Abstract
Infants born at very low birth weight (VLBW; birth weight <1500 g) are at high risk of mortality and are some of the most expensive patients in the hospital. Additionally, VLBW infants are susceptible to prematurity-related morbidities, including late-onset sepsis, bronchopulmonary dysplasia (BPD), necrotizing enterocolitis, and retinopathy of prematurity, which have short- and long-term economic consequences. The incremental cost of these morbidities during the neonatal intensive care unit (NICU) hospitalization is high, ranging from $10,055 (in 2009 US$) for late-onset sepsis to $31,565 for BPD. Human milk has been shown to reduce both the incidence and severity of some of these morbidities and, therefore, has an indirect impact on the cost of the NICU hospitalization. Furthermore, human milk may also directly reduce NICU hospitalization costs, independent of the indirect impact on the incidence and/or severity of these morbidities. Although there is an economic cost to both the mother and institution for providing human milk during the NICU hospitalization, these costs are relatively low. This review describes the total cost of the initial NICU hospitalization, the incremental cost associated with these prematurity-related morbidities, and the incremental benefits and costs of human milk feedings during critical periods of the NICU hospitalization as a strategy to reduce the incidence and severity of these morbidities.
Introduction
Infants born at very low birth weight (VLBW8; <1500 g) represent only 1.4% of total births, but have a mortality rate of 23.1% and account for 53.9% of all infant deaths (1). VLBW infants are some of the most expensive patients in the hospital, with mean direct costs to the hospital of $76,224 (2009 US$) (2). Further, VLBW infants are at considerable risk of developing prematurity-related morbidities, including late-onset sepsis, bronchopulmonary dysplasia (BPD), necrotizing enterocolitis (NEC), and retinopathy of prematurity (ROP). These morbidities require additional expensive treatments and longer stays in the neonatal intensive care unit (NICU). The morbidities also increase the risk of long-term chronic illness, rehospitalization, and neurodevelopmental and neurocognitive delay.
Every healthcare system, regardless of whether it is publicly or privately funded, has limited resources and must allocate its resources in a cost-effective way (3). By first identifying potentially preventable morbidities that are costly and have long-term health consequences for VLBW infants, society can then prioritize interventions based on their impact on reducing the incidence and severity of these morbidities, with those interventions having the largest benefit relative to their cost receiving the highest priority. Three economic issues critical to VLBW infant care are the baseline cost (i.e., cost of care for VLBW infants without any morbidities) of the initial NICU hospitalization (throughout this review, the term “NICU hospitalization” is used to refer to the initial NICU hospitalization at birth), the incremental cost associated with prematurity-related morbidities, and the incremental benefits and costs of interventions to reduce the incidence and severity of these morbidities.
A substantial body of literature has evaluated the NICU hospitalization costs for VLBW and/or preterm infants. In a review of the economic consequences of preterm birth, Petrou et al. (4) identified 19 studies published between 1980 and June 2009 that reported total costs associated with the initial NICU hospitalization. In this review, there was a consistent relation between infant birth weight (BW) and costs incurred during the initial NICU hospital stay. The relation between infant BW and costs is due to both longer NICU stays and more intensive resource use for infants with lower BW as well as to the higher incidence of costly morbidities that require additional days in the NICU and costly resources, such as mechanical ventilation and surgery. Very few studies have addressed the economic consequences of individual and/or combinations of prematurity-related morbidities in VLBW infants. This review synthesizes the literature about the costs associated with individual morbidities, describes the incremental benefits (i.e., cost savings) achieved by reducing the prevalence and/or severity of these morbidities through the use of high doses of human milk feedings during specific critical exposure periods during the NICU hospitalization, describes the incremental benefits (i.e., cost savings) of human milk independent of the incidence of these morbidities, and summarizes the incremental costs required to support human milk feedings in the NICU.
The Cost of Morbidities in VLBW Infants
Although costs can be studied from the perspective of the insurer (e.g., the amount paid for the care provided), patient (e.g., the amount paid out-of-pocket), or society (taking into account the costs incurred by all stakeholders), this review focuses on the cost of the NICU hospitalization from the hospital’s perspective, which represents the dollars spent by the hospital to provide care to the infant (e.g., direct cost of care). Costs from the hospital’s perspective can be determined using at least 2 different methodologies. One approach sums micro-level cost information collected from an individual hospital that takes into account the costs of labor, medical and nonmedical supplies, drugs, equipment, and other resources used. The micro-level costing approach is a “bottom-up” approach that requires detailed information about the different resources used and their associated unit costs.
When detailed resource-level information is not available (as is often the case), the ratio of cost-to-charges approach is used in which a hospital-specific ratio is applied to charges to estimate the actual costs incurred by the hospital. Although the ratio of cost-to-charges approach is relatively accurate at the hospital level, it is often less accurate for individual units or unit-based resource use, because the actual ratio of costs to charges can vary across resources (5). The micro-level cost accounting approach is the more accurate methodology, because it accounts for the actual costs for individual resources used. Differences in the mark-up of charges relative to the costs of individual resources within an individual hospital are irrelevant in the micro-level cost accounting approach. Not all hospitals collect detailed, micro-level costs, however, and it is particularly difficult to obtain micro-level costs across hospitals. Despite the limitations of the ratio of cost-to-charges approach, most published research on the cost of the NICU hospitalization for VLBW infants uses this methodology due to a lack of detailed resource-level cost information.
Four studies were located in which either the cost or care for VLBW infants with and without specific morbidities or the incremental cost associated with one or more specific morbidities were evaluated (2, 6–8). Three studies focused on the cost of NEC and 2 studies focused the cost of late-onset sepsis. Table 1 summarizes these studies and describes the actual costs, the costs inflated to 2011 US$ using the Consumer Price Index for Medical Care (9), and the methods used for estimating the costs.
TABLE 1.
Comparison of costs of preventable morbidities in VLBW infants1
| Morbidity and authors | Type of costs | BW or GA | Cost as reported by authors | Year of costs | Cost inflated to 2011 US$ |
| Brain injury | |||||
| Johnson et al. (2) | Adjusted incremental cost | VLBW (<1500 g) | $12,045 | 2009 | $13,305 |
| BPD | |||||
| Johnson et al. (2) | Adjusted incremental cost | VLBW (<1500 g) | $31,565 | 2009 | $34,868 |
| Late-onset sepsis | |||||
| Payne et al. (6) | Unadjusted costs | VLBW (401–1500 g) | $54,539 ($104,473 vs. $49,934) | 1999 | $90,316 |
| Payne et al. (6) | Adjusted incremental cost | VLBW (401–1500 g) | $5,875, BW 401–750 g | 1999 | $9729 |
| $12,480, BW 751–1000 g | $20,667 | ||||
| $9,583, BW 1001–1250 g | $15,869 | ||||
| $6,276, BW 1251–1500 g | $10,393 | ||||
| Johnson et al. (2) | Adjusted incremental cost | VLBW (<1500 g) | $10,055 | 2009 | $11,107 |
| NEC | |||||
| Medically managed only | |||||
| Bisquera et al. (7) | Unadjusted charges | VLBW (<1500 g) | $73,700 | 1992–1994 | $144,910 |
| Ganapathy et al. (7) | Adjusted incremental cost | ≤28 wk GA | $74,004 | 2011 | $76,716 |
| Surgically managed only | |||||
| Bisquera et al. (7) | Unadjusted charges | VLBW (<1500 g) | $186,200 | 1992–1994 | $366,110 |
| Ganapathy et al. (8) | Adjusted incremental cost | ≤28 wk GA | $198,040 | 2011 | $205,299 |
| Medically and surgically managed | |||||
| Johnson et al. (2) | Adjusted incremental cost | VLBW (<1500 g) | $15,440 | 2009 | $17,056 |
Costs inflated to 2011 US$ using the Consumer Price Index for medical care (9). BPD, bronchopulmonary dysplasia; BW, birth weight; GA, gestational age; NEC, necrotizing enterocolitis; VLBW, very low birth weight.
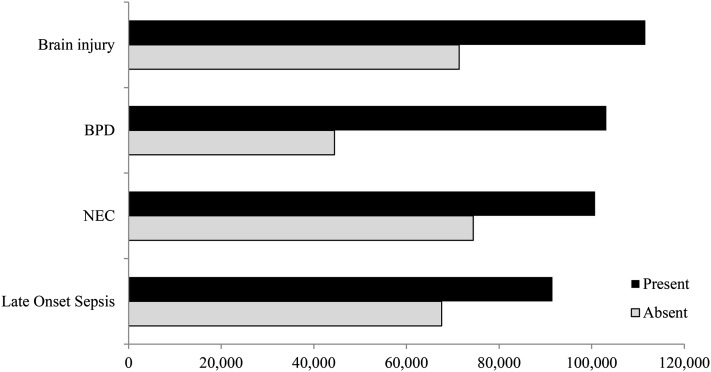
Only one study could be located in which the costs of combinations of morbidities were studied. Using data from a large cohort of VLBW infants, our study team (2) demonstrated that the baseline NICU hospitalization cost for infants without any prematurity-related morbidities was $40,227 (in 2009 US$). We found that the total cost for the NICU hospitalization was significantly higher when infants acquired 1 or more of these 4 potentially preventable morbidities, even after controlling for other infant characteristics (Fig. 1). The difference in unadjusted direct hospital costs for infants with and without these morbidities ranged from $23,901 (in 2009 US$) for late-onset sepsis to $58,686 for BPD. After adjusting for the presence of the other morbidities, BW, and infant sociodemographic characteristics, the incremental cost of these morbidities ranged from $10,055 for late-onset sepsis to $31,565 for BPD.
FIGURE 1.
Comparison of hospital direct costs with and without specific morbidities in 2009 US$. BPD, bronchopulmonary dysplasia; NEC, necrotizing enterocolitis.
These studies indicate that acquisition of potentially preventable prematurity-related morbidities is costly from the perspective of the hospital. Additionally, certain morbidities increase the risk of a VLBW infant acquiring an additional morbidity(ies), thereby further increasing the costs associated with the NICU hospitalization. Therefore, strategies that reduce the incidence, severity, and/or risk of these morbidities are important from an economic perspective.
Incremental Benefits of Human Milk
Benefits of human milk in reducing prematurity-related morbidities.
There is substantial evidence that links human milk from the infant’s own mother during the NICU hospitalization to a reduction in the risk of short- and long-term morbidities in VLBW infants. Human milk provides this protection through a synergistic mix of nutritional, bioactive, immunomodulatory, and epigenetic properties (10). Studies have demonstrated the effectiveness of human milk in reducing the incidence, severity, and/or risk of prematurity-related morbidities, including late-onset sepsis (11–16), NEC (12, 16, 17), and ROP (18), during the NICU hospitalization. Most recently, the impact of human milk on these morbidities has emerged as a dose-response relation, meaning that higher doses of human milk provide greater risk reduction (10). Furthermore, it appears that there are certain critical periods in the NICU hospitalization (e.g., the first 14 or 28 d of life) that are especially important for infants to receive high doses of human milk and/or avoid bovine-based formula products entirely for the incidence, severity, and/or risk of these prematurity-related morbidities to be reduced. The link between a reduction in risk and the specific human milk protective mechanism likely varies across morbidities such that the mechanisms protecting from late-onset sepsis may be different from those that provide protection from inflammation-based morbidities, such as NEC, BPD, and ROP.
Because human milk reduces the incidence and/or severity of prematurity-related morbidities, human milk feedings have an indirect relation with healthcare costs during the NICU hospitalization (e.g., human milk reduces the risk of the morbidity and thereby indirectly reduces the associated costs). However, human milk feedings may also have a direct impact on healthcare costs independent of their association with morbidities such as late-onset sepsis, NEC, BPD, and ROP. Only one study has evaluated the direct relation between the dose of human milk and healthcare costs, after controlling for the presence of one or more morbidities (13). Our study found significantly lower NICU hospitalization costs with higher doses of human milk, defined as mL ⋅ kg−1 ⋅ d−1, in the first 28 d post-birth.
The role of human milk in reducing the risk of long-term chronic conditions.
Prematurity-related morbidities that present during the NICU hospitalization also predispose VLBW infants to chronic conditions that result in rehospitalization and high rates of post-NICU discharge healthcare use, such as vision care for ROP or respiratory complications due to BPD (4, 19–24). In particular, late-onset sepsis and NEC during NICU hospitalization significantly increase the risk of neurodevelopmental and neurocognitive problems (25–27). For all preterm births, the annual societal economic burden is $51,600 per birth (in 2005 US$), translating into an additional $928,800 per birth in societal costs through age 18 y (28). Thus, from an economic perspective, human milk feedings during NICU hospitalization for VLBW infants could serve as a primary prevention strategy with considerable potential for cost savings during the NICU hospitalization and throughout the lifespan for families, health care systems, educational programs, and society at large.
NEC and human milk as a case study of the indirect relation with NICU hospitalization costs.
One study explicitly quantified the economic value of human milk feedings. Ganapathy et al. (8) evaluated the hospital costs associated with human milk vs. bovine milk-based fortifier compared with 100% human milk feedings (with a human milk-based milk fortifier). The difference in costs between bovine milk-based fortifier and 100% human milk diet was due to a reduction in the incidence of medically and surgically managed NEC. They found a reduction in costs of $8167 per infant associated with the 100% human milk diet.
Late-onset sepsis and human milk as a case study of the indirect and direct relation with NICU hospitalization costs.
The indirect cost savings of human milk feedings are due to a decrease in the incidence and/or severity of morbidities during the NICU hospitalization. This relation has been exemplified in several studies of late-onset sepsis, as follows. In a study of the impact of human milk feedings on the incidence of infections for VLBW infants, Hylander et al. (14) demonstrated that any human milk feedings significantly reduced the risk of sepsis during the hospital stay compared with infants who received exclusive formula feedings. Further, Schanler (12) demonstrated that infants receiving exclusive human milk feedings during the hospital stay had significantly lower odds of having sepsis than infants with partial or exclusive formula feedings. Sullivan et al. (29), however, found no difference in the incidence of sepsis for infants fed with exclusively human milk-based diets compared with infants receiving human milk plus bovine milk-based diets. However, the infants in all arms of Sullivan’s randomized clinical trial received relatively high doses of maternal human milk, regardless of bovine-based supplemental formulas and fortifiers in the bovine arm, which may explain why these findings differ from those of Schanler and Hylander.
Furman et al. (11) determined that the relation between human milk and incidence of late-onset sepsis varied by dose of human milk. They found that high doses of human milk (≥50 mL ⋅ kg−1 ⋅ d−1 during the first 28 d of life) were associated with a significantly lower risk of sepsis compared with infants receiving exclusive formula feedings; however, there was no difference in the risk of sepsis for infants with lower doses of human milk (1–24 and 25–49 mL ⋅ kg−1 ⋅ d−1 compared with exclusive formula feedings). Corpeleijn et al. (30) used a shorter exposure period of human milk than Furman et al. (11), evaluating the relation between dose of human milk in the first 10 d of life rather than 28 d of life. They found that high doses of human milk in days 6–10 of life were associated with significantly lower odds of late-onset sepsis compared with infants with no human milk.
Our study (13) of the relation between dose of human milk in the first 28 d of life with sepsis and NICU hospitalization costs in a cohort of VLBW infants has been the only study to date, to our knowledge, to evaluate the association between dose of human milk with both the incidence of sepsis and costs. Similar to Furman et al. (11) and Corpeleijn et al. (30), we found that mean daily dose of human milk in the first 28 d of life was associated with lower odds of sepsis (OR: 0.98; 95% CI: 0.97, 1.00; P = 0.008) after controlling for a single propensity score that incorporated multiple risk factors into a single measure for the risk of morbidity. The propensity score included BW, receipt of surfactant, receipt of parenteral nutrition on life day 10, race, and day of life of enteral feeding initiation.
In this study, we evaluated the economic value of human milk feedings after accounting for a reduction in the incidence of late-onset sepsis (13). Similar to Furman et al. (11), the dose of human milk was classified into 3 groups: <25, 25–49.99, and ≥50 mL ⋅ kg−1 ⋅ d−1 human milk for the first 28 d post-birth. After controlling for the incidence of sepsis and the previously defined propensity score (a composite measure for the risk of sepsis), we found that cost of the NICU hospitalization was $20,384 (in 2010 US$) higher for infants with <25 mL ⋅ kg−1 ⋅ d−1 human milk compared with infants fed 25–49.99 mL ⋅ kg−1 ⋅ d−1 human milk during the first 28 d post-birth and $31,514 higher than infants fed ≥50 mL ⋅ kg−1 ⋅ d−1. However, there were no significant incremental cost savings for infants who received ≥50 mL ⋅ kg−1 ⋅ d−1 compared with those who received 25–49.99 mL ⋅ kg−1 ⋅ d−1, suggesting that the threshold dose of 25 mL ⋅ kg−1 ⋅ d−1 may be sufficient to reduce the risk of late-onset sepsis and its associated costs.
Table 2 summarizes the studies that have evaluated the indirect and direct cost savings of human milk during the NICU hospitalization. These studies provide evidence of the substantial cost savings associated with human milk feedings during critical periods of the NICU stay and provide the foundation for future work to evaluate the direct and indirect cost savings associated with early post-birth human milk feedings across the spectrum of costly morbidities in VLBW infants.
TABLE 2.
Impact of human milk on costs of preventable morbidities in VLBW infants1
| Authors | Type of costs | BW | Morbidity | Cost savings of HM | Year of costs |
| Ganapathy et al. (8) | Incremental cost due to reduction in NEC: HM bovine | ≤1250 g | NEC | Bovine milk associated with $8167 higher cost than HM | 2011 |
| Patel et al. (13) | Incremental cost, after controlling for sepsis: <25, 25–49.99, and ≥50 mL ⋅ kg−1 ⋅ d−1 | <1500 g | Sepsis | <25 mL ⋅ kg−1 ⋅ d−1 HM had $31,514 higher cost than ≥50 mL ⋅ kg−1 ⋅ d−1 HM and $20,384 higher cost than 25–49.99 mL ⋅ kg−1 ⋅ d−1 HM | 2010 |
BW, birth weight; HM, human milk; NEC, necrotizing enterocolitis.
Incremental Costs of Human Milk Feedings in the NICU
Although evidence has demonstrated that human milk feedings, particularly in the early post-birth period, directly reduce the incidence of prematurity-related morbidities in VLBW infants, there are also costs to the institution and the mother associated with acquiring and providing human milk feedings. To ensure adequate milk supply, NICUs need to supply at least 3 universal resources: hospital-grade breast pumps, breast pump collection kits, and disposable food-grade storage containers. Jegier et al. (31) demonstrated that the cost to the institution to acquire 100 mL/d of human milk from the infant’s mother is relatively low when the institution provides the mother with a hospital-grade electric breast pump collection kit and storage containers for the milk. Further, the downstream direct and indirect cost savings from the human milk feedings are likely to far exceed the hospital’s costs to acquire human milk in most cases.
Our study team has conducted 2 studies to evaluate the maternal and institutional costs of providing human milk to VLBW infants during the NICU stay. In a study of the maternal costs that included the breast pump rental, pump kit, and maternal opportunity cost, Jegier et al. (32) found that the mean cost of providing 100 mL human milk ranged from $2.60 to $6.18 (in 2008 US$). The largest component of costs was maternal opportunity cost; however, this cost decreased over time as mothers became more efficient at pumping.
In evaluating the institution’s cost to acquire 100 mL of human milk from the biologic mother for different doses and exposure periods, Jegier et al. (32) demonstrated that the median cost to the institution ranged from $7.93/100 mL (in 2012 US$) for mothers who produced <100 mL/d of human milk to $0.51/100 mL for mothers who provided >700 mL/d. These data included the institution’s cost of hospital-grade electric breast pumps, breast pump collection kits, and disposable food-grade storage containers. Additionally, the median cost for institutions to acquire human milk was substantially lower than donor human milk (cost per 100 mL = $14.84) after ~7 d of pumping and commercial formula (cost per 100 mL = $3.18) after 19 d of pumping for all volumes of human milk pumped, except when <100 mL human milk was pumped per day. In fact, the institution’s cost was less than donor human milk after 4 d of pumping and commercial formula after 10 d of pumping for women who pumped ≥400 mL/d of human milk.
There is mounting evidence of the substantial economic benefits associated with human milk feedings during critical periods of the NICU hospitalization and, at the same time, low economic costs to the institution and mother for providing human milk. There are still a number of unanswered questions regarding the direct and indirect economic benefits associated with human milk. More comprehensive analyses of the human milk doses required and critical exposure periods for each specific morbidity and their downstream relation with NICU hospitalization costs are needed to better understand the cost savings of human milk. Additionally, although one study has demonstrated a direct relation between human milk and NICU hospitalization costs, more work is needed to validate this finding and determine whether this relation remains after controlling for other prematurity-related morbidities.
Acknowledgments
All authors read and approved the final manuscript.
Footnotes
Abbreviations used: BPD, bronchopulmonary dysplasia; BW, birth weight; NEC, necrotizing enterocolitis; NICU, neonatal intensive care unit; ROP, retinopathy of prematurity; VLBW, very low birth weight.
Literature Cited
- 1. Linked birth / infant death records 2007–2009 on CDC WONDER on-line database [homepage on the Internet] [cited 2010 Oct 20]. Available from: http://wonder.cdc.gov/lbd.html.
- 2.Johnson TJ, Patel AL, Jegier B, Engstrom JL, Meier J. The cost of morbidities in very low birth weight infants. J Pediatr. 2013;162:243–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petrou S. Preterm birth: what are the relevant economic issues? Early Hum Dev. 2006;82:75–6 [DOI] [PubMed] [Google Scholar]
- 4. Petrou S, Eddama O, Mangham L. A structured review of the recent literature on the economic consequences of preterm birth. Archives of disease in childhood: fetal and neonatal edition; 2011;96:F225–32. [DOI] [PubMed]
- 5.Young DW. Management accounting in health care organizations. 2nd ed. San Francisco: Jossey-Bass; 2008.
- 6.Payne NR, Carpenter JH, Badger GJ, Horbar JD, Rogowski J. Marginal increase in cost and excess length of stay associated with nosocomial bloodstream infections in surviving very low birth weight infants. Pediatrics. 2004;114:348–55 [DOI] [PubMed] [Google Scholar]
- 7.Bisquera JA, Cooper TR, Berseth CL. Impact of necrotizing enterocolitis on length of stay and hospital charges in very low birth weight infants. Pediatrics. 2002;109:423–8 [DOI] [PubMed] [Google Scholar]
- 8.Ganapathy V, Hay JW, Kim JH. Costs of necrotizing enterocolitis and cost-effectiveness of exclusively human milk-based products in feeding extremely premature infants. Breastfeed Med. 2012;7:29–37 [DOI] [PubMed] [Google Scholar]
- 9. Consumer price index for 2011, series ID CUSR0000SAM [homepage on the Internet] [cited 2013 Aug 1]. Available from: http://www.bls.gov/cpi/
- 10.Meier PP, Engstrom JL, Patel AL, Jegier BJ, Bruns N. Improving the use of human milk during and after the NICU stay. Clin Perinatol. 2010;37:217–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Furman L, Taylor G, Minich N, Hack M. The effect of maternal milk on neonatal morbidity of very low-birth-weight infants. Arch Pediatr Adolesc Med. 2003;157:66–71 [DOI] [PubMed] [Google Scholar]
- 12.Schanler RJ. Post-discharge nutrition for the preterm infant. Acta Paediatr Suppl. 2005;94:68–73 [DOI] [PubMed] [Google Scholar]
- 13.Patel AL, Johnson TJ, Engstrom JL, Fogg LF, Jegier BJ, Bigger HR, Meier PP. Impact of early human milk on sepsis and health care costs in very low birthweight infants. J Perinatol. 2013;33:514–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hylander MA, Strobino DM, Dhanireddy R. Human milk feedings and infection among very low birth weight infants. Pediatrics. 1998;102:E38. [DOI] [PubMed] [Google Scholar]
- 15.Meinzen-Derr JK, Guerrero ML, Altaye M, Ruiz-Palacios GM, Morrow AL. Duration of exclusive breastfeeding and risk of anemia in a cohort of Mexican infants. Adv Exp Med Biol. 2004;554:395–8 [DOI] [PubMed] [Google Scholar]
- 16.Schanler RJ, Shulman RJ, Lau C. Feeding strategies for premature infants: beneficial outcomes of feeding fortified human milk versus preterm formula. Pediatrics. 1999;103:1150–7 [DOI] [PubMed] [Google Scholar]
- 17.Lucas A, Cole TJ. Breast milk and neonatal necrotising enterocolitis. Lancet. 1990;336:1519–23 [DOI] [PubMed] [Google Scholar]
- 18.Hylander MA, Strobino DM, Pezzullo JC, Dhanireddy R. Association of human milk feedings with a reduction in retinopathy of prematurity among very low birthweight infants. J Perinatol. 2001;21:356–62 [DOI] [PubMed] [Google Scholar]
- 19.Hack M, Taylor HG, Drotar D, Schluchter M, Cartar L, Andreias L, Wilson-Costello D, Klein N. Chronic conditions, functional limitations, and special health care needs of school-aged children born with extremely low-birth-weight in the 1990s. JAMA. 2005;294:318–25 [DOI] [PubMed] [Google Scholar]
- 20.Drotar D, Hack M, Taylor G, Schluchter M, Andreias L, Klein N. The impact of extremely low birth weight on the families of school-aged children. Pediatrics. 2006;117:2006–13 [DOI] [PubMed] [Google Scholar]
- 21.Petrou S, Sach T, Davidson L. The long-term costs of preterm birth and low birth weight: results of a systematic review. Child Care Health Dev. 2001;27:97–115 [DOI] [PubMed] [Google Scholar]
- 22.Mangham LJ, Petrou S, Doyle LW, Draper ES, Marlow N. The cost of preterm birth throughout childhood in England and Wales. Pediatrics. 2009;123:e312–27 [DOI] [PubMed] [Google Scholar]
- 23.Perlman JM. Neurobehavioral deficits in premature graduates of intensive care: potential medical and neonatal environmental risk factors. Pediatrics. 2001;108:1339–48 [DOI] [PubMed] [Google Scholar]
- 24.Hack M, Flannery DJ, Schluchter M, Cartar L, Borawski E, Klein N. Outcomes in young adulthood for very-low-birth-weight infants. N Engl J Med. 2002;346:149–57 [DOI] [PubMed] [Google Scholar]
- 25.Vohr BR, Poindexter BB, Dusick AM, McKinley LT, Wright LL, Langer JC, Poole WK. NICHD Neonatal Research Network. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics. 2006;118:e115–23 [DOI] [PubMed] [Google Scholar]
- 26.Vohr BR, Poindexter BB, Dusick AM, McKinley LT, Higgins RD, Langer JC, Poole WK. National Institute of Child Health and Human Development National Research Network. Persistent beneficial effects of breast milk ingested in the neonatal intensive care unit on outcomes of extremely low birth weight infants at 30 months of age. Pediatrics. 2007;120:e953–9 [DOI] [PubMed] [Google Scholar]
- 27.Rees CM, Pierro A, Eaton S. Neurodevelopmental outcomes of neonates with medically and surgically treated necrotizing enterocolitis. Arch Dis Child Fetal Neonatal Ed. 2007;92:F193–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Behrman RE, Butler AS, editors. Preterm birth: causes, consequences, and prevention. Washington, DC: National Academies Press; 2009 [PubMed]
- 29.Sullivan S, Schanler RJ, Kim JH, Patel AL, Trawoger R, Kiechl-Kohlendorfer U, Chan GM, Blanco CL, Abrams S, Cotten CM, Laroia N, et al. An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J Pediatr. 2010;156:562,7.e1 [DOI] [PubMed] [Google Scholar]
- 30.Corpeleijn WE, Kouwenhoven SM, Pappa MC, van Vilet I, Scheerder I, Mulzer Y, Helder OK, van Goudoever JB, Vermeulen MJ. Intake of own mother's milk during the first days of life is associated with decreased morbidity and mortality in very low birth weight infants during the first 60 days of life. Neonatology. 2012;102:276–81 [DOI] [PubMed] [Google Scholar]
- 31.Jegier BJ, Johnson TJ, Engstrom JL, Patel AL, Loera F, Meier PP. The institutional cost of acquiring 100 mL of human milk for very low birth weight infants in the neonatal intensive care unit. J Hum Lact. 2013;29:390–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jegier BJ, Meier PP, Engstrom JL, McBride TM. The initial maternal cost of providing 100 mL of human milk for very low birth weight infants in the neonatal intensive care unit. Breastfeed Med. 2010;5:71–7 [DOI] [PMC free article] [PubMed] [Google Scholar]