Abstract
Antiretroviral therapy has changed human immunodeficiency virus (HIV) infection from a near-certainly fatal illness to one that can be managed chronically. More patients are taking antiretroviral drugs (ARVs) for longer periods of time, which naturally results in more observed toxicity. Overdose with ARVs is not commonly reported. The most serious overdose outcomes have been reported in neonates who were inadvertently administered supratherapeutic doses of HIV prophylaxis medications. Typical ARV regimens include a “backbone” of two nucleoside reverse transcriptase inhibitors (NRTI) and a “base” of either a protease inhibitor (PI) or nonnucleoside reverse transcriptase inhibitor. New classes of drugs called entry inhibitors and integrase inhibitors have also emerged. Older NRTIs were associated with mitochondrial toxicity, but this is less common in the newer drugs, emtricitabine, lamivudine, and tenofovir. Mitochondrial toxicity results from NRTI inhibition of a mitochondrial DNA polymerase. Mitochondrial toxicity manifests as myopathy, neuropathy, hepatic failure, and lactic acidosis. Routine lactate assessment in asymptomatic patients is not indicated. Lactate concentration should be obtained in patients taking NRTIs who have fatigue, nausea, vomiting, or vague abdominal pain. Mitochondrial toxicity can be fatal and is treated by supportive care and discontinuing NRTIs. Metabolic cofactors like thiamine, carnitine, and riboflavin may be helpful in managing mitochondrial toxicity. Lipodystrophy describes changes in fat distribution and lipid metabolism that have been attributed to both PIs and NRTIs. Lipodystrophy consists of loss of fat around the face (lipoatrophy), increase in truncal fat, and hypertriglyceridemia. There is no specific treatment of lipodystrophy. Clinicians should be able to recognize effects of chronic toxicity of ARVs, especially mitochondrial toxicity.
Keywords: Antiretroviral, Mitochondrial toxicity, NRTI, Toxicity, HIV, Overdose, ART, HART, Protease inhibitor, NNRTI, Nonnucleoside reverse transcriptase inhibitor, Nucleoside reverse transcriptase inhibitor, Mitochondrial toxicity, Lactic acidosis, Tenofovir, Stavudine, Lamivudine, Emtricitabine, Didanosine, Abacavir, Zalcitabine, Zidovudine, Nevirapine, Efavirenz, Etravirine, Delavirdine, Maraviroc, Raltegravir, Enfuvirtide
Introduction
Antiretroviral therapy has changed human immunodeficiency virus (HIV) infection from a near-certainly fatal illness to one that can be managed chronically. With the increased use of antiretroviral drugs (ARV), clinicians should be able to recognize common toxicities. HIV-infected patients live longer so clinicians are more likely to encounter chronic toxicity. The purpose of this review is to examine adverse effects associated with therapeutic use and overdose of ARV. The review is organized by drug class. We will discuss each drug in three principle classes of ARV—the nucleoside reverse transcriptase inhibitors (NRTI), nonnucleoside reverse transcriptase inhibitors (NNRTI), and protease inhibitors (PI). We also discuss the newest ARV classes, which include entry inhibitors and fusion inhibitors.
Methods
We conducted a comprehensive search for articles related to toxicity of HIV medications. A keyword search with controlled vocabulary was performed. We used the PubMed Medical Subject Headings controlled vocabulary thesaurus for indexing articles including clinical trials, meta-analyses, practice guideline, and reviews. Additionally, Google and Google Scholar were all searched using the following terms: drug toxicity, adverse drug reaction, HIV fusion inhibitors, HIV protease inhibitors, nucleoside reverse transcriptase inhibitor, nonnucleoside reverse transcriptase inhibitor, integrase inhibitor, anti-HIV agents, antiretroviral agents, CCR5 receptor blocker, nucleotide reverse transcriptase inhibitor, specific antiretroviral drug names, drug interactions, and names of frequently used recreational drugs. Textbooks of pharmacology and medical toxicology were also reviewed for references.
Clinical Use of ARV Drugs (ARVs)
The goal of therapy is to suppress HIV viral load, restore immune function, prevent HIV transmission, prevent resistance, and improve quality of life. There is some debate about when to initiate ARVs, and there has been a trend toward earlier initiation. Experts recommend initiating for CD4 count ≤ 500 cells/μL, pregnancy, coinfection with hepatitis B or C, age >60 years, HIV-associated nephropathy, acute primary HIV infection, coinfection with tuberculosis, and presence of opportunistic infections [1].
Early attempts at use of single-agent therapy resulted in viral resistance. Antiretroviral regimens today typically have three drugs, consisting of two NRTIs with either a boosted PI or a NNRTI. In treatment-naïve patients, the use of four-drug regimens does not result in improved outcome and introduces more adverse effects [2]. HIV specialists commonly refer to the two-drug NRTI combination as the “backbone” and the PI or NNRTI as the “base” of the regimen. In PI-based regimens, a low dose of a second PI, ritonavir, is often used to interfere with cytochrome P450 (CYP) metabolism of the principle PI and thereby increase its concentration. This practice is typically referred to as “boosting.” Darunavir/ritonavir and atazanavir/ritonavir are usually the preferred boosted PI combinations while efavirenz is the preferred NNRTI. Recently, the integrase inhibitor raltegravir has emerged as another option as a “base” in three-drug therapy. In special circumstances NRTI-sparing antiretroviral therapy with PIs and an integrase inhibitor or NNRTI (i.e., darunavir/ritonavir and etravirine or darunavir/ritonavir and raltegravir) may be used. An ideal regimen meets treatment goals with a minimum of adverse effects. Care should also be taken to ensure the patient can adhere to the regimen by reducing “pill burden.” Once-daily regimens are associated with better adherence [3].
The majority of toxic effects from ARV result from adverse drug effects of therapeutic doses of ARV and drug–drug interactions. Overdose, either intentional or unintentional, with ARV is rare. Following the introduction of zidovudine, there were a number of reported overdoses [4]. The more recent reports have been of unintentional supratherapeutic administrations in neonates [5–7].
The relative paucity of intentional overdoses is also seen in yearly data collected by the American Association of Poison Control Centers in the National Poison Data System (NPDS) (Table 1). An examination of the last 5 years (2007–2011) of published poison center data, describing single antiretroviral exposures, demonstrates that the majority of the single exposures can be accounted for by unintentional ingestion. When examining the outcome of these single exposures, the data demonstrate the “None” outcome (indicating no effect), was most common. Additionally, developing a “Major” outcome or death from ingestion, whether the motive intentional or unintentional, was very rare in each year evaluated. The number of adverse reactions recorded over this 5-year period was fairly uniform [8–12]. Comparing these data to the data from 10 years prior (2002) demonstrates an overall decline in adverse reactions from 85 in 2002 to 16 in 2011 [13]. This may be a result of the use of safer medications or coformulation of medications in ways that decrease the opportunity for unintentional overdose. However, the decrease in reports may also be due to increased clinician comfort in dealing with adverse effects of ARV and less perceived need to get assistance [8–13]. Overall, these data represent a fraction of actual events as not all events are recognized, and not all recognized events are reported.
Table 1.
Antiretroviral exposures reported to the National Poison Data System
| Reason | Outcome | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Year | No. of single exposures | Unintentional | Intentional | Other | Adverse reaction | None | Minor | Moderate | Major | Death |
| 2007 | 279 | 203 | 60 | 0 | 16 | 68 | 32 | 10 | 2 | 0 |
| 2008 | 277 | 209 | 53 | 1 | 14 | 65 | 20 | 11 | 1 | 0 |
| 2009 | 390 | 320 | 45 | 0 | 23 | 89 | 39 | 8 | 2 | 0 |
| 2010 | 354 | 277 | 63 | 0 | 14 | 91 | 30 | 18 | 0 | 1 |
| 2011 | 371 | 296 | 55 | 2 | 16 | 78 | 34 | 9 | 0 | 0 |
Antiretroviral Drugs
Reverse Transcriptase Inhibitors
Reverse transcriptase inhibitors (RTIs) inhibit transcription of viral RNA into proviral DNA. The RTIs are subdivided into nucleoside reverse transcriptase inhibitors (NRTIs), for which zidovudine is the prototype, and the NNRTIs, for which nevirapine is the prototype. In the United States, commercially available NRTIs include abacavir, emtricitabine, didanosine, lamivudine, stavudine, and zidovudine. Because tenofovir has a phosphate group bound to the nitrogenous base, it is actually a nucleotide analog, not a nucleoside analog. However, this nucleotide reverse transcriptase inhibitor is traditionally included in the NRTI class. Commercially available NNRTIs in the U.S. include nevirapine, efavirenz, rilpivirine, and delavirdine. Intentional overdose with NRTIs occurs less frequently than unintentional overdose, and the majority of adverse effects are seen with chronic use.
Nucleoside Reverse Transcriptase Inhibitors (NRTIs)
There are seven NRTIs that are commercially available for use in HIV in the United States. There are adverse effects that are specific to individual NRTI drugs (see Table 2). The hallmark toxicity of the NRTI class is mitochondrial toxicity, which may manifest as peripheral neuropathy, myopathy, lipoatrophy, or hepatic steatosis with lactic acidosis (see section on “Mitochondrial Toxicity”).
Table 2.
Summary of toxic effects of nucleoside reverse transcriptase inhibitors
| NRTI | Potential for mitochondrial toxicity | Other predominant toxicities |
|---|---|---|
| Abacavir (ABC) | + | Hypersensitivity reaction |
| Didanosine (ddI) | ++++ | Pancreatitis, peripheral neuropathy |
| Emtricitabine (FTC) | + | Mild headache, rash, GI upset |
| Lamivudine (3TC) | + | Constitutional symptoms |
| Stavudine (d4T) | ++++ | Lipoatrophy, pancreatitis, peripheral neuropathy |
| Tenofovir (TDF) | + | Fanconi’s syndrome, renal insufficiency, gastrointestinal upset |
| Zalcitabine (no longer availabe) | ++++ | Thrombocytopenia (5 %), anemia (10 %), pancreatitis, cardiomyopathy, peripheral neuropathy (35 %), lactic acidosis |
| Zidovudine (ZDV, AZT) | ++ | Myelosuppression, lipodystrophy |
Abacavir (ABC)
Abacavir (Ziagen™) is a dideoxy-guanosine analogue. Abacavir is not a substrate for CYP. Approximately 30 % of its metabolism is by alcohol dehydrogenase and 36 % by glucuronidation. The serum half-life is 21 h [14]. As with other NRTIs, abacavir is phosphorylated intracellularly to an active metabolite. The phosphorylation effectively “traps” the drug within cells. The presence of the HLA-B*5701 gene allele is associated with elevated odds of developing a hypersensitivity reaction [15]. The hypersensitivity syndrome develops early after initiation of abacavir in 2.3–9 % of adults and children without HLA-B*5701 testing [16]. The practice of screening for HLA-B*5701in patients considered for abacavir reduces the incidence to nearly zero. The syndrome, which may occur within 6 weeks of starting the drug, is characterized by fever, rash, gastrointestinal symptoms, generalized malaise, fatigue, achiness, and/or respiratory symptoms. In severe cases, patients develop anaphylaxis, renal failure, or hepatic failure. Clinical manifestations and etiology are similar to that of the drug reaction with eosinophilia and systemic symptoms or Steven’s Johnson syndrome/toxic epidermal necrosis. Abacavir should be stopped immediately if symptoms occur. Abacavir has also been associated with increased risk of myocardial infarction in epidemiological studies [17]. However, a recent meta-analysis found no increased risk of cardiovascular events [18]. Overdose with abacavir has not been reported.
Didanosine (ddI)
Didanosine (Videx™) is an analogue of deoxyadenosine. The triphosphate metabolite acts as a competitive inhibitor of HIV through chain termination. Didanosine is renally eliminated. The serum half-life is 1.5 h; the phosphorylated active metabolite maintains an intracellular half-life of 25–40 h [19]. The intracellular half-life describes the amount of time the drug maintains a concentration within the CD4 cell, where it is active. The intracellular half-life can provide a better estimate of the drug duration of action than the serum half-life. The most significant drug-limiting toxicities associated with use of ddI include pancreatitis, peripheral neuropathy, hepatic steatosis, and lactic acidosis, which are manifestations of mitochondrial toxicity. Peripheral neuropathy is thought to be dose-dependent and develops in approximately 20 % of individuals, while pancreatitis may occur in 1–7 % of patients receiving didanosine [20]. This drug is rarely used because of toxicity. Overdose with didanosine has not been reported.
Emtricitabine (FTC)
Emtricitabine (Emtriva™) is a dideoxycytidine analog with a structure and resistance profile that is similar to lamivudine (3TC.) The drug differs from lamivudine in the addition of fluorine to emtricitabine, which alters its pharmacokinetic and pharmacodynamic characteristics. Like lamivudine, emtricitabine is renally eliminated via glomerular filtration and tubular secretion. Emtricitabine has a serum half-life of 8–10 h. The intracellular half-life of the active metabolite may be as long as 39 h [21]. Although the clinical significance of a longer intracellular half-life of emtricitabine compared with lamivudine has been debated, this may help prevent development of K65R mutations when co-administered with tenofovir. Emtricitabine is used in popular combination drug formulations, including emtricitabine/tenofovir (Truvada™) and efavirenz/emtricitabine/tenofovir (Atripla™.) Drug-limiting toxicities of emtricitabine are uncommon and generally include hyperpigmentation of the palm and sole, headache, gastrointestinal upset, and rash [22]. Emtricitabine does not cause significant mitochondrial toxicity. Overdose with emtricitabine has not been reported.
Lamivudine (3TC)
Lamivudine (Epivir™) is a dideoxycytidine analog similar to emtricitabine. Lamivudine is renally eliminated via glomerular filtration and tubular secretion. Lamivudine has a short serum half-life (5–7 h), although much of the drug is transported intracellularly and phosphorylated, the active metabolite has a half-life of 12–18 h [23]. The dose of lamivudine should be adjusted in patients with renal impairment [24]. Active lamivudine metabolites are not concentrated in the mitochondria, which may account for the low incidence of mitochondrial toxicity of lamivudine. The most common reported adverse reactions when lamivudine is co-administered with other ARVs (incidence ≥15 %) in adults were constitutional symptoms including headache, nausea, malaise and fatigue, nasal signs and symptoms, and cough [25]. Overdose with lamivudine has not been reported.
Stavudine (d4T)
Stavudine (Zerit™) is a thymidine analogue and a highly potent inhibitor of HIV-1 replication in vitro. About 40 % of stavudine is renally eliminated by glomerular filtration and tubular secretion. The serum half-life is about 1 h. Much of the remainder is transported intracellularly where it is phosphorylated to the active compound with a half-life of 3.5 h. Peripheral neuropathy, observed in about 12 % of patients, is the most important adverse effect of stavudine [26]. Neuropathy is thought to be dose-dependent manifestation of mitochondrial toxicity. Lipoatrophy, also seen with stavudine, is likely also caused by mitochondrial toxicity. Stavudine is not frequently used because of toxicity. Overdose with stavudine has not been reported.
Tenofovir (TDF)
Tenofovir (Viread™) is an acyclic nucleotide diester analog of adenosine monophosphate. It is the only nucleotide analog that is marketed for HIV. Tenofovir has a serum half-life of 14 to 17 h. It is renally eliminated and actively secreted by the renal tubules [27]. Tenofovir is used alone in mono-infected HBV patients or in combination with other ARVs for treatment of HIV-1. Combination includes efavirenz/emtricitabine/tenofovir (Atripla™), emtricitabine/rilpivirine/tenofovir (Complera™), and emtricitabine/tenofovir (Truvada™.) Long-term tenofovir use is associated with a decrease in glomerular filtration rate [28]. The most common adverse reactions observed in tenofovir clinical trials were gastrointestinal upset (nausea, emesis, and abdominal pain) and dizziness. There have been rare cases of proximal renal tubular dysfunction, or Fanconi syndrome. This is characterized by glucosuria, hypophosphatemia, and renal tubular acidosis from diminished bicarbonate reabsorption [29]. Among patients with pre-existing renal insufficiency, long-term tenofovir is associated with nephrotoxicity and should be avoided [30]. This is also true when the patient is simultaneously taking other nephrotoxic medications, as this too predisposes the patient to tenofovir-induced renal dysfunction. Overdose with tenofovir has not been reported.
Zidovudine (ZDV, AZT)
Zidovudine (AZT, Retrovir ™), a pyrimidine analogue, has an azido group substituting for the 3’ hydroxyl group on the ribose ring. Zidovudine is rapidly glucuronidated by first-pass hepatic metabolism and the serum half-life is 1 h. However, the intracellular triphosphate has a half-life of 3–4 h [31]. Clinical use of this drug has evolved from use as monotherapy to use in combination with other ARVs. Initially, patients may experience anorexia, fatigue, myalgias, and insomnia, although these symptoms may resolve spontaneously with continued use. With long-term use, the predominant adverse effect of zidovudine is myelosuppression, specifically neutropenia and anemia, which have been shown to occur in 16 % and 24 % of patients, respectively [32]. Zidovudine is associated with myopathy, lactic acidosis, and hepatic steatosis resulting from mitochondrial toxicity, which we will discuss below. Zidovudine overdose has been observed in neonates receiving postnatal HIV prophylaxis. In most cases, there was a self-limited lactic acidosis and neutropenia. One newborn died from sepsis due to neutropenia [5, 6].
Common Toxicities Associated with Nucleoside Reverse Transcriptase Inhibitors
Mitochondrial Toxicity
Manifestations of mitochondrial toxicity are regarded as the most significant adverse effects of the NRTI class and are associated with the development of key drug-limiting toxicities. Newer drugs have less propensity for causing mitochondrial toxicity, so the incidence may be declining even as more patients undergo NRTI treatment.
Mitochondrial toxicity of NRTI results from NRTI inhibition of a mitochondrial DNA (mtDNA) polymerase. NRTIs are effective at inhibiting HIV replication because of their high affinity for the viral DNA polymerase, reverse transcriptase (RT). However, the NRTIs can also inhibit structurally similar human DNA polymerases, such as mtDNA polymerase ɤ. This polymerase is responsible for replication of mtDNA [33]. Inhibition of mtDNA polymerase ɤ leads to the depletion of mtDNA, resulting in production of dysfunctional mitochondrial protein. As the proportion of dysfunctional mitochondrial protein accumulates, the mitochondria become unable to perform critical metabolic functions, such as oxidation of fatty acid and oxidative phosphorylation. Disruption of oxidative phosphorylation results in increased production of reactive oxygen species due to leakage of electrons from the electron transport chain [34]. These reactive oxygen species lead to further damage of proteins, lipids, and DNA. Over time, accumulation of dysfunctional mitochondria results in clinical signs and symptoms.
There are four major types of NRTI mitochondrial toxicity. These include NRTI-induced myopathy, neuropathy, lipoatrophy, and lactic acidosis, with or without hepatic steatosis [33, 35, 36]. Mitochondria are present in most human cells, with erythrocytes being a notable exception. The propensity for different NRTIs to cause toxicity in different tissues may have to do with the relative distribution of different thymidine kinases in different tissues. These enzymes phosphorylate NRTIs to their active compounds. If more of the NRTI is activated by a thymidine kinase in a given tissue, the possibility of toxicity may be greater [37].
Myopathy
Myopathy is a clinical manifestation of mitochondrial toxicity that is most commonly seen with zidovudine. Myopathy is caused by NRTI inhibition of muscle mtDNA polymerase ɤ and the resultant depletion of muscle mtDNA. Zidovudine also induces myocyte oxidative stress and reduces cellular l-carnitine levels independently of mtDNA damage [38]. Symptoms of myopathy include proximal muscle tenderness and myalgias. Most patients will have an accompanying elevated serum creatine phosphokinase (CPK) [39–41]. Histologically, the myopathy is characterized as inflammatory, with ragged-red fibers present on trichrome stain [41]. A consequence of the structurally and functionally abnormal mitochondria is that long-chain fatty acids cannot be effectively utilized. This results in lipid accumulation within the muscle [42]. There is no specific therapy for NRTI-induced myopathy. The NRTI (usually zidovudine) should be discontinued, and the patient can be started on another drug in the class. In a group of patients with zidovudine-associated myopathy, CPK normalized within 4 weeks of discontinuation, and symptoms improved within 8 weeks [43].
Lipoatrophy
Lipoatrophy describes the asymmetric loss of body fat from the face and extremities often seen in HIV-infected patients. Loss of fat from deep and superficial areas around temporal, cheek, and periorbital areas can be significant, resulting in an emaciated appearance (see Fig. 1). Lipoatrophy has been considered part of a larger group of changes in body fat distribution known as lipodystrophy. Lipodystrophy consists of a combination of lipoatrophy and lipid accumulation in the trunk. Because some drugs predispose to fat accumulation and others predispose to fat atrophy, lipodystrophy may actually be two syndromes occurring simultaneously. Lipid accumulation is likely more related to protease inhibitor therapy, and lipoatrophy is more closely associated with NRTIs, although this is difficult to study because the drugs are often administered together. Lipodystrophy has been associated with HIV infection itself, although it is not related to viral load or CD4 count [44]. Lipdystrophy does not directly cause harm but does contribute to poor self-image among HIV-infected patients and may hurt drug adherence when patients perceive that the drugs are causing a change in appearance.
Fig. 1.
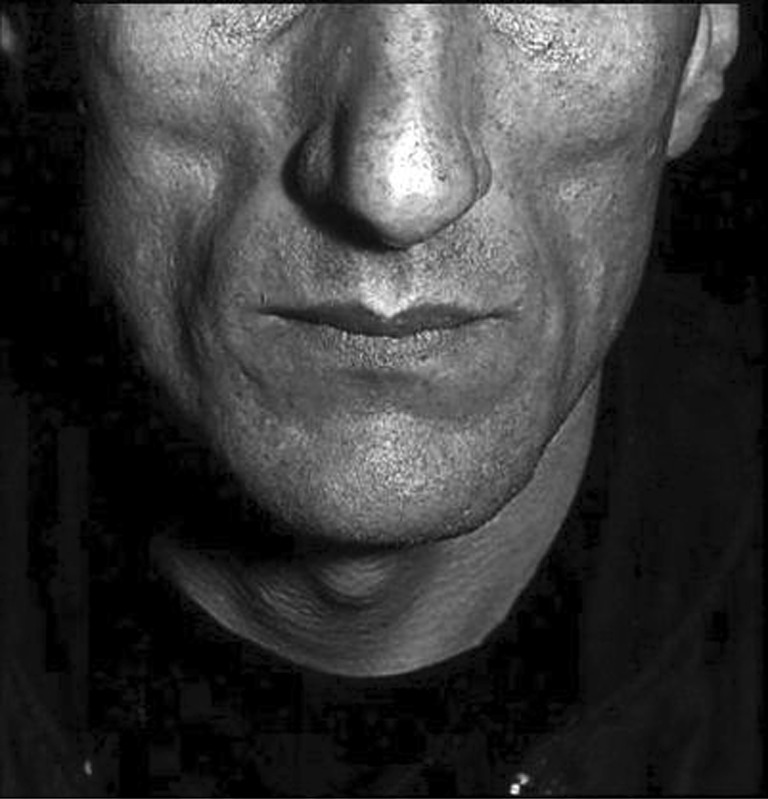
Lipoatrophy of the face. Image courtesy of: AIDS Images Library www.aidsimages.ch
Lipoatrophy has been associated with decreases in mtDNA in subcutaneous fat [45]. The duration of NRTI use and the use of NRTIs with strong inhibition of mtDNA are the most important risk factors for development of lipoatrophy. Stavudine, a strong in vitro inhibitor of mtDNA, is particularly associated with lipoatrophy. Lipoatrophy can be addressed by switching patients to another NRTI. Switching patients from stavudine to abacavir (preferred) or zidovudine improved fat distribution in HIV-infected patients [46].
Neuropathy
Sensory neuropathies remain the most frequent neurological disorders associated with HIV infection and its treatment with ARV [47, 48]. There are at least five forms of HIV-associated peripheral neuropathies including distal symmetric polyneuropathy (DSP), inflammatory demyelinating polyneuropathy (IDP), mononeuritis multiplex (MM), progressive polyradiculopathy (PP), and autonomic neuropathy. Different forms of peripheral neuropathy occur with increased frequency at particular stages of HIV infection [49]. In patients with preserved immune function, IDP is more commonly observed. Inflammatory demyelinating polyneuropathy is characterized by progressive weakness, paresthesias, and the development of mild sensory loss and areflexia. As immunocompetence wanes, other types of peripheral neuropathy predominate, including PP and MM, which may be secondary to opportunistic infections such as cytomegalovirus. Progressive polyneuropathy is characterized by lower extremity weakness, saddle distribution anesthesia, sphincter dysfunction, and impaired reflexes while mononeuritis multiplex is more consistent with multifocal cranial and peripheral neuropathies such as foot or wrist drop and facial weakness. Overall, DSP is the most common form of peripheral neuropathy in HIV infection and is characterized by distal symmetric numbness, tingling, and burning sensations in a stocking-glove distribution along with depressed ankle reflexes [49]. There are two major types of HIV-associated distal sensory peripheral neuropathies: primary HIV-associated distal sensory polyneuropathy and antiretroviral toxic neuropathy, which affect the majority of patients with advanced HIV disease [49, 50]. Antiretroviral toxic neuropathy is the most common toxicity of antiretroviral therapy in sub-Saharan Africa [51]. Lastly, autonomic neuropathy is more commonly observed in patients with AIDS and characterized by manifestations of an impaired sympathetic and parasympathetic nervous system. Failure of the sympathetic nervous system can present as orthostatic hypotension, syncope, diarrhea, and anhidrosis while parasympathetic dysfunction is associated with resting tachycardia, urinary dysfunction, and sexual dysfunction [49]. While peripheral neuropathy is known to complicate untreated HIV infection, most cases result from exposure to NRTI, particularly the dideoxynucleosides didanosine, zalcitabine, and stavudine [52, 53].
There is evidence that NRTI-associated peripheral neuropathy is caused by interference with mtDNA synthesis and inhibition of DNA polymerase [49]. Reduced mtDNA levels in subcutaneous fat obtained by punch skin biopsies have been associated with antiretroviral toxic neuropathy [54]. In a rat model, animals treated with zalcitabine developed a dose-dependent axonal neuropathy with abnormal mitochondria within the axons [55]. The relative specificity of some NRTIs for nerve tissue may be due to increased distribution of certain thymidine kinases in nerve tissue [56].
Hepatic Steatosis
Hepatic steatosis has also been reported in conjunction with NRTI use [57]. Mitochondria are responsible for generating energy from the β-oxidation of fatty acids. β-oxidation of fatty acid chains with an even number of carbon atoms produces acetyl-CoA, which can then be used in the citric acid cycle. Β-oxidation of fatty acids with an odd number of carbon atoms produces both acetyl CoA and propionyl CoA. The latter then is converted into succinyl-CoA and fed into the citric acid cycle [58]. Decreased mitochondrial beta β-oxidation of fatty acids results in esterification of triglycerides, which accumulate in the liver. Hepatic steatosis usually occurs in conjunction with hyperlactatemia and can be fatal [59].
Hyperlactatemia and Lactic Acidosis
Hyperlactatemia is the most concerning manifestation of mitochondrial toxicity, although the incidence is expected to decrease as the use of older NRTIs becomes less common. The severity ranges from mild hyperlactatemia without acidosis to severe lactic acidemia. Lactate accumulation results from overproduction of lactate along with decreased ability to oxidize lactate. Lactate accumulation occurs when mitochondrial toxicity results in insufficient oxidative phosphorylation. Under such condition, pyruvate is metabolized to lactate rather than acetyl CoA. Sustained elevations of blood lactate levels indicate decreased uptake by tissues (notably the liver) that normally oxidize lactate or use it as a substrate for gluconeogenesis. Hepatic dysfunction may be an essential prerequisite for the development of lactate accumulation since the liver is the most important organ with respect to lactate metabolism.
The clinical manifestations of NRTI-associated hyperlactatemia are nonspecific and include malaise dyspnea, abdominal pain, nausea, vomiting, weight loss, tachypnea, dyspnea, seizures, changes in mental status, dysrhythmias, and heart failure. Laboratory studies may indicate anemia, leukopenia, as well as elevations in CPK, lipase, and aminotransferases. Imaging may reveal hepatic steatosis [60].
The prevalence of NRTI-associated hyperlactatemia depends on the case definition chosen by the investigator, the specific NRTIs used in the cohort, and characteristics of the population. The least severe presentations are seen the most. The most common presentation is that of mild hyperlactatemia. The incidence of symptomatic mild hyperlactatemia was estimated to be 20.9 cases in 1,000 patient-years in one series. In all ten cases described by the authors, the patients were taking stavudine along with at least one other ARV medication. The cases had mean lactate concentrations of 4.4 mmol/L, and all had hepatic steatosis [61]. The severity of illness in this cohort was mild. One patient was hospitalized and none died.
The incidence decreases when investigators consider only patients with more elevated lactate concentrations. A prospective cohort study in Australia found 3.9 cases of severe hyperlactatemia (lactate >5 mmol/L) with hepatic steatosis per 1,000 patient years. In the same cohort, investigators identified 9.7 cases per 1,000 patient years in which patients had mildly elevated lactate (<5 mmol/L) and mild symptoms that resolved when NRTI therapy was stopped. Many more patients had asymptomatic mild lactate elevations (<5 mmol/L.) In the majority of patients, lactate rose at the start of therapy but then stabilized at a mildly elevated concentration. Approximately 45 % of patients were on stavudine and 29 % on zidovudine [62]. For the most severe manifestation of this condition, the incidence is even lower. The incidence of severe lactic acidemia (hyperlactatemia and pH < 7.4) was 0.85 per 1,000 patient-years in another large cohort. The median lactate in these patients was 6.5 mmol/L, and the mortality was 33 % [63].
Reports demonstrate that the great majority of patients taking NRTIs do not experience significant mitochondrial toxicity. When mitochondrial toxicity occurs, the onset does not occur at a predictable point in therapy. It is generally agreed that mitochondrial toxicity from NRTIs occurs after a threshold of mitochondrial dysfunction has occurred, but the timing of this is variable during the course of therapy. Cases have occurred from 1–20 months after the start of NRTI therapy [63]. The unpredictability of mitochondrial toxicity is attributed to a multitude of factors. Differential susceptibility to NRTIs may result from variability in energy requirements among tissues and variants in DNA polymerase. Clinically, female gender, advanced immunosuppression, and possibly ethnicity have been cited as factors that play a role in increasing an individual’s risk for hyperlactatemia/lactic acidosis [64]. To further emphasize the complexity and multifactorial nature of this problem, mitochondrial dysfunction has also been reported in HIV-infected individuals who are naïve to ARVs [65].
All NRTIs have been implicated in hyperlactatemia, but some drugs are more likely to cause the problem than others. Mitochondrial toxicity due to NRTI use in HIV-infected adults has been reported most often in patients taking zidovudine, lamivudine, stavudine, and didanosine. In vitro, the potencies of inhibition of mtDNA synthesis by the NRTIs tested were zalcitabine (no longer available in US) > didanosine > stavudine > zidovudine > lamivudine = abacavir = tenofovir [66].
The initial diagnosis of mitochondrial toxicity can be challenging in mildly symptomatic patients. Routine lactate assessment in asymptomatic patients is not indicated [67]. Lactate concentration should be obtained in patients taking NRTIs who have fatigue, nausea, vomiting, or vague abdominal pain. There is no specific therapy for NRTI-associated mitochondrial toxicity. Patients with asymptomatic hyperlactatemia may be switched to an NRTI associated with less risk of hyperlactatemia, such as abacavir, lamivudine, or tenofovir.
In symptomatic patients, all HIV medications should be stopped. Supportive care is the mainstay of therapy. Some authors recommend administration of metabolic cofactors [63]. However, the evidence supporting these interventions is weak, the risk is very low as well. Riboflavin is a precursor for the electron transport chain cofactors flavin mononucleotide and flavin adenine dinucleotide. Carnitine facilitates the passage of fatty acids into the mitochondrial matrix where beta-oxidation can occur. Thiamine is an essential cofactor for several metabolic processes, including the conversion of pyruvate to acetyl CoA by the pyruvate dehydrogenase complex. A reasonable regimen would include carnitine 50 mg/kg intravenously once, followed by 50 mg/kg over 24 h divided into six doses, riboflavin 100 mg twice daily, and thiamine 100 mg daily [68–70].
Resolution of hyperlactatemia requires mtDNA to be replenished. Normal lactate concentrations are preceded by normalization of mtDNA concentrations. In a series of patients with NRTI-associated hyperlactatemia, 4–28 weeks were required for lactate normalization [71]. After recovery, a new antiretroviral regimen should be reinstituted in consultation with the patient’s HIV provider. Nonnucleoside reverse-transcriptase inhibitors and PIs lack affinity for mtDNA polymerases [35]. Combinations of NNRTIs and protease inhibitors could be a safe treatment regimen for these patients.
Non-nucleoside Reverse Transcriptase Inhibitors
Nonnucleoside reverse transcriptase inhibitors bind to a hydrophobic pocket adjacent to the active site of reverse transcriptase and cause a conformational change that reduces the ability of nucleosides to be added to the growing DNA chain. In general, the NNRTIs have a lower incidence of adverse effects in comparison to the NRTIs (Table 3). When used as single agent, the drugs quickly suppress viral replication, but resistance and virologic relapse soon develop [72]. With the exception of etravirine and rilpivirine, resistance develops with the substitution of a single amino acid at the NNRTI binding site. The drugs must be used as part of multidrug therapy to prevent resistance. All NNRTIs are hepatically metabolized. Nevirapine and delavirdine are metabolized primarily by CYP3A4, while efavirenz is metabolized by CYP2B6 as well.
Table 3.
Summary of adverse effects of non-nucleoside reverse transcriptase inhibitors
| DRUG | Rash | Other toxicity |
|---|---|---|
| Nevirapine (NVP) | Yes | Hepatitis |
| Efavirenz (EFV) | Yes | CNS manifestations |
| Etravirine (ETR) | Yes | Dyslipidemia, hepatitis |
| Delavirdine (DLV) | Yes | Neutropenia |
As a group, the NNRTIs share some adverse effects. They cause rash, which frequently resolves early in therapy. In very rare cases, Stevens-Johnson syndrome and toxic epidermal necrolysis have occurred.
Nevirapine (NVP)
Nevirapine (Viramune™) is metabolized by CYP3A4 and CYP2B6. The serum half-life is 25–50 h. Nevirapine induces its own metabolism, so half-life will shorten within the first few weeks of therapy. Nevirapine is associated with a nonpruritic rash in 16 % of patients, although there are reports of it occurring in as many as 50 % of patients who receive 400 mg/day. Elevated aminotransferases are observed in 14 % of patients but frank hepatitis in only 1 % [73]. An 8-day-old girl was inadvertently administered a 40-fold overdose of nevirapine when Viramune™ was confused with Viracept™ [73]. The patient experienced mild neutropenia and a peak lactate of 2.4 mmol/L but recovered.
Efavirenz (EFV)
Efavirenz (Sustiva™) is metabolized by CYP2B6 and CYP3A4. The serum half-life is 40–55 h. Efavirenz is associated with CNS effects. As many as 53 % of patients report mood problems, insomnia, or disturbing dreams. Fewer than 5 % discontinue the drug because of CNS effects. Rash, characterized by blistering or moist desquamation, was reported in 27 % of patients. Ulceration was present in 1 % [73]. An ingestion of 3 g efavirenz in a 12-year-old boy resulted in tremors, screaming at night, and motor deficits in lower limbs. All symptoms resolved [74]. Overdoses of efavirenz have been associated with transient CNS disturbances [75, 76].
Etravirine (ETR)
Etravirine (Intelence™) is metabolized by CYP3A4, 2C9, and 2C19. The serum half-life is 41 h. As with other NNRTIs, etravirine is associated with rash. In one series, eruption was present in 17 % of patients and resolved in several weeks. Only 2 % of patients discontinued the drug because of rash [77]. Overdose of etravirine has not been reported.
Delavirdine (DLV)
Delavirdine (Rescriptor™) is metabolized by CYP3A4. The serum half-life is 5.8 h. Because of the relatively short half-life, the drug requires three-times-daily dosing and has fallen out of favor. The maculopapular rash occurs in 18–36 % of patients. As with the other NNRTIs, the rash resolves after a few weeks. There have been rare reports of neutropenia, possibly a result of zidovudine co-administration [78]. Overdose of delavirdine has not been reported.
Protease Inhibitors
Cleavage of the HIV virion by HIV protease is necessary for HIV replication and release from infected cells. Protease inhibitors inhibit HIV replication by binding to the active site of the HIV protease enzyme [79]. PIs which are Food and Drug Administration (FDA)-approved for use in HIV include saquinavir, lopinavir, darunavir, indinavir, tipranavir, atazanavir, nelfinavir, fosamprenavir, and ritonavir.
PIs are primarily metabolized by CYP3A4 (with the exception of nelfinavir), and all inhibit the enzyme. Ritonavir is a PI and strong inhibitor of CYP3A4. However, due to GI intolerance, ritonavir is rarely used at doses that inhibit HIV protease. Rather, lower-dose ritonavir is co-administered with other PIs as a pharmacologic “booster” to decrease CYP metabolism, increase drug concentrations, and therefore decrease pill burden of the PI.
In general, the PIs are tolerated well. As with other ARVs, there are few reports of overdose, and most toxicity is described after long-term use. Gastrointestinal effects are the most common. Abdominal pain, nausea, vomiting, and diarrhea frequently occur but often resolve after starting treatment. In addition to gastrointestinal effects, there are several other adverse effects shared among PIs (Table 4).
Table 4.
Summary of toxic effects of protease inhibitors
| Drug | GI toxicity | Dyslipidemia | Other toxicity |
|---|---|---|---|
| Saquinavir (SQV) | Yes | Yes | – |
| Lopinavir (ABT) | Yes | Yes | Risk for MI |
| Darunavir (DRV) | Yes | – | Rash |
| Indinavir (IDV) | Yes | Yes | Unconjugated hyperbilirubinemia, nephrolithiasis |
| Tipranavir (TPV) | Yes | Yes | Intracranial hemorrhage, rash |
| Atazanavir (ATV) | Yes | – | Unconjugated hyperbilirubinemia |
| Nelfinavir (NFV) | Yes | – | – |
| Fosamprenavir (FPV) | Yes | – | Rash, risk for MI |
| Ritonavir (RTV) | Yes | Yes | Risk for MI |
Patients on ARVs have higher total cholesterol, LDL, trigylcerides, and lower HDL. Because ARVs are administered in combination, it is difficult to separate out the effects of specific drugs. Nevertheless, PIs are thought to be an important contributor to dyslipidemia [80]. The mechanism is probably related to increased hepatic very low-density lipoprotein secretion [81]. There are variations in lipid effects within the PI class. Atazanavir appears to be associated with less dyslipidemia while lopinavir and ritonavir are associated with more dyslipidemia [82]. In large observational studies, there appears to be an increased risk for cardiovascular events in patients on PIs compared with other HIV medications. Some of this risk was associated with dyslipidemia [83]. Other cohorts have not shown an increased risk for cardiovascular disease for patients on any type of ARV [84]. The reason for this discrepancy is not clear but will hopefully be clarified as more data are available.
Protease inhibitors have been associated with development of insulin resistance and type II diabetes [85]. The effect may be greatest with indinavir, lopinavir, and ritonavir and may be absent in atazanavir [86]. The mechanism is likely related to PI interference with glucose transporters [87].
There is no specific management for cardiovascular disease and lipid abnormalities in the patient on PIs. Clinicians should work to manage cardiovascular risk factors and encourage lifestyle modifications in HIV-infected patients as they would for other patients. Patients with lipid abnormalities who are taking a PI associated with that effect may be switched to atazanavir or a NRTI that is not associated with lipid effects.
Lipodystrophy describes changes in fat distribution that have been traditionally associated with PIs. Lipodystrophy has been noted with up to an 83 % prevalence, especially with inidavir, nelfinavir, and saquinavir/ritonavir combination [88]. As discussed earlier in the NRTI section, lipoatrophy may be a manifestation of mitochondrial toxicity while lipid accumulation may be related to protease inhibitors or have multifactorial causes.
Saquinavir (SQV)
Saquinavir (Invirase™) became the first FDA-approved PI in 1995. Saquinavir was initially marketed as single agent therapy, but viral resistance quickly developed. Saquinavir is rapidly metabolized by CYP3A4 via first-pass hepatic metabolism. When coformulated with ritonavir (currently the only available formulation), the bioavailability of saquinavir is much higher [89]. Common adverse effects of saquinavir include nausea, diarrhea, and abdominal discomfort. Saquinavir is no longer commonly used, and overdose has not been reported.
Lopinavir (ABT)
Lopinavir is metabolized by CYP3A4 and is coformulated with ritonavir (Kaletra™) to increase concentrations and decrease dosing frequency. Diarrhea, nausea, and abdominal pain are common with lopinavir/ritonavir [90]. Lopinavir/ritonavir is more likely than other combinations to cause hypertriglyceridemia [82]. Large cohort studies have linked its cumulative exposure with an increased risk of myocardial infarction (MI). An intentional overdose of 54 g of lopinavir and 13.5 g of ritonavir resulted in abdominal pain, vomiting, and headache, but the patient’s symptoms resolved spontaneously [91].
Darunavir (DRV)
Darunavir (Prezista™) is a nonpeptidic protease inhibitor metabolized by CYP3A4. When combined with ritonavir the serum half-life is 15 h [92]. Darunavir has a lower incidence of glucose intolerance, hypertriglyceridemia, and increased total cholesterol compared with lopinavir [93]. In clinical trials, the most common adverse effects were diarrhea (20 %), nausea (18 %), and headache (15 %) [94]. A pediatric patient received four times the recommended dose of darunavir for 14 weeks and achieved improved virus suppression without adverse effect [95].
Indinavir (IDV)
Indinavir (Crixivan™) was one of the first PIs to be commercially available. Because of toxicity, indinavir has been supplanted by other PIs. Indinavir is metabolized by CYP3A4 and has a serum half-life of 1.8 h when administered without ritonavir [96]. The most important adverse effect of indinavir is nephrolithiasis, which can occur early in the treatment course but has been reported as late as three and one-half years after cessation of the drug [97]. The prevalence ranges from 3–15 % [98]. The drug is poorly soluble in water and forms crystals in the renal collecting system [99]. Indinavir causes fewer GI problems compared with other PIs. As with atazanavir, unconjugated hyperbilirubinemia has been observed [96]. Insulin resistance and hyperglycemia are common relative to other PIs. A review of 79 intentional overdoses and supratherapeutic ingestions showed gastrointestinal toxicity and nephrolithiasis but no deaths [100].
Ritonavir (RTV)
Ritonavir (Norvir™) is metabolized by CYP3A4 (major) CYP2D6 (minor) and has a serum half-life of 3–5 h. Ritonavir induces its own metabolism [89]. Ritonavir is rarely used at doses with PI activity. Rather, ritonavir is used with other PIs as a pharmacokinetic enhancer or “booster.” Ritonavir is associated with dose-dependent nausea, vomiting, and abdominal pain, especially early in the treatment course. Ritonavir boosting appears to be associated with hypertriglyceridemia. This is likely both a direct effect of the ritonavir and associated with increased concentrations of the boosted PI [81]. Overdose of ritonavir has not been reported.
Tipranavir (TPV)
Tipranavir (Aptivus™) is active against strains of HIV with resistance to other PIs. Metabolism of tipranavir is via CYP3A4, and serum half-life is 5–6 h [101]. Tipranavir is administered with ritonavir. Tipranavir exhibits more hepatotoxicity than other PIs. This effect is thought to be more severe in patients with hepatitis B or C. Several patients in clinical trials had fatal hepatotoxicity, and the drug was given an FDA boxed warning [102]. Significant aminotransferase elevations were observed in more than 10 % of patients in clinical trials [103]. Diarrhea, nausea, and fatigue were also common in clinical trials. Tipranavir also received an FDA boxed warning for intracranial hemorrhages, although the incidence was low. From a case-control study, some authors concluded that 455–5,000 HIV-infected patients treated with tipranavir would result in one excess intracranial hemorrhage [104]. This effect may be related to decreased platelet aggregation and thromboxane B2 formation [105]. Overdose of tipranavir has not been reported.
Atazanavir (ATV)
Atazanavir (Reyataz™) is metabolized by CYP3A4. At typical doses, the serum half-life is 7 h [106]. Atazanavir is associated with an unconjugated hyperbilirubinema from inhibition of UDP-glucuronosyl transferase. In one cohort, clinical jaundice was present in 5 % of patients, although hepatotoxicity was rare [107]. Compared with other PIs, atazanavir is associated with less hyperlipidemia and glucose intolerance. Long-term use of boosted atazanavir is associated with decreased renal function [28].
Nelfinavir (NFV)
Nelfinavir (Viracept™) is metabolized mainly by CYP2C19 but also by CYP3A4 and CYP2D6. The serum half-life is 3.5–5 h [89]. Because nelfinavir induces its own metabolism, trough concentrations at 1 week are about half of those at day 2 [108]. Although nelfinavir is not associated with glucose intolerance or lipid effects, it is not frequently used because it requires a fatty meal for adequate absorption and is not boosted by ritonavir. Diarrhea is frequently reported in patients taking nelfinavir [108]. Overdose of nelfinavir has not been reported.
Fosamprenavir (FPV)
Fosamprenavir (Lexiva™) is a prodrug of the PI amprenavir, which is no longer marketed. Amprenavir is metabolized by CYP3A4 and can be dosed once daily when administered with ritonavir [109]. Fosamprenavir use is associated with nausea, vomiting, and diarrhea. A drug eruption has been seen in 8 % of patients within 2 weeks of starting the drug [109]. Unlike other protease inhibitors, fosamprenavir does not have strong metabolic lipid effects. Overdose of fosamprenavir has not been reported.
Entry Inhibitors
Combination of ARVs has led to the improved survival of patients infected with human immunodeficiency virus type 1. However, even with the advent of combination ARV therapy, there is still the persistence of drug resistance. Newer agents target different areas of the viral replication cycle with the intent of reducing the development of resistance and thus improving survival. The entry inhibitors interfere with the binding of the HIV virion to the human cell.
Enfuviritide (T-20)
Enfuvirtide (Fuzeon™), the first of the entry inhibitors, was approved by the FDA in 2003. Enfuvirtide must be administered parenterally and is added to therapy in patients who have viral replication despite standard therapy. Enfuvirtide binds to the gp41 envelope of the HIV membrane, preventing a conformational change of the glycoprotein which allows for fusion of the viral and cellular membranes. Enfuvirtide inhibits both virus-to-cell and cell-to-cell HIV transmission [110]. The exact pathway of enfuvirtide metabolism is unknown; however, in vitro metabolism of enfuvirtide undergoes a non-NADPH dependent hydrolysis. The serum half-life is 3.8 h [111].
Common adverse events found with enfuvirtide include local site reactions of pain, erythema, pruritis, and induration. Rare adverse events include systemic hypersensitivity reaction, glomerulonephritis, thrombocytopenia, hyperglycemia, pneumonia, and pancreatitis [111]. Overdose has not been reported.
Maraviroc (MVC)
Maraviroc (Selzentry™) was approved for use in the US in 2007. Maraviroc is a substrate for CYP3A4 and has a serum half-life of 10.6 h [112]. Maraviroc is the first approved antagonist of chemokine co-receptor 5 (CCR5). The CCR5 antagonists are considered to be a separate class or a subtype of the entry inhibitors. Maraviroc is a negative allosteric modulator of the CCR5 receptor, which is found on macrophages and T cells, preventing the HIV protein gp120 from binding the receptor and thus gaining entry into the cell. A tropism assay is required prior to use because maraviroc only has antiretroviral activity if the individual is infected with HIV that uses CCR5 exclusively. The drug does not affect another chemokine receptor, CXCR4, which is used by some HIV virions to gain access to the T lymphocyte.
Common adverse events found with maraviroc include diarrhea, nausea, fatigue, and headache. In clinical trials, there was no statistically significant difference in these effects noted between placebo and maraviroc arms [113]. Increased aminotransferases were observed in maraviroc patients as compared with patients on non-maraviroc therapy, but no significant difference in the number of patients with large aminotransferase elevations. Nonetheless, maraviroc has an FDA boxed warning regarding hepatotoxicity. Overdose has not been reported with maraviroc.
Integrase inhibitor
Raltegravir (RAL)
Raltegravir (Isentress™), the first integrase inhibitor, was approved by the FDA in 2007. The incorporation of the HIV genome into host DNA is called integration. This process is catalyzed by integrase, an enzyme not present in humans [114]. Raltegravir prevents integrase insertion essential for endonucleolytic processing of viral DNA ends, and the subsequent strand transfer of viral and cellular DNA. Raltegravir is metabolized hepatically through the uridine diphosphate glycuronosyltransferase-mediated glucuronidation. Elimination of raltegravir is biphasic. The alpha elimination half-life is 1 h, and the terminal phase is about 9 h [115]. Common adverse effects are nausea, dizziness, headache, insomnia, and fatigue. In clinical trials, overall adverse events were similar between the raltegravir and optimal background therapy arms [116]. Serious adverse events, found in less than 2 % of recipients, include Stevens-Johnson syndrome, toxic epidermal necrolysis, hypersensitivity reaction, rhabdomyolysis, and renal failure. Overdose has not been reported with raltegravir.
Conclusion
Antiretrovirals have allowed people infected with HIV to live normal lives. Adverse effects are inevitably seen with all medications. It is rare to encounter patients with intentional overdose of ARVs. Rather, the clinician will encounter adverse effects of ARVs in patients taking the medications in recommended therapeutic doses. The most consequential of these effects result from mitochondrial toxicity from NRTIs. Patients with this condition may present with a host of nonspecific symptoms. Mitochondrial toxicity may manifest itself as myopathy, neuropathy, or most consequentially, lactic acidosis. The incidence of lactic acidosis is decreasing because the drugs that are most likely to cause it, didanosine, stavudine, and zalcitabine, are used much less frequently. However, because the sheer number of patients on NRTI therapy is still rising, mitochondrial toxicity will continue to occur. Lactate concentration should be obtained in patients taking NRTIs who have fatigue, nausea, vomiting, or vague abdominal pain. The key to management of this complication is supportive care.
Acknowledgments
Conflicts of Interest
Dr. Stolbach owns stock in Gilead Pharmaceuticals (see Universal COI form). No other conflicts are reported.
References
- 1.Thompson MA, Aberg JA, Hoy JF, Telenti A, Benson C, Cahn P, et al. Antiretroviral treatment of adult HIV infection: 2012 recommendations of the International Antiviral Society-USA panel. JAMA. 2012;308(4):387. doi: 10.1001/jama.2012.7961. [DOI] [PubMed] [Google Scholar]
- 2.Shafer RW, Smeaton LM, Robbins GK, De Gruttola V, Snyder SW, D’Aquila RT, Johnson VA, Morse GD, Nokta MA, Martinez AI, Gripshover BM, Kaul P, Haubrich R, Swingle M, McCarty SD, Vella S, Hirsch MS, Merigan TC, AIDS Clinical Trials Group 384 Team Comparison of four-drug regimens and pairs of sequential three-drug regimens as initial therapy for HIV-1 infection. N Engl J Med. 2003;349(24):2304. doi: 10.1056/NEJMoa030265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parienti JJ, Bangsberg DR, Verdon R, Gardner EM. Better adherence with once-daily antiretroviral regimens: a meta-analysis. Clin Infect Dis. 2009;48(4):484–488. doi: 10.1086/596482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maignen F, Meglio S, Bidault I, Castot A. Acute toxicity of zidovudine. Analysis of the literature and number of cases at the Paris Poison Control Center. Therapie. 1993;48(2):129–31. [PubMed] [Google Scholar]
- 5.Livshits Z, Lee S, Hoffman RS, Nelson LS, Esteban-Cruciani N. Zidovudine (AZT) overdose in a healthy newborn receiving postnatal prophylaxis. Clin Toxicol (Phila) 2011;49(8):747–9. doi: 10.3109/15563650.2011.602081. [DOI] [PubMed] [Google Scholar]
- 6.Chiappini E, Galli L, Gabiano C, Gattinara GC, Martino A, Scolfaro C, et al. Preventable zidovudine overdose during postnatal prophylaxis in healthy children born to HIV-1-positive mothers. AIDS. 2008;22(2):316–7. doi: 10.1097/QAD.0b013e3282f33580. [DOI] [PubMed] [Google Scholar]
- 7.Brasme JF, Mille F, Benhayoun M, Bavoux F, Faye A, Teissier N, et al. Uncomplicated outcome after an accidental overdose of nevirapine in a newborn. Eur J Pediatr. 2008;167(6):689–90. doi: 10.1007/s00431-007-0541-9. [DOI] [PubMed] [Google Scholar]
- 8.Bronstein AC, Spyker DA, Cantilena LR, Jr, Green JL, Rumack BH, Dart RC. 2011 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 29th Annual Report. Clin Toxicol (Phila) 2012;50:911–1164. doi: 10.3109/15563650.2012.746424. [DOI] [PubMed] [Google Scholar]
- 9.Bronstein AC, Spyker DA, Cantilena LR, Jr, Green JL, Rumack BH, Dart RC. 2010 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 28th Annual Report. Clin Toxicol (Phila) 2011;49:910–941. doi: 10.3109/15563650.2011.635149. [DOI] [PubMed] [Google Scholar]
- 10.Bronstein AC, Spyker DA, Cantilena LR, Jr, Green JL, Rumack BH, Giffin SL. 2009 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 27th Annual Report. Clin Toxicol (Phila) 2010;48(10):979–1178. doi: 10.3109/15563650.2010.543906. [DOI] [PubMed] [Google Scholar]
- 11.Bronstein AC, Spyker DA, Cantilena LR, Jr, Green JL, Rumack BH, Giffin SL. 2008 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 26th Annual Report. Clin Toxicol (Phila) 2009;47(10):911–1084. doi: 10.3109/15563650903438566. [DOI] [PubMed] [Google Scholar]
- 12.Bronstein AC, Spyker DA, Cantilena LR, Jr, Green JL, Rumack BH, Heard SE. 2007 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 25th Annual Report. Clin Toxicol (Phila) 2008;46(10):927–1057. doi: 10.1080/15563650802559632. [DOI] [PubMed] [Google Scholar]
- 13.William WA, Litovitz TL, Rodgers GC, Klein-Schwartz W, Youniss J, Rose SR, Borys D, May ME. Annual Report of the American Association of Poison Control Centers Toxic Exposure Surveillance System (2003) Am J Emergency Med. 2002;21(5):353–421. doi: 10.1016/s0735-6757(03)00088-3. [DOI] [PubMed] [Google Scholar]
- 14.Hervey PS, Perry CM. Abacavir: a review of its clinical potential in patients with HIV infection. Drugs. 2000;60(2):447–479. doi: 10.2165/00003495-200060020-00015. [DOI] [PubMed] [Google Scholar]
- 15.Mallal S, Nolan D, Witt C, Masel G, Martin AM, Moore C, et al. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse-transcriptase inhibitor abacavir. Lancet. 2002;359(9308):727–732. doi: 10.1016/s0140-6736(02)07873-x. [DOI] [PubMed] [Google Scholar]
- 16.Clay PG. The abacavir hypersensitivity reaction: a review. Clin Ther. 2002;24(10):1502–1514. doi: 10.1016/s0149-2918(02)80057-1. [DOI] [PubMed] [Google Scholar]
- 17.D:A:D Study Group. Sabin CA, Worm SW, Weber R, et al. Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients enrolled in the D:A:D study: a multi-cohort collaboration. Lancet. 2008;371(9622):1417. doi: 10.1016/S0140-6736(08)60423-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cruciani M, Zanichelli V, Serpelloni G, Bosco O, Malena M, Mazzi R, et al. Abacavir use and cardiovascular disease events: a meta-analysis of published and unpublished data. AIDS. 2011;25(16):1993–2004. doi: 10.1097/QAD.0b013e328349c6ee. [DOI] [PubMed] [Google Scholar]
- 19.Moreno S, Hernández B, Dronda F. Didanosine enteric-coated capsule: current role in patients with HIV-1 infection. Drugs. 2007;67(10):1441–1462. doi: 10.2165/00003495-200767100-00006. [DOI] [PubMed] [Google Scholar]
- 20.Floridia M, Vella S, Seeber AC, Tomino C, Fragola V, Weimer LE, et al. A randomized trial (ISS 902) of didanosine versus zidovudine in previously untreated patients with mildly symptomatic human immunodeficiency virus infection. J Infect Dis. 1997;175(2):255–264. doi: 10.1093/infdis/175.2.255. [DOI] [PubMed] [Google Scholar]
- 21.Saag MS. Emtricitabine. a new antiretroviral agent with activity against HIV and hepatitis B virus. Clin Infect Dis. 2006;42(1):126–131. doi: 10.1086/498348. [DOI] [PubMed] [Google Scholar]
- 22.Drugs @ FDA [webpage on the Internet]. FDA approved drug products. Silver Spring, MD: U.S. Food and Drug Administration [updated 2012 July 23; cited 2012 Dec 1]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/021500s019lbl.pdf)
- 23.Moore KH, Barrett JE, Shaw S, Pakes GE, Churchus R, Kapoor A, et al. The pharmacokinetics of lamivudine phosphorylation in peripheral blood mononuclear cells from patients infected with HIV-1. AIDS. 1999;13(16):2239–2250. doi: 10.1097/00002030-199911120-00006. [DOI] [PubMed] [Google Scholar]
- 24.Johnson MA, Verpooten GA, Daniel MJ, Plumb R, Moss J, Van Caesbroeck D, et al. Single dose pharmacokinetics of lamivudine in subjects with impaired renal function and the effect of haemodialysis. Br J Clin Pharmacol. 1998;46(1):21–27. doi: 10.1046/j.1365-2125.1998.00044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drugs @ FDA [webpage on the Internet]. FDA approved drug products. Silver Spring, MD: U.S. Food and Drug Administration. [updated 2011 Nov 18; cited 2012 Dec 1]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/020564s031,020596s030lbl.pdf
- 26.Hurst M, Noble S. Stavudine: an update of its use in the treatment of HIV infection. Drugs. 1999;58(5):919–949. doi: 10.2165/00003495-199958050-00012. [DOI] [PubMed] [Google Scholar]
- 27.Chapman T, McGavin J, Noble S. Tenofovir disoproxil fumarate. Drugs. 2003;63(15):1597–1608. doi: 10.2165/00003495-200363150-00006. [DOI] [PubMed] [Google Scholar]
- 28.Young J, Scha¨ fer J, Fux CA, Furrer H, Bernasconni E, Vernazza P, Calmy A, Cavassani M, Weber R, Battegay M, Bucher HC, Swiss HIV Cohort Study Renal function in patients with HIV starting therapy with tenofovir and either efavirenz, lopinavir or atazanavir. AIDS. 2012;26(5):567–575. doi: 10.1097/QAD.0b013e32834f337c. [DOI] [PubMed] [Google Scholar]
- 29.Mathew G, Knaus SJ. Acquired Fanconi's syndrome associated with tenofovir therapy. J Gen Intern Med. 2006;21(11):C3–C5. doi: 10.1111/j.1525-1497.2006.00518.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scherzer R, Estrella M, Li Y, Choi AI, Deeks SG, Grunfeld C, et al. Association of tenofovir exposure with kidney disease risk in HIV infection. AIDS. 2012;26(7):867–875. doi: 10.1097/QAD.0b013e328351f68f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dudley MN. Clinical pharmacokinetics of nucleoside antiretroviral agents. J Infect Dis. 1995;171:S99–112. doi: 10.1093/infdis/171.supplement_2.s99. [DOI] [PubMed] [Google Scholar]
- 32.Kinloch-De Loes S, Hirschel BJ, Hoen B, Cooper DA, Tindall B, Carr A, et al. A controlled trial of zidovudine in primary human immunodeficiency virus infection. N Engl J Med. 1995;333(7):408–413. doi: 10.1056/NEJM199508173330702. [DOI] [PubMed] [Google Scholar]
- 33.Kakuda TN. Pharmacology of nucleoside and nucleotide reverse transcriptase inhibitor-induced mitochondrial toxicity. Clin Ther. 2000;22(6):685–708. doi: 10.1016/S0149-2918(00)90004-3. [DOI] [PubMed] [Google Scholar]
- 34.Lewis W, Day BJ, Copeland WC. Mitochondrial toxicity of NRTI antiviral drugs: an integrated cellular perspective. Nat Rev Drug Discov. 2003;2(10):812–822. doi: 10.1038/nrd1201. [DOI] [PubMed] [Google Scholar]
- 35.Brinkman K, ter Hofstede HJM, Burger DM, Smeitink JA, Koopmans PP. Adverse effects of reverse transcriptase inhibitors: mitochondrial toxicity as a common pathway. AIDS. 1998;12(14):1735–1744. doi: 10.1097/00002030-199814000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Cossarizza A, Moyle G. Antiretroviral nucleoside and nucleotide analogues and mitochondria. AIDS. 2004;18(2):137–151. doi: 10.1097/00002030-200401230-00002. [DOI] [PubMed] [Google Scholar]
- 37.Sales SD, Hoggard PG, Sunderland D, Khoo S, Hart CA, Back DJ. Zidovudine phosphorylation and mitochondrial toxicity in vitro. Toxicol Appl Pharmacol. 2001;177(1):54–58. doi: 10.1006/taap.2001.9288. [DOI] [PubMed] [Google Scholar]
- 38.Scruggs ER, Dirks Naylor AJ. Mechanisms of zidovudine-induced mitochondrial toxicity and myopathy. Pharmacology. 2008;82(2):83–88. doi: 10.1159/000134943. [DOI] [PubMed] [Google Scholar]
- 39.Moyle G. Clinical manifestations and management of antiretroviral nucleoside analog-related mitochondrial toxicity. Clin Ther. 2000;22(8):911–936. doi: 10.1016/S0149-2918(00)80064-8. [DOI] [PubMed] [Google Scholar]
- 40.Arnaudo E, Dalakas M, Shanske S, Moraes CT, DiMauro S, Schon EA. Depletion of muscle mitochondrial DNA in AIDS patients with zidovudine-induced myopathy. Lancet. 1991;337(8740):508–510. doi: 10.1016/0140-6736(91)91294-5. [DOI] [PubMed] [Google Scholar]
- 41.Dalakas MC, Illa I, Pezeshkpour GH, Laukaitis JP, Cohen B, Griffin JL. Mitochondrial myopathy caused by long-term zidovudine therapy. N Engl J Med. 1990;322(16):1098–1105. doi: 10.1056/NEJM199004193221602. [DOI] [PubMed] [Google Scholar]
- 42.Dalakas MC, Leon-Monzon ME, Bernardini I, Gahl WA, Jay CA. Zidovudine-induced mitochondrial myopathy is associated with muscle carnitine deficiency and lipid storage. Ann Neurol. 1994;35(4):482–487. doi: 10.1002/ana.410350418. [DOI] [PubMed] [Google Scholar]
- 43.Peters BS, Winer J, Landon DN, Stotter A, Pinching AJ. Mitochondrial myopathy associated with chronic zidovudine therapy in AIDS. Q J Med. 1993;86(1):5–15. [PubMed] [Google Scholar]
- 44.Bacchetti P, Gripshover B, Grunfeld C, Heymsfield S, McCreath H, Osmond D, Saag M, Scherzer R, Shlipak M, Tien P, Study of Fat Redistribution and Metabolic Change in HIV Infection (FRAM) Fat distribution in men with HIV infection. J Acquir Immune Defic Syndr. 2005;40(2):121–131. doi: 10.1097/01.qai.0000182230.47819.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shikuma CM, Hu N, Milne C, Yost F, Waslien C, Shimizu S, et al. Mitochondrial DNA decrease in subcutaneous adipose tissue of HIV-infected individuals with peripheral lipoatrophy. AIDS. 2001;15(14):1801–1809. doi: 10.1097/00002030-200109280-00009. [DOI] [PubMed] [Google Scholar]
- 46.McComsey GA, Ward DJ, Hessenthaler SM, Sension MG, Shalit P, Lonergan JT, Fisher RL, Williams VC, Hernandez JE, Trial to Assess the Regression of Hyperlactatemia and to Evaluate the Regression of Established Lipodystrophy in HIV-1-Positive Subjects (TARHEEL, ESS40010) Study Team Improvement in lipoatrophy associated with highly active antiretroviral therapy in human immunodeficiency virus-infected patients switched from stavudine to abacavir or zidovudine: the results of the TARHEEL study. Clin Infect Dis. 2004;38(2):263–270. doi: 10.1086/380790. [DOI] [PubMed] [Google Scholar]
- 47.Bacellar H, Munoz A, Miller EN, Cohen BA, Besley D, Selnes OA, et al. Temporal trends in the incidence of HIV-1-related neurologic diseases: multicenter AIDS Cohort Study, 1985–1992. Neurology. 1994;44(10):1892–1900. doi: 10.1212/wnl.44.10.1892. [DOI] [PubMed] [Google Scholar]
- 48.McArthur JC, Brew BJ, Nath A. Neurological complications of HIV infection. Lancet Neurol. 2005;4(9):543–555. doi: 10.1016/S1474-4422(05)70165-4. [DOI] [PubMed] [Google Scholar]
- 49.Wulff EA, Wang AK, Simpson DM. HIV-associated peripheral neuropathy: epidemiology, pathophysiology and treatment. Drugs. 2000;59(6):1251–1260. doi: 10.2165/00003495-200059060-00005. [DOI] [PubMed] [Google Scholar]
- 50.Cornblath DR, McArthur JC. Predominantly sensory neuropathy in patients with AIDS and AIDS-related complex. Neurology. 1988;38(5):794–796. doi: 10.1212/wnl.38.5.794. [DOI] [PubMed] [Google Scholar]
- 51.Simpson DM, Kitch D, Evans SR, McArthur JC, Asmuth DM, Cohen B, Goodkin K, Gerschenson M, So Y, Marra CM, Diaz-Arrastia R, Shriver S, Millar L, Clifford DB, ACTG A547 Study Group HIV neuropathy natural history cohort study: assessment measures and risk factors. Neurology. 2006;66(11):1679–1687. doi: 10.1212/01.wnl.0000218303.48113.5d. [DOI] [PubMed] [Google Scholar]
- 52.Browne MJ, Mayer KH, Chafee SB, Dudley MN, Posner MR, Steinberg SM, et al. 2’, 3’-Didehydro-3’-deoxythymidine (d4T) in patients with AIDS or AIDS-related complex: a phase I trial. J Infect Dis. 1993;167(1):21–29. doi: 10.1093/infdis/167.1.21. [DOI] [PubMed] [Google Scholar]
- 53.Simpson DM, Tagliati M. Nucleoside analogue-associated peripheral neuropathy in human immunodeficiency virus infection. J Acquir Immune defic Syndr Hum Retrovirol. 1995;9(2):153–161. [PubMed] [Google Scholar]
- 54.Cherry CL, Gahan ME, McArthur J, Lewin SR, Hoy JF, Wesseling SL. Exposure to dideoxynucleosides is reflected in lowered mitochondrial DNA in subcutaneous fat. J Acquir Immune Defic Syndr. 2002;30(3):271–277. doi: 10.1097/00126334-200207010-00002. [DOI] [PubMed] [Google Scholar]
- 55.Russel JW, Cupler EJ, Dalakas MC. Electrophysiological and pathological changes in 2’,3’-dideoxycytidine (ddC)-induced myopathy in an animal model. Ann Neurol. 1995;38:306. [Google Scholar]
- 56.Dalakas MC. Peripheral neuropathy and antiretroviral drugs. J Peripher Nerv Syst. 2001;6(1):14–20. doi: 10.1046/j.1529-8027.2001.006001014.x. [DOI] [PubMed] [Google Scholar]
- 57.Coghlan ME, Sommadossi JP, Jhala NC, Many WJ, Saag MS, Johnson VA. Symptomatic lactic acidosis in hospitalized antiretroviral-treated patients with human immunodeficiency virus infection: a report of 12 cases. Clin Infect Dis. 2001;33(11):1914–1921. doi: 10.1086/323783. [DOI] [PubMed] [Google Scholar]
- 58.Bartlett K, Eaton S. Mitochondrial beta-oxidation. Eur J Biochem. 2004;271(3):462–469. doi: 10.1046/j.1432-1033.2003.03947.x. [DOI] [PubMed] [Google Scholar]
- 59.Lai KK, Gang DL, Zawacki JK, Cooley TP. Fulminant hepatic failure associated with 2',3'-dideoxyinosine (ddI) Ann Intern Med. 1991;115(4):283–284. doi: 10.7326/0003-4819-115-4-283. [DOI] [PubMed] [Google Scholar]
- 60.Calza L, Manfredi R, Chiodo F. Hyperlactatemia and lactic acidosis in HIV-infected patients receiving antiretroviral therapy. Clin Nutr. 2005;24(1):5–15. doi: 10.1016/j.clnu.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 61.Lonergan JT, Behling C, Pfander H, Hassanein TI, Mathews WC. Hyperlactatemia and hepatic abnormalities in 10 human immunodeficiency virus-infected patients receiving nucleoside analogue combination regimens. Clin Infect Dis. 2000;31(1):162–166. doi: 10.1086/313912. [DOI] [PubMed] [Google Scholar]
- 62.John M, Moore CB, James IR, Nolan D, Upton RP, McKinnon EJ, et al. Chronic hyperlactatemia in HIV-infected patients taking antiretroviral therapy. AIDS. 2001;15(6):717–723. doi: 10.1097/00002030-200104130-00007. [DOI] [PubMed] [Google Scholar]
- 63.Falcó V, Rodríguez D, Ribera E, Martínez E, Miró JM, Domingo P, Diazaraque R, et al. Severe nucleoside-associated lactic acidosis in human immunodeficiency virus-infected patients: report of 12 cases and review of the literature. Clin Infect Dis. 2002;34(6):838–846. doi: 10.1086/339041. [DOI] [PubMed] [Google Scholar]
- 64.Lactic Acidosis International Study Group Risk factors for lactic acidosis and severe hyperlactataemia in HIV-1-infected adults exposed to antiretroviral therapy. AIDS. 2007;21(18):2455–2464. doi: 10.1097/QAD.0b013e3282f08cdc. [DOI] [PubMed] [Google Scholar]
- 65.Miro O, Lopez S, Martinez E, Pedrol E, Milinkovic A, Deig E, et al. Mitochondrial effects of HIV infection on the peripheral blood mononuclear cells of HIV-infected patients who were never treated with antiretrovirals. Clin Infect Dis. 2004;39(5):710–716. doi: 10.1086/423176. [DOI] [PubMed] [Google Scholar]
- 66.Birkus G, Hitchcock MJ, Cihlar T. Assessment of mitochondrial toxicity in human cells treated with tenofovir: comparison with other nucleoside reverse transcriptase inhibitors. Antimicrob Agents Chemother. 2002;46(3):716–723. doi: 10.1128/AAC.46.3.716-723.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brinkman K. Management of hyperlactatemia: no need for routine lactate measurements. AIDS. 2001;15(6):795–797. doi: 10.1097/00002030-200104130-00016. [DOI] [PubMed] [Google Scholar]
- 68.Fouty B, Frerman F, Reves R. Riboflavin to treat nucleoside analogue-induced lactic acidosis. Lancet. 1998;352(9124):291–292. doi: 10.1016/S0140-6736(05)60266-8. [DOI] [PubMed] [Google Scholar]
- 69.Claessens YE, Cariou A, Chiche JD, Dauriat G, Dhainaut JF. l-Carnitine as a treatment of life-threatening lactic acidosis induced by nucleoside analogues. AIDS. 2000;14(4):472–473. doi: 10.1097/00002030-200003100-00029. [DOI] [PubMed] [Google Scholar]
- 70.Venhoff N, Setzer B, Lebrecht D, Walker UA. Dietary supplements in the treatment of nucleoside reverse transcriptase inhibitor-related mitochondrial toxicity. AIDS. 2002;16(5):800–802. doi: 10.1097/00002030-200203290-00021. [DOI] [PubMed] [Google Scholar]
- 71.Côté HC, Brumme ZL, Craib KJ, Alexander CS, Wynhoven B, Ting L, et al. Changes in mitochondrial DNA as a marker of nucleoside toxicity in HIV-infected patients. N Engl J Med. 2002;346(11):811–820. doi: 10.1056/NEJMoa012035. [DOI] [PubMed] [Google Scholar]
- 72.Havlir D, McLaughlin MM, Richman DD. A pilot study to evaluate the development of resistance to nevirapine in asymptomatic human immunodeficiency virus-infected patients with CD4 cell counts of >500/mm3: AIDS Clinical Trials Group Protocol 208. J Infect Dis. 1995;172(5):1379–1383. doi: 10.1093/infdis/172.5.1379. [DOI] [PubMed] [Google Scholar]
- 73.Sheran M. The nonnucleoside reverse transcriptase inhibitors efavirenz and nevirapine in the treatment of HIV. HIV Clin Trials. 2005;6(3):158–168. doi: 10.1310/4KC0-56TM-VLBF-78BN. [DOI] [PubMed] [Google Scholar]
- 74.Nazziwa R, Sekadde M, Kanyike F, Wobudeya E, Nabukeera-Barungi N (2012) Efavirenz poisoning in a 12 year old HIV negative African boy. Pan Afr Med J 12:86. 12:86, Epub 2012 Jul 26 [PMC free article] [PubMed]
- 75.Blanch J, Corbella B, García F, Parellada E, Gatell JM. Manic syndrome associated with efavirenz overdose. Clin Infect Dis. 2001;33(2):270–271. doi: 10.1086/321828. [DOI] [PubMed] [Google Scholar]
- 76.Pasticci MB, Bonora S, DICandilo F, Lapalorcia LM, Palladino N, Baldelli F. Transitory severe CNS adverse effects after accidental efavirenz overdose during post-exposure HIV prophylaxis. J Chemother. 2007;19(1):110. doi: 10.1179/joc.2007.19.1.110. [DOI] [PubMed] [Google Scholar]
- 77.Deeks ED, Keating GM. Etravirine. Drugs. 2008;68(16):2357–2372. doi: 10.2165/0003495-200868160-00007. [DOI] [PubMed] [Google Scholar]
- 78.Scott LJ, Perry CM. Delavirdine: a review of its use in HIV infection. Drugs. 2000;60(6):1411–1444. doi: 10.2165/00003495-200060060-00013. [DOI] [PubMed] [Google Scholar]
- 79.Cameron DW, Heath-Chiozzi M, Danner S, Cohen C, Kravcik S, Maurath C, et al. Randomised placebo-controlled trial of ritonavir in advanced HIV-1 disease, The Advanced HIV Disease Ritonavir Study Group. Lancet. 1998;351(9102):543–549. doi: 10.1016/s0140-6736(97)04161-5. [DOI] [PubMed] [Google Scholar]
- 80.Carr A, Samaras K, Burton S, Law M, Freund J, Chisholm DJ, et al. A syndrome of peripheral lipodystrophy, hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS. 1998;12(7):F51–F58. doi: 10.1097/00002030-199807000-00003. [DOI] [PubMed] [Google Scholar]
- 81.Kotler DP. HIV and antiretroviral therapy: lipid abnormalities and associated cardiovascular risk in HIV-infected patients. J Acquir Immune Defic Syndr. 2008;49(Suppl 2):S79–S85. doi: 10.1097/QAI.0b013e318186519c. [DOI] [PubMed] [Google Scholar]
- 82.Stanley TL, Joy T, Hadigan CM, Liebau JG, Makimura H, Chen CY, et al. Effects of switching from lopinavir/ritonavir to atazanavir/ritonavir on muscle glucose uptake and visceral fat in HIV-infected patients. AIDS. 2009;23(11):1349–1357. doi: 10.1097/QAD.0b013e32832ba904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.DAD Study Group, Friis-Møller N, Reiss P, Sabin CA, Weber R, Monforte AD, El-Sadr W, Thiebaut R, DeWit S, Kirk O, Fontas E, Law S, Phillips A, Lundgren JD Class of antiretroviral drugs and the risk of myocardial infarction. N Engl J Med. 2007;356(17):1723–1735. doi: 10.1056/NEJMoa062744. [DOI] [PubMed] [Google Scholar]
- 84.Bozzette SA, Ake CF, Tam HK, Chang SW, Louis TA. Cardiovascular and cerebrovascular events in patients treated for human immunodeficiency virus infection. N Engl J Med. 2003;348(8):702–710. doi: 10.1056/NEJMoa022048. [DOI] [PubMed] [Google Scholar]
- 85.Brown TT, Cole SR, Li X, Kingsley LA, Palella FJ, Riddler SA, et al. Antiretroviral therapy and the prevalence and incidence of diabetes mellitus in the multicenter AIDS cohort study. Arch Intern Med. 2005;165(10):1179–1184. doi: 10.1001/archinte.165.10.1179. [DOI] [PubMed] [Google Scholar]
- 86.Hruz PW. HIV protease inhibitors and insulin resistance: lessons from in-vitro, rodent and healthy human volunteer models. Curr Opin HIV AIDS. 2008;3(6):660–665. doi: 10.1097/COH.0b013e3283139134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Vyas AK, Koster JC, Tzekov A, Hruz PW. Effects of the HIV protease inhibitor ritonavir on GLUT4 knock-out mice. J Biol Chem. 2010;285(47):36395–36400. doi: 10.1074/jbc.M110.176321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Carr A, Samaras K, Thorisdottir A, Kaufmann GR, Chisholm DJ, Cooper DA. Diagnosis, prediction, and natural course of HIV-1 protease-inhibitor-associated lipodystrophy, hyperlipidaemia, and diabetes mellitus: a cohort study. Lancet. 1999;353(9170):2093–2099. doi: 10.1016/S0140-6736(98)08468-2. [DOI] [PubMed] [Google Scholar]
- 89.Flexner C. HIV-protease inhibitors. N Engl J Med. 1998;338(18):1281–1292. doi: 10.1056/NEJM199804303381808. [DOI] [PubMed] [Google Scholar]
- 90.Murphy RL, da Silva BA, Hicks CB, Eron JJ, Gulick RM, Thompson MA, et al. Seven-year efficacy of a lopinavir/ritonavir-based regimen in antiretroviral-naïve HIV-1-infected patients. HIV Clin Trials. 2008;9(1):1–10. doi: 10.1310/hct0901-1. [DOI] [PubMed] [Google Scholar]
- 91.Roberts DM, Ray JE, Buckley NA. Mild clinical toxicity and dose-dependent pharmacokinetics following acute lopinavir/ritonavir poisoning in a HIV-positive patient. AIDS. 2008;22(6):792–793. doi: 10.1097/QAD.0b013e3282f4a0dd. [DOI] [PubMed] [Google Scholar]
- 92.McKeage K, Perry CM, Keam SJ. Darunavir: a review of its use in the management of HIV infection in adults. Drugs. 2009;69(4):477–503. doi: 10.2165/00003495-200969040-00007. [DOI] [PubMed] [Google Scholar]
- 93.Mills AM, Nelson M, Jayaweera D, Ruxrungtham K, Cassetti I, Girard PM, et al. Once-daily darunavir/ritonavir vs. lopinavir/ritonavir in treatment-naive, HIV-1-infected patients: 96-week analysis. AIDS. 2009;23(13):1679–1688. doi: 10.1097/QAD.0b013e32832d7350. [DOI] [PubMed] [Google Scholar]
- 94.Clotet B, Bellos N, Molina JM, POWER 1 and 2 study groups et al. Efficacy and safety of darunavir-ritonavir at week 48 in treatment-experienced patients with HIV-1 infection in POWER 1 and 2: a pooled subgroup analysis of data from two randomised trials. Lancet. 2007;369(9568):1169–1178. doi: 10.1016/S0140-6736(07)60497-8. [DOI] [PubMed] [Google Scholar]
- 95.Rakhmanina NY, Neely MN, Capparelli EV. High dose of darunavir in treatment-experienced HIV-infected adolescent results in virologic suppression and improved CD4 cell count. Ther Drug Monit. 2012;34(3):237–241. doi: 10.1097/FTD.0b013e3182511efe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Plosker GL, Noble S. Indinavir: a review of its use in the management of HIV infection. Drugs. 1999;58(6):1165–1203. doi: 10.2165/00003495-199958060-00011. [DOI] [PubMed] [Google Scholar]
- 97.Huynh J, Hever A, Tom T, Sim JJ. Indinavir-induced nephrolithiasis three and one-half years after cessation of indinavir therapy. Int Urol Nephrol. 2011;43(2):571–573. doi: 10.1007/s11255-010-9751-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Crixivan [package insert]. Whitehouse Station, NJ: Merck Sharp & Dohme Corp, a subsidiary of Merck & Co., Inc; 2004
- 99.Kopp JB, Miller KD, Mican JA, Feuerstein IM, Vaughan E, Baker C, et al. Crystalluria and urinary tract abnormalities associated with indinavir. Ann Intern Med. 1997;127(2):119–125. doi: 10.7326/0003-4819-127-2-199707150-00004. [DOI] [PubMed] [Google Scholar]
- 100.Lehman HP, Benson JO, Beninger PR, Anderson CA, Blumenthal SJ, Sharrar RG. A five-year evaluation of reports of overdose with indinavir sulfate. Pharmacoepidemiol Drug Saf. 2003;12(6):449–457. doi: 10.1002/pds.868. [DOI] [PubMed] [Google Scholar]
- 101.Orman JS, Perry CM. Tipranavir: a review of its use in the management of HIV infection. Drugs. 2008;68(10):1435. doi: 10.2165/00003495-200868100-00006. [DOI] [PubMed] [Google Scholar]
- 102.Drugs @ FDA [webpage on the Internet]. FDA approved drug products. Silver Spring, MD: U.S. Food and Drug Administration. [updated 2012 Feb 17; cited 2012 Dec 1]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/021814s013,022292s006lbl.pdf
- 103.Dong BJ, Cocohoba JM. Tipranavir: a protease inhibitor for HIV salvage therapy. Ann Pharmacother. 2006;40(7–8):1311–1321. doi: 10.1345/aph.1G598. [DOI] [PubMed] [Google Scholar]
- 104.Justice AC, Zingmond DS, Gordon KS, Fultz SL, Goulet JL, King JT Jr, Bravata DM, Valdez H, Kraft M, Mattocks KM, Veterans Aging Cohort Study Project Team Drug toxicity, HIV progression, or comorbidity of aging: does tipranavir use increase the risk of intracranial hemorrhage? Clin Infect Dis. 2008;47(9):1226–1230. doi: 10.1086/592302. [DOI] [PubMed] [Google Scholar]
- 105.Graff J, von Hentig N, Kuczka K, Angioni C, Gute P, Klauke S, et al. Significant effects of tipranavir on platelet aggregation and thromboxane B2 formation in vitro and in vivo. J Antimicrob Chemother. 2008;61(2):394–399. doi: 10.1093/jac/dkm486. [DOI] [PubMed] [Google Scholar]
- 106.Croom KF, Dhillon S, Keam SJ. Atazanavir: a review of its use in the management of HIV-1 infection. Drugs. 2009;69(8):1107–1140. doi: 10.2165/00003495-200969080-00009. [DOI] [PubMed] [Google Scholar]
- 107.McDonald C, Uy J, Hu W, Wirtz V, Juethner S, Butcher D, et al. Clinical significance of hyperbilirubinemia among HIV-1-infected patients treated with atazanavir/ritonavir through 96 weeks in the CASTLE study. AIDS Patient Care STDS. 2012;26(5):259264. doi: 10.1089/apc.2011.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bardsley-Elliot A, Plosker GL. Nelfinavir: an update on its use in HIV infection. Drugs. 2000;59(3):581–620. doi: 10.2165/00003495-200059030-00014. [DOI] [PubMed] [Google Scholar]
- 109.Arvieux C, Tribut O. Amprenavir or fosamprenavir plus ritonavir in HIV infection: pharmacology, efficacy and tolerability profile. Drugs. 2005;65(5):633–659. doi: 10.2165/00003495-200565050-00005. [DOI] [PubMed] [Google Scholar]
- 110.Nagashima KA, Thompson DA, Rosenfield SI, Maddon PJ, Dragic T, Olson WC. Human immunodeficiency virus type 1 entry inhibitors PRO 542 and T-20 are potentially synergistic in blocking virus-cell and cell-cell fusion. J Infect Dis. 2001;183(7):1121–1125. doi: 10.1086/319284. [DOI] [PubMed] [Google Scholar]
- 111.Dando TM, Perry CM. Enfuvirtide. Drugs. 2003;63(24):2755–2766. doi: 10.2165/00003495-200363240-00005. [DOI] [PubMed] [Google Scholar]
- 112.MacArthur RD, Novak RM. Reviews of anti-infective agents: maraviroc: the first of a new class of antiretroviral agents. Clin Infect Dis. 2008;47(2):236–241. doi: 10.1086/589289. [DOI] [PubMed] [Google Scholar]
- 113.Hardy WD, Gulick RM, Mayer H, Fätkenheuer G, Nelson M, Heera J, et al. Two-year safety and virologic efficacy of maraviroc in treatment-experienced patients with CCRt-tropic HIV-1 infection: 96-week combined analysis of MOTIVATE 1 and 2. J Acquir Immune Defic Syndr. 2010;55(5):558–564. doi: 10.1097/QAI.0b013e3181ee3d82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Palmisano L. Role of integrase inhibitors in the treatment of HIV disease. Expert Rev Anti Infect Ther. 2007;5(1):67–75. doi: 10.1586/14787210.5.1.67. [DOI] [PubMed] [Google Scholar]
- 115.Hicks C, Gulick RM. Raltegravir: the first HIV type 1 integrase inhibitor. Clin Infect Dis. 2009;48(7):931–939. doi: 10.1086/597290. [DOI] [PubMed] [Google Scholar]
- 116.Nguyen BY, Isaacs RD, Teppler H, Leavitt RY, Sklar P, Iwamoto M, Wenning LA, et al. Raltegravir: the first HIV-1 integrase strand transfer inhibitor in the HIV armamentarium. Ann N Y Acad Sci. 2011;1222:83–89. doi: 10.1111/j.1749-6632.2011.05972.x. [DOI] [PubMed] [Google Scholar]


