Abstract
Aims
Multiple forms of drug abuse/dependence frequently co-occur with problem/pathological gambling (PPG). The current study examines the extent to which genetic and environmental factors contribute to their co-occurrences.
Design
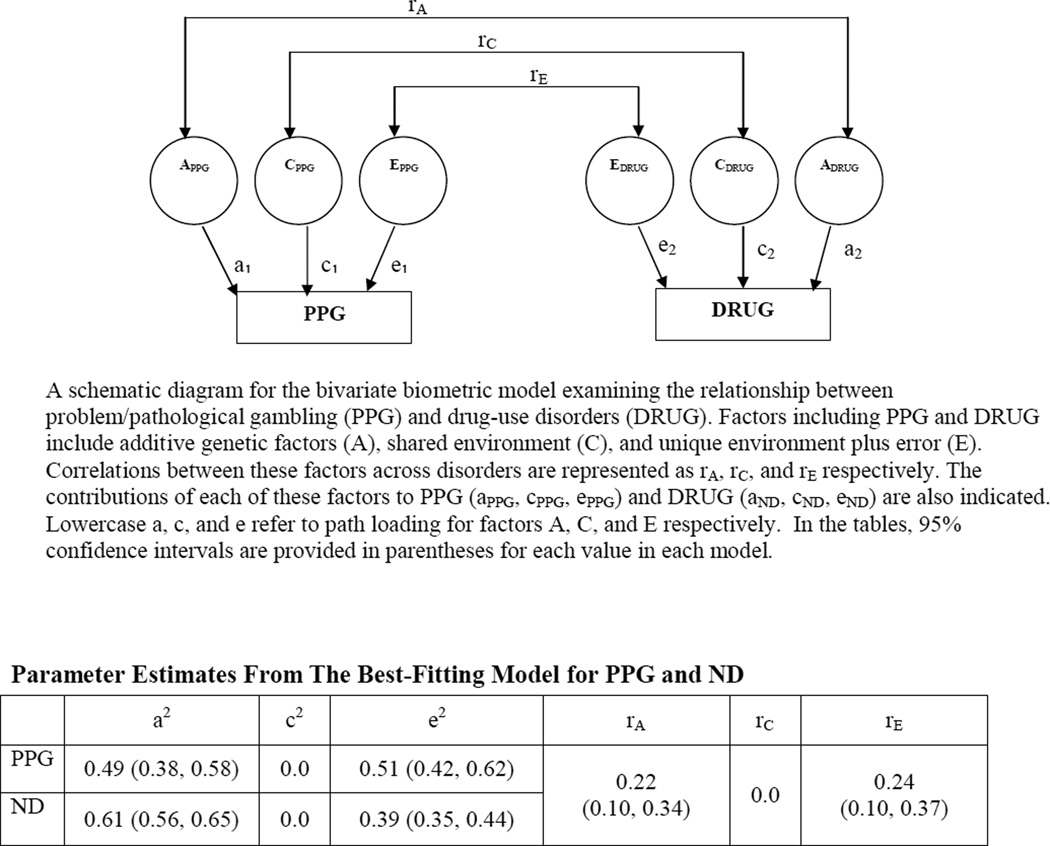
Bivariate models investigated the magnitudes and correlations of genetic and environmental contributions to problem/pathological gambling and its co-occurrence with nicotine dependence, cannabis abuse/dependence, and stimulant abuse/dependence.
Setting
Computer-assisted telephone interviews in the community.
Participants
Participants were 7,869 male twins in the Vietnam Era Twin Registry, a USA-based national twin registry.
Measurements
Lifetime DSM-III-R diagnoses for problem/pathological gambling, nicotine dependence, cannabis abuse/dependence, and stimulant abuse/dependence were determined using the Diagnostic Interview Schedule.
Findings
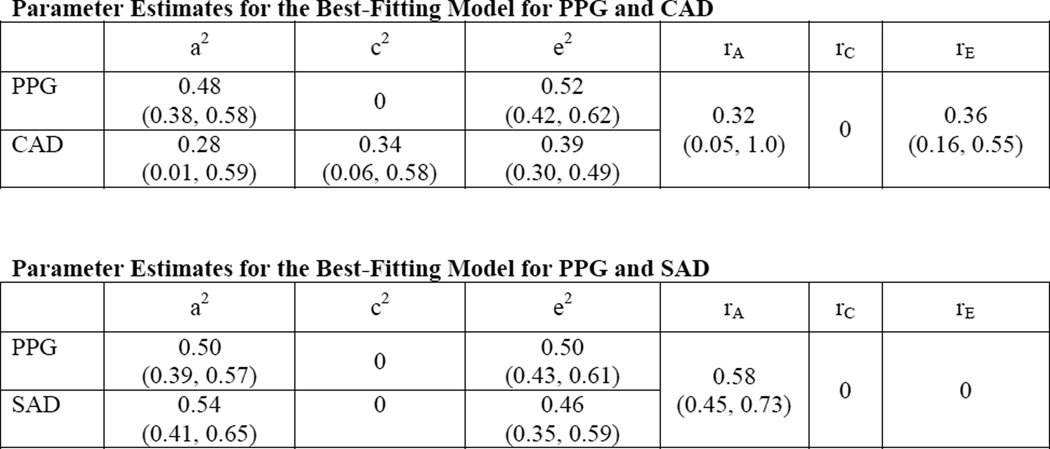
All drug-use disorders displayed additive genetic and non-shared environmental contributions, with cannabis abuse/dependence also displaying shared environmental contributions. Both genetic (genetic correlation rA=0.22; 95%CI:0.10–0.34) and non-shared environmental components (environmental correlation rE=0.24; 95%CI:0.10–0.37) contributed to the co-occurrence of problem/pathological gambling and nicotine dependence. This pattern was shared by cannabis abuse/dependence (rA=0.32; 95%CI:0.05–1.0; rE=0.36; 95%CI:0.16–0.55) but not stimulant abuse/dependence (SAD), which showed only genetic contributions to the co-occurrence with problem/pathological gambling (rA=0.58; 95%CI:0.45–0.73).
Conclusions
Strong links between gambling and stimulant-use disorders may relate to the neurochemical properties of stimulants or the illicit nature of using “hard” drugs like cocaine. The greater contribution of environmental factors to the co-occurrences between problem/pathological gambling and “softer” forms of drug abuse/dependence (cannabis, tobacco) suggest that environmental interventions (perhaps relating to availability and legality) may help diminish the relationship between problem/pathological gambling and tobacco- and cannabis-use disorders.
INTRODUCTION
Pathological gambling is defined by persistent and recurrent maladaptive gambling [1]. Although currently categorized in DSM-IV-TR as an impulse-control disorder [1], pathological gambling is being recommended for inclusion in DSM-5 as an addictive disorder based on clinical and biological similarities [2–4]. Both subsyndromal and syndromal levels of pathological gambling, based on one or more inclusionary criteria for pathological gambling and termed disordered or problem/pathological gambling (PPG), co-occur with substance-use disorders [5–10]. Prior investigations have identified shared genetic and environmental contributions to PPG and alcohol abuse/dependence in men [11]. However, similar approaches have not been applied to the investigation of the relationships between PPG and other substance-use disorders. Information relating to the relative genetic and environmental contributions to PPG and its co-occurrences with specific substance-use disorders (e.g., involving tobacco, cannabis and stimulants like cocaine) may help improve prevention and treatment strategies [12]. Different environmental and genetic factors may contribute to specific substance-use disorders and their co-occurrence with PPG through specific actions of each drug. Given data indicating considerable genetic influences on criminal behaviors [13] and addictions involving illicit substances (e.g., cocaine and cannabis), genetic contributions between illicit substance-use disorders may overlap with genetic contributions to PPG [14, 15].
Given that PPG and drug-use disorders frequently co-occur (a relationship that has been observed in the general population for several decades) [12], it is important to understand the degree to which environmental and genetic factors contribute independently to their co-occurrences. To examine environmental and genetic contributions to PPG and drug-use disorders, we analyzed data from the Vietnam Era Twin Registry (VET-R). The VET-R offers advantages in that it is comprised of a large sample of twins with diagnostic assessments for gambling, drug-use and other psychiatric disorders [9]. Specifically, the VET-R includes over seven thousand male twins and has been used to investigate the environmental and genetics contributions to the co-occurrences between PPG and alcohol-use disorders [11], anti-social behaviors [16], major depression [17] and anxiety disorders [18]. The current study investigated the following hypotheses. First, lifetime PPG would be associated with lifetime drug abuse/dependence relating to nicotine, cannabis and stimulants. Second, given that both tobacco and alcohol are both legal substances and prior analyses of VET-R data have indicated that genetic and unique environmental factors contribute to PPG’s co-occurrence with alcohol-use disorders [11, 19], the co-occurrence of PPG and nicotine dependence (ND) would show shared genetic and unique environmental contributions. Third, given the illegal nature of cannabis and stimulants like cocaine, genetic factors would contribute strongly to the co-occurrence between PPG and cannabis abuse/dependence (CAD) and PPG and stimulant abuse/dependence (SAD).
METHODS
Participants
The VET-R is a large national sample of male twin pairs consisting of 10,253 male twins. Participants were born between 1939–1957 and served during the Vietnam era (1965–1975). In 1992, 7,869 (76.7%) participants were successfully interviewed to ascertain Diagnostic and Statistical Manual, Third Edition-Revised (DSM-III-R) diagnoses for various psychiatric disorders. Questionnaires assessing physical appearance and supplemental blood typing were administered, identifying 1,874 monozygotic and 1,498 dizygotic twin pairs, with remaining participants being singletons [20].
At the time of interviewing, the mean(SD) age of respondents was 42.0(2.8) years. The racial profile of the sample was predominantly white (93.4%; n=7,349), with the remainder acknowledging black (6.2%; n=489) and other (0.4%; n=30) racial identities. The majority of participants had at least a high-school education (64%; n=4929) and were above the poverty level, with annual household incomes generally falling between $20,000-$40,000 (49.1%, n=3,657).
Measures
Lifetime DSM-III-R diagnoses for ND, cannabis abuse and dependence and stimulant abuse and dependence and pathological gambling were determined using the Diagnostic Interview Schedule (DIS) [21]. Lay interviewers obtained verbal informed consent. Criteria for pathological gambling were only assessed in participants who gambled 25 times or more in a year. Participants who had acknowledged using a drug more than five times were administered structured DIS questions that assessed abuse and dependence [22]. Drug abuse/dependence for cannabis and stimulant refers to abuse and/or dependence on (1) marijuana (hashish, ganja, bhang) and (2) stimulants (uppers, amphetamines, speed, ice, crack, cocaine), respectively, and all subjects who met criteria for lifetime regular smoking, having smoked daily for at least 1 month or more, were asked questions to assess ND [23].
Respondents endorsing one or more inclusionary criteria for pathological gambling were categorized as exhibiting PPG. This threshold has been used in other studies examining gambling behaviors in the VET-R [16, 24, 25], Epidemiological Catchment Area study [12], and National Epidemiological Survey of Alcohol and Related Conditions [26] and the National Comorbidity Survey Replication [27].
Hypothesis Testing: Analyses Examining the Relationship Between PPG and Drug-Use Disorders
Odds ratios (ORs) were determined for drug-use disorders in subjects with PPG in order to examine the hypothesis that lifetime drug-use disorders are comorbid with lifetime PPG. In order to adjust for errors of variance of non-independent observations, the SURVEYLOGISTIC procedure in SAS v9.2 was used. Using logistic regression, both unadjusted and adjusted ORs were examined by adjusting for sociodemographic variables (education, age, and income), affective disorders and antisocial personality disorder in a step-wise fashion, controlling first for influences of internalizing disorders (generalized anxiety disorder, panic disorder, depression) and then externalizing disorders (alcohol dependence, antisocial personality disorder).
To examine the hypothesis that drug-use disorders would correlate more strongly in monozygotic twins than dizygotic twins, tetrachoric correlations were examined. To investigate the hypotheses regarding genetic and environmental contributions to PG and drug-use disorders, bivariate model fitting was used. Genetic and environmental contributions were deconstructed into three factors: additive genetic (A), shared environmental (C) and unique environmental, including influences of measurement error (E). The bivariate model thus allowed for the genetic and environmental associations between PPG and drug-use disorders to be examined [11]. Models of maximum likelihood were fitted using MX software [28]. Models were tested for their goodness of fit against a saturated model that included no constraints on the correlation matrices that were estimated for monozygotic and dizygotic twin correlations. The most parsimonious model was selected as best-fitting, with ninety-five-percent confidence-intervals (95% CIs) used to evaluate whether the genetic and environmental contributions to PG and drug-use disorders differed significant from 0 to 1.
RESULTS
Lifetime criteria for PPG, ND, CAD and SAD were met by 614 (7.83%), 3762 (47.81%), 564 (7.20%) and 359 (4.58%) of participants, respectively. Sociodemographics are presented (Table 1A). In unadjusted models, PPG frequently co-occurred with all drug-use disorders: odds ratios (ORs) of 2.08 (95% CI:1.75–2.49) for ND, 2.82 (95% CI:2.23–3.56) for CAD and 3.42 (95% CI:2.61–4.50) for SAD, respectively. After adjusting for sociodemographics and internalizing disorders, ORs remained elevated for ND at 1.69 (95% CI:1.40–2.05), CAD at 2.13 (95% CI:1.63–2.80), and SAD at 2.51 (95% CI:1.83–3.42). After also adjusting for externalizing disorders, all relationships (with the exception of that with CAD) remained significantly elevated: ORs of 1.30 (95% CI:1.06–1.60) for ND, 1.35 (95% CI:0.99–1.84) for CAD, and 1.52 (95% CI:1.06–2.18) for CAD (Table 1B).
Table 1.
| A. Frequency and Percentage of DSM-III-R Disorders and Sociodemographic Variables | |||
|---|---|---|---|
| DSM-III-R Diagnostic Information | Percent | Frequency (n) | Missing (n) |
| Conditions of Focus in Manuscript | |||
| Problem/Pathological Gambling | 7.83% | 614 | 26 |
| Nicotine Dependence | 47.81% | 3762 | 0 |
| Cannabis Abuse/Dependence | 7.20% | 564 | 31 |
| Simulant Abuse/Dependence | 4.58% | 359 | 30 |
| Internalizing Diagnoses | |||
| General Anxiety Disorder | 2.25% | 177 | 18 |
| Panic Disorder | 1.75% | 137 | 18 |
| Major Depression Disorder | 9.61% | 755 | 16 |
| Posttraumatic Stress Disorder | 10.05% | 785 | 56 |
| Externalizing Diagnoses | |||
| Alcohol Dependence | 35.89% | 2817 | 20 |
| Antisocial Personality Disorder | 2.89% | 227 | 18 |
| Sociodemographic Information | Percent | Frequency (n) | Missing (n) |
| Annual Household Income (≥ $30,000) | 45.76% | 3407 | 424 |
| White Race | 93.40% | 7349 | 1 |
| Other Race | 6.60% | 519 | 1 |
| Employed | 95.77% | 7296 | 251 |
| Less Than a High School Education | 3.60% | 274 | 268 |
| High School Education | 31.55% | 2398 | 268 |
| More Than a High School Education | 64.85% | 4929 | 268 |
| B. Logistic Regression Model Examining the Relationships Between Problem/Pathological Gambling and Drug Abuse/Dependence Adjusting for Sociodemographics, Internalizing and Externalizing Disorders | |
|---|---|
| Variable | Odds Ratio (95% CI) |
| Age | 1.00 (0.97 – 1.04) |
| Annual Household Income | 0.97 (0.80 – 1.16) |
| High School Education | 0.95 (0.59 – 1.54) |
| College | 0.83 (0.51 – 1.33) |
| White Race | 1.83 (1.31 – 2.55) |
| Employed | 0.72 (0.50 – 1.04) |
| Alcohol Dependence | 1.89 (1.54 – 2.34) |
| Antisocial Personality Disorder | 2.23 (1.47 – 3.37) |
| Generalized Anxiety Disorder | 1.29 (0.78 – 2.14) |
| Panic Disorder | 1.35 (0.77 – 2.37) |
| Major Depression Disorder | 1.40 (1.05 – 1.87) |
| Posttraumatic Stress Disorder | 1.10 (0.83 – 1.47) |
| Nicotine Dependence | 1.30 (1.06 – 1.60) |
| Stimulant Abuse/Dependence | 1.52 (1.06 – 2.18) |
| Cannabis Abuse/Dependence | 1.35 (0.99 – 1.84) |
| B_ND1. Logistic Regression Model Examining the Relationships Between Problem/Pathological Gambling and Nicotine Dependence without Adjustment | |
|---|---|
| Variable | Odds Ratio (95% CI) |
| Nicotine Dependence | 2.08 (1.75 – 2.49) |
| B_ND2. Logistic Regression Model Examining the Relationships Between Problem/Pathological Gambling and Nicotine Dependence, Adjusting for Sociodemographics | |
|---|---|
| Variable | Odds Ratio (95% CI) |
| Nicotine Dependence | 1.88 (1.56 – 2.27) |
| Age | 0.98 (0.94 – 1.01) |
| Annual Household Income | 0.91 (0.76 – 1.09) |
| High School Education | 0.89 (0.57 – 1.40) |
| College | 0.80 (0.51 – 1.24) |
| White Race | 1.91 (1.38 – 2.64) |
| Employed | 0.61 (0.43 – 0.88) |
| B_ND3. Logistic Regression Model Examining the Relationships Between Problem/Pathological Gambling and Nicotine Dependence, Adjusting for Sociodemographics and Internalizing Disorders | |
|---|---|
| Variable | Odds Ratio (95% CI) |
| Nicotine Dependence | 1.68 (1.39 – 2.04) |
| Age | 0.98 (0.95 – 1.01) |
| Annual Household Income | 0.93 (0.78 – 1.12) |
| High School Education | 0.92 (0.58 – 1.45) |
| College | 0.79 (0.50 – 1.23) |
| White Race | 1.89 (1.37 – 2.61) |
| Employed | 0.67 (0.47 – 0.95) |
| Generalized Anxiety Disorder | 1.49 (0.91 – 2.44) |
| Panic Disorder | 1.54 (0.88 – 2.69) |
| Major Depression Disorder | 1.70 (1.29 – 2.24) |
| Posttraumatic Stress Disorder | 1.39 (1.06 – 1.81) |
| B_SAD1. Logistic Regression Model Examining the Relationships Between Problem/Pathological Gambling and Stimulant Abuse/Dependence without Adjustment | |
|---|---|
| Variable | Odds Ratio (95% CI) |
| Stimulant Abuse/Dependence | 3.42 (2.61 – 4.50) |
| B_SAD2. Logistic Regression Model Examining the Relationships Between Problem/Pathological Gambling and Stimulant Abuse/Dependence, Adjusting for Sociodemographics | |
|---|---|
| Variable | Odds Ratio (95% CI) |
| Stimulant Abuse/Dependence | 3.19 (2.36 – 4.32) |
| Age | 0.98 (0.95 – 1.02) |
| Annual Household Income | 0.91 (0.75 – 1.09) |
| High School Education | 0.83 (0.53 – 1.32) |
| College | 0.70 (0.45 – 1.11) |
| White Race | 1.67 (1.20 – 2.31) |
| Employed | 0.65 (0.45 – 0.93) |
| B_SAD3. Logistic Regression Model Examining the Relationships Between Problem/Pathological Gambling and Stimulant Abuse/Dependence, Adjusting for Sociodemographics and Internalizing Disorders | |
|---|---|
| Variable | Odds Ratio (95% CI) |
| Stimulant Abuse/Dependence | 2.47 (1.81 – 3.37) |
| Age | 0.99 (0.95 – 1.02) |
| Annual Household Income | 0.94 (0.78 – 1.23) |
| High School Education | 0.86 (0.54 – 1.37) |
| College | 0.71 (0.45 – 1.12) |
| White Race | 1.70 (1.22 – 2.35) |
| Employed | 0.68 (0.48 – 0.97) |
| Generalized Anxiety Disorder | 1.49 (0.90 – 2.45) |
| Panic Disorder | 1.51 (0.87 – 2.61) |
| Major Depression Disorder | 1.65 (1.24 – 2.20) |
| Posttraumatic Stress Disorder | 1.43 (1.09 – 1.88) |
| B_CAD1. Logistic Regression Model Examining the Relationships Between Problem/Pathological Gambling and Cannabis Abuse/Dependence without Adjustment | |
|---|---|
| Variable | Odds Ratio (95% CI) |
| Cannabis Abuse/Dependence | 2.82 (2.23 – 3.56) |
| B_CAD2. Logistic Regression Model Examining the Relationships Between Problem/Pathological Gambling and Cannabis Abuse/Dependence, Adjusting for Sociodemographics | |
|---|---|
| Variable | Odds Ratio (95% CI) |
| Cannabis Abuse/Dependence | 2.68 (2.07 – 3.49) |
| Age | 0.99 (0.95 – 1.02) |
| Annual Household Income | 0.93 (0.78 – 1.13) |
| High School Education | 0.86 (0.54 – 1.37) |
| College | 0.72 (0.46 – 1.15) |
| White Race | 1.73 (1.25 – 2.39) |
| Employed | 0.62 (0.43 – 0.88) |
| B_CAD3. Logistic Regression Model Examining the Relationships Between Problem/Pathological Gambling and Cannabis Abuse/Dependence, Adjusting for Sociodemographics and Internalizing Disorders | |
|---|---|
| Variable | Odds Ratio (95% CI) |
| Cannabis Abuse/Dependence | 2.12 (1.62 – 2.78) |
| Age | 0.99 (0.95 – 1.02) |
| Annual Household Income | 0.95 (0.79 – 1.15) |
| High School Education | 0.90 (0.56 – 1.44) |
| College | 0.74 (0.46 – 1.17) |
| White Race | 1.74 (1.25 – 2.40) |
| Employed | 0.66 (0.47 – 0.94) |
| Generalized Anxiety Disorder | 1.50 (0.92 – 2.43) |
| Panic Disorder | 1.49 (0.85 – 2.62) |
| Major Depression Disorder | 1.64 (1.24 – 2.18) |
| Posttraumatic Stress Disorder | 1.41 (1.07 – 1.84) |
Appendix: Abuse/Dependence refers to an individual who met the DSM-III-R criteria for abuse and/or dependence on (1) nicotine (dependence only) (2) cannabis (hashish,ganja, bhang); (3) stimulants (uppers, amphetamines, speed, ice, crack, cocaine); (Xian, et al., 2000).
Abbreviations: CI = confidence interval
In tetrachoric correlations between PPG and drug-use disorders, within-diagnosis concordance frequencies were higher in monozygotic twins than in dizygotic twins (Table 2). These findings are consistent with genetic contributions to each of the gambling and drug-use disorders. The cross-diagnosis cross-twin concordance frequencies were also numerically higher in monozygotic as compared to dizygotic twins. Although this pattern is suggestive of shared genetic contributions to each condition, the overlapping standard errors preclude a definitive interpretation.
Table 2.
Tetrachoric Correlations Between Problem/Pathological Gambling and Drug-Use Disorders in Monozygotic and Dizygotic Twins
| Within-Diagnosis Tetrachoric | Cross-Diagnosis Tetrachoric Correlations | |||
|---|---|---|---|---|
| Correlations (SE) | Between PPG and Drug-Use Disorder (SE) | |||
| Zygosity | PPG | ND | Within-twin | Cross-twin |
| Monozygotic | 0.49 (0.05) | 0.60 (0.03) | 0.21 (0.05) | 0.10 (0.05) |
| Dizygotic | 0.19 (0.08) | 0.31 (0.04) | 0.24 (0.05) | 0.04 (0.07) |
| Zygosity | PPG | CAD | Within-twin | Cross-twin |
| Monozygotic | 0.49 (0.05) | 0.62 (0.05) | 0.23 (0.06) | 0.13 (0.07) |
| Dizygotic | 0.19 (0.08) | 0.46 (0.07) | 0.30 (0.06) | –0.02 (0.09) |
| Zygosity | PPG | SAD | Within-twin | Cross-twin |
| Monozygotic | 0.49 (0.05) | 0.53 (0.07) | 0.26 (0.07) | 0.20 (0.08) |
| Dizygotic | 0.19 (0.08) | 0.23 (0.11) | 0.34 (0.07) | 0.04 (0.10) |
Bivariate genetic models investigated relationships between PPG and individual drug-use disorders (Figure 1). Parameter estimates in these models generally suggested significant genetic and environmental contributions. The best-fitting bivariate model for the relationship between PPG and ND demonstrated significant correlations in the additive genetic (rA=0.22; 95% CI:0.10–0.34) and unique environmental (rE=0.24; 95% CI:0.10–0.37) domains (Supplemental Table 1A). For the relationship between PPG and CAD (Supplemental Table 1B), the best-fitting bivariate model demonstrated correlations in the additive genetic (rA=0.32; 95% CI:0.05–1.0) and unique environmental (rE=0.36; 95% CI:0.16–0.55) domains. Lastly, for PPG and SAD, the best fitting model displayed significant correlations only within the genetic domain (rA=0.58; 95% CI: 0.45–0.73) (Supplemental Table 1C).
Figure 1.
Bivariate Model: Problem/Pathological Gambling and Drug-Use Disorders 1
1 The schematic diagram is a representation of the bivariate models which were similarly independently conducted for all the disorders: nicotine abuse/dependence, cannabis abuse/dependence and stimulant/abuse/ dependence
When comparing PPG and ND, of the 49% genetic variance observed in PPG, 2% (95% CI:1–6%) was shared with ND. Of the 61% genetic variance contribution to ND, 3% (95% CI:1–7%) was shared with PPG. In PPG and ND, the unique environmental component accounted for 51% (95% CI:42–62%) of the variance in PPG and 39% (95% CI:35–44%) of that observed in ND. Of the 51% of the unique environmental component contributing to PPG, 3% (95% CI:1–7%) was shared with ND. Of the 39% of the unique environmental component contributing to ND, 2% (95% CI:4–6%) was shared with PPG.
When comparing PPG and CAD, of the 48% genetic variance observed in PPG, 5% (95% CI:1–54%) was shared with CAD. Of the 28% genetic variance contribution to CAD, 3% (95% CI:1–9%) was shared with PPG. The unique environmental component accounted for 52% (95% CI:42–62%) of the variance in PPG and 39% (95% CI:30–49%) of that observed in CAD. Of the 52% of the unique environmental component contributing to PPG, 7% (95% CI:1–16%) was shared with CAD. Of the 39% of the unique environmental component contributing to CAD, 5% (95% CI:1–12%) was shared with PPG.
When comparing PPG and SAD, of the 50% genetic variance observed in PPG, 17% (95%CI:10–26%) was shared with SAD. Of the 54% genetic variance contribution to SAD, 17% (95% CI:10–26%) was shared with PPG. The unique environmental component accounted for 50% (95% CI:43–61%) of the variance in PPG and 46% (95% CI:35–59%) of that observed in SAD; however, there was no unique environmental overlap between PPG and SAD. Thus, the overlap between PPG and SAD appeared entirely genetic in nature.
DISCUSSION
The hypothesis that individual classes of drug-use disorders would be frequently comorbid with PPG was confirmed in both unadjusted and adjusted models. PPG and all three classes of drugs (ND, CAD and SAD) remained elevated following adjustments for sociodemographic, externalizing and internalizing psychiatric variables, with the exception of CAD (which approached significance). The results from the tetrachoric correlations and bivariate models for PPG and drug-use disorders are consistent with the hypothesis that common environmental and genetic factors contribute to the co-occurrence of PPG and ND. Our third hypothesis was partially supported in that models indicated solely genetic contributions to the co-occurrence of PPG and SAD, whereas both common environmental and genetic factors contributed to the co-occurrence of PPG and CAD.
This study has clinical significance in both understanding of comborbid drug use with PPG and developing targeted interventions. First, the shared environmental contribution to PPG and ND and PPG and CAD suggest that environmental factors may contribute significantly to the co-occurrence of gambling and licit/”soft” drug-use disorders. Multiple factors (multiple genes and environmental factors relating to peers, parents, perceptions and other factors) have been proposed to contribute to gambling and substance-use disorders amongst youth and adults [29, 30]. While the current study does not identify specific factors, one possibility relates to accessibility. Increased rates of substance use have been found in contexts where drug accessibility is greater and where there are strong social influences such as substance-using peers [31–35]. The extent to which accessibility might influence the co-occurrence of PPG and ND warrants additional examination. For example, as cigarettes and lottery tickets may be purchased in common venues such as convenience stores, improving interventions (particularly for youth who may purchase such products illegally) should be examined further [36]. Although such efforts have not been examined to our knowledge, data linking early age of gambling, lottery gambling and problem-gambling severity in youth suggest a need for such studies [37]. Additional environmental factors that might contribute to both PPG and ND (like tobacco smoking in casinos) also warrant consideration, particularly given the increased accessibility in the United States of casino gambling over the past several decades. The extent to which peer influences might influence the co-occurrences of PPG and ND and PPG and CAD also warrants additional investigation. Limiting accessibility and targeting peer influences may influence the initiation and maintenance of inter-related ND, CAD and PPG behaviors, although this hypothesis warrants direct investigation.
It has been reported that when examining genetic and environmental variances, the relationship between drug availability and drug-use disorders differs for stimulants as compared to tobacco and cannabis [38, 39]. For example, with cigarette availability, there is an increase in additive genetic variance and a decrease in shared environmental variance over time [38]. Shared environmental contributions to cannabis use peak between 12 and 17 years and then decline and instead are favored for additive genetic factors. However, for stimulants, additive genetic factors account for more of the variance between ages 8 and 17 years, and then there is an increase in the variance explained by shared environmental variance. As stimulants did not share a pattern observed with other classes of drug-use disorders, it suggests that there may be different risk factors and outcomes for SADs compared to other drug-use disorders with respect to their co-occurrence with PPG [38].
It may be that “harder” drugs, as represented by stimulants (including cocaine) in the current study, have lower accessibility and carry greater consumption-related risks, particularly at the time of data collection for this study [39]; as such, there may be higher thresholds for use and consumption may be mediated more so by hereditary components. The stronger genetic association that exists between PPG and stimulants might relate to shared underlying neurobiologies relating to dopaminergic or noradrenergic systems and/or interactive effects of stimulants and gambling [40]. Additionally, the psychoactive property of stimulants versus cannabis and nicotine may relate to the magnitude of the genetic contributions to the co-occurrence of PPG and drug-use disorders. Neurochemical factors linking gambling and stimulants may overlap at a genetic level to a greater extant than do gambling and nicotine or cannabis. Stimulants, perhaps through dopaminergic and/or adrenergic mechanisms, have been linked with gambling behaviors [41], with stimulants having been found to promote gambling motivations and behaviors [42]. While some research suggests that common genetic elements relating to the dopamine system might underlie PPG and SAD and substance-use disorders more broadly (e.g., with respect to allelic variations in genes coding for dopamine receptors) [43], other data do not support such findings [44]. Further research is needed to identify specific genetic factors underlying the co-occurrence of PPG and SAD and to translate these findings into improved interventions. As shared genetic contributions were also identified for PPG and ND and PPG and CAD, studies examining nicotinic and cannabinoid genes and neurochemicals are warranted in PPG.
Limitations
Several limitations exist. First, as data were collected in 1992, the findings may not extend fully to the current gambling and drug-use environments that include greater availability of gambling and possibly differential accessibility of drugs (e.g., arguably greater accessibility of methamphetamine and lesser accessibility of crack cocaine) and gambling (e.g., greater accessibility of casinos and Internet gambling). Additionally, there are different trends in substance-use behaviors, with smoking no longer as socially acceptable in public places, decreased frequency of SAD, and increased frequency of CAD [45]. Attitudes towards certain drugs may have also changed, with increased knowledge of the health risks of tobacco more prevalent and increased acceptance towards cannabis as reflected in more states in the US having legalized its use. Despite these differences, several studies suggest that relationships between gambling and alcohol-, tobacco- and other drug-use disorders have remained relatively consistent across time [9, 12]. These relationships, consistent with those in current sample, suggest that the reported findings may generalize to the current environment, although this warrants direct examination, particularly as some other data (including those from the VET sample) suggest that alterations in socio-cultural factors in the environment may contribute differentially to PPG across time [46]. Second, the sample included only males; therefore, the results may not generalize to women, and future studies should examine the relationship between PPG and drug-use disorders in women. Such studies are particularly relevant given gender-related differences in environmental factors contributing to substance use and gambling [10], even though studies have found similar genetic and environmental contributions to PPG in women and men. Third, due to the cross-sectional nature of the data, we could not examine the temporal relationship between drug-use disorders and PPG. Future longitudinal studies would help better understand the relationships between PPG and drug-use disorders. Fourth, the extent to which PPG represents a reasonable threshold for considering problematic gambling may be questioned. Using more stringent thresholds in analyses generated similar results (data not shown), with the exception that significance levels were more robust using the current approach, likely due to the larger sample of individuals with PPG versus pathological gambling. Fifth, drug-use disorders were based on self-report. Although toxicological screening may be helpful in verifying current diagnoses, the current study’s use of validated diagnostic-interview methodologies is a strength. Six, the diagnostic criteria for gambling and substance-use disorders in DSM-5 differ from those used in the present study. Future studies should examine the potential impact of changes in diagnostic criteria on the relationships between gambling and drug-use disorders, as has been recently done for gambling and alcohol use disorders [47].
Conclusion
In conclusion, our findings suggest different patterns of genetic and environmental contributions to the co-occurrence of PPG and different drug-use disorders among adult males. The predominantly genetic contributions to the co-occurrence of PPG and SAD as compared to the combination of genetic and environmental contributions to the co-occurrences of PPG and ND and PPG and CAD suggest that biological mechanisms linking gambling to specific drug-use disorders may differ. As a result, interventions targeting the co-occurrences of specific addictive behaviors may vary, with the environmental contributions to the co-occurrences of PPG and ND and PPG and CAD suggesting consideration of interventions targeting environmental factors that might link the behaviors.
Supplementary Material
Acknowledgements
We would like to acknowledge the continual cooperation and participation of the VET-R members and their families. We greatly appreciate their assistance and without them this research would not have been possible. We would like to thank the numerous organizations that have provided assistance for the conductance of this study, including the Department of Defense (Washington, DC); National Personnel Records Center (St Louis, MO); National Archives and Records Administration (College Park, MD); Internal Revenue Service (Washington, DC); National Opinion Research Center (Chicago, IL); National Research Council (Washington); National Academy of Sciences (Washington, DC); and Institute for Survey Research, Temple University (Philadelphia, PA).This work was supported in part by the NIH (MH60426, P20 DA027844), the Connecticut Mental Health Center, the Connecticut Department of Mental Health and Addictive Services and a Center of Excellence in Gambling Research Award from the National Center for Responsible Gaming. The funding from the National Center for Responsible Gaming was obtained through a peer-review process involving a grant application in response to a request for applications. The applications received were then evaluated by an independent scientific review group. Next, the evaluations were reviewed by a scientific advisory board. This procedure is modeled after that employed by NIH. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Responsible Gaming or any of the other funding agencies. The funding agencies had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
Conflicts of Interest/Disclosures: Dr. Potenza has received financial support or compensation from several sources that may represent a conflict of interest. Dr. Potenza has consulted for and advised Boehringer Ingelheim, Lundbeck and Ironwood; has had financial interests in Somaxon; has received research support from Mohegan Sun Casino, the National Center for Responsible Gaming, and Forest Laboratories and Psyadon pharmaceuticals; has consulted for law offices and gambling entities on issues related to addictions or impulse-control disorders. The National Center for Responsible Gaming is supported by the gambling industry. Dr. Potenza’s grant support from the National Center for Responsible Gaming underwent NIH-style peer-review from an independent scientific review group. All other authors report no disclosures. The content of the manuscript reflects the thoughts of the authors and not necessarily the funding agencies (specifically, the funding agencies had no input into the content of the manuscript).
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Revised 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.Potenza MN. Should addictive disorders include non-substance-related conditions? Addiction. 2006;101(S1):142–151. doi: 10.1111/j.1360-0443.2006.01591.x. [DOI] [PubMed] [Google Scholar]
- 3.Petry NM. Should the scope of addictive behaviors be broadened to include pathological gambling? Addiction. 2006;101(S1):152–160. doi: 10.1111/j.1360-0443.2006.01593.x. [DOI] [PubMed] [Google Scholar]
- 4.Holden C. Psychiatry. Behavioral addictions debut in proposed DSM-V. Science. 2010;327:935. doi: 10.1126/science.327.5968.935. [DOI] [PubMed] [Google Scholar]
- 5.Cunningham-Williams RM, Hong SI. A Latent Class Analysis (LCA) of problem gambling among a sample of community-recruited gamblers. J Nerv Mental Dis. 2007;195(11):939–947. doi: 10.1097/NMD.0b013e31815947e1. [DOI] [PubMed] [Google Scholar]
- 6.Jazaeri SA, Habil MH. Reviewing two types of addiction - pathological gambling and substance use. Indian J Psychol Med. 2012;34(1):5–11. doi: 10.4103/0253-7176.96147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnes GM, Welte JW, Hoffman JH, Dintcheff BA. Shared predictors of youthful gambling, substance use, and delinquency. Psychol Addict Behav. 2005;19(2):165–174. doi: 10.1037/0893-164X.19.2.165. [DOI] [PubMed] [Google Scholar]
- 8.Petry NM, Stinson FS, Grant BF. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66(5):564–574. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- 9.Desai RA, Potenza MN. Gender differences in the associations between past-year gambling problems and psychiatric disorders. Soc Psychiatry Psychiatr Epi. 2008;43(3):173–183. doi: 10.1007/s00127-007-0283-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nower L, Derevensky JL, Gupta R. The relationship of impulsivity, sensation seeking, coping, and substance use in youth gamblers. Psychol Addict Behav. 2004;18(1):49–55. doi: 10.1037/0893-164X.18.1.49. [DOI] [PubMed] [Google Scholar]
- 11.Slutske WS, Eisen S, True WR, Lyons MJ, Goldberg J, Tsuang M. Common genetic vulnerability for pathological gambling and alcohol dependence in men. Arch Gen Psychiatry. 2000;57(7):666–673. doi: 10.1001/archpsyc.57.7.666. [DOI] [PubMed] [Google Scholar]
- 12.Cunningham-Williams RM, Cottler LB, Compton WM, 3rd, Spitznagel EL. Taking chances: Problem gamblers and mental health disorders - Results form the St. Louis Epidemiologic Catchment Area Study. Am J Public Health. 1998;88(7):1093–1096. doi: 10.2105/ajph.88.7.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barnes JC, Beaver KM, Boutwell BB. Examining the genetic underpinnings to Moffitt's developmental taxonomy: A behavioral genetic analysis. Criminology. 2011;49(4):923. [Google Scholar]
- 14.Saxon AJ, Oreskovich MR, Brkanac Z. Genetic determinants of addiction to opioids and cocaine. Harv Rev Psychiatry. 2005;13(4):218–232. doi: 10.1080/10673220500243364. [DOI] [PubMed] [Google Scholar]
- 15.Tsuang MT, Bar JL, Harley RM, Lyons MJ. The Harvard Twin Study of Substance Abuse: what we have learned. Harv Rev Psychiatry. 2001;9(6):267–279. [PubMed] [Google Scholar]
- 16.Slutske WS, Eisen S, Xian H, True WR, Lyons MJ, Goldberg J, et al. A twin study of the association between pathological gambling and antisocial personality disorder. J Abnorm Psychol. 2001;110(2):297–308. doi: 10.1037//0021-843x.110.2.297. [DOI] [PubMed] [Google Scholar]
- 17.Potenza MN, Xian H, Shah K, Scherrer JF, Eisen SA. Shared genetic contributions to pathological gambling and major depression in men. Arch Gen Psychiatry. 2005;62(9):1015–1021. doi: 10.1001/archpsyc.62.9.1015. [DOI] [PubMed] [Google Scholar]
- 18.Giddens JL, Xian H, Scherrer JF, Eisen SA, Potenza MN. Shared genetic contributions to anxiety disorders and pathological gambling in a male population. J Affect Disord. 2011;132(3):406–412. doi: 10.1016/j.jad.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah KR, Eisen SA, Xian H, Potenza MN. Genetic studies of pathological gambling: a review of methodology and analyses of data from the Vietnam Era Twin Registry. J Gambl Stud. 2005;21(2):179–203. doi: 10.1007/s10899-005-3031-x. [DOI] [PubMed] [Google Scholar]
- 20.Eisen S, True W, Goldberg J, Henderson W, Robinette CD. The Vietnam Era Twin (VET) Registry: method of construction. Acta Genet Med Gemellol. 1987;36(1):61–66. doi: 10.1017/s0001566000004591. [DOI] [PubMed] [Google Scholar]
- 21.Robins LN, Regier DA. Psychiatric disorders in America. New York, NY, USA: New York Free Press; 1991. [Google Scholar]
- 22.Tsuang MT, Lyons MJ, Eisen SA, Goldberg J, True W, Lin N, et al. Genetic influences on DSM-III-R drug abuse and dependence: a study of 3,372 twin pairs. Am J Med Genet. 1996;67(5):473–477. doi: 10.1002/(SICI)1096-8628(19960920)67:5<473::AID-AJMG6>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 23.Xian H, Scherrer JF, Eisen SA, Lyons MJ, Tsuang M, True WR, et al. Nicotine dependence subtypes: association with smoking history, diagnostic criteria and psychiatric disorders in 5440 regular smokers from the Vietnam Era Twin Registry. Addict Behav. 2007;32(1):137–147. doi: 10.1016/j.addbeh.2006.03.031. [DOI] [PubMed] [Google Scholar]
- 24.Slutske WS, Jackson KM, Sher KJ. The natural history of problem gambling from age 18 to 29. J Abnorm Psychol. 2003;112(2):263–274. doi: 10.1037/0021-843x.112.2.263. [DOI] [PubMed] [Google Scholar]
- 25.Smart RG, Ferris J. Alcohol, drugs and gambling in the Ontario adult population, 1994. Can J Psychiatry. 1996;41(1):36–45. doi: 10.1177/070674379604100109. [DOI] [PubMed] [Google Scholar]
- 26.Chou KL, Afifi TO. Disordered (pathologic or problem) gambling and axis I psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Am J Epidemiol. 2011;173(11):1289–1297. doi: 10.1093/aje/kwr017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler RC, Hwang I, LaBrie R, Petukhova M, Sampson NA, Winters KC, et al. DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psycholog Med. 2008;38(9):1351–1360. doi: 10.1017/S0033291708002900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neale MC, Cardon LR. Dordrecht. The Netherlands: Kluwer Academic Publishers; 1992. Methodology for genetic studies of twins and families. [Google Scholar]
- 29.Wickwire EM, Jr., Whelan JP, West R, Meyers A, McCausland C, Leullen J. Perceived availability, risks, and benefits of gambling among college students. J Gambl Stud. 2007;23(4):395–408. doi: 10.1007/s10899-007-9057-5. [DOI] [PubMed] [Google Scholar]
- 30.Dickson L, Dervensky JL, Gupta R. Youth gambling problems: Examining risk and protective factors. Int Gambl Stud. 2008;8(1):25–47. [Google Scholar]
- 31.Dembo R, Schmeidler J, Burgos W. Factors in the drug involvement of inner city junior high school youths: a discriminant analysis. Int J Soc Psychiatry. 1979;25(2):92–103. doi: 10.1177/002076407902500204. [DOI] [PubMed] [Google Scholar]
- 32.Freisthler B, Needell B, Gruenewald PJ. Is the physical availability of alcohol and illicit drugs related to neighborhood rates of child maltreatment? Child Abuse Negl. 2005;29(9):1049–1060. doi: 10.1016/j.chiabu.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 33.Freisthler B, Gruenewald PJ, Johnson FW, Treno AJ, Lascala EA. An exploratory study examining the spatial dynamics of illicit drug availability and rates of drug use. J Drug Educ. 2005;35(1):15–27. doi: 10.2190/25QY-PBC3-B1EB-JB5Y. [DOI] [PubMed] [Google Scholar]
- 34.Alexander C, Piazza M, Mekos D, Valente T. Peers, schools, and adolescent cigarette smoking. J Adolesc Health. 2001;29(1):22–30. doi: 10.1016/s1054-139x(01)00210-5. [DOI] [PubMed] [Google Scholar]
- 35.Korf DJ. Dutch coffee shops and trends in cannabis use. Addict Behav. 2002;27(6):851–866. doi: 10.1016/s0306-4603(02)00291-5. [DOI] [PubMed] [Google Scholar]
- 36.Byrne AM, Dickson L, Derevensky JL, Gupta R, Lussier I. The application of youth substance use media campaigns to problem gambling: A critical evaluation. J Health Commun. 2005;10:681–700. doi: 10.1080/10810730500326658. [DOI] [PubMed] [Google Scholar]
- 37.Rahman AS, Pilver CE, Desai RA, Steinberg MA, Rugle L, Krishnan-Sarin S, et al. The relationship between age of gambling onset and adolescent problematic gambling severity. J Psychiatr Res. 2012;46(5):675–683. doi: 10.1016/j.jpsychires.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gillespie NA, Kendler KS, Prescott CA, Aggen SH, Gardner CO, Jr., Jacobson K, et al. Longitudinal modeling of genetic and environmental influences on self-reported availability of psychoactive substances: alcohol, cigarettes, marijuana, cocaine and stimulants. Psychol Med. 2007;37(7):947–959. doi: 10.1017/S0033291707009920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lynskey MT, Heath AC, Bucholz KK, Slutske WS, Madden PA, Nelson EC, et al. Escalation of drug use in early-onset cannabis users vs co-twin controls. JAMA. 2003;289(4):427–433. doi: 10.1001/jama.289.4.427. [DOI] [PubMed] [Google Scholar]
- 40.Leeman RF, Potenza MN. Similarities and differences between pathological gambling and substance use disorders: a focus on impulsivity and compulsivity. Psychopharmacol. 2012;219(2):469–490. doi: 10.1007/s00213-011-2550-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zack M, Poulos CX. Parallel roles for dopamine in pathological gambling and psychostimulant addiction. Curr Drug Abuse Rev. 2009;2(1):11–25. doi: 10.2174/1874473710902010011. [DOI] [PubMed] [Google Scholar]
- 42.Zack M, Poulos CX. Amphetamine primes motivation to gamble and gambling-related semantic networks in problem gamblers. Neuropsychopharmacol. 2004;29(1):195–207. doi: 10.1038/sj.npp.1300333. [DOI] [PubMed] [Google Scholar]
- 43.Comings DE, Rosenthal RJ, Lesieur HR, Rugle LJ, Muhleman D, Chiu C, et al. A study of the dopamine D2 receptor gene in pathological gambling. Pharmacogenet. 1996;6(3):223–234. doi: 10.1097/00008571-199606000-00004. [DOI] [PubMed] [Google Scholar]
- 44.Lobo DS, Souza RP, Tong RP, Casey DM, Hodgins DC, Smith GJ, et al. Association of functional variants in the dopamine D2-like receptors with risk for gambling behaviour in healthy Caucasian subjects. Biol Psychol. 2010;85(1):33–37. doi: 10.1016/j.biopsycho.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 45.McCabe SE, Cranford JA, West BT. Trends in prescription drug abuse and dependence, co-occurrence with other substance use disorders, and treatment utilization: results from two national surveys. Addict Behav. 2008;33(10):1297–1305. doi: 10.1016/j.addbeh.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xian H, Scherrer JF, Slutske WS, Shah KR, Volberg R, Eisen SA. Genetic and environmental contributions to pathological gambling symptoms in a 10-year follow-up. Twin Res Hum Genet. 2007;10(1):174–179. doi: 10.1375/twin.10.1.174. [DOI] [PubMed] [Google Scholar]
- 47.Slutske WS, Ellingson JM, Richmond-Rakerd LS, Zhu G, Martin NG. Shared genetic vulnerability for disordered gambling and alcohol use disorder in men and women: Evidence from a national community-based Australian twin study. Twin Res Hum Genet. 2013;16(2):525–534. doi: 10.1017/thg.2013.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.