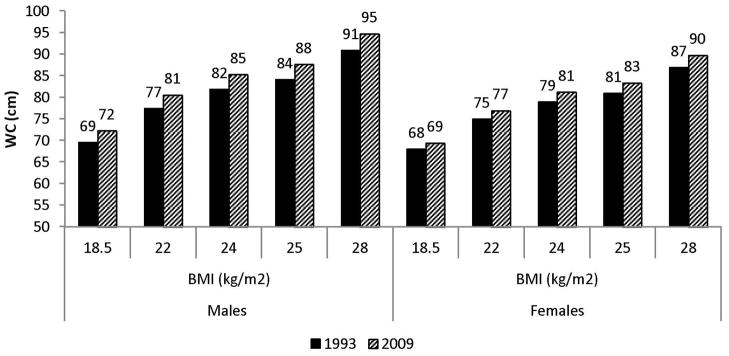
Predicted mean WC (cm) for given BMI using linear regression in Chinese men and women aged 20–59 years in 1993 compared with 2009, CHNS
URBANICITY AND EDUCATION EFFECTS
Jesse C. Jones-Smith et al.60 examined incident overweight and obesity from 1991 to 2004 for the subset of the women who had BMIs measured at both points, finding that the odds of overweight were significantly higher for women in communities with greater baseline and change in urban scores compared to those in the least urban communities that did not change in urbanicity. We ran the same analysis for women but for the period from 1991 to 2011 (Figure 4), finding that for women living in communities with a low initial urbanicity score (~ 30), a higher level of change in urban score over the follow-up years (versus no change) was associated with higher incident overweight. However, in the midrange initial urbanicity score (40, 50) there was little difference in incident overweight associated with change in urbanicity from 1991 to 2011. For women with high baseline urbanicity scores (60, 70), greater increase in urbanicity (i.e., change of 30 points on the scale, or communities with relatively greater change over time) was associated with lower overweight incidence. Thus change in urbanicity over time was positively associated with overweight incidence in communities initially at low levels of urbanicity. But in the middle range of baseline urbanicity there was overall higher obesity incidence but little difference with the temporal changes in urbanicity in those communities. However, in communities that were already more urbanized at baseline, greater change in urbanicity over time was associated with lower overweight incidence. Of note, the three megacities are not included in this incident overweight analysis as they were only sampled in 2011. Recall that we see higher cross-sectional overweight in the three megacities (Table 5) relative to the provinces assessed in 2011 for adults according to the WHO classification (table 2) and for children aged 2 to 18 (table 3) according to the IOTF classification.
Figure 4.
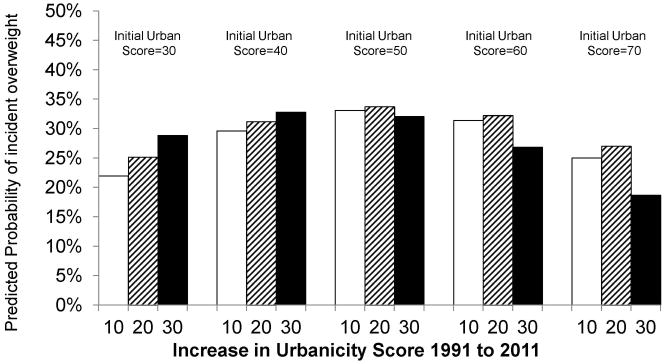
Predicted incident overweight* across different combinations of baseline urbanicity and increase in urbanicity, 1991 to 2011
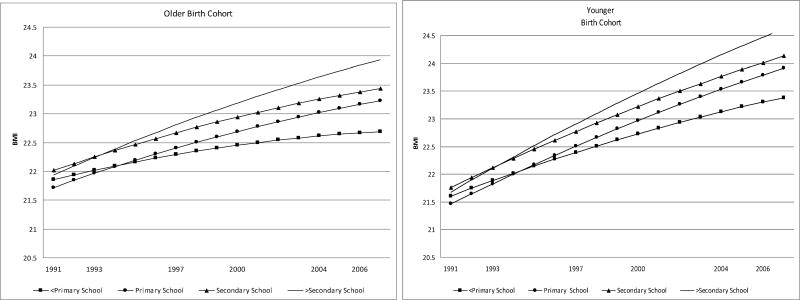
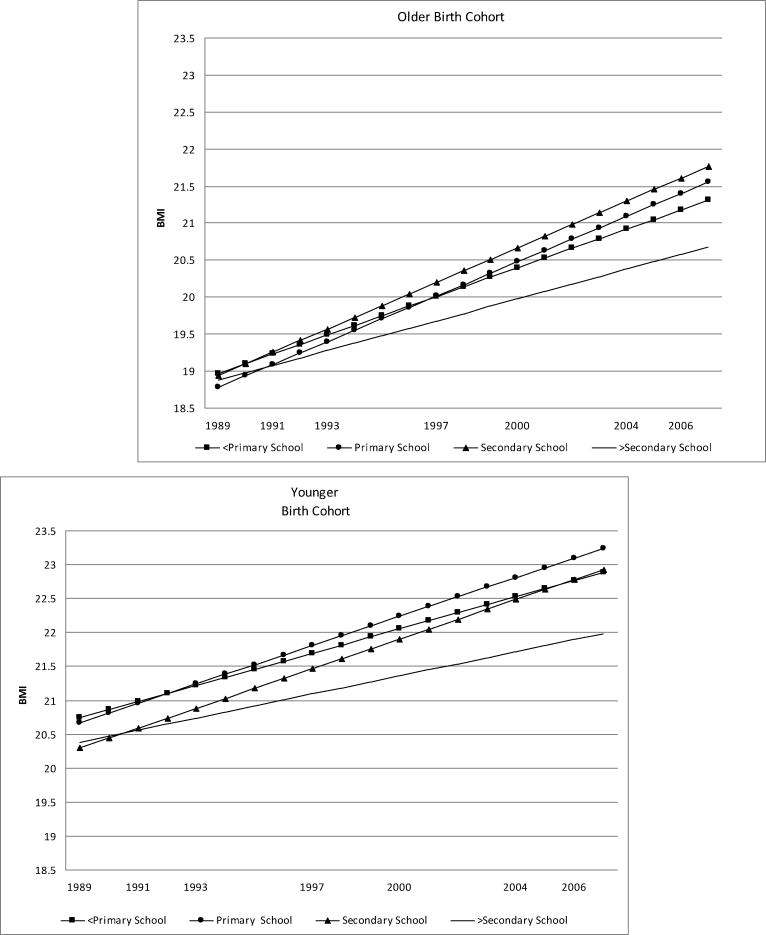
Jones-Smith et al.61 examined trends in overweight in relation to educational attainment in the CHNS from 1989 to 2006 using sex-stratified, random-effects models to estimate the associations for low (< primary school) versus high (> secondary school) eucational attainment and interactions by birth cohort. Model results suggest comparatively higher BMI increases over time for women of lowest education. Estimated weight gains (based on a female of average height [156 cm]) with an initial BMI of 22 for the highest-educated women was 0.19 kg/year or 3.31 kg over the 17-year period compared to that for the least-educated women, who had 0.27 kg/year or 4.54 kg over the 17-year period. The reverse trend is seen for men. At baseline there were no differences in overweight by educational attainment. However, by 2006 the odds of overweight were over threefold higher (odds ratio [OR] = 3.4; CI: 1.82, 6.18) for men at the highest education versus those at the lowest.
In Figure 5 we present BMI trajectories for men and women from 1989 to 2006 by educational attainment and birth cohort (older cohort born before 1955, younger cohort born after 1955) from Jones et al.61 The older birth cohort of women (top left panel) had comparatively lower BMIs than the older cohort across time. Yet among both birth cohorts, the women of highest education had a lower rate of increase in BMI compared to the other educational groups, which resulted in a widening educational disparity in BMIs over time. Trends for men were quite different. Initial BMI was comparatively higher for the older cohort, but the younger cohort had a more rapid increase in BMI over time. BMI was comparatively higher among the more higly educated men versus the less educated.
Figure 5.
Predicted BMI trajectories for men (top panel) and women (bottom panel) by birth cohort (older birth cohort born in or prior to 1955; younger birth cohort born after 1955), 1989–2006
CONCLUSION
Our findings suggest that the rise in overweight in China continues its upward trajectory. Using 20 years of data from the CHNS, we have shown a doubling of overweight prevalence and incidence and substantial temporal increases in WC across all age groups. The fact that we see the higher burden of these temporal increases in overweight in the younger age cohorts is particularly worrisome, as children are entering the adult years at higher body weights and higher WCs than in previous generations. Furthermore the observed higher WCs at all BMIs forebodes greater cardiometabolic risk at lower BMI levels. These changes are ubiquitous, as we see these increases in rural areas and even among the poor, and suggest substantial health care costs particularly to disadvantaged and rural segments of China. At the same time the cross-sectional data for the three megacities (Beijing, Shangai, and Chongqing) suggest extraordinarily high adult overweight.
Rates of obesity-related chronic diseases are already having a dramatic impact in China.14, 62–65 These changes will no doubt put a further drain on the health care system in China and will increase chronic disease–related economic costs.66–69 Recent findings from the Global Burden of Diseases, Injuries, and Risk Factors Study show that the leading causes of death in 2010 were stroke (with 1.7 million deaths), ischemic heart disease, and chronic obstuctrive pulmonary disease (the last two with just under 1 million deaths each), and dietary risk factors and high blood pressure contribute the largest number of attributable disability-adjusted life years.12, 70
Urbanicity and modernization have played a key role in the changes in disease patterns seen in China. China’s history of undernutrition has been followed by a rapid increase in obesity and related diseases, with differential rates across rural and urban areas.1, 2, 71 In the last decade changes in diet and activity in China have occurred more rapidly than previously recorded for any country1 and have included increased intake of edible oils, fried foods, animal-source foods, and snacking as well as declining occupational, domestic, and travel activity and increasing TV time.72–75 It is clear that these changes in lifestyle throughout China are playing a role in the observed increases in overweight reported here. With much higher increases in overweight among more rural areas and among the poor, access to health care for these subpopulations becomes an even greater challenge for China.
The changes that have occurred have had differential effects on segments of the Chinese population. Our updated analysis of the original Jones-Smith paper60 suggests that over time we now see the increases in overweight extending equally to less urbanized areas. Increases in obesity in even rural and poor areas of China mean that all segments of Chinese society are impacted by the changes in lifestyle, obesity, and chronic diseases. As we have shown here, women of low SES bear the greatest burden of overweight among women, whereas the converse is seen for men (higher overweight among high SES men). Overweight prevention and screening for overweight as well as for high blood pressure, diabetes, and dyslipidemia across all segments of society will be critical.
Preventive efforts will have to address the food system, in particular increased consumption of fried foods and edible oils and the more recent modernization of the food supply that has resulted in a rapid increase in consumption of processed foods and beverages high in added sugar, fat, and salt. The poor are particularly affected given the relatively low prices of such foods. There are still small pockets of stunting and micronutrient deficiencies coupled with very limited levels of acute malnutrition in China, which complicates the task. Thus the challenge is to address undernutrition without exacerbating overweight and obesity.
Acknowledgments
This analysis was supported by The National Institutes of Health (NIH): NHLBI (R01-HL108427). This research uses data from China Health and Nutrition Survey (CHNS). We also thank the National Institute of Nutrition and Food Safety, China Center for Disease Control and Prevention, the University of North Carolina at Chapel Hill, the NIH (R01-HD30880, DK056350, R24 HD050924, and R01-HD38700) and the Fogarty International Center, NIH for financial support for the CHNS data collection and analysis files from 1989 to 2011. The NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. We also are grateful to the Carolina Population Center (R24 HD050924) for general support. We thank Ms. Frances Dancy, BS, Carolina Population Center, University of North Carolina at Chapel Hill, for her helpful administrative assistance; Mr. Tom Swasey for graphics support. Jim Terry, AB, Guifeng Jin, MS, and Phil Bardsley, PhD, for programming and technical support; and Samantha Attard, BS, for analysis of time trends in overweight and obesity.
ABBREVIATIONS
- BMI
body mass index
- SES
socioeconomic status
- CHNS
China Health and Nutrition Survey
- WC
waist circumference
- cm
centimeter
- kg
kilogram
- WHO
World Health Organization
- kg/m2
kilograms per square meter
- IOTF
International Obesity Taskforce
- LCTA
latent class trajectory analysis
- CNORM
censored normal model
- CI
confidence interval
- OR
odds ratio
- SE
standard error
Footnotes
Conflict of Interest: None of the authors have financial disclosures or conflicts of interest.
References
- 1.Popkin BM. Will China’s nutrition transition overwhelm its health care system and slow economic growth? Health Aff (Millwood) 2008;27:1064–76. doi: 10.1377/hlthaff.27.4.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van de Poel E, O’Donnell O, Van Doorslaer E. Are urban children really healthier? Evidence from 47 developing countries. Soc Sci Med. 2007;65:1986–2003. doi: 10.1016/j.socscimed.2007.06.032. [DOI] [PubMed] [Google Scholar]
- 3.Xi B, Liang Y, He T, et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993–2009. Obes Rev. 2012;13:287–96. doi: 10.1111/j.1467-789X.2011.00944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dearth-Wesley T, Wang H, Popkin BM. Under- and overnutrition dynamics in Chinese children and adults (1991–2004) Eur J Clin Nutr. 2008;62:1302–7. doi: 10.1038/sj.ejcn.1602853. [DOI] [PubMed] [Google Scholar]
- 5.Wildman RP, Gu D, Muntner P, et al. Trends in overweight and obesity in Chinese adults: between 1991 and 1999–2000. Obesity (Silver Spring, Md) 2008;16:1448–53. doi: 10.1038/oby.2008.208. [DOI] [PubMed] [Google Scholar]
- 6.Wang H, Du S, Zhai F, Popkin BM. Trends in the distribution of body mass index among Chinese adults, aged 20–45 years (1989–2000) Int J Obes. 2007;31:272–8. doi: 10.1038/sj.ijo.0803416. [DOI] [PubMed] [Google Scholar]
- 7.Jones-Smith JC, Gordon-Larsen P, Siddiqi A, Popkin BM. Cross-national comparisons of time trends in overweight inequality by socioeconomic status among women using repeated cross-sectional surveys from 37 developing countries, 1989–2007. Am J Epidemiol. 2011;173:667–75. doi: 10.1093/aje/kwq428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doak C, Adair L, Bentley M, Fengying Z, Popkin B. The underweight/overweight household: an exploration of household sociodemographic and dietary factors in China. Public Health Nutr. 2002;5:215–21. doi: 10.1079/PHN2001296. [DOI] [PubMed] [Google Scholar]
- 9.Doak CM, Adair LS, Monteiro C, Popkin BM. Overweight and underweight coexist within households in Brazil, China and Russia. J Nutr. 2000;130:2965–71. doi: 10.1093/jn/130.12.2965. [DOI] [PubMed] [Google Scholar]
- 10.Wang Y, Monteiro C, Popkin BM. Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. Am J Clin Nutr. 2002;75:971–7. doi: 10.1093/ajcn/75.6.971. [DOI] [PubMed] [Google Scholar]
- 11.Mendez MA, Monteiro CA, Popkin BM. Overweight exceeds underweight among women in most developing countries. Am J Clin Nutr. 2005;81:714–21. doi: 10.1093/ajcn/81.3.714. [DOI] [PubMed] [Google Scholar]
- 12.He J, Gu D, Wu X, et al. Major causes of death among men and women in China. N Engl J Med. 2005;353:1124–34. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- 13.Yoon K-H, Lee J-H, Kim J-W, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–88. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 14.Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090–101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 15.Boffetta P, McLerran D, Chen Y, et al. Body mass index and diabetes in Asia: a cross-sectional pooled analysis of 900,000 individuals in the Asia cohort consortium. PLoS One. 2011;6:e19930. doi: 10.1371/journal.pone.0019930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Bank. World Development Indicators. 2010. [Google Scholar]
- 17.Monteiro CA, Conde WL, Lu B, Popkin BM. Obesity and inequities in health in the developing world. Int J Obes. 2004;28:1181–6. doi: 10.1038/sj.ijo.0802716. [DOI] [PubMed] [Google Scholar]
- 18.Ezzati M, Vander Hoorn S, Lawes CM, et al. Rethinking the “diseases of affluence” paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med. 2005;2:e133. doi: 10.1371/journal.pmed.0020133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Popkin BM. The implications of the nutrition transition for obesity in the developing world. In: Crawford D, Jeffery R, editors. Obesity Prevention in the 21st Century: Public Health Approaches to Tackle the Obesity Pandemic. Oxfort University Press; New York: 2010. pp. 75–98. [Google Scholar]
- 21.Popkin BM. Global changes in diet and activity patterns as drivers of the nutrition transition. Nestle Nutr Workshop Ser Pediatr Program. 2009;63:1–10. doi: 10.1159/000209967. discussion 10–4, 259–68. [DOI] [PubMed] [Google Scholar]
- 22.Popkin BM, Mendez M. The rapid shifts in stages of the nutrition transition: The global obesity epidemic. In: Kawachi I, Wamala S, editors. Globalization and Health. Oxford Scholarship Online; 2006. pp. 68–80. [Google Scholar]
- 23.Popkin BM, Du S. Dynamics of the nutrition transition toward the animal foods sector in China and its implications: a worried perspective. J Nutr. 2003;133:3898S–906. doi: 10.1093/jn/133.11.3898S. [DOI] [PubMed] [Google Scholar]
- 24.Popkin BM. An overview on the nutrition transition and its health implications: the Bellagio meeting. Public Health Nutr. 2002;5:93–103. doi: 10.1079/phn2001280. [DOI] [PubMed] [Google Scholar]
- 25.Du S, Mroz TA, Zhai F, Popkin BM. Rapid income growth adversely affects diet quality in China--particularly for the poor! Socl Sci Med. 2004;59:1505–15. doi: 10.1016/j.socscimed.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 26.Wang Y, Popkin B, Zhai F. The nutritional status and dietary pattern of Chinese adolescents, 1991 and 1993. Eur J Clin Nutr. 1998;52:908–16. doi: 10.1038/sj.ejcn.1600664. [DOI] [PubMed] [Google Scholar]
- 27.Wang Z, Zhai F, He Y, Hu Y. Trends and prevalence of malnutrition among children under five year-old in Chinese rural of different classes. Wei sheng yan jiu/J Hygiene Res. 2007;36:82–5. [PubMed] [Google Scholar]
- 28.Popkin BM. Recent dynamics suggest selected countries catching up to US obesity. Am J Clin Nutr. 2010;91:284S–88S. doi: 10.3945/ajcn.2009.28473C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Popkin BM, Conde W, Hou N, Monteiro C. Is there a lag globally in overweight trends for children compared with adults? Obesity. 2006;14:1846–53. doi: 10.1038/oby.2006.213. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organisation International Association for the Study of Obesity International Obesity TaskForce. The Asia-Pacific perspective: redefining obesity and its treatment. Health Communications: Sydney. 2000:1–56. [Google Scholar]
- 31.Li G, Chen X, Jang Y, et al. Obesity, coronary heart disease risk factors and diabetes in Chinese: an approach to the criteria of obesity in the Chinese population. Obes Rev. 2002;3:167–72. doi: 10.1046/j.1467-789x.2002.00067.x. [DOI] [PubMed] [Google Scholar]
- 32.Balkau B, Deanfield JE, Despres J-P, et al. International Day for the Evaluation of Abdominal Obesity (IDEA): A study of waist circumference, cardiovascular disease, and diabetes mellitus in 168, 000 primary care patients in 63 countries. Circulation. 2007;116:1942–51. doi: 10.1161/CIRCULATIONAHA.106.676379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee CMY, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol. 2008;61:646–53. doi: 10.1016/j.jclinepi.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 34.Nakamura T, Tokunaga K, Shimomura I, et al. Contribution of visceral fat accumulation to the development of coronary artery disease in non-obese men. Atherosclerosis. 1994;107:239–46. doi: 10.1016/0021-9150(94)90025-6. [DOI] [PubMed] [Google Scholar]
- 35.Nicklas BJ, Penninx BW, Cesari M, et al. Association of visceral adipose tissue with incident myocardial infarction in older men and women: the Health, Aging and Body Composition Study. Am J Epidemiol. 2004;160:741–9. doi: 10.1093/aje/kwh281. [DOI] [PubMed] [Google Scholar]
- 36.Demerath EW, Reed D, Rogers N, et al. Visceral adiposity and its anatomical distribution as predictors of the metabolic syndrome and cardiometabolic risk factor levels. Am J Clin Nutr. 2008;88:1263–71. doi: 10.3945/ajcn.2008.26546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tuan NT, Adair LS, Stevens J, Popkin BM. Prediction of hypertension by different anthropometric indices in adults: the change in estimate approach. Public Health Nutr. 2010;13:639–46. doi: 10.1017/S1368980009991479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gordon-Larsen P, Adair LS, Meigs JB, et al. Discordant risk: Overweight and cardiometabolic risk in Chinese adults: Overweight and cardiometabolic risk in China. Obesity. 2012 doi: 10.1038/oby.2012.152. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang X, Shu X-O, Gao Y-T, Yang G, Li H, Zheng W. General and abdominal adiposity and risk of stroke in Chinese women. Stroke. 2009;40:1098–104. doi: 10.1161/STROKEAHA.108.539692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jia Z, Zhou Y, Liu X, et al. Comparison of different anthropometric measures as predictors of diabetes incidence in a Chinese population. Diabetes Res Clin Practice. 2011;92:265–71. doi: 10.1016/j.diabres.2011.01.021. [DOI] [PubMed] [Google Scholar]
- 41.Du T, Sun X, Yin P, Huo R, Ni C, Yu X. Increasing trends in central obesity among Chinese adults with normal body mass index, 1993–2009. BMC Public Health. 2013;13:327. doi: 10.1186/1471-2458-13-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang B, Zhai F, Du S, Popkin BM. The China Health and Nutrition Survey, 1989–2011. Obes Rev. 2013:14. doi: 10.1111/obr.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.National Bureau of Statistics of China. China Statistical Yearbook. China Statistics Press; 2012. http://www.stats.gov.cn/english/2013. [Google Scholar]
- 44.Popkin BM, Du S, Zhai F, Zhang B. Cohort Profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol. 2010;39:1435–40. doi: 10.1093/ije/dyp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stookey JD, Adair L, Stevens J, Popkin BM. Patterns of long-term change in body composition are associated with diet, activity, income and urban residence among older adults in China. J Nutr. 2001;131:2433S–40S. doi: 10.1093/jn/131.9.2433S. [DOI] [PubMed] [Google Scholar]
- 46.WHO Expert Committee. WHO Technical Report Series 854. World Health Organization; Geneva: 1995. Physical Status: The Use and Interpretation of Anthopometry: Report of a WHO Expert Committee. [PubMed] [Google Scholar]
- 47.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 48.Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15:83–96. [PubMed] [Google Scholar]
- 49.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Group of China Obesity Task Force. Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents. Chinese J Epidemiol. 2004;25:97–102. [PubMed] [Google Scholar]
- 51.Jaacks LM, Gordon-Larsen P, Mayer-Davis EJ, Adair LS, Popkin B. Age, period and cohort effects on adult body mass index and overweight from 1991 to 2009 in China: the China Health and Nutrition Survey. Int J Epidemiol. 2013:1–10. doi: 10.1093/ije/dyt052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Croudace TJ, Jarvelin M-R, Wadsworth MEJ, Jones PB. Developmental typology of trajectories to nighttime bladder control: Epidemiologic application of longitudinal latent class analysis. Am J Epidemiol. 2003;157:834–42. doi: 10.1093/aje/kwg049. [DOI] [PubMed] [Google Scholar]
- 53.Andruff H, Carrari N, Thompson A, Gaudreau P, Louvet B. Latent class growth modelling: A tutorial. Tutorials Quant Methods Psychol. 2009;5:11–24. [Google Scholar]
- 54.Nagin DS. Analyzing developmental trajectories: A semiparametric, group-based approach. Psychol Methods. 1999;4:139. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- 55.Nagin DS. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 56.Jones BL, Nagin DS. Advances in group-nased trajectory modeling and an SAS procedure for estimating them. Soc Methods Res. 2007;35:542–71. [Google Scholar]
- 57.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Soc Methods Res. 2001;29:374–93. [Google Scholar]
- 58.Paynter L, Herring AH, Adair LS, Thompson AL, Gordon-Larsen P. Weight history in a modernizing country context: a latent class trajectory approach. Int J Epidemiol. In progress. [Google Scholar]
- 59.Stern D, Smith L, Zhang B, Gordon-Larsen P, Popkin B. Changes in waist circumference relative to body mass index in Chinese adults, 1991 to 2009. University of North Carolina; Chapel Hill: In Progress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jones-Smith JC, Popkin BM. Understanding community context and adult health changes in China: development of an urbanicity scale. Soc Sci Med. 2010;71:1436–46. doi: 10.1016/j.socscimed.2010.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jones-Smith JC, Gordon-Larsen P, Siddiqi A, Popkin BM. Emerging disparities in overweight by educational attainment in Chinese adults (1989–2006) Int J Obes. 2012;36:866–75. doi: 10.1038/ijo.2011.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.WHO; World Health Organization, editor. The Global Status Report on Noncommunicable Diseases. 2010. World Health Organization; 2011. p. 176. [Google Scholar]
- 63.Lee CM, Huxley RR, Lam TH, et al. Prevalence of diabetes mellitus and population attributable fractions for coronary heart disease and stroke mortality in the WHO South-East Asia and Western Pacific regions. Asia Pac J Clin Nutr. 2007;16:187–92. [PubMed] [Google Scholar]
- 64.Gu D, Gupta A, Muntner P, et al. Prevalence of cardiovascular disease risk factor clustering among the adult population of China: results from the International Collaborative Study of Cardiovascular Disease in Asia (InterAsia) Circulation. 2005;112:658–65. doi: 10.1161/CIRCULATIONAHA.104.515072. [DOI] [PubMed] [Google Scholar]
- 65.Yan S, Li J, Li S, et al. The expanding burden of cardiometabolic risk in China: the China Health and Nutrition Survey. Obes Rev. 2012;13:810–21. doi: 10.1111/j.1467-789X.2012.01016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhao W, Zhai Y, Hu J, et al. Economic burden of obesity-related chronic diseases in Mainland China. Obes Rev. 2008;9 (Suppl 1):62–7. doi: 10.1111/j.1467-789X.2007.00440.x. [DOI] [PubMed] [Google Scholar]
- 67.Popkin BM, Kim S, Rusev ER, Du S, Zizza C. Measuring the full economic costs of diet, physical activity and obesity-related chronic diseases. Obes Rev. 2006;7:271–93. doi: 10.1111/j.1467-789X.2006.00230.x. [DOI] [PubMed] [Google Scholar]
- 68.Zhao W. Healthcare Policy and Burden of Diet and Nutrition-Related Chronic Diseases in China. In: Gussler J, Graham MA, editors. Nutrition Health Economics and Outcomes Research. Abbott Nutrition; Columbus, Ohio: 2013. pp. 47–53. [Google Scholar]
- 69.Moran A, Zhao D, Gu D, et al. The future impact of population growth and aging on coronary heart disease in China: projections from the Coronary Heart Disease Policy Model-China. BMC Public Health. 2008;8:394. doi: 10.1186/1471-2458-8-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381:1987–2015. doi: 10.1016/S0140-6736(13)61097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Reynolds K, Gu D, Whelton PK, et al. Prevalence and risk factors of overweight and obesity in China. Obesity (Silver Spring, Md) 2007;15:10–8. doi: 10.1038/oby.2007.527. [DOI] [PubMed] [Google Scholar]
- 72.Ng SW, Zhai F, Popkin BM. Impacts of China’s edible oil pricing policy on nutrition. Soc Sci Med. 2008;66:414–26. doi: 10.1016/j.socscimed.2007.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Monda KL, Adair LS, Zhai F, Popkin BM. Longitudinal relationships between occupational and domestic physical activity patterns and body weight in China. Eur J Clin Nutr. 2008;62:1318–25. doi: 10.1038/sj.ejcn.1602849. [DOI] [PubMed] [Google Scholar]
- 74.Wang Z, Zhai F, Zhang B, Popkin BM. Trends in Chinese snacking behaviors and patterns and the social-demographic role between 1991 and 2009. Asia Pac J Clin Nutr. 2012;21:253–62. [PMC free article] [PubMed] [Google Scholar]
- 75.Popkin BM, Keyou G, Zhai F, Guo X, Ma H, Zohoori N. The nutrition transition in China: a cross-sectional analysis. Eur J Clin Nutr. 1993;47:333–46. [PubMed] [Google Scholar]