Abstract
Background
Little information exists on lifestyle factors that affect prognosis after treatment for ductal carcinoma in situ (DCIS) breast cancer. Improved understanding of the role of lifestyle factors is important to survivors wishing to reduce their risk of a second breast cancer diagnosis.
Methods
We examined the association between body mass index (BMI), physical activity, and alcohol intake and risk of a second breast cancer diagnosis among 1,925 DCIS survivors in the Wisconsin In Situ Cohort. Exposures were self-reported during biennial patient interviews. Second breast cancer diagnoses were validated via pathology report. Cox proportional hazards regression was used to estimate the association between pre-diagnosis, post-diagnosis, and change in exposure levels and the risk of a second diagnosis, with adjustment for patient, tumor, and treatment factors.
Results
Over a mean of 6.7 years of follow-up, 162 second breast cancer diagnoses were reported, including 57 invasive events, 60 in situ events, and 45 diagnoses of unknown stage. A significant trend of increasing risk of a second diagnosis was found over increasing categories of post-diagnosis alcohol intake (ptrend=0.02). Among premenopausal women, increased pre-diagnosis BMI was associated with a reduced risk of a second diagnosis (HR 0.93, 95% CI 0.88-0.99).
Conclusion
DCIS survivors may reduce their risk of a second diagnosis by reducing post-diagnosis alcohol consumption.
Impact
The population of DCIS survivors is projected to surpass 1 million by the year 2016. Our results suggest that these women may be able to reduce their risk of a second diagnosis through moderation of alcohol consumption.
Introduction
Ductal carcinoma in situ (DCIS) is a non-invasive breast cancer characterized by the development of malignant cells that are confined to the basement membrane of the breast duct (1). The incidence of DCIS has increased steadily since the 1980s (2), mirroring the rise in screening mammography (3). Although overall survival after treatment for DCIS is high (5-year disease-specific survival rates approach 100%) (2), the risk of developing invasive breast cancer is 4-fold higher for women with a DCIS diagnosis compared to the general population (4).
Given the large numbers of DCIS survivors and the increased risk of subsequent breast cancer diagnoses in this population, research specific to the prevention of second events is needed. A number of tumor factors have been identified that are associated with an increased likelihood of a second breast cancer diagnosis, including nuclear grade, larger tumor size, and detection by palpation rather than mammography (5). However, little information exists on lifestyle factors that may affect prognosis after a DCIS diagnosis and may be useful to DCIS survivors wishing to reduce their risk of a second event.
Elevated BMI, physical activity, and alcohol consumption have been established as risk factors for both primary invasive and DCIS breast cancer (6-11). Studies have also examined these factors in relation to recurrence after an invasive breast cancer diagnosis, with suggestive but inconclusive results (12-20). There is very little evidence regarding the impact of these lifestyle factors on the risk of a second breast cancer diagnosis after DCIS. A single study of BMI and second breast cancer diagnoses in a DCIS population reported a twofold increase in risk for those who were obese at diagnosis compared to those who were normal weight (21). To our knowledge, no studies have assessed post-diagnosis BMI, physical activity, or alcohol intake and the risk of second breast cancer events in an exclusively DCIS population.
We examined the association of BMI, physical activity, and alcohol intake with the risk of a second in situ or invasive breast cancer diagnosis in a large, population-based cohort of DCIS survivors. Measurements of exposure at pre-diagnosis, post-diagnosis, and the change from pre- to post-diagnosis were considered.
Materials and Methods
Study population
Details of the Wisconsin In Situ Cohort (WISC) have been described previously (22). Briefly, the cohort enrolled women with a first primary diagnosis of non-invasive breast cancer reported to the mandatory Wisconsin Cancer Reporting System during 1997-2006. The current study population includes 1,925 women with a first primary DCIS diagnosis, and is comprised of 838 incident DCIS cases recruited for a case-control study during 1997-2001 (23, 24) and 1087 additional cases recruited during 2002-2006. All participants in the cohort were female residents of Wisconsin age 20-74 at diagnosis. Eligibility was limited to cases with a known date of diagnosis, a listed telephone number, and the ability to conduct a telephone interview. All subjects provided verbal informed consent and the study was approved by the University of Wisconsin Health Sciences Institutional Review Board.
Data collection
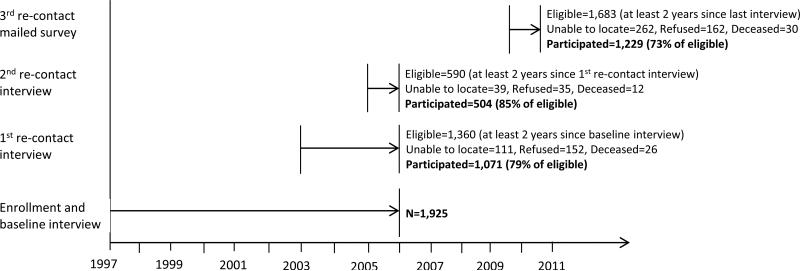
All participants completed a baseline telephone interview at enrollment into the study (median of 1.3 years after diagnosis). Follow-up interviews were conducted biennially starting in 2003 and are on-going. Interviews were conducted by telephone until 2010, at which point a mailed survey was utilized. The current study uses data collected through 2010 and includes a baseline and up to three follow-up interviews (Figure 1). A woman was eligible for re-contact if at least two years had passed since her last interview. Because enrollment and re-contact periods overlapped, not all women were eligible for each cycle of re-contact interviews. Of the women eligible for a first re-contact interview, 79% participated; of those who were eligible for a second re-contact interview, 85% participated; and of those who were eligible for a third re-contact (mailed survey), 73% participated.
Figure 1.
Study timeline and participation rates: WISC 1997-2010
Breast cancer second events
During each interview, women were asked to self-report new breast cancer diagnoses. In years that women were not contacted, a questionnaire was mailed to each subject for reporting new diagnoses. For the purposes of these analyses, a second event was defined as any second breast cancer diagnosis (invasive or in situ), and includes ipsilateral events, contralateral events, and events of unknown laterality. Pathology reports were requested to confirm the self-reported diagnoses. Of the 126 self-reported diagnoses for which pathology information could be gathered, 117 were verified and 9 were refuted (93% accuracy). Pathology reports were unavailable for an additional 45 self-reported diagnoses as a result of patient or facility refusal to disclose records, and were included as second events in these analyses.
Behavioral characteristics
All exposure information was assessed via self-report during telephone interviews (1997-2006) or mailed survey (2010). During the baseline interview, subjects were asked to report their current weight, their weight at one year pre-diagnosis, and their height. Current weight was subsequently reported at each re-contact interview or survey. BMI at each data collection period was then calculated from the self-reported weights and height.
Information was gathered at baseline on regular participation in recreational physical activity at one year pre-diagnosis using a questionnaire patterned after the Nurses’ Health Study that had been previously validated (25). Physical activity categories included: jogging, running, bicycling, racquet sports, aerobics/dance, swimming, walking/hiking, and other strenuous activity. Subjects reported the hours per week spent on the activity and the number of months per year in which the activity was performed. Recreational physical activity was updated at each subsequent interview, with subjects reporting their regular participation in strenuous exercises or sports over the past year in an open-ended question. This assessment of physical activity during follow-up has demonstrated an association between physical activity and breast cancer risk in previous analysis within the WISC cohort (26). In all assessments, activities performed for at least 30 minutes per week for at least 3 months of the year were considered regular. A variable was created for each data collection period to reflect the average total hours per week spent on regular recreational physical activity.
Subjects reported the number of bottles or cans of beer, glasses of wine, and drinks of hard liquor consumed per day, week, or month at one year pre-diagnosis at the baseline interview. The same information was gathered during subsequent interviews in reference to typical alcohol consumed over the past year. This information was used to create a variable representing the total drinks consumed per week for each data collection period.
Information on reproductive and menstrual histories, past and current exogenous hormone use, medication use, medical and family history, mammographic screening history, method of tumor detection (screening mammography or symptomatic), and demographics was obtained during the baseline and follow-up interviews or survey. Tumor characteristics for the initial DCIS diagnosis were obtained from the Wisconsin Cancer Registry, which receives mandatory cancer diagnosis reports from physicians, hospitals, and clinics across Wisconsin. Tumor characteristics included date of diagnosis, histology, laterality, grade, and tumor size. The registry also provided treatment information for the initial DCIS breast cancer, including treatment type and date of treatment.
Statistical analysis
Descriptive characteristics of the study population were examined overall and by outcome status. Missing values for all covariates and for exposures at each data collection period were estimated using multiple imputation with ten imputations (27). The imputation model included all covariates listed in Table 1 in addition to mammographic screening history, age at first birth, age at menarche, and history of breast biopsy and benign breast disease, all assessed at the baseline interview. Regression analyses used the combined results of the ten imputations to create valid statistical inferences that account for the uncertainty created by the missing values (28, 29). Where variables with imputed values were categorized for presentation, classification of subjects into categories was based on the mode (categorical) or mean (continuous) of the ten estimated values for each subject created under the imputation model.
Table 1.
Pre-diagnosis subject characteristics and distribution of second breast cancer diagnoses; N (%): WISC DCIS cohort, 1997-2010
| Total N=1,925 | Second breast cancer diagnosis N=162 | No second breast cancer diagnosis N=1,763 | P valuea | |
|---|---|---|---|---|
| Age at diagnosis (years) | 0.13 | |||
| 20-44 | 238 (12.4) | 21 (13.0) | 217 (12.3) | |
| 45-54 | 684 (35.5) | 66 (40.7) | 618 (35.1) | |
| 55-64 | 585 (30.4) | 36 (22.2) | 549 (31.1) | |
| 65-74 | 418 (21.7) | 39 (24.1) | 379 (21.5) | |
| Menopausal status | 0.01 | |||
| Premenopausal | 617 (32.1) | 70 (43.2) | 547 (31.0) | |
| Postmenopausal | 1147 (59.6) | 82 (50.6) | 1065 (60.4) | |
| Unknown | 161 (8.4) | 10 (6.2) | 151 (8.6) | |
| First degree family history of breast cancer | 0.85 | |||
| No | 1380 (71.7) | 114 (70.4) | 1266 (71.8) | |
| Yes | 430 (22.3) | 39 (24.1) | 391 (22.2) | |
| Unknown | 115 (6.0) | 9 (5.6) | 106 (6.0) | |
| Postmenopausal hormone use | <0.01 | |||
| Never | 1287 (66.9) | 129 (79.6) | 1158 (65.7) | |
| Ever | 587 (30.5) | 30 (18.5) | 557 (31.6) | |
| Unknown | 51 (2.7) | 3 (1.9) | 48 (2.7) | |
| Parity | 0.55 | |||
| No births | 270 (14.0) | 27 (16.7) | 243 (13.8) | |
| One birth | 197 (10.2) | 13 (8.0) | 184 (10.4) | |
| Two births | 594 (30.9) | 53 (32.7) | 541 (30.7) | |
| 3+ births | 839 (43.6) | 67 (41.4) | 772 (43.8) | |
| Unknown | 25 (1.3) | 2 (1.2) | 23 (1.3) | |
| Education | 0.37 | |||
| < High school diploma | 93 (4.8) | 5 (3.1) | 88 (5.0) | |
| High school diploma | 736 (38.2) | 64 (39.5) | 672 (38.1) | |
| Some college | 514 (26.7) | 47 (29.0) | 467 (26.5) | |
| College degree | 552 (28.7) | 46 (28.4) | 506 (28.7) | |
| Unknown | 30 (1.6) | 0 | 30 (1.7) | |
| Smoking Status | 0.38 | |||
| Never | 1053 (54.7) | 88 (54.3) | 965 (54.7) | |
| Former | 557 (28.9) | 54 (33.3) | 503 (28.5) | |
| Current | 288 (15.0) | 20 (12.4) | 268 (15.2) | |
| Unknown | 27 (1.4) | 0 | 27 (1.5) | |
| Surgical treatment | <0.01 | |||
| Ipsilateral mastectomy | 593 (30.8) | 41 (25.3) | 552 (31.3) | |
| Bilateral mastectomy | 81 (4.2) | 0 | 81 (4.6) | |
| BCS without radiation | 176 (9.1) | 28 (17.3) | 148 (8.4) | |
| BCS with radiation | 826 (42.9) | 74 (45.7) | 752 (42.7) | |
| Biopsy only | 49 (2.6) | 7 (4.3) | 42 (2.4) | |
| Unknown | 200 (10.4) | 12 (7.4) | 188 (10.7) | |
| Tamoxifen use (excluding after recurrence) | 0.02 | |||
| No | 1039 (54.0) | 105 (64.8) | 934 (53.0) | |
| Yes | 638 (33.1) | 44 (27.2) | 594 (33.7) | |
| Unknown | 248 (12.9) | 13 (8.0) | 235 (13.3) | |
| Mode of detection | 0.41 | |||
| Mammography | 1595 (82.9) | 129 (79.6) | 1466 (83.2) | |
| Symptomatic | 266 (13.8) | 28 (17.3) | 238 (13.5) | |
| Unknown | 64 (3.3) | 5 (3.1) | 59 (3.3) | |
P value for Chi-square test comparing women with and without a second breast cancer diagnosis among those with known covariate status
Cox proportional hazards regression was used to estimate the crude and multivariable-adjusted hazard ratios (HR) for the associations between the exposures and outcomes. Follow-up time for each subject was defined as the time from initial DCIS diagnosis to the date of a second breast cancer diagnosis or date of last contact or death. The multivariable models were adjusted for the following confounding factors that were selected a priori based on previous literature (15, 16, 18, 19, 30, 31) and included: age at diagnosis, menopausal status, method of detection, surgical treatment type, radiation therapy, tamoxifen use, year of diagnosis, tumor size, and tumor grade. Each exposure was additionally adjusted for the remaining two exposures (e.g., the analysis for BMI was adjusted for physical activity and alcohol intake). The post-diagnosis analyses were further adjusted for pre-diagnosis values of the exposures.
To make use of the post-diagnosis measurement of each exposure at each data collection period, repeated measures were incorporated in the Cox proportional hazard model in the post-diagnosis analyses. BMI, physical activity, and alcohol intake were treated as time-dependent variables and updated with the most relevant values during the analysis (32). Entry into the post-diagnosis model was at the time of the first interview assessing post-diagnosis exposures (baseline interview for the evaluation of BMI and first re-contact interview for the evaluation of physical activity and alcohol intake). Second breast cancer diagnoses that occurred before the entry time were excluded from each analysis.
Change in exposure was calculated as the difference in exposure level between pre-diagnosis and each post-diagnosis data collection period. Annualized rates of change were established by dividing the change in exposure by the time interval of the change in years to account for differences in the spacing of patient interviews and surveys. The annualized rates of change were included in the multivariable models as time-dependent variables and updated with the relevant values during the analysis. Categories for the annualized rate of change were chosen to reflect a change of approximately 1 kg/m2 for BMI, 1 hour/week for physical activity, and 0.5 drinks/week for alcohol intake over the mean follow-up period. Models for change in exposure were additionally adjusted for time since diagnosis.
Effect modification was evaluated by entering cross-product terms in the multivariable model using the time-dependent exposure variables. Menopausal status, postmenopausal hormone use, type of surgical treatment for original DCIS, and tamoxifen use were tested in each model as potential effect modifiers. Interactions were considered significant at the p ≤ 0.05 level. Where significant interaction was observed, results were stratified by levels of the effect modifier and presented separately.
Forty-five of the 162 second breast cancer events included in these analyses were not confirmed via pathology report as a result of patient or facility refusal to disclose records. A sensitivity analysis was performed excluding these 45 self-reported diagnoses to assess the robustness of our results. Since second diagnoses of invasive breast cancer are of particular importance, exploratory analyses were performed using only invasive second events as the outcome variable using the same multivariable models and methods described above.
All statistical analysis was performed using SAS statistical software Version 9.2 (SAS Institute Inc., Cary, North Carolina).
Results
Over an average of 6.7 years of follow-up (range 0.4 – 15.3 years), 162 second breast cancer events were observed. Of the 117 second events that could be confirmed via pathology report, 57 (49%) were invasive diagnoses and 60 (51%) were in situ diagnoses. Characteristics of the study population are provided in Table 1. Women with any second breast cancer diagnosis were more likely to be premenopausal and to have never taken hormone therapy. These women were also more likely to have elected breast conserving surgery (BCS) as opposed to mastectomy as surgical treatment and were less likely to have used tamoxifen following their original diagnosis (Table 1).
BMI was not associated with the risk of any second breast cancer event in the full cohort (pre-diagnosis HR=0.99, 95% CI 0.96-1.02; post-diagnosis HR 1.03, 95% CI 0.97-1.10 per 1 kg/m2) (Table 2). However, the relation between both pre- and post-diagnosis BMI and risk of a second breast cancer diagnosis was significantly modified by menopausal status (pinteraction < 0.01). In premenopausal women, a statistically significant decrease in risk was observed with increasing pre-diagnosis BMI (HR 0.93, 95% CI 0.88-0.99), and premenopausal women who were obese at pre-diagnosis were at significantly reduced risk compared to normal weight counterparts (HR 0.23, 95% CI 0.07-0.71) (Table 2). A similar inverse association was observed between premenopausal BMI and risk of an invasive second breast cancer diagnosis (HR 0.87, 95% CI o.74-0.99). There was no association between post-diagnosis BMI and risk of any second event or an invasive second event among premenopausal women. In postmenopausal women, no association was observed between pre- or post-diagnosis BMI and risk of any second breast cancer diagnosis (pre-diagnosis HR 1.03, 95% CI 0.99-1.06; post-diagnosis HR 1.03, 95% CI 0.94, 1.12); and these results did not change when examining invasive second events only (Table 2). The association between BMI and a second breast cancer event was not modified by postmenopausal hormone use, tamoxifen use, or type of treatment.
Table 2.
Hazard ratios and 95% confidence intervals for the association between body mass index (BMI) and the risk of a second breast cancer diagnosis: WISC DCIS cohort, 1997-2010
| All second breast cancer diagnoses |
Invasive second breast cancer diagnoses |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Second diagnosis | Pre-diagnosis (N=1925) | Post-diagnosis (N=1903)b | Second diagnosis | Pre-diagnosis (N=1925) | Post-diagnosis (N=1903)b | |||||
| HR (95% CI)a | Ptrendc | HR (95% CI)a | Ptrendc | HR (95% CI)a | Ptrendc | HR (95% CI)a | Ptrendc | |||
| All women (kg/m2) | ||||||||||
| <25.0 | 78 | 1.00 (Ref) | 0.27 | 1.00 (Ref) | 0.21 | 26 | 1.00 (Ref) | 0.75 | 1.00 (Ref) | 0.64 |
| 25-29.9 | 56 | 1.10 (0.77, 1.58) | 1.03 (0.60, 1.44) | 22 | 1.29 (0.71, 2.35) | 0.71 (0.32, 1.55) | ||||
| 30+ | 28 | 0.83 (0.53, 1.30) | 1.15 (0.52, 2.13) | 9 | 0.82 (0.38, 1.81) | 1.34 (0.44, 4.07) | ||||
| Continuous per 1 kg/m2 | 162 | 0.99 (0.96, 1.02) | 1.03 (0.97, 1.10) | 57 | 0.99 (0.94, 1.04) | 1.00 (0.90, 1.11) | ||||
| Premenopausal women (kg/m2) | ||||||||||
| <25.0 | 50 | 1.00 (Ref) | 0.19 | 1.00 (Ref) | 0.44 | 18 | 1.00 (Ref) | 0.04 | 1.00 (Ref) | 0.43 |
| 25-29.9 | 20 | 0.83 (0.48, 1.43) | 1.17 (0.54, 2.11) | 5 | 0.53 (0.18, 1.49) | 0.40 (0.11, 1.45) | ||||
| 30+ | 4 | 0.23 (0.07, 0.71) | 1.14 (0.33, 3.92) | 1 | 0.16 (0.02, 1.28) | 0.50 (0.05, 5.42) | ||||
| Continuous per 1 kg/m2 | 74 | 0.93 (0.88, 0.99) | 1.04 (0.95, 1.13) | 24 | 0.87 (0.74, 0.99) | 0.95 (0.82, 1.13) | ||||
| Postmenopausal women (kg/m2) | ||||||||||
| <25.0 | 28 | 1.00 (Ref) | 0.37 | 1.00 (Ref) | 0.22 | 8 | 1.00 (Ref) | 0.89 | 1.00 (Ref) | 0.22 |
| 25-29.9 | 36 | 1.53 (0.91, 2.57) | 1.04 (0.50, 1.79) | 17 | 1.93 (0.75, 4.13) | 1.26 (0.41, 3.88) | ||||
| 30+ | 24 | 1.50 (0.84, 2.66) | 1.21 (0.42, 2.45) | 8 | 1.17 (0.63, 4.95) | 2.39 (0.57, 10.1) | ||||
| Continuous per 1 kg/m2 | 88 | 1.03 (0.99, 1.06) | 1.03 (0.94, 1.12) | 33 | 1.03 (0.97, 1.10) | 1.03 (0.90, 1.18) | ||||
Adjusted for age at diagnosis, menopausal status, mode of detection, treatment type, postmenopausal hormone use, tamoxifen use, year of diagnosis, tumor size, tumor grade, and remaining lifetyle factors
Post-diagnosis results are additionally adjusted for pre-diagnosis levels of each lifestyle factor
P value is for linear trend across categories of each lifestyle factor
Pre- and post-diagnosis levels of physical activity were not significantly associated with risk of any second breast cancer diagnosis in the full cohort (pre-diagnosis HR 0.98, 95% CI 0.94-1.02, post-diagnosis HR 0.97, 95% CI 0.88-1.08), and these results were similar when considering only invasive second events (Table 3). A significant interaction was observed between physical activity and type of treatment for the original DCIS in the post-diagnosis analysis (pinteraction=0.01). A trend suggested that women treated with ipsilateral mastectomy had a reduced risk of any second breast cancer diagnosis with every additional hour per week of post-diagnosis physical activity (HR 0.67, 95% CI 0.45, 1.02; ptrend 0.07) (Table 3). In contrast, no association between post-diagnosis physical activity and risk of any second breast cancer diagnosis was observed for women treated with BCS with or without radiation (HR 0.99, 95% CI 0.88, 1.12). The low number of invasive second events among women treated with ipsilateral mastectomy precluded stratified analysis of post-diagnosis physical activity in this subgroup (Table 3). Likewise, small numbers of women treated with bilateral mastectomy and biopsy prohibited separate analysis of these treatment types. No significant interaction was observed between physical activity and menopausal status, postmenopausal hormone use, or tamoxifen use.
Table 3.
Hazard ratios and 95% confidence intervals for the association between physical activity and the risk of a second breast cancer diagnosis: WISC DCIS cohort, 1997-2010
| All second breast cancer diagnoses |
Invasive second breast cancer diagnoses |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Second diagnosis | Pre-diagnosis (N=1925) | Post-diagnosis (N=1903)b | Second diagnosis | Pre-diagnosis (N=1925) | Post-diagnosis (N=1903)b | |||||
| HR (95% CI)a | Ptrendc | HR (95% CI)a | Ptrendc | HR (95% CI)a | Ptrendc | HR (95% CI)a | Ptrendc | |||
| Total Physical Activity (hrs/week) | ||||||||||
| No activity | 44 | 1.00 (Ref) | 0.66 | 1.00 (Ref) | 0.90 | 17 | 1.00 (Ref) | 0.15 | 1.00 (Ref) | 0.08 |
| >0 -2 | 37 | 0.97 (0.62, 1.52) | 0.37 (0.12, 1.07) | 15 | 1.02 (0.50, 2.08) | 1.05 (0.20, 5.58) | ||||
| >2 -5 | 54 | 1.16 (0.77, 1.75) | 0.92 (0.47, 1.81) | 17 | 0.93 (0.47, 1.86) | 1.75 (0.55, 5.81) | ||||
| 5+ | 27 | 0.81 (0.49, 1.33) | 0.89 (0.36, 2.22) | 8 | 0.60 (0.25, 1.43) | 1.78 (0.41, 7.61) | ||||
| Continuous per 1 hr/week | 162 | 0.98 (0.94, 1.02) | 0.97 (0.88, 1.08) | 57 | 0.98 (0.91, 1.05) | 1.03 (0.90, 1.17) | ||||
| BCS with or without radiation (hours/week) | ||||||||||
| No activity | 27 | 1.00 (Ref) | 0.54 | 1.00 (Ref) | 0.58 | 11 | 1.00 (Ref) | 0.14 | 1.00 (Ref) | 0.24 |
| >0 -2 | 27 | 1.07 (0.62, 1.84) | 0.31 (0.07, 1.40) | 10 | 0.95 (0.39, 2.32) | 1.98 (0.27, 14.0) | ||||
| >2 -5 | 36 | 1.17 (0.70, 1.96) | 1.41 (0.61, 3.22) | 11 | 0.95 (0.39, 2.27) | 3.91 (0.82, 19.5) | ||||
| 5+ | 17 | 0.76 (0.40, 1.42) | 1.24 (0.39, 3.92) | 6 | 0.70 (0.25, 2.00) | 2.78 (0.37, 22.0) | ||||
| Continuous per 1 hour/week | 107 | 0.97 (0.92, 1.02) | 0.99 (0.88, 1.12) | 38 | 1.00 (0.92, 1.08) | 1.05 (0.90, 1.28) | ||||
| Ipsilateral mastectomy (hours/week) | ||||||||||
| No activity | 15 | 1.00 (Ref) | 0.18 | 1.00 (Ref) | 0.07 | 6 | d | d | ||
| >0 -2 | 10 | 1.03 (0.45, 2.35) | 0.40 (0.07. 2.23) | 5 | ||||||
| >2 -5 | 12 | 0.84 (0.37, 1.88) | 0.13 (0.01, 1.57) | 3 | ||||||
| 5+ | 8 | 0.72 (0.30, 1.75) | 0.06 (0.00, 1.51) | 1 | ||||||
| Continuous per 1 hour/week | 45 | 0.97 (0.88, 1.06) | 0.67 (0.45, 1.02) | 15 | ||||||
Adjusted for age at diagnosis, mode of detection, treatment type, postmenopausal hormone use, tamoxifen use, year of diagnosis, tumor size, tumor grade, and remaining lifetyle factors
Post-diagnosis results are additionally adjusted for pre-diagnosis levels of each lifestyle factor
P value is for linear trend across categories
Low numbers of invasive second breast cancer diagnoses among women treated with ipsilateral mastectomy precluded separate analysis of this subgroup
Although the risk estimates for individual categories of alcohol intake did not reach statistical significance, a significant linear trend of increasing risk of any second breast cancer diagnosis was observed over the categories of increasing post-diagnosis alcohol intake (p=0.02). When measured continuously, increases in risk of any second breast cancer diagnosis with increasing alcohol intake were not statistically significant in either the pre- or post-diagnosis analysis (pre-diagnosis HR 1.02, 95% CI 0.99, 1.05; post-diagnosis HR 1.03, 95% CI 0.94, 1.11) (Table 4). When considering only invasive second breast cancer diagnoses, risk estimates increased with increasing post-diagnosis alcohol intake, but the linear trend was no longer significant (p=0.15) (Table 4). No significant interaction was observed between alcohol intake and menopausal status, treatment type, postmenopausal hormone use, or tamoxifen use.
Table 4.
Hazard ratios and 95% confidence intervals for the association between alcohol consumption and the risk of a second breast cancer diagnosis: WISC DCIS cohort, 1997-2010
| All second breast cancer diagnoses |
Invasive second breast cancer diagnoses |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Second diagnosis | Pre-diagnosis (N=1925) | Post-diagnosis (N=1903)b | Second diagnosis | Pre-diagnosis (N=1925) | Post-diagnosis (N=1903)b | |||||
| HR (95% CI)a | Ptrendc | HR (95% CI)a | Ptrendc | HR (95% CI)a | Ptrendc | HR (95% CI)a | Ptrendc | |||
| Total Alcohol (drinks/week) | ||||||||||
| No alcohol | 27 | 1.00 (Ref) | 0.88 | 1.00 (Ref) | 0.02 | 9 | 1.00 (Ref) | 0.18 | 1.00 (Ref) | 0.15 |
| >0 - <2 | 80 | 0.98 (0.62, 1.53) | 1.28 (0.59, 2.78) | 25 | 0.95 (0.43, 2.08) | 1.38 (0.37, 5.47) | ||||
| 2 - <7 | 35 | 0.91 (0.54, 1.53) | 1.76 (0.64, 4.80) | 15 | 1.23 (0.52, 2.90) | 1.40 (0.14, 4.35) | ||||
| 7+ | 20 | 1.04 (0.58, 1.88) | 2.59 (0.61, 11.0) | 8 | 1.21 (0.45, 3.22) | 1.74 (0.17, 9.68) | ||||
| Continuous per 1 drink/week | 162 | 1.02 (0.99, 1.05) | 1.03 (0.94, 1.11) | 57 | 1.04 (0.99, 1.09) | 1.05 (0.90, 1.23) | ||||
Adjusted for age at diagnosis, menopausal status, mode of detection, postmenopausal hormone use, tamoxifen use, year of diagnosis, tumor size, tumor grade, remaining lifetyle factors, and pre-diagnosis levels of each lifestyle factor
Post-diagnosis results are additionally adjusted for pre-diagnosis levels of each lifestyle factor
P value is for linear trend across categories
No association was observed between the pre- to post-diagnosis change in BMI (HR 0.98, 95% CI 0.84-1.15 for 1 kg/m2 per year change), physical activity (HR 0.93, 95% CI 0.73, 1.20 for 1 hour/week per year change), or alcohol intake (HR 1.01, 0.70-1.46 for 1 drink/week per year change) and risk of any second breast cancer diagnosis or invasive second breast cancer diagnosis (Table 5). No significant interactions were observed between change in any exposure and menopausal status, treatment type, postmenopausal hormone use, or tamoxifen use.
Table 5.
Hazard ratios and 95% confidence intervals for pre- to post-diagnosis change in lifestyle factors and the risk of a second breast cancer diagnosis: WISC DCIS cohort, 1997-2010
| All second breast cancer diagnoses |
Invasive second breast cancer diagnoses |
|||||
|---|---|---|---|---|---|---|
| Second diagnosis | HR (95% CI)b | Ptrendc | Second diagnosis | HR (95% CI)b | Ptrendc | |
| Change in BMIa,d | ||||||
| Decrease > 0.13 kg/m2 per year | 33 | 0.95 (0.55, 1.63) | 0.61 | 13 | 1.06 (0.43, 2.65) | 0.33 |
| Stable within ± 0.13 kg/m2 per year | 36 | 1.00 (Ref) | 12 | 1.00 (Ref) | ||
| Increase > 0.13 kg/m2 per year | 71 | 0.88 (0.55, 1.41) | 27 | 1.00 (0.44, 2.26) | ||
| Continuous for 1 kg/m2 per year change | 140 | 0.98 (0.84, 1.15) | 52 | 0.93 (0.71, 1.21) | ||
| Change in Total Physical Activitya,d | ||||||
| Decrease > 0.13 hours/week per year | 19 | 0.95 (0.48, 1.88) | 0.45 | 6 | 1.00 (0.30, 3.46) | 0.33 |
| Stable within ± 0.13 hours/week per year | 24 | 1.00 (Ref) | 7 | 1.00 (Ref) | ||
| Increase > 0.13 hours/week per year | 11 | 0.74 (0.35, 1.57) | 5 | 1.04 (0.30, 3.67) | ||
| Continuous for 1 hour/week change | 54 | 0.93 (0.73, 1.20) | 18 | 1.02 (0.61, 1.68) | ||
| Change in Total Alcohola,d | ||||||
| Decrease > 0.064 drinks/week per year | 7 | 0.73 (0.32, 1.66) | 0.13 | 3 | 0.62 (0.15, 2.72) | 0.13 |
| Stable within ± 0.064 drinks/week per year | 30 | 1.00 (Ref) | 8 | 1.00 (Ref) | ||
| Increase > 0.064 drinks/week per year | 17 | 1.58 (0.81, 3.06) | 7 | 1.79 (0.61, 5.47) | ||
| Continuous for 1 drink/week per year change | 54 | 1.01 (0.70, 1.46) | 18 | 1.23 (0.67, 2.16) | ||
Categories for BMI, physical activity, and alcohol intake represent the annualized change from pre-diagnosis to most recent post-diagnosis level (or last contact before a second breast diagnosis)
Adjusted for age at diagnosis, menopausal status, mode of detection, treatment type, postmenopausal hormone use, tamoxifen use, year of diagnosis, tumor size, tumor grade, physical activity, alcohol use, time since diagnosis, remaining lifetyle factors, and pre-diagnosis levels of each lifestyle factor
P value is for linear trend across categories of each change in lifestyle factor
Categories reflect a change of approximately 1 kg/m2 for BMI, 1 hour/week for physical activity, and 0.5 drinks/week for alcohol intake over the median follow-up period
Sensitivity analysis using only those second events that could be confirmed via pathology report (N=117) resulted in wider confidence intervals; however, the risk estimates remained stable for all of the exposure-outcome relationships (data not shown).
Discussion
In this large, population-based cohort of DCIS survivors, we observed a significant trend of increasing risk of a second breast cancer diagnosis over categories of increasing post-diagnosis alcohol intake. We also found a decrease in the risk of a second breast cancer diagnosis with increasing pre-diagnosis BMI in premenopausal women. No significant associations were observed between BMI in postmenopausal women or physical activity and the overall risk of a second breast cancer diagnosis in this cohort. Similar patterns in risk were observed in analyses limited to invasive second breast cancer diagnoses.
Our observed trend of increasing risk of a second breast cancer diagnosis over the categories of increasing post-diagnosis alcohol intake is consistent with previous studies of this association in survivors of invasive breast cancer. In a study of women diagnosed with early-stage invasive breast cancer, Kwan et al found a 35% increase in risk of local, distant, or new primary breast cancer for those consuming six or more grams of alcohol per day (approximately 3-4 drinks per week) at 1-2 years post-diagnosis compared to those consuming fewer than 0.5 grams per day (19). Similarly, Holm et al found a 65% increase in the risk of any second breast cancer event following an invasive diagnosis for women consuming 20 or more grams of alcohol per day (approximately 10 drinks per week) post-diagnosis compared to those consuming less than ten grams per day, excluding non-drinkers (18). Recently, Newcomb et al found that moderate alcohol consumption prior to diagnosis was associated with improved breast cancer survival after an invasive diagnosis, although there was no association between post-diagnosis alcohol consumption and breast cancer survival (33). It is possible that alcohol consumption may increase risk of second breast cancer incidence, but may not substantially increase the likelihood of aggressive second diagnoses that result in death, particularly among DCIS survivors, who have very high survival rates with current treatments.
Few studies have investigated body mass and the risk of second breast cancer diagnosis in premenopausal women. In the only study to our knowledge examining BMI and second events in an exclusively DCIS population, Habel et al found a two-fold increase in risk for women in the highest decile of BMI at diagnosis (>30.8 kg/m2) compared to the lowest decile (<22.0 kg/m2) (21). Their study included both pre- and postmenopausal women and noted that risk estimates were similar when stratified by menopausal status, although separate results were not shown. Analyses of BMI and recurrence after invasive breast cancer in premenopausal women have shown an increase in risk (34) or no association (12, 13) with elevated pre-diagnosis BMI. In contrast, we observed a reduction in overall risk of any second breast cancer diagnosis and risk of an invasive second breast cancer diagnosis with increasing pre-diagnosis BMI in premenopausal women. Two factors may contribute to the differences in these results. First, our study included both ipsilateral and contralateral second events as endpoints. Therefore, new primary breast cancers may have been included as second events, and there is evidence that elevated BMI is protective against primary breast cancer in premenopausal women (35). Some previous studies, including Habel et al, restricted second events to those in the ipsilateral breast or metastasis. Secondary analysis of our data in premenopausal women with ipsilateral second events still indicated a reduction in risk with increasing pre-diagnosis BMI, but was limited in power by the small number of confirmed ipsilateral events. Second, previous studies conducted in survivors of invasive breast cancer involved women who had been treated with chemotherapy. It has been suggested that under-dosing of chemotherapy may occur in obese women because of concern for toxicity (35). Under-dosing may have contributed to an increase in the risk of recurrence in obese women in previous studies. Chemotherapy is not recommended for the treatment of DCIS (1, 36).
In postmenopausal women, the risk estimates indicated an elevated risk of a second breast cancer diagnosis with increasing categories of pre- and post-diagnosis BMI, although these results were not statistically significant. In a population of pre- and postmenopausal breast cancer survivors, Chen et al observed a significant increase in the risk of an ipsilateral second event or metastasis for women who were obese at 6 months post-diagnosis compared to those who were normal weight (HR 1.49, 95% CI 1.08-2.06 for BMI>30 kg/m2) (31). Using a definition of second breast cancer events similar to ours, Inkampe et al found a 43% increased risk for women who were obese versus non-obese at enrollment (pre- and postmenopausal combined) (30). Our findings are consistent with these previous studies, and the lack of significant association in our analysis may be a result of limited statistical power after stratifying by menopausal status.
Previous studies of second breast cancers after invasive disease have reported a reduction in risk with increased levels of physical activity (17, 37) or no association (15, 16). Although we did not observe an association between physical activity and risk of any second breast cancer diagnosis in the full cohort, we found suggestive trend for reduction in risk with increasing post-diagnosis physical activity among women treated with ipsilateral mastectomy. A similar reduction in risk was not observed among women treated with BCS, with or without radiation. Previous studies examining recurrence after invasive breast cancer have not stratified results by type of treatment for the original breast cancer, although most controlled for chemotherapy and radiation therapy in their analyses. Since the majority of second events among women treated with ipsilateral mastectomy were in the contralateral breast, it may be that physical activity reduces the risk of new primary cancers as opposed to being associated with the previously diagnosed DCIS. Stratified analysis of ipsilateral and contralateral second breast cancer events among women treated with ipsilateral mastectomy in our cohort was precluded by small numbers of second breast cancer events. Likewise, stratified analysis examining only invasive second breast cancer diagnoses were limited by the small number of second events in each subgroup.
BMI, physical activity, and alcohol consumption all may affect levels of circulating sex hormones that could impact a woman's risk of a second breast cancer diagnosis. A positive association has been found between BMI and levels of circulating estrogen as a result of the conversion of androstenedione to estrogen in adipose tissue (38, 39). Alcohol consumption has also been shown to be directly related to elevated endogenous estrogen levels in both pre- and postmenopausal women (19). Another possible mechanism linking lifestyle factors to second breast cancer diagnoses may be related to insulin and insulin-like growth factors, which promote the development of sex steroid hormones and may elevate cell proliferation (40). Both weight loss and regular physical activity may reduce insulin levels (41). The effect of insulin on survival after breast cancer has been shown to be independent of BMI (42), suggesting that physical activity may be an effective means of risk reduction even for women of healthy weight.
The results of our study must be interpreted in the context of the limitations. All of our exposures were self-reported. Sub-studies conducted in the study cohort found good reliability for body weight and alcohol consumption (intraclass correlation coefficient > 0.75) (22); however, the possibility exists for misclassification. This is particularly true for the assessment of pre-diagnosis behaviors, since these were reported at a median of 1.3 years after diagnosis and may have been affected by the knowledge of the DCIS diagnosis. Second breast cancer events occurring before the baseline interview were excluded from the pre-diagnosis analyses and second events occurring before the first post-diagnosis interview were excluded from post-diagnosis analyses, meaning that it is unlikely that any misclassification differs by the knowledge of a second breast cancer diagnosis. Although participation rates in the WISC cohort are high (Figure 1), non-response at each data collection period may have the potential to affect our results. Women with a second breast cancer diagnosis may have been more likely to drop out of the study because of additional treatment burden, and this would limit our ability to detect an association between the lifestyle exposures ant the risk of a second breast cancer event. A comparison of women who participated in at least one re-contact interview to non-participating women did not reveal significant differences in pre-diagnosis BMI, physical activity, or alcohol consumption (data not shown).
Invasive second events are of particular importance for women with DCIS. With a relatively small number of invasive second events, we had limited power to detect statistically significant associations, although similar patterns in the associations were observed for the risk of any second event and the risk of invasive second events. Laterality of the second breast cancer diagnosis must also be considered in the interpretation of our results. Second events in the contralateral breast may reflect new primary breast cancers as opposed to an association with the original DCIS. Our definition is consistent with much of the previous literature investigating BMI, physical activity, alcohol intake and second breast cancer events, but may have limited our ability to specifically understand DCIS as a marker of propensity to develop a second breast cancer diagnosis. Separate analyses of second events by laterality were limited to exploratory investigations. As data collection continues in this study population, further analyses of specific outcomes are planned. Finally, data on estrogen receptor (ER) and progesterone receptor (PR) status were largely unavailable in our study, although the majority of DCIS appear to be ER-positive (43). The mechanisms relating BMI, physical activity, and alcohol intake to breast cancer development are thought to involve sex hormone production, which suggests that the effects could be modified by ER and PR status. Further research is required to understand if our results are modified by these prognostic features.
This is the first study to our knowledge to assess physical activity, alcohol intake, and post-diagnosis BMI in relation to risk of second breast cancer diagnoses in an exclusively DCIS population, and the second to explore pre-diagnosis BMI and second breast cancer diagnoses. Strengths of our study include the large, population-based cohort of DCIS survivors with extensive follow-up. In addition, we were able to control for tumor characteristics such as size, grade, and method of detection in our analysis, all of which have been previously associated with the risk of a second event after non-invasive breast cancer (5). Our prospective study design allowed us to take advantage of multiple exposure measurements to reflect changes in exposure with time since the original DCIS diagnosis.
Diagnoses of DCIS continue to rise with the widespread use of screening mammography and the population of DCIS survivors is projected to surpass 1 million by the year 2016 (44). Our findings regarding BMI, physical activity, and alcohol consumption may suggest ways for women with DCIS to reduce their risk of a second breast cancer diagnosis. Future studies are needed to establish the consistency of our results. Such studies would benefit from the use of objective measures of BMI and physical activity, the incorporation of biomarkers to evaluate mechanistic pathways, and the evaluation of variation in risk estimates by hormone receptor status of the original DCIS diagnosis.
Acknowledgments
Funding: National Cancer Institute (U54 CA163303 to B. L. Sprague, R01 CA067264 to A. Trentham-Dietz, R01 CA047147 to P. A. Newcomb, P30 CA014520 to A. Trentham-Dietz); Department of Defense Breast Cancer Research Program (W81XWH-11-0214 to A. Trentham-Dietz); American Society of Preventive Oncology Fellowship Award sponsored by Susan G. Komen for the Cure and the Prevent Cancer Foundation (PCF-0596 to B. L. Sprague)
Footnotes
Conflicts of Interest: None
Disclosure: Preliminary results from this study were presented at the American Society of Preventive Oncology annual meeting in March 2013.
References
- 1.Lee, Vallow Richard, McLaughlin Laura, Tzou Sarah, Hines Katherine, Peterson Stephanie, Jennifer Ductal carcinoma in situ of the breast. International Journal of Surgical Oncology. 2012;2012:123549. doi: 10.1155/2012/123549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.SEER cancer statistics review, 1975-2010 [homepage on the Internet] National Cancer Institute; Bethesda, MD: based on November 2012 SEER data submission. Available from: http://seer.cancer.gov/csr/1975_2010/ [Google Scholar]
- 3.Ernster, Ballard Barbash Virginia, Barlow Rachel, Zheng William, Weaver Yingye, Cutter Donald, Gary, et al. Detection of ductal carcinoma in situ in women undergoing screening mammography. J Natl Cancer Inst. 2002;94:1546–54. doi: 10.1093/jnci/94.20.1546. [DOI] [PubMed] [Google Scholar]
- 4.Wrnberg F, Yuen J, Holmberg L. Risk of subsequent invasive breast cancer after breast carcinoma in situ. Lancet. 2000;355:724–5. doi: 10.1016/S0140-6736(99)03703-4. [DOI] [PubMed] [Google Scholar]
- 5.Shamliyan T, Wang S, Virnig B, Tuttle T, Kane R. Association between patient and tumor characteristics with clinical outcomes in women with ductal carcinoma in situ. Journal of the National Cancer Institute. Monographs. 2010;2010:121–9. doi: 10.1093/jncimonographs/lgq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suzuki R, Orsini N, Saji S, Key T, Wolk A. Body weight and incidence of breast cancer defined by estrogen and progesterone receptor status--a meta-analysis. International journal of cancer. 2009;124:698–712. doi: 10.1002/ijc.23943. [DOI] [PubMed] [Google Scholar]
- 7.McTiernan A. Behavioral risk factors in breast cancer: Can risk be modified? Oncologist. 2003;8:326–34. doi: 10.1634/theoncologist.8-4-326. [DOI] [PubMed] [Google Scholar]
- 8.Key J, Hodgson S, Omar R, Jensen TK, Thompson SG, Boobis AR, et al. Meta-analysis of studies of alcohol and breast cancer with consideration of the methodological issues. CCC.Cancer causes control. 2006;17:759–70. doi: 10.1007/s10552-006-0011-0. [DOI] [PubMed] [Google Scholar]
- 9.La Vecchia C, Giordano S, Hortobagyi G, Chabner B. Overweight, obesity, diabetes, and risk of breast cancer: Interlocking pieces of the puzzle. Oncologist. 2011;16:726–9. doi: 10.1634/theoncologist.2011-0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monninkhof E, Elias S, Vlems F, van der Tweel I, Schult AJ, Voskuli DW, et al. Physical activity and breast cancer: A systematic review. Epidemiology. 2007;18:137–57. doi: 10.1097/01.ede.0000251167.75581.98. [DOI] [PubMed] [Google Scholar]
- 11.Coronado G, Beasley J, Livaudais J. Alcohol consumption and the risk of breast cancer. Salud pública de México. 2011;53:440–7. [PubMed] [Google Scholar]
- 12.Caan B, Emond J, Natarajan L, Castillo A, Gunderson EP, Habel L, et al. Post-diagnosis weight gain and breast cancer recurrence in women with early stage breast cancer. Breast Cancer Res Treat. 2006;99:47–57. doi: 10.1007/s10549-006-9179-y. [DOI] [PubMed] [Google Scholar]
- 13.Caan B, Kwan M, Hartzell G, Castillo A, Slattery ML, Sternfeld B, et al. Pre-diagnosis body mass index, post-diagnosis weight change, and prognosis among women with early stage breast cancer. CCC.Cancer causes control. 2008;19:1319–28. doi: 10.1007/s10552-008-9203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kroenke C, Chen W, Rosner B, Holmes M. Weight, weight gain, and survival after breast cancer diagnosis. Journal of clinical oncology. 2005;23:1370–8. doi: 10.1200/JCO.2005.01.079. [DOI] [PubMed] [Google Scholar]
- 15.Bertram LAC, Stefanick M, Saquib N, Natarajan L, Patterson RE, Bardwell W, et al. Physical activity, additional breast cancer events, and mortality among early-stage breast cancer survivors: Findings from the WHEL study. CCC.Cancer causes control. 2011;22:427–35. doi: 10.1007/s10552-010-9714-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sternfeld B, Weltzien E, Quesenberry C, Castillo AL, Kwan M, Slattery ML, et al. Physical activity and risk of recurrence and mortality in breast cancer survivors: Findings from the LACE study. Cancer epidemiology, biomarkers prevention. 2009;18:87–95. doi: 10.1158/1055-9965.EPI-08-0595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holmes M, Chen W, Feskanich D, Kroenke C, Colditz G. Physical activity and survival after breast cancer diagnosis. JAMA (Chicago, Ill.) 2005;293:2479–86. doi: 10.1001/jama.293.20.2479. [DOI] [PubMed] [Google Scholar]
- 18.Holm M, Olsen A, Christensen J, Kroman NT, Bidstrup PE, Johansen C, et al. Pre-diagnostic alcohol consumption and breast cancer recurrence and mortality - results from a prospective cohort with a wide range of variation in alcohol intake. International journal of cancer. 2013;132:686–94. doi: 10.1002/ijc.27652. [DOI] [PubMed] [Google Scholar]
- 19.Kwan M, Kushi L, Weltzien E, Tam EK, Castillo A, Sweeney C, et al. Alcohol consumption and breast cancer recurrence and survival among women with early-stage breast cancer: The life after cancer epidemiology study. Journal of clinical oncology. 2010;28:4410–6. doi: 10.1200/JCO.2010.29.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flatt S, Thomson C, Gold E, Natarajan L, Rock CL, Al-Delaimy WK, et al. Low to moderate alcohol intake is not associated with increased mortality after breast cancer. Cancer epidemiology, biomarkers prevention. 2010;19:681–8. doi: 10.1158/1055-9965.EPI-09-0927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Habel LA, Daling JR, Newcomb PA, Self SG, Porter PL, Stanford JL, et al. Risk of recurrence after ductal carcinoma in situ of the breast. Cancer epidemiology, biomarkers prevention. 1998;7:689–96. [PubMed] [Google Scholar]
- 22.Sprague B, Trentham Dietz A, Nichols H, Hampton J, Newcomb P. Change in lifestyle behaviors and medication use after a diagnosis of ductal carcinoma in situ. Breast Cancer Res Treat. 2010;124:487–95. doi: 10.1007/s10549-010-0869-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nichols H, Trentham Dietz A, Egan K, Titus Ernstoff L, Hampton J, Newcomb P. Oral contraceptive use and risk of breast carcinoma in situ. Cancer epidemiology, biomarkers prevention. 2007;16:2262–8. doi: 10.1158/1055-9965.EPI-07-0456. [DOI] [PubMed] [Google Scholar]
- 24.Trentham Dietz A, Nichols H, Egan K, Titus Ernstoff L, Hampton J, Newcomb P. Cigarette smoking and risk of breast carcinoma in situ. Epidemiology. 2007;18:629–38. doi: 10.1097/EDE.0b013e318127183a. [DOI] [PubMed] [Google Scholar]
- 25.Wolf AM, Hunter DJ, Colditz GA, Manson JE, Stampfer MJ, Corsano KA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994;23:991–9. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- 26.Sprague, Trentham Dietz Brian, Newcomb Amy, Titus Ernstoff Polly, Hampton Linda, Egan John, Kathleen Lifetime recreational and occupational physical activity and risk of in situ and invasive breast cancer. Cancer epidemiology, biomarkers & prevention. 2007;16:236–43. doi: 10.1158/1055-9965.EPI-06-0713. [DOI] [PubMed] [Google Scholar]
- 27.Schafer J. Analysis of incomplete multivariate data. Chapman and Hall; London: 1997. [Google Scholar]
- 28.Rubin DB. Multiple imputation for nonresponse in surveys. John Wiley & Sons; New York: 1987. [Google Scholar]
- 29.Rubin DB. Inference and missing data. Biometrika. 1976;63:581–92. [Google Scholar]
- 30.Imkampe A, Bates T. Impact of a raised body mass index on breast cancer survival in relation to age and disease extent at diagnosis. Breast J. 2010;16:156–61. doi: 10.1111/j.1524-4741.2009.00872.x. [DOI] [PubMed] [Google Scholar]
- 31.Chen X, Lu W, Zheng W, Gu K, Chen Z, Zheng Y, et al. Obesity and weight change in relation to breast cancer survival. Breast Cancer Res Treat. 2010;122:823–33. doi: 10.1007/s10549-009-0708-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Therneau T. Modeling survival data: Extending the cox model. Springer-Verlag; New York: 2000. [Google Scholar]
- 33.Newcomb. Kampman Polly, Trentham Dietz Ellen, Egan Amy, Titus Kathleen, Baron Linda, John, et al. Alcohol consumption before and after breast cancer diagnosis: Associations with survival from breast cancer, cardiovascular disease, and other causes. Journal of clinical oncology. 2013;31:1939–46. doi: 10.1200/JCO.2012.46.5765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Loi S, Milne R, Friedlander M, McCredie MR, Giles GG, Hopper JL, et al. Obesity and outcomes in premenopausal and postmenopausal breast cancer. Cancer epidemiology, biomarkers prevention. 2005;14:1686–91. doi: 10.1158/1055-9965.EPI-05-0042. [DOI] [PubMed] [Google Scholar]
- 35.Protani M, Coory M, Martin J. Effect of obesity on survival of women with breast cancer: Systematic review and meta-analysis. Breast Cancer Res Treat. 2010;123:627–35. doi: 10.1007/s10549-010-0990-0. [DOI] [PubMed] [Google Scholar]
- 36.Morrow, Strom Monica, Bassett Eric, Dershaw Lawrence, Fowble DD, Harris Barbara, Jay, et al. Standard for the management of ductal carcinoma in situ of the breast (DCIS). Ca. 2002;52:256–76. doi: 10.3322/canjclin.52.5.256. [DOI] [PubMed] [Google Scholar]
- 37.Friedenreich C, Gregory J, Kopciuk K, Mackey J, Courneya K. Prospective cohort study of lifetime physical activity and breast cancer survival. International journal of cancer. 2009;124:1954–62. doi: 10.1002/ijc.24155. [DOI] [PubMed] [Google Scholar]
- 38.MacDonald PC, Edman CD, Hemsell DL, Porter JC, Siiteri PK. Effect of obesity on conversion of plasma androstenedione to estrone in postmenopausal women with and without endometrial cancer. Obstet Gynecol. 1978;130:448–55. doi: 10.1016/0002-9378(78)90287-9. [DOI] [PubMed] [Google Scholar]
- 39.McTiernan A, Rajan K, Tworoger S, Irwin M, Bernstein L, Baumgartner R, et al. Adiposity and sex hormones in postmenopausal breast cancer survivors. Journal of clinical oncology. 2003;21:1961–6. doi: 10.1200/JCO.2003.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yu H, Rohan T. Role of the insulin-like growth factor family in cancer development and progression. J Natl Cancer Inst. 2000;92:1472–89. doi: 10.1093/jnci/92.18.1472. [DOI] [PubMed] [Google Scholar]
- 41.McTiernan A, Irwin M, Vongruenigen V. Weight, physical activity, diet, and prognosis in breast and gynecologic cancers. Journal of clinical oncology. 2010;28:4074–80. doi: 10.1200/JCO.2010.27.9752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goodwin P, Ennis M, Pritchard K, Trudeau ME, Koo J, Madarnas Y, et al. Fasting insulin and outcome in early-stage breast cancer: Results of a prospective cohort study. Journal of clinical oncology. 2002;20:42–51. doi: 10.1200/JCO.2002.20.1.42. [DOI] [PubMed] [Google Scholar]
- 43.Altintas, Lambein Sevilay, Huizing Kathleen, Braems Manon, Asjoe Geert, Hellemans Fernando, Hilde, et al. Prognostic significance of oncogenic markers in ductal carcinoma in situ of the breast: A clinicopathologic study. Breast J. 2009;15:120–32. doi: 10.1111/j.1524-4741.2009.00686.x. [DOI] [PubMed] [Google Scholar]
- 44.Sprague B, Trentham Dietz A. Prevalence of breast carcinoma in situ in the united states. JAMA (Chicago, Ill.) 2009;302:846–8. doi: 10.1001/jama.2009.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]