Abstract
Tremendous progress has been made with the scale-up of antiretroviral therapy in Africa, with an estimated seven million people now receiving antiretroviral therapy in the region. The long-term success of antiretroviral therapy programs depends on appropriate strategies to deal with potential threats, one of which is the emergence and spread of antiretroviral drug resistance. Whilst public health surveillance forms the mainstay of the World Health Organization approach to antiretroviral drug resistance, there is likely to be increasing demand for access to drug resistance testing as programs mature and as HIV clinical management becomes more complex. African-owned research initiatives have helped to develop affordable resistance testing appropriate for use in the region, and have developed delivery models for resistance testing at different levels of the public health system. Some upper-middle-income countries such as Botswana and South Africa have introduced drug resistance testing for selected patient groups to guide clinical management. The scale-up of resistance testing will require substantial expansion of clinical and laboratory capacity in the region, but the expertise and resources exist in Africa to support this. The long-term population health impact and cost-effectiveness of resistance testing in the region will also require further investigation.
Keywords: HIV-1, Drug resistance, Antiretroviral therapy, Treatment failure
Introduction
The scale-up of antiretroviral therapy (ART) for the treatment of HIV infection has been one of the largest and most successful public health initiatives in recent years. In sub-Saharan Africa, which accounts for approximately 70% of all people living with HIV (an estimated 25 million), improved access to treatment in the last decade has had profound benefits and has transformed HIV from a death sentence to a manageable chronic disease1. The long-term success of HIV treatment programs is still threatened by certain issues, one of which is antiretroviral drug resistance2. The emergence and transmission of drug-resistant HIV has the potential not only to impair individual health outcomes, but also to limit the population-level benefits of ART3.
In 2012, an estimated seven million people were receiving ART in sub-Saharan Africa, largely through the public health approach recommended by the World Health Organization (WHO), with standardized drug regimens and simplified monitoring systems1. The WHO global strategy for the prevention and assessment of drug resistance has three main components: monitoring of HIV drug resistance early warning indicators; surveys of acquired drug resistance in populations receiving ART and surveys of transmitted drug resistance in recently infected populations4-6. This strategy focuses on population-based methods assuming individualized assessment of drug resistance is not available or affordable in the majority of low- and middle-income countries. However, as HIV treatment programs mature and clinical management becomes more complex, there is likely to be a need for more advanced diagnostic tools, such as drug resistance testing, to assist treatment monitoring and to guide clinical decision-making7,8. In this article, we provide an update on the current knowledge about HIV drug resistance levels in Africa and recent advances in genotypic resistance testing and consider the potential role of drug resistance testing in routine clinical care.
Current status of drug resistance
Adult transmitted resistance
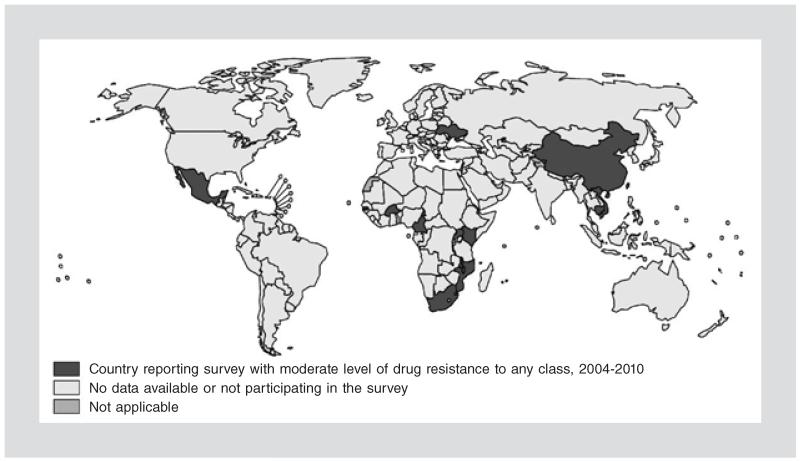
The WHO HIV Drug Resistance Report 2012 summarized the results from 72 surveys of transmitted drug resistance in 26 countries between 2004 and 2010 (60% of the surveys were from the African region)9. While the majority of surveys (n = 52; 72.2%) found a low prevalence (< 5%) of drug resistance-associated mutations (DRAM) in all three drug classes, there was an increase over time in surveys reporting moderate prevalence (5-15%) of DRAM for at least one class. In Africa, seven countries have had at least one survey reporting a moderate prevalence of DRAM (Fig. 1), and the proportion of surveys reporting moderate prevalence of DRAM increased from 17.6% in 2004-2006 to 40.7% in 2007-20109.
Figure 1.
Location of World Health Organization surveys with moderate levels (5-15%) of drug resistance to any drug class (reproduced with permission from World Health Organization HIV drug resistance report9). The seven African countries are Burkina Faso, Cameroon, Kenya, Malawi, Mozambique, South Africa, and Uganda.
In a systematic review of 218 datasets from 2001-2011 containing data on 26,102 untreated adults (15 years or older), a similar increase in transmitted drug resistance over time was revealed10. The increase was most pronounced in East Africa, where the prevalence of any DRAM increased from 0.9% (95% CI: 0.5-1.6) to 7.4% (95% CI: 4.2-12.9) after 8-9 years of program roll-out. The increase was less pronounced in Southern Africa, from 2.1% (95% CI: 1.6-2.6) to 3.7% (95% CI: 2.5-5.4) after 5-7 years. A separate review of studies specifically from South Africa, home to the largest ART program in the world, found no evidence of an increase in transmitted drug resistance between 2002 and 2010, and apart from 2002, the level was below 5%11. However, one study in the KwaZulu-Natal region of South Africa has reported approximately 6% of naive patients with DRAM12.
Adult acquired resistance
The majority of adults treated with ART achieve virological suppression. Systematic reviews have shown that around three-quarters of adults initiated on ART in low- and middle-income countries are still on therapy with virological suppression (< 1,000 copies/ml) at 12 months13, although there seems to be substantial variation in program performance14. Surveillance for acquired resistance usually involves sampling those individuals with viremia > 1,000 copies/ml at around 12 months of ART, which corresponds to 1-2 in 20 of all adults who initiated ART.
In the WHO African region, an estimated 70% of adults with viremia > 1,000 copies/ml at 12 months had at least one DRAM9. As most individuals surveyed (87%) were receiving regimens which included thymidine analogues (stavudine or zidovudine), the prevalence of thymidine analogue mutations (TAM) was of particular interest as these mutations can confer cross-resistance and impair susceptibility to standard second-line regimens. A total of 13.4% of adults in the WHO African region had one or more TAM9. Similar results have been reported from other multicentre studies. The PharmAccess African Studies to Evaluate Resistance (PASER), which incorporated data from 13 sites in six African countries, estimated 70.4% of those with viral load > 1,000 copies/ml after 11-15 months of first-line ART to have at least one DRAM and 8.5% to have one or more TAM15. Another study involving countries in West Africa and in south-east Asia, reported 71.0% of those with viral load > 1,000 copies/ml at 12 months to have at least one DRAM and 13.8% to have one or more TAM14. A recently published study in rural KwaZulu-Natal identified a much higher level of resistance in patients with longer duration of ART including thymidine analogues (medium duration on ART 42 months. In this study, 40% of patients had one or more TAM and 15% of patients had a genotypic susceptibility score for the standard second-line regimen of less than two, suggesting a significantly compromised regimen16.
Recently, tenofovir disoproxil fumarate (TDF) was added as part of first-line ART regimens in Africa. Drug resistance studies are emerging about the use of TDF. At present, mixed reports have been presented in South Africa, where HIV-1 subtype C dominates the epidemic. One study pointed to a failure rate of 6% (35/585) at six months of ART, but with very high levels (69.7%; 23/33) of K65R, which is one of the main mutations causing resistance to TDF17. However, a more recent study did not see this effect, with 16% (270/1,682) of patients failing ART at six months but only 12% (5/40) of the genotyped patients with K65R18. It is important to note that the two studies were done on subtype C viruses and used low sample numbers. Subtype C has been reported to develop K65R with greater propensity than other subtypes19 and more research is needed to determine the patterns and impact of drug resistance with TDF-based regimens.
Pediatric acquired resistance
Studies of pediatric drug resistance are often limited by difficulties in combining data for children on nonnucleoside reverse transcriptase inhibitor (NNRTI)-based and protease inhibitor (PI)-based regimens, and by the lack of data on the presence of drug resistance prior to ART. In a systematic review of 30 studies, including children on both NNRTI-based and PI-based regimens, the pooled proportion of children with at least one DRAM was 90% (95% CI: 88-93). The proportion was considerably higher in NNRTI-exposed children than in PI-exposed children (88 vs. 54%) and the high proportion with at least one TAM (56%) was also noteworthy20.
The relatively low proportion of children failing ritonavir-boosted PI-based regimens with resistance has also been reported from individual programs21. This not only highlights the challenges of HIV treatment and care in the population of young children, but also underlines the potential importance of drug resistance testing for this group, especially as there is little evidence to inform standardized second-line options in this group.
Importance and impact of drug resistance testing
The most common form of resistance testing is genotypic resistance testing, where HIV-specific mutations known to be associated with reduced susceptibility to certain antiretroviral drugs are detected. Individualized resistance testing is routinely used in high-income countries prior to ART and at the time of virological failure in order to guide clinical management22-25. Within developing countries, where a sequence of standardized ART regimens is carefully chosen, taking into account potential drug resistance, the role of resistance testing is, at present, less clear26-28. However, as clinical case management becomes more complex and as more drugs and regimens are used over time, the demand for individualized resistance testing to guide clinical management of virological failure is likely to increase.
The potential benefits of resistance testing are not restricted to selecting an appropriate drug regimen in the presence of DRAM. The absence of drug resistance can point to particularly poor adherence, the undisclosed interruption of therapy, or problems with drug dosing or absorption. Accurately identifying these issues allows for targeted interventions to be made in order to conserve first-line regimens. Studies from South Africa using standard population sequencing have reported 5-33% of adults with virological failure on first-line ART to have wild-type genotypes29. The PASER study in six sub-Saharan countries also documented a relatively high proportion (30%) with wild-type genotype15. In the absence of resistance testing, these individuals will be switched to second-line ART regimens and the root cause of their virological failure may not be addressed. This may partially explain the poorer outcomes on second-line ART for individuals with wild-type genotype30,31 and also the high levels of wild-type genotype in studies reporting early virological failure on second-line regimens in Africa (38-85% had no DRAM at the time of second-line ART failure)32-35.
The association between virological failure on second-line regimens and subtherapeutic drug concentrations before and after regimen switch, further strengthens the interpretation that unresolved adherence issues remain a significant driver of second-line ART failure30,35. Even in settings with routine viral load monitoring, the identification of treatment failure can be difficult and decisions around whether or not to switch can be complex30,36. At the root of this are the challenges in accurately assessing antiretroviral adherence37 as well as the relative paucity of evidence-based adherence interventions38. Whether outcomes could be improved, through the use of genotypic resistance testing to identify those with poor adherence and to target adherence interventions, requires further investigation.
In high-income countries, the use of genotypic resistance testing to guide regimen selection in adults with virological failure has been shown to have a positive, albeit modest, impact on subsequent virological outcomes39-41. There is as yet no published evidence about the effectiveness of resistance testing in Africa, although there is at least one clinical trial investigating the impact of pre-ART resistance testing on virological outcomes of first-line ART42. Estimates from mathematical modeling studies have suggested that, in the context of the South African ART program, genotypic resistance testing would have a modest beneficial effect on clinical outcomes43 and would be cost-effective at failure of first- and second-line ART43,44.
The cost-effectiveness of genotyping at failure of first-line ART was shown to be particularly sensitive to the prevalence of wild-type genotype: resistance testing was estimated to be very cost-effective (i.e. the incremental cost-effectiveness ratio was less than the per capita gross domestic product) when the prevalence of wild-type genotype was! 12% and the cost of drug resistance testing was US$ 250. Given the recent decrease in costs of genotyping, resistance testing is expected to become more affordable and cost-effective. For example, in Botswana, the cost of second-line ART is three-times the costs of first-line ART and third-line ART is ten-times the cost of first-line. A resistance genotype in Botswana would cost approximately the same as one month on third-line therapy.
If higher levels of transmitted drug resistance (> 15%) are documented during public health surveillance, resistance testing prior to treatment to guide first-line regimen choice might be required6. Whether or not the use of resistance testing would be a more cost-effective strategy than modification of the standard regimens for all individuals (for example from a NNRTI-based to a PI-based first-line regimen) will require further research, should the situation arise.
Opportunities for resistance testing within the public health approach to antiretroviral therapy
In most low- and middle-income countries, ART is delivered through the public health approach, with standardized drug regimens and simplified laboratory monitoring. Drug regimens are selected on the basis of predicted drug resistance patterns, and regimen sequencing aims to achieve optimal long-term ART efficacy26-29,45. The use of routine viral load monitoring is intended to monitor adherence, limit the emergence of drug resistance, and enable regimen switching before the onset of immunological and clinical failure46.
High coverage of routine virological monitoring has so far been achieved only in South Africa and Botswana, but other countries are scaling up the implementation of viral load testing47. In South Africa, the implementation of routine virological monitoring has required rapid growth in laboratory capacity, with 17 laboratories now performing almost two million viral load tests annually48,49. In the past three years, the South African National Health Laboratory Service (NHLS) has also scaled up laboratory capacity to deliver Xpert MTB/RIF testing for the diagnosis of tuberculosis and antituberculosis drug resistance50. Whilst these laboratory systems are still largely centralized, there are plans to decentralize services as appropriate technologies and systems are developed49. In Botswana, where viral load monitoring was offered from the beginning of the national ART program and laboratory services are largely decentralized, there are now 24 laboratories performing routine viral load monitoring. The rapid scale-up of Xpert MTB/RIF testing is also underway.
In both South Africa and Botswana, genotypic resistance testing is now recommended for adults when virological failure occurs on second-line ART51,52. This is in order to preserve second-line regimens due to the limited availability and the high cost of third-line regimens. Additional priority groups in both countries include children with virological failure on PI-based regimens (first- or second-line)51,52. Specialist treatment failure management teams to coordinate the management of complex cases have already been established in Botswana52 and are planned in South Africa.
Recent advances with genotypic resistance testing
The main barriers to implementation of genotypic resistance testing have been related to the cost, the need for complex laboratory infrastructure, and issues with specimen transport to centralized laboratories. In the past decade, there has been a rapid evolution of genome sequencing technologies and this has driven huge reductions in genome sequencing costs53. Whilst these cost reductions can be slow to translate into more affordable technologies for use in clinical practice, there is already evidence that this can happen. The Southern African Treatment and Resistance Network (SATuRN) has developed laboratory methods to reduce the cost of resistance testing and has, through collaboration with a major biotechnology company, enabled access to cheaper sequencing reagents54. The Affordable Resistance Test for Africa (ART-A) initiative has similarly developed and validated simple, robust genotyping methods specifically designed for subtype C viruses55-57. In both of these initiatives, cost reductions were achieved through a reduction in the number of sequencing primers, a reduction in reagent volumes, simplification of polymerase chain reaction methods, and targeted amplification of reverse transcriptase and protease fragments or reverse transcriptase alone16,55-58. The availability of open-source bioinformatics software and publicly accessible databases specific to the region also help to reduce costs associated with the analysis and interpretation of genotypic data and to maximize the value of the data generated through drug resistance testing59.
Standard genotypic resistance testing incorporates population (Sanger) sequencing methods. One limitation of this method is the inability to detect minority variants present at frequencies below 20%25. The use of next-generation sequencing technologies allows detection of these minority variants60. Further research is necessary to determine the true significance of minority variants in relation to clinical outcomes, and to compare the cost-effectiveness and impact of different sequencing technologies.
The issue of specimen collection, handling, and transport to centralized laboratories is an important one in low- and middle-income countries, where the laboratory infrastructure often exists remotely from where patients access healthcare. Dried blood spots (DBS) are easy to collect in the field, easily transported, and HIV-1 nucleic acids remain stable on DBS for long periods at ambient temperatures61. Several studies have reported successful genotyping from DBS61,62. However, the sensitivity is lower than from whole plasma specimens and depends largely on the HIV-1 viral load. In a study involving ten WHO/HIVResNet-accredited laboratories, HIV-1 was successfully amplified for more than half the replicates with viral load 1,000 copies/ml in only two of ten laboratories. At a threshold of 10,000 copies/ml, seven of ten laboratories were able to successfully amplify more than half the replicates63.
Scaling up capacity for public health implementation
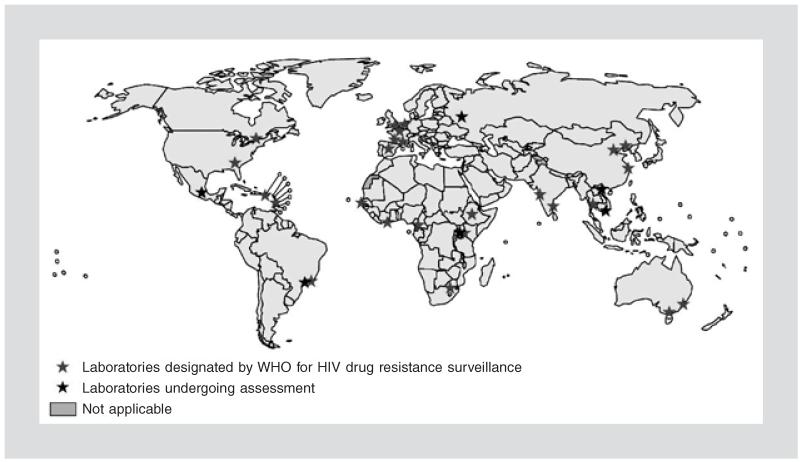
At present, drug resistance surveillance activities in low- and middle-income countries are coordinated through a network of national and regional WHO-accredited genotyping laboratories. As of 2011, this included laboratories in seven African countries (Fig. 2). Both the PASER and SATuRN networks are working to develop laboratory capacity in order to provide quality assured genotypic resistance testing in the region58,64,65. Implementation of resistance testing in the clinical care context would require substantial expansion of existing laboratory capacity. Given the laboratory infrastructure required and the relative complexity of the techniques, it is unlikely that genotypic resistance testing could be decentralized below the level of provincial or national laboratories.
Figure 2.
WHO-accredited laboratories performing HIV drug resistance testing for public health surveillance (reproduced with permission from World Health Organization HIV drug resistance report9). This includes laboratories in Cameroon, Cote d’Ivoire, Ethiopia, Kenya, Senegal, South Africa, and Uganda.
In addition to the expansion of laboratory capacity, introducing resistance testing into clinical care will require the parallel development of clinical capacity. Genotypic resistance testing provides most value when the results are interpreted by a specialist clinician in parallel with relevant clinical information. In sub-Saharan Africa, clinical virologists and specialist HIV clinicians are a scarce resource. There is, therefore, a need to expand teaching on HIV drug resistance in existing training programs and to develop educational methods around drug resistance for frontline healthcare workers. It is likely that initially services would be centralized around existing clinical and laboratory expertise, but systems could be decentralized over time as demand grows. This is the model that has been adopted in Botswana52 and it is also similar to how programs for the management of drug-resistant tuberculosis (TB) have evolved in South Africa66.
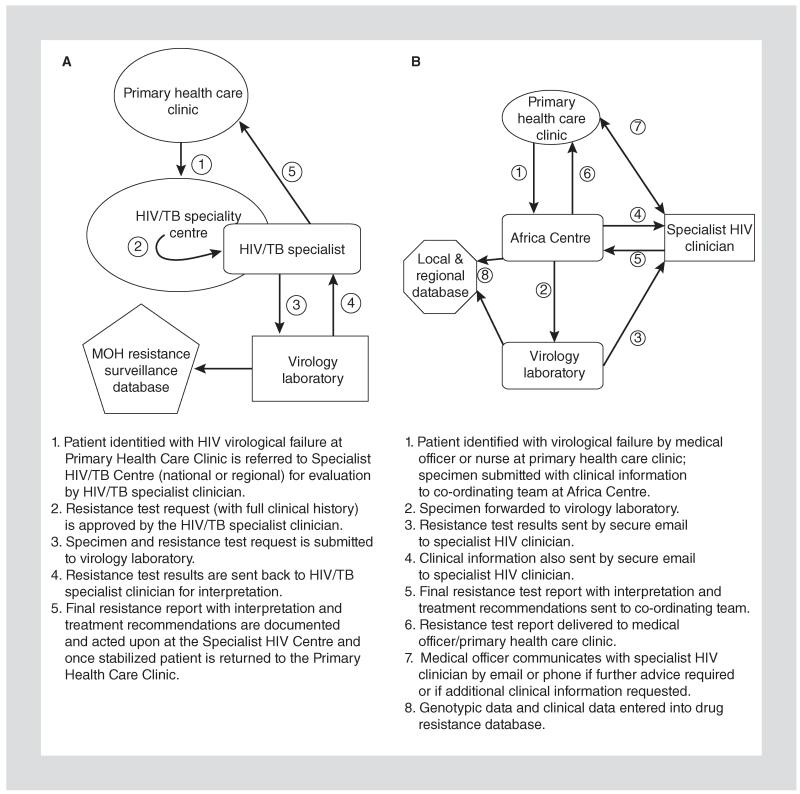
The Botswana national ART program currently incorporates the use of genotypic resistance testing, primarily at the time of second-line ART failure in adults52. Capacity for resistance testing has been available since the beginning of the national program in 2002 and resistance testing is carried out at one reference laboratory, located in Gaborone. With the maturation of the ART program, the demand for resistance testing has continued to increase and with it the need for a more decentralized HIV specialist care model. Therefore, plans are now underway to develop HIV/TB specialty centers in six districts across Botswana in order to meet the need for advanced clinical management of both HIV and TB. These centers will build upon existing HIV/TB specialty care and also allow for more decentralized HIV/TB clinical training and HIV/TB resistance surveillance. This model of care is illustrated in figure 3. Under this model, identification of second-line virological failure at primary healthcare clinics and district hospitals prompts referral of the patient to one of six HIV/TB specialty centers. After assessment at these centers, a specimen is submitted to the laboratory for HIV genotyping with a form containing clinical information (including a detailed treatment history), which has been approved by an HIV specialist clinician on the basis of the clinical information provided. Once the resistance report is generated, it is interpreted by the same specialist clinician, who then sends the report with interpretation and management recommendations directly back to the referring doctor.
Figure 3.
Models for the implementation of HIV-1 genotypic resistance testing for routine clinical management: Botswana national model (A) and a primary healthcare HIV program in Hlabisa sub-district, KwaZulu-Natal, South Africa (B).
A similar model has been adapted for the primary healthcare context by SATuRN and has been implemented in Hlabisa sub-district in northern KwaZulu-Natal, South Africa16. The difference in this model is that patients receive care throughout at the primary healthcare clinic, while specimens are transported to a central laboratory and the specialist clinician can function remotely through electronic communication (Fig. 3). A feature of both these models is the integration of data systems where the sequence data is accumulated along with clinical information67. These databases can then be used by frontline healthcare workers for patient management, but can also be resources for real-time surveillance, research, and training59,67.
Other than these examples, there is a paucity of published evidence around the use of genotypic resistance testing for clinical care in Africa and there is certainly the need to develop and evaluate different systems for the programmatic implementation of genotypic resistance testing.
Challenges for implementation
There are substantial challenges around the expansion of laboratory monitoring strategies in low- and middle-income countries, as previously highlighted in the context of viral load testing68. However, the scale-up of laboratory capacity to deliver CD4+ T-cell count and viral load testing also provides a framework through which genotypic resistance testing could be introduced. However, CD4+ T-cell count and viral load technologies are starting to move out of the laboratory to more peripheral levels of the health system where patients access care69,70. From the perspective of frontline healthcare workers, technologies integrating viral load measurement and identification of DRAM might have the most value in low- and middle-income countries and it is important that such tools are developed and evaluated.
The interpretation of genotypic resistance data is complex. A number of algorithms exist to assist with interpretation, such as the Stanford HIVdB71, Rega algorithm72 and the ANRS algorithm73. Whilst the algorithms do differ in their interpretation of mutational patterns, particularly for non-B HIV-1 subtypes74, the evidence suggests that they perform equally well in terms of predicting virological response to subsequent antiretroviral regimens75. SATuRN hosts a mirror of RegaDB and of Stanford HIVdB in order to gather and analyze subtype C HIV-1 sequences. This data is then used to guide regional public health policies59.
Lastly, while genotypic resistance testing might have a role in routine HIV care in Africa, we should be cautious about the extent to which health technologies can contribute to improved programmatic and population outcomes. Resistance testing should not be seen as a technological solution to the problem of drug resistance. Long-term reductions in the emergence and spread of drug resistance will best be achieved by improving the quality of care in HIV programs in low- and middle-income countries76.
Conclusions
Genotypic resistance testing may become an increasingly important component of routine care in Africa as HIV programs mature. Local research and development, coupled with advancements in genomic sequencing technologies, have made resistance testing affordable for upper-middle-income countries such as South Africa and Botswana and models for implementation in these countries are continuing to be developed. The introduction of resistance testing to support clinical care will require substantial expansion of laboratory and clinical capacity. To guide the future scale-up of resistance testing, research is needed to demonstrate its impact on individual clinical outcomes and population health outcomes.
Footnotes
Conflicts of interest and source of funding
Tulio de Oliveira is the Director and Richard Lessells is an Executive Committee Member of the Southern African Treatment and Resistance Network (SATuRN). Richard Lessells and Tulio de Oliveira are supported by the Wellcome Trust (grant numbers 090999/Z/09/Z and 082384/Z/07/Z).
References
- 1.Joint United Nations Programme on HIV/AIDS (UNAIDS) [Accessed 7 October 2013];Global report: UNAIDS report on the global AIDS epidemic 2013. 2013 http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf
- 2.Hamers R, Kityo C, Lange J, Wit T, Mugyenyi P. Global threat from drug resistant HIV in sub-Saharan Africa. BMJ. 2012;344:e4159. doi: 10.1136/bmj.e4159. [DOI] [PubMed] [Google Scholar]
- 3.Cambiano V, Bertagnolio S, Jordan M, Lundgren J, Phillips A. Transmission of drug resistant HIV and its potential impact on mortality and treatment outcomes in resource-limited settings. J Infect Dis. 2013;207(Suppl 2):S57–62. doi: 10.1093/infdis/jit111. [DOI] [PubMed] [Google Scholar]
- 4.Bennett D, Bertagnolio S, Sutherland D, Gilks C. The World Health Organization’s global strategy for prevention and assessment of HIV drug resistance. Antivir Ther. 2008;13(Suppl 2):1–13. [PubMed] [Google Scholar]
- 5.Jordan M, Bennett D, Wainberg M, et al. Update on World Health Organization HIV Drug Resistance Prevention and Assessment Strategy: 2004-2011. Clin Infect Dis. 2012;54(Suppl 4):S245–9. doi: 10.1093/cid/cis206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization [Accessed 7 October 2013];World Health Organization global strategy for the surveillance and monitoring of HIV drug resistance: an update. 2012 http://apps.who.int/iris/bitstream/10665/77349/1/9789241504768_eng.pdf
- 7.Atun R, Bataringaya J. Building a durable response to HIV/AIDS: implications for health systems. J Acquir Immune Defic Syndr. 2011;57(Suppl 2):S91–5. doi: 10.1097/QAI.0b013e3182218441. [DOI] [PubMed] [Google Scholar]
- 8.Katzenstein DA. HIV RNA and Genotype in resource limited settings. Can we do better? Clin Infect Dis. 2014;58:110–112. doi: 10.1093/cid/cit634. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization [Accessed 7 October 2013];The HIV drug resistance report 2012. http://apps.who.int/iris/bitstream/10665/75183/1/9789241503938_eng.pdf
- 10.Gupta R, Jordan M, Sultan B, et al. Global trends in antiretroviral resistance in treatment-naive individuals with HIV after rollout of antiretroviral treatment in resource-limited settings: a global collaborative study and meta-regression analysis. Lancet. 2012;380:1250–8. doi: 10.1016/S0140-6736(12)61038-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manasa J, Katzenstein D, Cassol S, Newell M, de Oliveira T. Primary drug resistance in South Africa: data from 10 years of surveys. AIDS Res Hum Retroviruses. 2012;28:558–65. doi: 10.1089/aid.2011.0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hunt G, Ledwaba J, Basson A, et al. Surveillance of transmitted HIV-1 drug resistance in Gauteng and KwaZulu-Natal Provinces, South Africa, 2005-2009. Clin Infect Dis. 2012;54(Suppl 4):S334–8. doi: 10.1093/cid/cir1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McMahon J, Elliott J, Bertagnolio S, Kubiak R, Jordan M. Viral suppression after 12 months of antiretroviral therapy in low- and middle-income countries: a systematic review. Bull World Health Organ. 2013;91:377–85E. doi: 10.2471/BLT.12.112946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aghokeng A, Monleau M, Eymard-Duvernay S, et al. Extraordinary heterogeneity of virological outcomes in Patients Receiving HAART and Monitored with the World Health Organization (WHO) Public Health Approach in sub-Saharan Africa and south-east Asia. Clin Infect Dis. 2014;58:99–109. doi: 10.1093/cid/cit627. [DOI] [PubMed] [Google Scholar]
- 15.Hamers R, Sigaloff K, Wensing A, et al. Patterns of HIV-1 drug resistance after first-line antiretroviral therapy (ART) failure in 6 sub-Saharan African countries: implications for second-line ART strategies. Clin Infect Dis. 2012;54:1660–9. doi: 10.1093/cid/cis254. [DOI] [PubMed] [Google Scholar]
- 16.Manasa J, Lessells R, Skingsley A, et al. High-levels of acquired drug resistance in adult patients failing first-line antiretroviral therapy in a rural HIV treatment programme in KwaZulu-Natal, South Africa. PLoS One. 2013;8:e72152. doi: 10.1371/journal.pone.0072152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sunpath H, Wu B, Gordon M, et al. High rate of K65R for antiretroviral therapy-naive patients with subtype C HIV infection failing a tenofovircontaining first-line regimen. AIDS. 2012;26:1679–84. doi: 10.1097/QAD.0b013e328356886d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoffmann C, Ledwaba J, Li J, et al. Resistance to tenofovir-based regimens during treatment failure of subtype C HIV-1 in South Africa. Antivir Ther. 2013;18:915–920. doi: 10.3851/IMP2652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coutsinos D, Invernizzi C, Xu H, Brenner B, Wainberg M. Factors affecting template usage in the development of K65R resistance in subtype C variants of HIV type-1. Antivir Chem Chemother. 2010;20:117–31. doi: 10.3851/IMP1443. [DOI] [PubMed] [Google Scholar]
- 20.Sigaloff K, Calis J, Geelen S, van Vugt M, de Wit T. HIV-1-resistance-associated mutations after failure of first-line antiretroviral treatment among children in resource-poor regions: a systematic review. Lancet Infect Dis. 2011;11:769–79. doi: 10.1016/S1473-3099(11)70141-4. [DOI] [PubMed] [Google Scholar]
- 21.van Zyl G, van der Merwe L, Claassen M, et al. Protease inhibitor resistance in South African children with virologic failure. Pediatr Infect Dis J. 2009;28:1125–7. doi: 10.1097/INF.0b013e3181af829d. [DOI] [PubMed] [Google Scholar]
- 22.Asboe D, Aitken C, Boffito M, et al. British HIV Association guidelines for the routine investigation and monitoring of adult HIV-1-infected individuals 2011. HIV Med. 2012;13:1–44. doi: 10.1111/j.1468-1293.2011.00971.x. [DOI] [PubMed] [Google Scholar]
- 23.Vandamme A, Camacho R, Ceccherini-Silberstein F, et al. European recommendations for the clinical use of HIV drug resistance testing: 2011 update. AIDS Rev. 2011;13:77–108. [PubMed] [Google Scholar]
- 24.Panel on Antiretroviral Guidelines for Adults and Adolescents [Accessed 7 October 2013];Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. http://aidsinfo.nih.gov/contentfiles/lvguidelines/AdultandAdolescentGL.pdf
- 25.Dunn D, Coughlin K, Cane P. Genotypic resistance testing in routine clinical care. Curr Opin HIV AIDS. 2011;6:251–7. doi: 10.1097/COH.0b013e32834732e8. [DOI] [PubMed] [Google Scholar]
- 26.Elliott J, Lynen L, Calmy A, et al. Rational use of antiretroviral therapy in low-income and middle-income countries: optimizing regimen sequencing and switching. AIDS. 2008;22:2053–67. doi: 10.1097/QAD.0b013e328309520d. [DOI] [PubMed] [Google Scholar]
- 27.De Luca A, Hamers R, Schapiro J. Antiretroviral treatment sequencing strategies to overcome HIV type 1 drug resistance in adolescents and adults in low-middle-income countries. J Infect Dis. 2013;207(Suppl 2):S63–9. doi: 10.1093/infdis/jit109. [DOI] [PubMed] [Google Scholar]
- 28.Pillay D, Albert J, Bertagnolio S, et al. Implications of HIV drug resistance on first- and second-line therapies in resource-limited settings: report from a workshop organized by the Collaborative HIV and Anti-HIV Drug Resistance Network. Antivir Ther. 2013;18:831–836. doi: 10.3851/IMP2650. [DOI] [PubMed] [Google Scholar]
- 29.Singh B. MSc thesis. London School of Hygiene and Tropical Medicine; 2013. Absence of drug resistance in patients with treatment failure in rural KwaZulu-Natal, South Africa. [Google Scholar]
- 30.Johnston V, Cohen K, Wiesner L, et al. Viral suppression following switch to second-line antiretroviral therapy: associations with nucleoside reverse transcriptase inhibitor resistance and subtherapeutic drug concentrations prior to switch. J Infect Dis. 2014;209:711–720. doi: 10.1093/infdis/jit411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murphy R, Sunpath H, Lu Z, et al. Outcomes after virologic failure of first-line ART in South Africa. AIDS. 2010;24:1007–12. doi: 10.1097/QAD.0b013e3283333639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Levison J, Orrell C, Gallien S, et al. Virologic failure of protease inhibitor-based second-line antiretroviral therapy without resistance in a large HIV treatment program in South Africa. PLoS One. 2012;7:e32144. doi: 10.1371/journal.pone.0032144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sigaloff K, Hamers R, Wallis C, et al. Second-line antiretroviral treatment successfully re-suppresses drug-resistant HIV-1 after first-line failure: prospective cohort in Sub-Saharan Africa. J Infect Dis. 2012;205:1739–44. doi: 10.1093/infdis/jis261. [DOI] [PubMed] [Google Scholar]
- 34.Wallis C, Mellors J, Venter W, Sanne I, Stevens W. Protease inhibitor resistance is uncommon in HIV-1 subtype C infected patients on failing second-line lopinavir/r-containing antiretroviral therapy in South Africa. AIDS Res Treat. 2011;2011:769627. doi: 10.1155/2011/769627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Zyl G, van Mens T, McIlleron H, et al. Low lopinavir plasma or hair concentrations explain second-line protease inhibitor failures in a resource-limited setting. J Acquir Immune Defic Syndr. 2011;56:333–9. doi: 10.1097/QAI.0b013e31820dc0cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harries A, Zachariah R, van Oosterhout J, et al. Diagnosis and management of antiretroviral-therapy failure in resource-limited settings in sub-Saharan Africa: challenges and perspectives. Lancet Infect Dis. 2010;10:60–5. doi: 10.1016/S1473-3099(09)70321-4. [DOI] [PubMed] [Google Scholar]
- 37.Berg K, Arnsten J. Practical and conceptual challenges in measuring antiretroviral adherence. J Acquir Immune Defic Syndr. 2006;43(Suppl 1):S79–87. doi: 10.1097/01.qai.0000248337.97814.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barnighausen T, Chaiyachati K, Chimbindi N, Peoples A, Haberer J, Newell M. Interventions to increase antiretroviral adherence in sub-Saharan Africa: a systematic review of evaluation studies. Lancet Infect Dis. 2011;11:942–51. doi: 10.1016/S1473-3099(11)70181-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baxter J, Mayers D, Wentworth D, et al. CPCRA 046 Study Team for the Terry Beirn Community Programs for Clinical Research on AIDS A randomized study of antiretroviral management based on plasma genotypic antiretroviral resistance testing in patients failing therapy. AIDS. 2000;14:F83–93. doi: 10.1097/00002030-200006160-00001. [DOI] [PubMed] [Google Scholar]
- 40.Durant J, Clevenbergh P, Halfon P, et al. Drug-resistance genotyping in HIV-1 therapy: the VIRADAPT randomised controlled trial. Lancet. 1999;353:2195–9. doi: 10.1016/s0140-6736(98)12291-2. [DOI] [PubMed] [Google Scholar]
- 41.Tural C, Ruiz L, Holtzer C, et al. Clinical utility of HIV-1 genotyping and expert advice: the Havana trial. AIDS. 2002;16:209–18. doi: 10.1097/00002030-200201250-00010. [DOI] [PubMed] [Google Scholar]
- 42.University of Washington [Accessed 1 October 2013];OLA Resistance Study. http://clinicaltrials.gov/ct2/show/NCT01898754
- 43.Levison J, Wood R, Scott C, et al. The clinical and economic impact of genotype testing at first-line antiretroviral therapy failure for HIV-infected patients in South Africa. Clin Infect Dis. 2013;56:587–97. doi: 10.1093/cid/cis887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lorenzana S, Hughes M, Grinsztejn B, et al. Genotype assays and third-line ART in resource-limited settings: a simulation and cost-effectiveness analysis of a planned clinical trial. AIDS. 2012;26:1083–93. doi: 10.1097/QAD.0b013e32835221eb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sohn A, Nuttall J, Zhang F. Sequencing of antiretroviral therapy in children in low- and middle-income countries. Curr Opin HIV AIDS. 2010;5:54–60. doi: 10.1097/COH.0b013e3283339bd8. [DOI] [PubMed] [Google Scholar]
- 46.Calmy A, Ford N, Hirschel B, et al. HIV viral load monitoring in resource-limited regions: optional or necessary? Clin Infect Dis. 2007;44:128–34. doi: 10.1086/510073. [DOI] [PubMed] [Google Scholar]
- 47.Clinton Health Access Initiative [Accessed 7 October 2013];HIV viral load testing. Market analysis. http://mat1.gtimg.com/gongyi/2012/enzhenduandahui/6ZachKatz.pdf
- 48.Stevens W, Marshall T. Challenges in implementing HIV load testing in South Africa. J Infect Dis. 2010;201(Suppl 1):S78–84. doi: 10.1086/650383. [DOI] [PubMed] [Google Scholar]
- 49.Scott L. South Africa’s experiences and future plans for CD4 and viral load implementation; 7th IAS Conference on HIV Pathogenesis, Treatment and Prevention; Kuala Lumpur, Malaysia. 2013. [Google Scholar]
- 50.Stevens W. South Africa’s “Reality Check”: >1 million Xpert tests; 5th Annual Global Laboratory Initiative Partners’ Meeting Veyrie-du-Lac; France. 2013. [Google Scholar]
- 51.Department of Health RoSA [Accessed 7 October 2013];The South African Antiretroviral Treatment Guidelines. 2013 http://www.doh.gov.za/docs/policy/2013/ART_Treatment_Guidelines_Final_25March2013.pdf
- 52.Ministry of Health GoB [Accessed 7 October 2013];Botswana National HIV & AIDS Treatment Guidelines. 2012 http://www.hiv.gov.bw/sites/default/files/documents/Bots%20Nat%20HIV-AIDS%20Treat%20Guide%2009-07-2012_0.pdf
- 53.Kircher M, Kelso J. High-throughput DNA sequencing--concepts and limitations. Bioessays. 2010;32:524–36. doi: 10.1002/bies.200900181. [DOI] [PubMed] [Google Scholar]
- 54.PRNewswire [Accessed 7 October 2013];Life Technologies and SATuRN Collaborate to Increase Access to HIV Testing in Africa. http://www.prnewswire.com/news-releases/life-technologies-and-saturn-collaborate-to-increase-access-to-hiv-testing-in-africa-163526506.html
- 55.Wallis C, Papathanasopoulos M, Lakhi S, et al. Affordable in-house antiretroviral drug resistance assay with good performance in non-subtype B HIV-1. J Virol Methods. 2010;163:505–8. doi: 10.1016/j.jviromet.2009.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aitken S, Kliphuis A, Wallis C, et al. Development and evaluation of an assay for HIV-1 protease and reverse transcriptase drug resistance genotyping of all major group-M subtypes. J Clin Virol. 2012;54:21–5. doi: 10.1016/j.jcv.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 57.Aitken S, Bronze M, Wallis C, et al. A pragmatic approach to HIV-1 drug resistance determination in resource-limited settings by use of a novel genotyping assay targeting the reverse transcriptase-encoding region only. J Clin Microbiol. 2013;51:1757–61. doi: 10.1128/JCM.00118-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Manasa J, Danaviah S, Pillay S, et al. Affordable HIV-1 Drug resistance monitoring system for resource limited settings. J Vis Exp. 2013 doi: 10.3791/51242. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.de Oliveira T, Shafer R, Seebregts C. Public database for HIV drug resistance in southern Africa. Nature. 2010;464:673. doi: 10.1038/464673c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Paredes R. Importance of minor variants and their detection (ultra-deep sequencing) in the management of HIV infection. J Int AIDS Soc. 2012;15:18309. [Google Scholar]
- 61.Bertagnolio S, Parkin N, Jordan M, Brooks J, Garcia-Lerma J. Dried blood spots for HIV-1 drug resistance and viral load testing: A review of current knowledge and WHO efforts for global HIV drug resistance surveillance. AIDS Rev. 2010;12:195–208. [PubMed] [Google Scholar]
- 62.Buckton A. New methods for the surveillance of HIV drug resistance in the resource poor world. Curr Opin Infect Dis. 2008;21:653–8. doi: 10.1097/QCO.0b013e3283186d1a. [DOI] [PubMed] [Google Scholar]
- 63.Parkin N, de Mendoza C, Schuurman R, et al. Evaluation of in-house genotyping assay performance using dried blood spot specimens in the Global World Health Organization laboratory network. Clin Infect Dis. 2012;54(Suppl 4):S273–9. doi: 10.1093/cid/cir982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hamers R, Straatsma E, Kityo C, et al. Building capacity for the assessment of HIV drug resistance: experiences from the PharmAccess African Studies to Evaluate Resistance network. Clin Infect Dis. 2012;54(Suppl 4):S261–5. doi: 10.1093/cid/cir995. [DOI] [PubMed] [Google Scholar]
- 65.Land S, Zhou J, Cunningham P, et al. Capacity building and predictors of success for HIV-1 drug resistance testing in the Asia-Pacific region and Africa. J Int AIDS Soc. 2013;16:18580. doi: 10.7448/IAS.16.1.18580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Department of Health RoSA . Multi-drug resistant tuberculosis. A policy framework on decentralised and deinstitutionalised management for South Africa. Department of Health; Pretoria, South Africa: 2011. [Google Scholar]
- 67.Libin P, Beheydt G, Deforche K, et al. RegaDB: community-driven data management and analysis for infectious diseases. Bioinformatics. 2013;29:1477–80. doi: 10.1093/bioinformatics/btt162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Roberts T, Bygrave H, Fajardo E, Ford N. Challenges and opportunities for the implementation of virological testing in resource-limited settings. J Int AIDS Soc. 2012;15:17324. doi: 10.7448/IAS.15.2.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pai N, Pai M. Point-of-care diagnostics for HIV and tuberculosis: landscape, pipeline, and unmet needs. Discov Med. 2012;13:35–45. [PubMed] [Google Scholar]
- 70.Wang S, Xu F, Demirci U. Advances in developing HIV-1 viral load assays for resource-limited settings. Biotechnol Adv. 2010;28:770–81. doi: 10.1016/j.biotechadv.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tang M, Liu T, Shafer R. The HIVdb system for HIV-1 genotypic resistance interpretation. Intervirology. 2012;55:98–101. doi: 10.1159/000331998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Van Laethem K, De Luca A, Antinori A, Cingolani A, Perna C, Vandamme A. A genotypic drug resistance interpretation algorithm that significantly predicts therapy response in HIV-1-infected patients. Antivir Ther. 2002;7:123–9. [PubMed] [Google Scholar]
- 73.Meynard J, Vray M, Morand-Joubert L, et al. Phenotypic or genotypic resistance testing for choosing antiretroviral therapy after treatment failure: a randomized trial. AIDS. 2002;16:727–36. doi: 10.1097/00002030-200203290-00008. [DOI] [PubMed] [Google Scholar]
- 74.Snoeck J, Kantor R, Shafer R, et al. Discordances between interpretation algorithms for genotypic resistance to protease and reverse transcriptase inhibitors of human immunodeficiency virus are subtype dependent. Antimicrob Agents Chemother. 2006;50:694–701. doi: 10.1128/AAC.50.2.694-701.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Frentz D, Boucher C, Assel M, et al. Comparison of HIV-1 genotypic resistance test interpretation systems in predicting virological outcomes over time. PLoS One. 2010;5:e11505. doi: 10.1371/journal.pone.0011505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ahonkhai A, Bassett I, Ferris T, Freedberg K. Improving HIV outcomes in resource-limited countries: the importance of quality indicators. BMC Health Serv Res. 2012;12:427. doi: 10.1186/1472-6963-12-427. [DOI] [PMC free article] [PubMed] [Google Scholar]