Abstract
Objectives
The prevalence of hearing loss (HL) in adolescents has grown over the past decade, but hearing-related quality of life (QOL) has not been well-measured. We sought to develop a reliable, valid measure of hearing-related QOL for adolescents, the Hearing Environments And Reflection on Quality of Life (HEAR-QL).
Study Design
Multi-site observational study.
Methods
Adolescents with HL and siblings without HL were recruited from five centers. Participants completed the HEAR-QL and validated questionnaires measuring generic pediatric QOL (PedsQL), depression and anxiety (RCADS-25), and hearing-related QOL for adults (HHIA) to determine construct and discriminant validity. Participants completed the HEAR-QL two weeks later for test-retest reliability. We used exploratory principal components analysis to determine the HEAR-QL factor structure and measured reliability. Sensitivity and specificity of the HEAR-QL, PedsQL, HHIA and RCADS-25 were assessed. We compared scores on all surveys between those with normal hearing, unilateral and bilateral HL.
Results
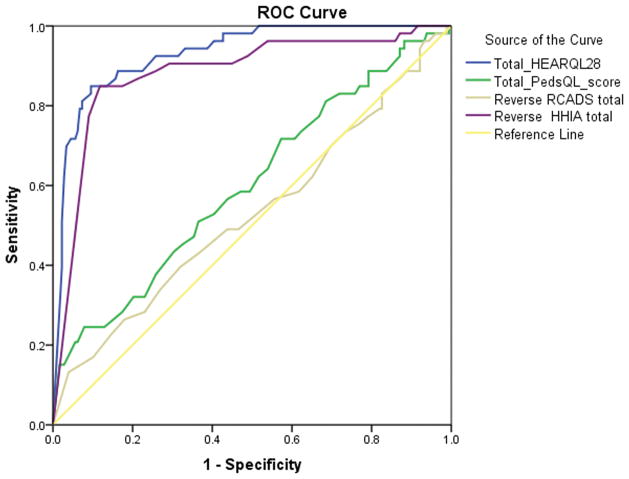
233 adolescents (13–18 years old) participated—179 with HL, 54 without HL. The original 45-item HEAR-QL was shortened to 28 items after determining factor structure. The resulting HEAR-QL-28 demonstrated excellent reliability (Cronbach’s alpha= 0.95) and construct validity (HHIA: r =.845, PedsQL: r =.587; RCADS-25: r =.433). The HEAR-QL-28 displayed excellent discriminant validity, with higher area under the curve (0.932) than the PedsQL (0.597) or RCADS-25 (0.529). Teens with bilateral HL using hearing devices reported worse QOL on the HEAR-QL and HHIA than peers with HL not using devices.
Conclusions
The HEAR-QL is a sensitive, reliable and valid measure of hearing-related QOL for adolescents.
Keywords: adolescents, quality of life, hearing loss, validation study
INTRODUCTION
The prevalence of hearing loss (HL) in adolescents in the United States has increased over the past decade, with rates of 19.5% for HL >15 dB and 5.3% for HL >25 dB.1 Adults with HL are 21–39% less likely to have attained post-secondary education than normal-hearing (NH) persons and are 1.5 to 2 times more likely to experience depression and career dissatisfaction.1–3 In children with HL, communication difficulties have been related to experiences of teasing, social isolation and maltreatment.4 Adolescence is a time during which social interactions and peer acceptance become increasingly important. Teens with HL who experience communication problems may have difficulty in establishing and maintaining relationships.
As the number of adolescents with HL grows, it is increasingly important to help these individuals realize their full educational, psychosocial and occupational potential. Treatment of HL may have substantial and lasting societal benefits, including the integration of children with HL into mainstream classrooms, higher educational attainment and improved career potential.3–5
Quality of life (QOL) is a key outcome of interest for children and adolescents with HL. Available questionnaires for adolescents with HL focus upon educational performance and hearing function. While many hearing assistive devices may improve audibility, it is also important to determine whether these treatments positively impact the QOL of adolescents with HL. In order to accurately assess the usefulness of interventions, healthcare providers need both age- and disease-specific tools. We previously validated a hearing-specific QOL scale, the Hearing Environments and Reflection on Quality of Life Questionnaire for children ages 7–12 years (HEAR-QL-26). We found large differences in hearing-related QOL between children with and without HL using the child HEAR-QL-26, and clinically significant differences between children with HL who wear and do not wear hearing devices.6
The objectives of this study were to validate an adolescent version of the HEAR-QL and to compare QOL using the HEAR-QL between adolescents with NH, unilateral and bilateral HL. We hypothesized that adolescents with HL would report worse QOL than NH adolescents.
METHODS
Study population
Participants were recruited for this cross-sectional validation study from five audiology and otolaryngology practices across the United States. Eligible adolescents with HL, 13–18 years of age, were identified using ICD-9 codes for HL. Siblings without HL in the same age range were also invited to participate. IRB approval was obtained at all participating institutions. Either written or implied informed consent was obtained from parents of all participants, and written or implied pediatric assent was obtained from all adolescents.
Eligibility criteria included permanent sensorineural, mixed, or conductive HL with a pure tone average of any three adjacent test-frequencies (e.g., 500, 1000, and 2000 Hz; or 2000, 4000 and 6000 Hz) of ≥ 30 dB hearing level in at least one ear. The control group consisted of siblings with NH in both ears, defined as a pure tone average < 20 dB hearing level in both ears at 500, 1000, and 2000 Hz, and threshold at 4000 Hz < 30 dB.
Potential participants were excluded if they had an ongoing temporary or fluctuating conductive HL, such as from otitis media; medical problem(s) associated with cognitive impairment (e.g., Down syndrome, congenital cytomegalovirus infection, history of chemotherapy); known cognitive impairment (defined as an IQ ≤ 70); or primary language other than English.
Research procedures
Three waves of study packets were mailed to potential participants and their parents, who could choose to return the hard-copy forms or complete the study forms online. Written informed consents and assents were returned with the hard-copy forms. Implied informed assent/consent was used for the online version; parents and participants indicated they had read the consent text and were willing to participate by clicking a consent/assent button.
Participants contacted the lead site if a NH sibling was willing to participate. Two weeks following receipt of the completed surveys, a second copy of the HEAR-QL was mailed to participants in order to assess test-re-test reliability.
Questionnaires
Participants completed four surveys: the adolescent HEAR-QL; the Pediatric Quality of Life Inventory™ (PedsQL™) 4.0;7 the Revised Child Anxiety and Depression Scale shortened form (RCADS-25);8 and the Hearing Handicap Inventory for Adults (HHIA).9, 10 The latter three validated surveys were used to determine concurrent and discriminant validity. Questionnaires were completed online, using the Research Electronic Database Capture system,11 or using paper versions, which were completed and returned by mail.
The adolescent HEAR-QL included 45 items based on experiences of children and adolescents with HL and their parents who previously participated in focus groups.12 A version for children ages 7–12 years was similarly validated with three factors emerging from the analysis: Environments, Activities and Feelings.6 The adolescent HEAR-QL was intended to be age-appropriate, addressing emotional, school and social issues specifically relevant to this age group. Relative to the children’s form, the adolescent form included items pertaining to hearing in social situations and interactions and fewer items about recess and playing. The adolescent form contained declarative statements, whereas the children’s form contained questions. Similar to the PedsQL Teen Form,7 adolescents are asked “how much of a problem” each situation has been for them “in the past month” using a five-point scale: “never” (1), “almost never” (2), “sometimes” (3), “often” (4) or “almost always” (5). Scores were reversed coded and transformed to a 0–100 scale, with higher scores indicating higher perceived QOL.
The PedsQL Teen Form (age 13–18) is a widely-used 23-item generic QOL measure with 15 items addressing psychosocial functioning (emotional, social and school subscales) and 8-items which deal with physical functioning.7 Response choices and scoring are the same as described above for the HEAR-QL. Higher scores indicate better QOL.
The RCADS-25 is a 25-item inventory with five subscales: social phobia, panic disorder, general anxiety disorder, separation anxiety disorder and major depressive disorder.8 RCADS-25 responses are scored on a four-point scale: “never” (0), “sometimes” (1), “often” (2), and “always” (3). Higher scores indicate more severe anxiety and depression.
The HHIA is a 25-item hearing-related QOL measure with a 13-item emotional subscale and a 12-item social/situational subscale typically used for monitoring intervention outcome in adults.9 A four-point scale is used: “Yes” (4), “Sometimes” (2), or “No” (0). Higher scores indicate worse hearing-related QOL.
In addition to completing these four questionnaires, participants reported if they used a hearing device (e.g., cochlear implant, hearing aids) and the frequency with which they used a device (“Never”, “Rarely”, “Sometimes”, or “Often”). Parents reported their teen’s age, sex, race/ethnicity, hearing status (NH, unilateral or bilateral HL), and HL severity (unilateral; mild, moderate, severe, profound bilateral), as well as parental marital status, medical insurance status, household income, and highest level of education.
Statistical analysis
We used exploratory principal components analysis (PCA) with varimax rotation to determine the underlying factor structure of the HEAR-QL and to reduce the number of items on the survey to minimize respondent burden. We used an iterative process of analysis, using an eigenvalue greater than 1.000 as the PCA criterion for factor identification, and Lautenschlager’s parallel analysis criteria,13 based on the work of Velicer,14 to determine the number of factors to retain. Items loading ≥ 0.600 on a factor or higher were retained; items were eliminated if they loaded ≥ 0.400 on more than one factor. The internal consistency of items on a factor was assessed using Cronbach’s alpha coefficient; items also were eliminated from the HEAR-QL if alpha could be increased by eliminating those items which, after discussion among three of the authors (TDR, DBJ, JECL), were determined to be redundant with other items. We assessed test-retest reliability of the HEAR-QL using the intraclass correlation coefficient (ICC).
We measured the construct validity of the adolescent HEAR-QL using Pearson r correlation coefficients comparing the HEAR-QL with each of the validated measures above. We expected the HEAR-QL to correlate highly with the HHIA and moderately with the PedsQL and the RCADS-25.
The ability of each measure and its subscale scores to discriminate between adolescents with and without HL was evaluated using two-sided t-tests. Sensitivity and specificity for the HEAR-QL were calculated to determine how well it would discriminate between adolescents with and without HL, plotted as receiver-operating-characteristics (ROC) curves, and compared using the area under the curve (AUC).
Analysis of variance (ANOVA) was used to compare HEAR-QL scores among adolescents with differing severity of HL. We conducted multivariable linear regression analysis with variables found to be associated with HEAR-QL scores in bivariate analysis. IBM SPSS Statistics version 20 (Armonk, New York) was used for all statistical analyses.
RESULTS
Of 555 letters sent out initially, 34 were returned (undelivered) and one child was ineligible for the study due to cognitive impairment. After three mailings, 233 participated (179 with HL, 54 siblings with NH; 44.8% of 520 eligible teens invited). Ninety-two (39.5%) responded electronically, and 141 (60.5%) responded via hard copies.
Table 1 shows the demographic characteristics of the participants. There were no significant differences between the NH, unilateral or bilateral HL groups. The frequency of hearing-device use by adolescents with unilateral and bilateral HL is shown in Table 2. Adolescents with bilateral HL used devices more frequently than adolescents with unilateral HL.
Table 1.
Demographic Characteristics of 226 Adolescent Participants, Ages 13–18 years, and Their Parents
| Variable | Normal Hearing (n = 54) | Unilateral HL (n = 63) | Bilateral HL (n = 109) |
|---|---|---|---|
| Age, mean (SD) | 15.6 (1.7) | 15.0 (1.6) | 15.4 (1.7) |
| Female, n (%) | 26 (48.1%) | 28 (44.4%) | 51 (46.8%) |
| Race/ethnicity, n (%) | |||
| White | 45 (83.3%) | 55 (87.3%) | 89 (81.7%) |
| African American | 4 (7.4%) | 4 (6.3%) | 7 (6.4%) |
| Asian or Pacific Islander | 3 (5.6%) | 2 (3.2%) | 4 (3.7%) |
| Native American/Alaska Native | 0 (0%) | 0 (0%) | 1 (0.9%) |
| Latino or Hispanic | 3 (5.6%) | 2 (3.2%) | 7 (6.4%) |
| Mixed or “other” | 2 (3.7%) | 2 (3.2%) | 8 (7.3%) |
| Family income, n (%) | |||
| <$10,000 | 2 (3.8%) | 4 (6.6%) | 5 (4.6%) |
| $10,000–$25,000 | 4 (7.5%) | 5 (8.2%) | 11 (10.2%) |
| $25,001–$40,000 | 1 (1.9%) | 4 (6.6%) | 6 (5.6%) |
| $40,001–$60,000 | 6 (11.3%) | 6 (9.8%) | 10 (9.3%) |
| $60,001–$80,000 | 3 (5.7%) | 8 (13.1%) | 14 (13.0%) |
| $80,001–$100,000 | 7 (13.2%) | 4 (6.6%) | 15 (13.9%) |
| Over $100,000 | 19 (35.8%) | 23 (37.7%) | 28 (25.9%) |
| No response | 11 (20.8%) | 7 (11.5%) | 19 (17.6%) |
| Maternal education level, n (%) | |||
| < High school diploma | 0 (0%) | 4 (6.3%) | 4 (3.7%) |
| Completed high school/GED | 6 (11.1%) | 12 (19.0%) | 22 (20.2%) |
| Some college/associate’s degree | 10 (18.5%) | 13 (20.6%) | 27 (24.8%) |
| College/bachelor’s degree | 21 (38.9%) | 16 (25.4%) | 33 (30.3%) |
| Postgraduate/advanced degree | 17 (31.5%) | 18 (28.6%) | 23 (21.1%) |
| Paternal education level, n (%) | |||
| < High school diploma | 2 (3.7%) | 7 (11.3%) | 6 (5.5%) |
| Completed high school/GED | 7 (13.0%) | 12 (19.4%) | 26 (23.9%) |
| Some college/associate’s degree | 9 (16.7%) | 14 (22.6%) | 27 (24.8%) |
| College/bachelor’s degree | 15 (27.8%) | 12 (19.4%) | 21 (19.3%) |
| Postgraduate/advanced degree | 21 (38.9%) | 16 (25.8%) | 28 (25.7%) |
| Missing | 0 (0%) | 1 (1.6%) | 1 (0.9%) |
| Severity of HL, n (%) | |||
| Mild | - | 6 (9.5%) | 11 (10.1%) |
| Moderate | - | 16 (25.4%) | 39 (35.8%) |
| Severe | - | 22 (34.9%) | 30 (27.5%) |
| Profound | - | 18 (28.6%) | 29 (26.6 %) |
| Missing | - | 1 (1.6%) | - |
| Insurance status, n (%) | |||
| Private | 49 (90.7%) | 47 (74.6%) | 76 (69.7%) |
| Public/Medicaid | 4 (7.4%) | 12 (19.0%) | 20 (18.3%) |
| Both private and public | 1 (1.9%) | 4 (6.3%) | 12 (11.0%) |
| None/unknown | 0 (0%) | 0 (0%) | 1 (0.9%) |
| Parent’s marital status, n (%) | |||
| Never married | 5 (9.3%) | 3 (4.8%) | 9 (8.3%) |
| Married and remarried | 44 (81.5%) | 45 (71.4%) | 80 (73.4%) |
| Divorced/separated | 5 (9.3%) | 11 (17.5%) | 20 (18.3%) |
HL, hearing loss; SD, standard deviation; GED, general equivalency degree
Table 2.
Participants Using Hearing Devices by Severity of Hearing Loss (HL)
| Hearing Device | Unilateral HL (n = 63) | Mild to Moderate Bilateral HL (n = 50) | Severe to Profound Bilateral HL (n = 59 ) |
|---|---|---|---|
| None | 47 (74.6%) | 19 (38%) | 6 (10.2%) |
| Any hearing device | 16 (25.4%) | 31 (63.3%) | 53 (89.8%) |
| Frequency-modulated | 5 (7.9%) | 4 (8.2%) | 14 (23.7%) |
| assistive listening system | |||
| Hearing aid – unilateral | 13 (20.6%) | 2 (4.1%) | 10 (17%) |
| Hearing aid – bilateral | 0 (0%) | 29 (59.2%) | 31 (52.5%) |
| Bone conduction device | 3 (4.8%) | 0 (0%) | 3 (5.1%) |
| Cochlear implant - unilateral | 0(0%) | 0 (0%) | 11 (18.7%) |
| Cochlear implant - bilateral | 0 (0%) | 0 (0%) | 4 (6.8%) |
N.B. Participants were separated by their approximate percentage usage and types of hearing devices into these three categories.
Principal components analysis for data reduction
Thirteen of the original 45 items were eliminated because they loaded at ≥ 0.400 on more than one factor in the PCA. Four factors emerged from the factor analysis: Social Interactions, School Difficulties, Feelings, and Hearing Situations. Four more items were subsequently removed due to redundancy in wording, resulting in a 28-item HEAR-QL. Table 3 demonstrates the internal consistencies of items on the total HEAR-QL-28 and subscales; Cronbach alphas were >0.85 with all participants and with only participants with HL.
Table 3.
Internal consistency at first administration and test-retest reliability for the total score and four subscales of the HEAR-QL-28 for adolescents.
| Cronbach’s alpha | Intraclass correlation coefficients (95% confidence interval [CI]) | ||
|---|---|---|---|
| All participants | HI participants | All participants | |
| Total score | 0.965 | 0.954 | 0.912 (0.881–0.935). |
| Social Interactions | 0.907 | 0.897 | 0.841 (0.788–0.881) |
| School Difficulties | 0.900 | 0.894 | 0.879 (0.837–0.911) |
| Feelings | 0.918 | 0.864 | 0.856 (0.807–0.893) |
| Hearing Situations | 0.909 | 0.850 | 0.880 (0.839–0.911) |
Test-retest reliability
After two weeks, 152 (60.8%) participants completed the HEAR-QL a second time (retest α = 0.974 [all participants], 0.966 [HL only]). Test-retest reliability was excellent (ICCs >0.850) between the first and second assessments of the HEAR-QL-28 (Table 3).
Construct validity
Correlations between the HEAR-QL-28 and the other instruments are shown in Table 4. Because the HHIA and HEAR-QL-28 both examined hearing-related QOL, the correlation between them was very high, regardless of whether all adolescents were analyzed or HL and NH participant data were analyzed separately (data not shown). The HEAR-QL-28 was moderately correlated with the PedsQL and the RCADS-25. The Feelings factor of the HEAR-QL-28 and the RCADS-25 also were moderately correlated.
Table 4.
Pearson correlation coefficients between HEAR-QL-28 and three other validated surveys for all participants (N = 226). All results were statistically significant, p < 0.001, except the results marked by * in which p <0.01.
| HEAR-QL-28 Total |
HEAR-QL-28 Social Interactions |
HEAR-QL-28 Hearing Situations |
HEAR-QL-28 School Difficulties |
HEAR-QL-28 Feelings |
|
|---|---|---|---|---|---|
|
| |||||
| PedsQL | |||||
| Total | 0.587 | 0.558 | 0.433 | 0.565 | 0.535 |
| Physical | 0.406 | 0.396 | 0.320 | 0.384 | 0.351 |
| Emotional | 0.436 | 0.439 | 0.296 | 0.366 | 0.443 |
| Social | 0.558 | 0.557 | 0.374 | 0.539 | 0.515 |
| School | 0.557 | 0.466 | 0.450 | 0.597 | 0.477 |
|
| |||||
| HHIA | |||||
| Total | −0.845 | −0.761 | −0.733 | −0.719 | −0.788 |
| Emotional | −0.802 | −0.686 | −0.675 | −0.676 | −0.790 |
| Social | −0.808 | −0.769 | −0.724 | −0.695 | −0.703 |
|
| |||||
| RCADS-25 | |||||
| Total | −0.443 | −0.375 | −0.297 | −0.407 | −0.467 |
| Major Depressive Disorder | −0.416 | −0.405 | −0.311 | −0.350 | −0.407 |
| Generalized Anxiety Disorder | −0.359 | −0.330 | −0.231 | −0.294 | −0.388 |
| Panic Disorder | −0.304 | −0.235 | −0.198* | −0.280 | −0.346 |
| Separation Anxiety Disorder | −0.261 | −0.230 | −0.170* | −0.245 | −0.269 |
| Social Phobia | −0.381 | −0.267 | −0.245 | −0.402 | −0.403 |
Note: Higher scores on the RCADS-25 and HHIA are indicative of more anxiety and depression, or a worse QOL, respectively, whereas higher scores on the HEAR-QL-28 are indicative of a better QOL.
Discriminative ability
Table 5 shows the HEAR-QL-28, PedsQL, HHIA and RCADS-25 scores in adolescents with NH and HL. Subscale and total HHIA and HEAR-QL-28 scores showed significantly worse QOL in adolescents with HL compared with NH adolescents. The PedsQL school subscale and total score also showed significantly worse QOL in adolescents with HL. However, there were no significant differences between groups on the RCADS-25.
Table 5.
Comparisons of the Adolescent Hearing Environments and Reflection on Quality of Life (HEAR-QL), Pediatric Quality of Life Inventory™ (PedsQL), the Hearing Handicap Inventory for Adults (HHIA), and the Revised Child Anxiety and Depression Scale, short form (RCADS-25) between Adolescents with Normal Hearing and Any Hearing Loss (HL) and between Adolescents with Unilateral HL and Bilateral HL.
| Scale | Normal Hearing (n =54) | Any HL (n = 172) | p* | Unilateral HL (n = 63) | Bilateral HL (n = 109) | p† |
|---|---|---|---|---|---|---|
|
| ||||||
| HEAR-QL, mean (SD), [range] | ||||||
| Social Interactions | 98 (7) [62–100] | 84 (21) [0–100] | <0.001 | 88 (17) [25–100] | 81 (23) [0–100] | 0.049 |
| Hearing Situations | 92 (12) [50–100] | 51 (22) [0–100] | <0.001 | 52 (21) [4–100] | 49 (23) [0–100] | 0.484 |
| School Difficulties | 96 (8) [64–100] | 69 (23) [0–100] | <0.001 | 71 (22) [14–100] | 67 (24) [0–100] | 0.288 |
| Feelings | 94 (11) [63–100] | 62 (25) [0–100] | <0.001 | 67 (23) [13–100] | 59 (27) [0–100] | 0.060 |
| Total | 95 (8) [70–100] | 67 (20) [0–100] | <0.001 | 70 (18) [18–100] | 64 (21) [0–100] | 0.083 |
|
| ||||||
| PedsQL, mean (SD), [range] | ||||||
| Physical | 88 (15) [25–100] | 86 (16) [19–100] | 0.371 | 89 (14) [44–100] | 84 (17) [19–100] | 0.045 |
| Emotional | 77 (20) [30–100] | 75 (20) [0–100] | 0.537 | 75 (21) [20–100] | 75 (21) [0–100] | 0.892 |
| Social | 87 (16) [20–100] | 81 (21) [0–100] | 0.052 | 85 (19) [25–100] | 78 (22) [0–100] | 0.033 |
| School | 79 (17) [45–100] | 70 (20) [0–100] | 0.001 | 70 (21) [15–100] | 69 (20) [0–100] | 0.632 |
| Total | 84 (14) [30–100] | 79 (15) [21–100] | 0.048 | 81 (15) [40–100] | 77 (16) [21–100] | 0.129 |
|
| ||||||
| HHIA, mean (SD), [range] | ||||||
| Emotional | 2 (6) [0–30] | 14 (12) [0–52] | <0.001 | 14 (12) [0–46] | 14 (12) [0–52] | 0.975 |
| Social | 2 (5) [0–24] | 12 (10) [0–48] | <0.001 | 10 (10) [0–40] | 13 (11) [0–48] | 0.153 |
| Total | 4 (11) [0–54] | 25 (21) [0–100] | <0.001 | 24 (20) [0–86] | 26 (21) [0–100] | 0.494 |
|
| ||||||
| RCADS-25, mean (SD), [range] | ||||||
| Major Depression | 2 (2) [0–10] | 2 (2) [0–12] | 0.467 | 2 (2) [0–10] | 2 (2) [0–12] | 0.942 |
| General Anxiety | 2 (2) [0–9] | 3 (3) [0–11] | 0.667 | 3 (3) [0–11] | 3 (3) [0–11] | 0.669 |
| Panic Disorder | 2 (3) [0–12] | 1 (2) [0–8] | 0.597 | 1 (2) [0–7] | 2 (2) [0–8] | 0.875 |
| Separation Anxiety | 1 (2) [0–11] | 1 (2) [0–14] | 0.523 | 1 (2) [0–8] | 1 (2) [0–14] | 0.403 |
| Social Phobia | 3 (3) [0–11] | 4 (3) [0–15] | 0.289 | 4 (3) [0–15] | 4 (3) [0–15] | 0.178 |
| Total | 11 (10) [0–48] | 12 (10) [0–55] | 0.704 | 11 (9) [0–42] | 12 (10) [0–55] | 0.436 |
Note: Higher scores indicate better QOL on the HEAR-QL and PedsQL, worse QOL on the HHIA, and greater depression and/or anxiety on the RCADS-25.
HL, hearing loss; SD, standard deviation
p values for comparisons between normal hearing and any HL.
p values for comparisons between unilateral and bilateral HL.
The social subscales of the PedsQL and HEAR-QL-28 showed worse QOL for adolescents with bilateral than unilateral HL. Neither the HHIA nor the RCADS-25 scores discriminated between these HL groups.
The ROC curves for the HEAR-QL-28, PedsQL, HHIA and RCADS-25 are plotted in Figure 1. The HHIA and RCADS-25 were reverse-scored on the ROC curve to denote better QOL with higher scores. The AUC, which illustrates how well the measurement categorizes persons as NH or HL, was highest for the HEAR-QL-28, followed by the HHIA, the PedsQL, and the RCADS-25. Sensitivities and specificities of the HEAR-QL-28 at various cutoff scores are shown in Table 6.
Figure 1.
Receiver operating curves for the 28-item Hearing Environments and Reflection on Quality of Life (HEAR-QL-28) questionnaire (area under the curve [AUC] = 0.932, 95% CI 0.896–0.968), (b) the Pediatric Quality of Life Inventory™ (PedsQL) questionnaire (AUC = 0.597, 95% CI 0.509–0.685), the Hearing Handicap Inventory for Adults (HHIA) (AUC = 0.883, 95% CI 0.826–0.940) and the Revised Child Anxiety and Depression Scale, shortened form (RCADS-25) (AUC = 0.529, 95% CI 0.436–0.621). The HHIA and RCADS-25 were reverse scored so that higher scores indicated better quality of life (HEAR-QL-28, PedsQL, and HHIA) and less severe anxiety/depression (RCADS-25).
Table 6.
Sensitivity and specificity of possible HEAR-QL-28 cutoff scores to discriminate adolescents with normal hearing from those with hearing impairment. Higher scores are suggestive of normal hearing, whereas lower scores are suggestive of hearing impairment.
| HEAR-QL-28 Cutoff Score | Sensitivity | Specificity |
|---|---|---|
| 65 | 100% | 36.9% |
| 70 | 98.1% | 49.7% |
| 75 | 94.4% | 62.0% |
| 80 | 92.6% | 72.1% |
| 85 | 88.9% | 83.8% |
| 90 | 85.2% | 90.5% |
| 95 | 72.2% | 95.5% |
Use of a hearing device was not associated with total scores on the HEAR-QL-28, PedsQL, HHIA, and RCADS-25 among adolescents with unilateral HL (Table 7) except for worse QOL on the School Difficulties subscale of the HEAR-QL-28. Adolescents with bilateral HL who used a device reported significantly worse scores on total and all HEAR-QL-28 subscales, the PedsQL Social subscale, and the HHIA total and Emotional subscale scores than those who did not use a device. The RCADS-25 scores did not change with device use/non-use.
Table 7.
Differences in mean (SD) Pediatric Quality of Life Inventory™ (PedsQL) Scores, Hearing Environments and Reflection on Quality of Life (HEAR-QL), Hearing Handicap Inventory for Adults (HHIA) and Revised Child Anxiety and Depression Scale, shortened form (RCADS-25) scores between adolescents with hearing loss (HL) who did and did not use a hearing device. Higher scores indicate better quality of life for the PedsQL and HEAR-QL, whereas lower scores indicate better quality of life for the HHIA and RCADS-25.
| Unilateral HL | Bilateral HL | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Scale | Used a Device (n = 16) | No Device (n = 47) | p | Used a Device (n = 84) | No Device (n = 25) | p |
|
| ||||||
| HEAR-QL | ||||||
| Social Interactions | 83 (18) | 90 (17) | 0.220 | 78 (24) | 92 (16) | 0.012 |
| Hearing Situations | 54 (21) | 51 (21) | 0.649 | 46 (22) | 60 (24) | 0.006 |
| School Difficulties | 62 (19) | 74 (22) | 0.043 | 63 (24) | 80 (20) | 0.002 |
| Feelings | 58 (23) | 70 (22) | 0.070 | 56 (27) | 71 (25) | 0.012 |
| Total | 64 (17) | 72 (18) | 0.134 | 61 (21) | 76 (19) | 0.002 |
|
| ||||||
| PedsQL | ||||||
| Physical | 86 (15) | 90 (13) | 0.310 | 83 (18) | 86 (12) | 0.491 |
| Emotional | 71 (19) | 77 (21) | 0.323 | 76 (21) | 72 (20) | 0.406 |
| Social | 80 (22) | 87 (17) | 0.160 | 75 (23) | 88 (15) | 0.011 |
| School | 65 (19) | 72 (22) | 0.233 | 67 (20) | 73 (20) | 0.204 |
| Total | 77 (16) | 83 (14) | 0.156 | 77 (16) | 80 (14) | 0.257 |
|
| ||||||
| HHIA | ||||||
| Emotional | 18 (13) | 12 (11) | 0.099 | 15 (12) | 9 (10) | 0.024 |
| Social | 13 (11) | 9 (9) | 0.173 | 14 (11) | 9 (8) | 0.059 |
| Total | 31 (23) | 22 (19) | 0.113 | 29 (22) | 18 (17) | 0.025 |
|
| ||||||
| RCADS-25 | ||||||
| Major Depression | 3 (3) | 2 (2) | 0.371 | 3 (3) | 2 (2) | 0.514 |
| General Anxiety | 3 (3) | 2 (3) | 0.181 | 3 (3) | 3 (3) | 0.878 |
| Panic Disorder | 2 (2) | 1 (2) | 0.166 | 2 (2) | 1 (2) | 0.863 |
| Separation Anxiety | 1 (2) | 1 (2) | 0.427 | 1 (2) | 1 (2) | 0.671 |
| Social Phobia | 4 (2) | 3 (3) | 0.373 | 4 (3) | 4 (3) | 0.697 |
| Total | 13 (8) | 10 (9) | 0.177 | 12 (10) | 12 (11) | 0.858 |
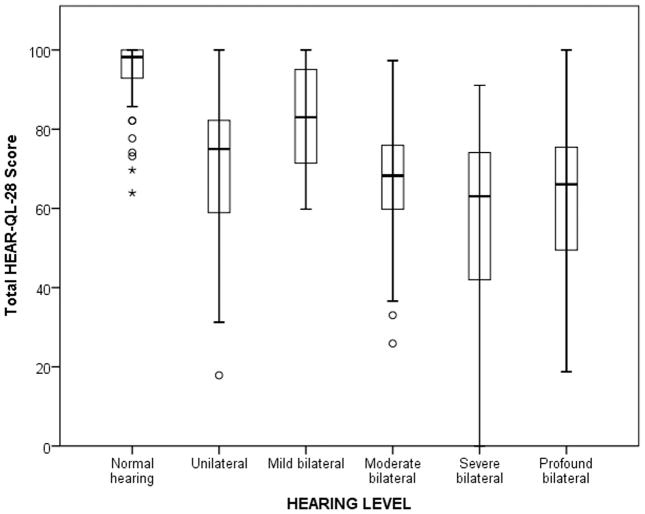
Table 8 shows the results of a multivariable regression model, with the total HEAR-QL-28 score as a dependent variable. Because HEAR-QL-28 scores did not differ to a clinically significant degree by severity of HL (Figure 2), hearing status was dichotomized as NH or any HL. Any HL, use of a hearing device, female gender, and lower maternal education levels were significantly associated with lower HEAR-QL-28 scores.
Table 8.
Multivariable linear regression of demographic variables, hearing status, and use of a hearing device on the Hearing Environments and Reflection on Quality of Life Scores (HEAR-QL-28).
| Variable | R2 | Nonstandardized β Coefficient | SE | Standardized β Coefficient | t value | p value |
|---|---|---|---|---|---|---|
|
| ||||||
| Step 1 | 0.062 | |||||
| Intercept | 39.67 | 14.42 | 2.75 | 0.006 | ||
| Age | 0.743 | 0.83 | 0.058 | 0.897 | 0.371 | |
| Male gender | 4.82 | 2.80 | 0.112 | 1.72 | 0.087 | |
| Maternal education | 4.21 | 1.22 | 0.225 | 3.46 | 0.001 | |
|
| ||||||
| Step 2 | 0.393 | |||||
| Intercept | 80.45 | 12.23 | 6.58 | <0.001 | ||
| Age | −0.118 | 0.691 | 0.001 | 0.018 | 0.986 | |
| Male gender | 5.42 | 2.28 | 0.132 | 2.509 | 0.013 | |
| Maternal education | 2.15 | 1.01 | 0.121 | 2.26 | 0.025 | |
| Any hearing loss | −21.04 | 3.03 | −0.415 | −6.941 | <0.001 | |
| Use/non-use of device | −11.54 | 2.6 | −0.266 | −4.435 | <0.001 | |
Figure 2.
Boxplot of HEAR-QL-28 scores by level of hearing loss, with possible scores of 1 to 100. Mean scores are indicated by the heavy horizontal line, interquartile range by the box, standard deviation by the whiskers, and outliers by circles (>1.5 SD) and asterisks (>3 SD). Post-hoc tests showed significant differences (p < .001) between those with normal hearing and all other levels of hearing loss except for mild bilateral hearing loss. Those with mild bilateral hearing loss had significantly higher scores than those with severe (p < .001) or profound (p = .005) bilateral hearing loss.
DISCUSSION
Our study showed that adolescents with HL experience significantly poorer hearing-related QOL than their NH peers on the validated HEAR-QL-28 on total and all subscales, confirming our hypothesis. Adolescents with HL also reported significantly lower QOL on the total and school subscale of the PedsQL. The ability of the adolescent HEAR-QL-28 to discriminate between those with and without HL was superior to the other tests used in the study (Figure 1). Siblings without HL were recruited as controls to minimize variability from socioeconomic status and family/school environment. However, it is possible that this group had higher hearing-related QOL than typical adolescents, given their experience with a family member with HL. We established the construct validity of the adolescent HEAR-QL-28 using three other validated questionnaires to demonstrate the specificity of the HEAR-QL-28 for hearing-related QOL.
We also hypothesized that adolescents with unilateral HL would report better QOL relative to adolescents with bilateral HL. However, we observed significant differences between these two groups only on the Social Interactions subscale of the HEAR-QL-28 and the Physical and Social subscales of the PedsQL (Table 4). These results suggest that unilateral HL affects the hearing-related QOL of adolescents to a similar degree as bilateral HL, and agree with prior research in children and adults with unilateral HL.6, 15
Similar to our findings in children with HL,6 adolescents with HL who used devices reported lower QOL than adolescents who did not use devices. This may be due to the stigma associated with wearing these devices.16, 17 Interestingly, these differences were significant only for adolescents with bilateral HL but not for those with unilateral HL; this may be related to the more conspicuous nature of devices commonly used in bilateral HL. Alternatively, children with lower QOL or their parents may be more motivated to use devices compared to children who perceive HL as less of a handicap. It is unknown what the QOL in these children would be if they did not utilize the devices; future studies could assess QOL before and after a device was initiated. While hearing aids do provide a benefit in QOL in adults, adolescents with HL may be less likely to wear them for fear of teasing and/or bullying.18 Educational programs for NH children and teens may serve to decrease stigma attached to using hearing devices and increase compliance with use amongst teens with HL.
Our results corroborate previous studies which suggested that HL can influence QOL and mental health. Van Eldik et al. found a higher percentage of mental health problems in teens with HL compared to NH teens (37% vs. 17%, respectively).19 Even with minimal sensorineural HL, children in the 3rd, 6th and 9th grades reported low self-esteem and higher stress levels.20 Parents of teenagers with HL reported high rates of perceived mental distress, emotional and conduct problems in their children; the teens reported high rates of peer-relationship problems.21 Children 8–12 years old with profound bilateral HL who used cochlear implants scored significantly lower than NH children on the KINDLR, a generic QOL survey, whereas the adolescents 13–16 years old with cochlear implants scored within the norm for NH.22 Possibly, the longer a child wears a device, the more accustomed he or she becomes to wearing it; thus QOL may improve after wearing a cochlear implant for many years. Another study using the KINDLR indicated that children and adolescents with cochlear implants reported similar QOL compared to their NH peers.23 However, generic surveys may not capture the issues that are particularly important to children with HL, as shown in the current study.
Intriguingly, adolescents with HL who did not wear devices reported better QOL than those who did, unlike studies of QOL in adults. In a study of veterans, hearing aid use resulted in sustained improvement in QOL social, environmental, and communication spheres.24 Adults also noted perceived benefits in QOL following cochlear implantation or bone-anchored hearing-aid implantation. A systematic review concluded that hearing aid use improves hearing-specific QOL in adults with sensorineural HL, though generic QOL instruments did not detect significant benefits.25 Adolescents may be more subject to ridicule than adults and may feel that hearing devices make them less “normal,” perhaps due to continuing development and susceptibility to emotional turmoil and social pressure.16 Adolescents with HL may encounter difficulties with speech and language comprehension that challenge their ability to communicate effectively both inside and outside of school and may lead to diminished self-esteem.19 Furthermore, adolescents with HL may choose not to wear hearing assistive devices, for cosmetic reasons or due to stigma, which might hamper communication.6, 16, 18, 26
This is one of the first hearing-related QOL questionnaires for adolescents validated psychometrically. The Youth Quality of Life Instrument – Deaf and Hard of Hearing Module (YQQL-DHH) is another recently developed hearing-related QOL instrument.17 Though the YQQL-DHH demonstrated good internal consistency and test-retest reliability, discriminative ability of this measure was not reported. We established the construct and discriminant validity of the HEAR-QL-28 using a generic QOL questionnaire for teens (PedsQL), a hearing-related QOL measure for adults (HHIA), and the RCADS-25 measure of depression and anxiety. We also showed that the HEAR-QL-28 discriminates between adolescents with and without HL very well. As expected, the HEAR-QL-28 correlated moderately with the PedsQL but had a strong correlation with the HHIA, as they were both assessing hearing-specific QOL issues. The RCADS-25 showed the lowest correlations with the HEAR-QL-28, which makes sense because anxiety and depression, though related to QOL, represent different constructs.
This validation study may be limited by self-selection bias. The participation rate was under 50%, and participants in our study were mostly white, from middle-to-higher income families, and had highly educated parents, which might limit the generalizability of our findings to other populations of teens with HL. Though we sampled a wide range of HL (unilateral and bilateral of varying severities), relatively few participants utilized cochlear implants, bone conduction devices and other devices. Further testing using the HEAR-QL is warranted to replicate our findings in other populations of adolescents with HL, especially in larger samples of teens who use various hearing devices.
Future work with the adolescent HEAR-QL-28 will focus on demonstrating the sensitivity to change in QOL following intervention as well as determining the minimal clinically important difference (either an improvement or deterioration) in total and subscale scores, which “would mandate, in the absence of troublesome side-effects and excessive cost, a change in patient’s management.”27
CONCLUSION
The adolescent HEAR-QL-28 is a sensitive, reliable and valid measure of hearing-related QOL for adolescents and discriminates between adolescents with and without HL.
Acknowledgments
The authors would like to acknowledge Roland Eavey, MD, SM, Donald Keamy, Jr. MD, MPH, Michael Cunningham, MD, Jerry Lin, MD, Banan Ead, Shana Lynn and Danielle Brown for their assistance with patient enrollment and recruitment. We also thank Dr. Jingxia (Esther) Liu in the Biostatistics Core of the Institute of Clinical and Translational Sciences and the Siteman Cancer Center for statistical support. Permission to use the Pediatric Quality of Life Inventory™ was received from the MAPI Research Institute.
Funding for this study was obtained from the American Hearing Research Foundation (AHRF) Wiley H. Harrison Memorial Research Award and the Clinical and Translational Science Award to Washington University funded by NIH/National Center for Research Resources (NCRR)/National Center for Advancing Translational Science (NCATS) grant (UL1RR024992). Dr. Lieu was supported in part by a National Institutes of Health (NIH) grant (K23 DC006638). Dr. Rachakonda also was supported by a training grant (5T32DC000022-2). Dr. Jeffe was supported in part by funding from the National Cancer Institute (NCI) Cancer Center Support Grant (P30 CA091842) to the Siteman Cancer Center for services provided through the Health Behavior, Communication and Outreach Core.
The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official view of the AHRF, NCRR, NCATS, NCI or NIH.
Footnotes
Level of Evidence: 2b (Diagnostic validation study, see http://www.cebm.net/index.aspx?o=1025)
Financial Disclosure Information: None.
Conflict of Interest: None
References
- 1.Shargorodsky J, Curhan SG, Curhan GC, Eavey R. Change in Prevalence of Hearing Loss in US Adolescents. JAMA. 2010;304(7):772–8. doi: 10.1001/jama.2010.1124. [DOI] [PubMed] [Google Scholar]
- 2.Teasdale TW, Sorensen MH. Hearing loss in relation to educational attainment and cognitive abilities: a population study. Int J Audiol. 2007;46(4):172–5. doi: 10.1080/14992020601089484. [DOI] [PubMed] [Google Scholar]
- 3.Woodcock K, Pole JD. Educational attainment, labour force status and injury: a comparison of Canadians with and without deafness and hearing loss. Int J Rehabil Res. 2008;31(4):297–304. doi: 10.1097/MRR.0b013e3282fb7d4d. [DOI] [PubMed] [Google Scholar]
- 4.Fellinger J, Holzinger D, Sattel H, Laucht M, Goldberg D. Correlates of mental health disorders among children with hearing impairments. Dev Med Child Neurol. 2009;51(8):635–41. doi: 10.1111/j.1469-8749.2008.03218.x. [DOI] [PubMed] [Google Scholar]
- 5.Mohr PE, Feldman JJ, Dunbar JL, et al. The societal costs of severe to profound hearing loss in the United States. Int J Technol Assess Health Care. 2000;16(4):1120–35. doi: 10.1017/s0266462300103162. [DOI] [PubMed] [Google Scholar]
- 6.Umansky AM, Jeffe DB, Lieu JE. The HEAR-QL: quality of life questionnaire for children with hearing loss. J Am Acad Audiol. 2011;22(10):644–53. doi: 10.3766/jaaa.22.10.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varni J. [Accessed March 14, 2013];Pediatric Quality of Life (Peds-QL) Inventory Administration Guidelines. Available at: URL: http://www.pedsql.org/PedsQLguidelines.doc.
- 8.Muris P, Meesters C, Schouten E. A Brief Questionnaire of DSM-IV Defined Anxiety and Depression Symptoms Among Children. Clinical Psychology and Psychotherapy. 2002;1(9):430–42. [Google Scholar]
- 9.Newman CW, Weinstein BE, Jacobson GP, Hug GA. The Hearing Handicap Inventory for Adults: psychometric adequacy and audiometric correlates. Ear Hear. 1990;11(6):430–3. doi: 10.1097/00003446-199012000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Newman CW, Weinstein BE, Jacobson GP, Hug GA. Test-retest reliability of the hearing handicap inventory for adults. Ear Hear. 1991;12(5):355–7. doi: 10.1097/00003446-199110000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Streufert A. Program in Audiology and Communication Sciences. Washington University School of Medicine; 2008. [Accessed 3-14-2013]. Quality of life measure for adolescents and children with hearing loss. Available at: http://digitalcommons.wustl.edu/pacs_capstones/437/ [Google Scholar]
- 13.Lautenschlager GJ. A Comparison of Alternatives to Conducting Monte Carlo Analyses for Determining Parallel Analysis Criteria. Multivariate Behavioral Research. 1989;24(3):365–95. doi: 10.1207/s15327906mbr2403_6. [DOI] [PubMed] [Google Scholar]
- 14.Velicer WF. Determining the number of components from the matrix of partial correlations. Psychometrika. 1976;41(3):321–7. [Google Scholar]
- 15.Newman CW, Jacobson GP, Hug GA, Sandridge SA. Perceived hearing handicap of patients with unilateral or mild hearing loss. Ann Otol Rhinol Laryngol. 1997;106(3):210–4. doi: 10.1177/000348949710600305. [DOI] [PubMed] [Google Scholar]
- 16.Kent B, Smith S. They only see it when the sun shines in my ears: exploring perceptions of adolescent hearing aid users. J Deaf Stud Deaf Educ. 2006;11(4):461–76. doi: 10.1093/deafed/enj044. [DOI] [PubMed] [Google Scholar]
- 17.Patrick DL, Edwards TC, Skalicky AM, et al. Validation of a quality-of-life measure for deaf or hard of hearing youth. Otolaryngol Head Neck Surg. 2011;145(1):137–45. doi: 10.1177/0194599810397604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horowitz JA, Vessey J, Carlson KL, et al. Teasing and bullying experiences of middle school students. J Am Nurses Assoc. 2005;10(4):165–72. [Google Scholar]
- 19.van Eldik T. Mental health problems of Dutch youth with hearing loss as shown on the Youth Self Report. Am Ann Deaf. 2005;150(1):11–6. doi: 10.1353/aad.2005.0024. [DOI] [PubMed] [Google Scholar]
- 20.Bess FH, Dodd-Murphy J, Parker RA. Children with minimal sensorineural hearing loss: prevalence, educational performance, and functional status. Ear Hear. 1998;19(5):339–54. doi: 10.1097/00003446-199810000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Fellinger J, Holzinger D, Beitel C, Laucht M, Goldberg DP. The impact of language skills on mental health in teenagers with hearing impairments. Acta Psychiatr Scand. 2009;120(2):153–9. doi: 10.1111/j.1600-0447.2009.01350.x. [DOI] [PubMed] [Google Scholar]
- 22.Huber M. Health-related quality of life of Austrian children and adolescents with cochlear implants. Int J Pediatr Otorhinolaryngol. 2005;69(8):1089–101. doi: 10.1016/j.ijporl.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 23.Loy B, Warner-Czyz AD, Tong L, Tobey EA, Roland PS. The children speak: an examination of the quality of life of pediatric cochlear implant users. Otolaryngol Head Neck Surg. 2010;142(2):247–53. doi: 10.1016/j.otohns.2009.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mulrow CD, Aguilar C, Endicott JE, et al. Quality-of-life changes and hearing impairment. A randomized trial. Ann Intern Med. 1990;113(3):188–94. doi: 10.7326/0003-4819-113-3-188. [DOI] [PubMed] [Google Scholar]
- 25.Chisolm TH, Johnson CE, Danhauer JL, et al. A systematic review of health-related quality of life and hearing aids: final report of the American Academy of Audiology Task Force On the Health-Related Quality of Life Benefits of Amplification in Adults. J Am Acad Audiol. 2007;18(2):151–83. doi: 10.3766/jaaa.18.2.7. [DOI] [PubMed] [Google Scholar]
- 26.Johnson CE, Danhauer JL, Gavin RB, Karns SR, Reith AC, Lopez IP. The “hearing aid effect” 2005: a rigorous test of the visibility of new hearing aid styles. Am J Audiol. 2005;14(2):169–75. doi: 10.1044/1059-0889(2005/019). [DOI] [PubMed] [Google Scholar]
- 27.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407–15. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]