Abstract
The purpose of this cross-sectional survey study was to examine the influence of self-efficacy, outcome expectations and environment on neighborhood walking in older adults with (n=163, mean age=78.7, SD=7.96 years) and without (n=163, mean age=73.6, SD=7.93 years) mobility limitations (controlling for demographic characteristics). Measures included: Neighborhood Physical Activity Questionnaire, Multidimensional Outcome Expectations for Exercise Scale, Neighborhood Environment Walkability Scale, and self-efficacy scales. Multiple regression revealed that in mobility-limited older adults, demographic characteristics, self-efficacy, and outcome expectations explained 17.4% of variance in neighborhood walking, while environment (neighborhood destinations and design) explained 9.5%. Destinations, self-efficacy, gender, and outcome expectations influenced walking. In those without mobility limitations, demographic characteristics, self-efficacy, and outcome expectations explained 15.6% of the variance, while environment explained 5.7%. Self-efficacy, gender, and design influenced walking. Neighborhood walking interventions for older adults should include self-efficacy strategies tailored to mobility status and neighborhood characteristics.
Regular physical activity is important for the prevention or delay of mobility-related disability (Alexander & Goldberg, 2005; Rejeski et al., 2009). The most common type of moderate physical activity chosen by older adults of all ethnic backgrounds is walking (Bassett, Fitzhugh, Crespo, King & McLaughlin, 2002; Belza et al., 2004), yet only 25% of older adults walk on a regular basis (LeMasurier et al., 2008). The onset of mobility limitations (Hughes, McDowell & Brody, 2008) and advancing age (Hughes et al., 2008; Shaw & Spokane, 2008) are associated with decreased walking. Regular walking may help to prevent or delay the progression of mobility limitations (Faber, Bosscher, Chin & van Wieringen, 2006; Luukinen et al., 2007) and does not have to be of long duration or distance in order to provide mobility benefits (Simonsick, Guralnik, Volpato, Balfour & Fried, 2005). Because neighborhood walking is convenient (King, 2001) and attractive to older adults, including those with chronic illness (Fuller, Stewart Williams & Byles, 2010), identification of factors that promote neighborhood walking is critical.
Neighborhood walking in older adults may be influenced by both individual and neighborhood environment factors, and the neighborhood environment may be particularly relevant for individuals with mobility limitations (Clarke, Ailshire, Bader, Morenoff & House, 2008; Shumway-Cook et al., 2003). However, no studies were identified that examined the impact of both individual and neighborhood environment factors in older adults with and without mobility limitations. Understanding how multiple factors influence neighborhood walking is important for increasing physical activity in older adults and for preventing the progression of mobility limitations. This study examined the influence of neighborhood environment and individual factors (self-efficacy and outcome expectations) on neighborhood walking in older adults with and without mobility limitations.
Background and Significance
Characteristics of the neighborhood environment that may encourage walking in older adults can be categorized within the “3Ds” framework (Cervero & Knockelman, 1996). Initially developed to examine transportation choices within the context of the built environment, the “3Ds” framework includes density of residences, presence of destinations such as neighborhood retail and services, and design characteristics such as neighborhood aesthetics (Saelens, Sallis & Frank, 2003). Older adults are more likely to walk in neighborhoods with higher residential density (Li, Fisher, Brownson & Bosworth, 2004; Rodriguez, Evenson, Diez Roux & Brines, 2009), destinations such as stores, libraries, coffee shops (Michael, Beard, Choi, Farquhar & Carlson, 2006; Michael, Green & Farquhar, 2005; Wang & Lee, 2009) within walking distance of their residences, and design features such as pleasant surroundings, maintained sidewalks, and safety from crime (Li et al., 2004; Roman & Chalfin, 2008; Wilcox, Bopp, Oberrecht, Kammerman & McElmurray, 2003) and traffic (Gomez et al., 2010; Michael et al., 2005; Patterson & Chapman, 2003; Shumway-Cook et al., 2003; Strath, Isaacs & Greenwald, 2007).
The impact of the neighborhood environment on walking may be heightened by vision, hearing and musculoskeletal deficits which limit the ability of some older adults to negotiate their environment (Frank, Engelke & Schmid, 2003). Mobility-limited older adults report more difficulty walking in neighborhoods with sidewalks in poor repair than older adults without mobility limitations (Clarke et al., 2008) and avoid obstacles such as curbs, and walking on uneven or icy surfaces (Shumway-Cook et al., 2003). In contrast, neighborhood environment has been associated with walking in older adults with normal lower-body function, but not in older adults with poor lower-body function (Satariano et al., 2010). Since the relationship between neighborhood factors and walking appears to be complex (Satariano et al., 2010) and avoidance of walking due to neighborhood characteristics may limit physical activity and hasten mobility decline (Balfour & Kaplan, 2002; Clarke & George, 2005), further examination of these relationships is warranted.
Individual factors also may impact neighborhood walking. Self-efficacy, an individual’s belief in his or her capability to perform a specific behavior (Bandura, 1997), has been positively associated with walking (Lord, Weatherall & Rochester, 2010; Morris, McAuley, & Motl, 2008; Rejeski, Ip, Marsh, Miller & Farmer, 2008) and negatively associated with mobility limitations in older adults (Bean, Bailey, Kiely & Leveille, 2007; Motl & McAuley, 2010). Yet it is unclear how self-efficacy influences neighborhood walking in mobility-limited older adults, or if distinct types of self-efficacy vary based on mobility status. Mobility limitations may be present due to slowed gait, dizziness, or lower extremity pain, stiffness, numbness, or weakness (Alexander & Goldberg, 2005); therefore, self-efficacy related to gait, walking duration, overcoming barriers, and balance may be particularly important for older adults with mobility limitations.
Outcome expectations are the belief that specific consequences are likely to occur in response to a particular behavior (Bandura, 1997). In some studies, outcome expectations have been associated with physical activity (Conn, 1998; Resnick, 2001) and walking (McAuley et al., 2009), while others have found no association (Anderson, Wojcik, Winett & Williams, 2006; Perkins, Multhaup, Perkins & Barton, 2008). Perceptions of negative outcomes of performing physical activity such as falling (Clark & Nothwehr, 1999), pain, or worsening of a chronic condition (Gretebeck et al., 2007) may influence physical activity in older adults (Resnick et al., 2006). Mobility-limited older adults perceive fewer positive outcomes of regular physical activity than those without mobility limitations (Resnick, Palmer, Jenkins & Spellbring, 2000), but little is known about the influence of outcome expectations on neighborhood walking in older adults with mobility limitations, or if outcome expectations differ by mobility status.
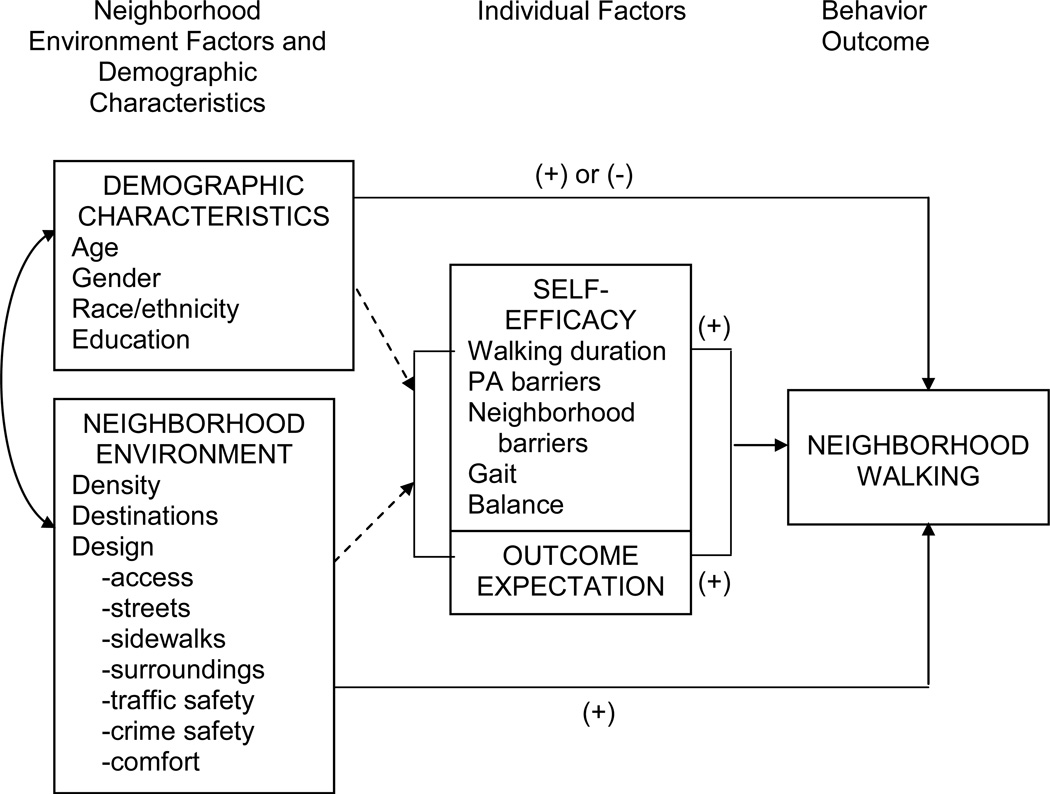
In order to plan effective strategies to increase physical activity (e.g. walking) and prevent or slow the progression of mobility limitations, it is important to understand the factors that impact neighborhood walking in older adults with and without mobility limitations. Guided by Social Cognitive Theory (Bandura, 1997), the purpose of this study was to examine both the neighborhood environment and individual factors (self-efficacy and outcome expectations) that influence neighborhood walking duration in older adults with and without mobility limitations. In Social Cognitive Theory (Figure 1), behavior is described as dynamic and dependent on a continuing interaction among aspects of both the individual (including self-efficacy and outcome expectations) and the environment (Bandura, 1997). In this study, the behavior neighborhood walking was hypothesized to be influenced by individual factors (outcome expectations and five types of self-efficacy relevant to neighborhood walking), and the neighborhood environment, while controlling for demographic factors (age, gender, race/ethnicity and education). The neighborhood environment variable was operationalized using the “3 Ds” concept, including density, destinations, and design (Cervero & Knockelman, 1996). In this model, design was comprised of seven categories of neighborhood characteristics: neighborhood access, streets, sidewalks, surroundings, traffic, crime (Saelens, Sallis, Black & Chen, 2003) and comfort (Gallagher et al., 2010). Although relationships may exist between the individual factors (self-efficacy, outcome expectations and mobility limitations), demographic factors, and the environment (Balfour & Kaplan, 2002; Bandura, 1997; Resnick et al., 2000; Satariano et al., 2010), these relationships were not tested in this study, and are represented in the model by dashed arrows.
Figure 1.
Theoretical model PA = physical activity
Method
Setting and Sample
Four hundred participants were recruited for this cross-sectional study from a database of older adults who agreed to be contacted for research participation. Inclusion criteria included being 60 years of age or older; living independently (e.g. not in a skilled nursing care facility), ability to walk with or without an assistive device, and residence in an urban or urbanized area as defined by the U.S. Census Bureau (2000).
After approval by the University Institutional Review Board, a cover letter describing the study, informed-consent form, return envelope, and survey were mailed to potential participants. Non-respondents received reminder postcards two weeks after the initial mailing and telephone contacts two weeks later (Dillman, 2000). Of the 400 surveys mailed, 340 were returned, of which 14 were excluded due to participant ineligibility or undeliverable or unusable surveys, resulting in a final sample size of 326 participants (81.5% response rate).
The average time to complete the questionnaire was anticipated to be 60–90 minutes. To limit burden and fatigue, participants were encouraged to complete the questionnaire in multiple sittings, if necessary, rather than in one sitting. Additional strategies to limit participant burden included using a large 14 font and adequate spacing between survey items.
Measures
Neighborhood walking was defined as weekly duration of walking within ½ mile of the participant’s residence. Two items from the Neighborhood Physical Activity Questionnaire (NPAQ) were used to measure neighborhood walking duration (Giles-Corti et al., 2006). Participants were asked to estimate the time they spent walking (in hours and minutes) in their neighborhoods each week for transportation, recreation, health or fitness. The responses were summed for the total duration of neighborhood walking. Reliability has been established for the 21- item NPAQ but not for physical activity subcomponents such as neighborhood walking duration.
Neighborhood environment (the area within a 15-minute walk or ½ mile of the participants’ home) was measured using the Neighborhood Environment Walkability Scale (NEWS) developed by Saelens, Sallis, Black and Chen (2003). Eight subscales of the NEWS were used to measure the density, destinations and design components of the “3Ds” framework (Cervero & Knockelman, 1996). Neighborhood density (concentration of buildings with multiple residences such as apartment buildings) was measured with the 6-item residential density subscale. Participants identified the frequency (none = 1 to all = 5) of specific types of residences (ranging from single-family homes to apartment buildings more than 13 stories tall) in their neighborhood. Item responses were weighted and summed to calculate the subscale score with higher scores indicating higher residential density (Saelens, Sallis, Black et al., 2003). Neighborhood destinations (neighborhood retail and services) were measured with the 23-item land-use mix-diversity subscale. Participants reported the length of time (from 1 to 30 minutes in 5-minute increments) to walk from their home to 23 different stores and services (schools, grocery stores, banks, etc.). A mean score was calculated with higher scores representing more stores and services within a shorter walking distance from the participant’s home (Saelens, Sallis, Black et al., 2003). Neighborhood design was measured with the remaining six NEWS subscales: land-use mix-access (access to services), street connectivity, walking facilities (sidewalks), aesthetics (neighborhood surroundings), pedestrian/traffic safety, and crime safety. A Comfort subscale (including places to rest and use the bathroom) was added based on a preliminary study (Gallagher et al., 2010). Responses for each of the subscales ranged from 1 = strong disagreement to 4 = strong agreement that the characteristic was present in their neighborhood. Mean scores were calculated for each of the subscales as well as a summary mean for neighborhood design; higher scores reflected design characteristics more conducive to walking. Cronbach’s alpha for the modified neighborhood design scale was .85.
Self-efficacy was measured with five self-efficacy scales specifically related to characteristics (e.g., gait, balance, overcoming barriers) that may impact perceived confidence of older adults participating in physical activity and walking. For each self-efficacy scale item, participants rated their level of confidence (in 10% increments) on an 11-point scale (0% = not at all confident to 100% = highly confident). The 8-item Self-efficacy for Walking Scale, (McAuley, Blissmer, Katula & Duncan, 2000) assessed participant confidence in walking for increasing durations of time in 5-minute increments from 0 to 40 minutes. The Self-efficacy for Physical Activity Barriers Scale (McAuley, 1992) measured confidence in performing moderate physical activity for 30 minutes five days a week in the face of 16 barriers such as low energy, pain, boredom or care-giving responsibilities. Confidence in the ability to navigate curbs, stairs, uneven surfaces and other obstacles was evaluated with the 9-item Gait Efficacy Scale (McAuley, Mihalko & Rosengren, 1997). The Activities-specific Balance Confidence Scale (Powell & Myers, 1995) measured confidence in maintaining balance under 16 circumstances such as sweeping the floor or walking on an icy sidewalk. The Self-efficacy for Neighborhood Barriers Scale, developed for this study, assessed confidence in walking for 10 or more minutes in the face of eight neighborhood barriers identified in preliminary focus groups: unattractive surroundings; lack of places to walk to, rest, or use the bathroom; poor lighting; poorly maintained sidewalks; heavy traffic; and crime or loose dogs (Gallagher et al., 2010). A mean of the five scale scores was calculated for a total self-efficacy score. The Cronbach’s alpha for the total scale in this study was .98.
The 19-item Multidimensional Outcome Expectations for Exercise Scale (Wojcicki, White & McAuley, 2009) was used to measure outcome expectations. Participants rated on a 5-point scale (1 = strongly disagree to 5 = strongly agree) how strongly they agreed that 30 minutes of moderate intensity physical activity five days per week would lead to specific positive consequences (e.g. strengthening bones or muscles or improving mood). Because negative outcomes also may influence physical activity in older adults (Resnick et al., 2006), four negative outcomes were added to the scale: fear of falling or injury (Resnick et al., 2006), pain (Gretebeck et al., 2007), worsening of a chronic condition (Gretebeck et al., 2007; Resnick et al., 2006) and heart attack, chest pain or shortness of breath (Clark & Norwehr, 1999). Negative items were reverse coded and a mean score that included the positive and negative outcomes was calculated. A higher mean score indicated stronger agreement that physical activity for 30 minutes five days per week would lead to positive outcomes. The Cronbach’s alpha for the modified outcome expectations scale was .92.
Demographic variables included age, gender (male or female), education (high school, trade/technical/business school or some college, bachelor’s degree, some graduate work, master’s degree, advanced degree) and race. Due to the limited number of nonwhite participants, the race variable was collapsed into white and nonwhite.
A cut-point on the Pepper Assessment Tool for Disability (PAT-D) was used to classify mobility status (Rejeski, Ettinger, Schumaker, Burns & Elam, 1995). Participants rated their level of difficulty (1 = no difficulty, 2 = a little difficulty, 3 = some difficulty, 4 = a lot of difficulty, and 5 = unable to do) in performing eight mobility-related tasks in the last month, walking one block, walking several blocks, climbing one flight of stairs, climbing several flights of stairs, lifting or carrying a heavy object, lifting or carrying 10 pounds, and getting in and out of a car (Rejeski et al., 1995). Two items were added, difficulty walking ½ mile and difficulty running errands, due to their potential relevance to neighborhood walking. A mean score was calculated for the modified PAT-D; higher scores indicated more difficulty with a task. The Cronbach’s alpha for the scale in this study was .88. To determine mobility status, participants with a mean PAT-D score below 1.33 (no difficulty with 2/3 or more of the tasks and minimal difficulty with the remainder) were classified as not mobility-limited (n=163), while those with a score of 1.33 or more (at least some difficulty with more than 1/3 of the tasks) were classified as mobility-limited (n=163).
Data Analysis
All statistical tests were conducted using SPSS (Version 19.0, SPSS Inc., Chicago, IL). Following bivariate correlation analyses, t-tests and chi-square tests were conducted to examine differences in the study variables. Multiple linear regression analyses were conducted to examine the influence of 1) demographic characteristics (age, race, gender and education), 2) individual factors (self-efficacy and outcome expectations), and 3) neighborhood environment (neighborhood destinations and design) on neighborhood walking duration in older adults with and without mobility limitations.
With the exception of 6.3% missing responses for the Self-efficacy for Physical Activity Barriers Scale, no scales had more than 5% missing data. Due to the nonrandom nature of the missing responses and the importance of retaining participants with a range of responses on these variables, missing responses were imputed with the mean of each participant’s nonmissing responses for that scale.
Results
Sample characteristics are summarized in Table 1. The majority of the sample was white, female, married, and retired, and most had earned a bachelor’s degree or higher. Mobility-limited participants were significantly older than participants with no mobility limitations, and were more likely to be female, widowed or divorced, work less than full-time, have fallen in the last year and use an assistive device.
Table 1.
Sample Characteristics and Mean Comparisons by Mobility Status
| Characteristic | Total Sample Frequency (%) n = 326 |
No mobility limitations Frequency (%) n = 163 |
Mobility limitations Frequency (%) n = 163 |
p value |
|---|---|---|---|---|
| Age in years: M (SD) (n = 321) | 76.1 (8.34) | 73.6 (7.93) | 78.7 (7.96) | < . 001a |
| 60–69 years | 78 (24.3) | 52 (32.1) | 26 (16.4) | |
| 70–79 years | 117 (36.4) | 71 (43.8) | 46 (28.9) | |
| 80–89 years | 111 (34.6) | 36 (22.2) | 75 (47.2) | |
| 90–99 years | 15 (4.7) | 3 (1.9) | 12 (7.5) | |
| Gender (n = 322) | .03b | |||
| Male | 106 (32.9) | 63 (38.9) | 43 (26.9) | |
| Female | 216 (67.1) | 99 (61.1) | 117 (73.1) | |
| Marital status (n = 323) | .001b | |||
| Single | 17 (5.3) | 5 (3.1) | 12 (7.5) | |
| Married | 192 (59.4) | 114 (69.9) | 78 (48.8) | |
| Widowed | 73 (22.6) | 25 (15.3) | 48 (30.0) | |
| Divorced/Separated/Other | 41 (12.7) | 19 (11.7) | 22 (13.8) | |
| Ethnicity (n = 320) | ns b,c | |||
| White | 302 (94.4) | 150 (93.2) | 152 (95.6) | |
| Black | 9 (2.8) | 4 (2.5) | 5 (3.1) | |
| Asian American | 5 (1.6) | 4 (2.5) | 1 (0.6) | |
| Other | 4 (1.3) | 3 (1.9) | 1 (0.6) | |
| Highest level education (n = 322) | nsb | |||
| HS graduate | 31 (9.6) | 12 (7.4) | 19 (11.9) | |
| Trade/college | 77 (23.9) | 32 (19.8) | 45 (28.1) | |
| Bachelor’s degree | 52 (16.1) | 31 (19.1) | 21 (13.1) | |
| Some graduate work | 26 (8.1) | 15 (9.3) | 11 (6.9) | |
| Master’s degree | 92 (28.6) | 49 (30.2) | 43 (26.9) | |
| Advanced degree | 44 (13.7) | 23 (14.2) | 21 (13.1) | |
| Living arrangement (n = 322) | nsb | |||
| House/apartment | 304 (94.4) | 156 (96.3) | 148 (92.5) | |
| Senior housing | 17 (5.3) | 6 (3.7) | 11 (6.9) | |
| Relative’s home | 1 (0.3) | 0 (0) | 1 (0.6) | |
| Employment status (n = 322) | .001b | |||
| Work full-time | 29 (9.0) | 24 (14.7) | 5 (3.1) | |
| Work part-time | 39 (12.1) | 19 (11.7) | 20 (12.6) | |
| Homemaker | 13 (4.0) | 5 (3.1) | 8 (5.0) | |
| Retired | 207 (64.3) | 98 (60.1) | 109 (68.6) | |
| Volunteer | 34 (10.6) | 17 (10.4) | 17 (10.7) | |
| Use of assistive device outside the home |
57 (17.5) | 9 (5.5) | 48 (29.4) | .001b |
| History of a fall within the last year | 108 (33.1) | 42 (25.8) | 66 (40.5) | .005b |
t-test,
χ,2
category collapsed into white and nonwhite.
Pearson correlation coefficients among the variables are displayed in Table 2. With the exception of density, all of the theoretical variables were significantly correlated with neighborhood walking (r = .213 - .432, p < .05 or lower). Mobility limitations were negatively correlated with neighborhood walking (r = -.338, p < .01). Pearson correlation and simple linear regression analyses indicated that density was not significantly associated with neighborhood walking or any other variables except design (r = .135, p < .05); therefore, density was removed from further analyses.
Table 2.
Pearson Correlation Matrix for Theoretical Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Self-efficacy | --- | ||||||
| 2. Outcome expectations | .422* | --- | |||||
| 3. Mobility Limitations | -.780** | -.420* | --- | ||||
| 4. Neighborhood Density | -.057 | .015 | .030 | --- | |||
| 5. Neighborhood Destinations | .214** | .074 | -.205* | .108 | --- | ||
| 6. Neighborhood Design | .140* | .105 | -.269* | .135* | .507* | --- | |
| 7. Neighborhood walking | .432** | .213** | -.338* | .106 | .304* | .245* | --- |
p < .05.
p < .01.
Descriptive statistics and group comparisons of the variables for participants with and without mobility limitations (Table 3) revealed that mobility-limited participants walked for shorter durations in their neighborhoods (M = 49.63, SD = 80.16), ranging from 0 to 450 minutes/week. For those without mobility limitations, total neighborhood walking duration ranged from 0 to 540 minutes/week (M = 128.83, SD = 129.74).
Table 3.
Descriptive Statistics of Theoretical Variables and Comparison between Groups Theoretical Variables
| Variable | Mobility limitations n = 163 |
No mobility limitations n = 163 |
t-value |
|---|---|---|---|
| M (SD) | M (SD) | ||
| Neighborhood walking (minutes/week) |
49.63 (80.16) |
128.83 (129.74) |
−6.63*** |
| SE totalª | 52.92 (21.04) |
77.27 (13.56) |
−12.42*** |
| SE walking durationb | 36.95 (33.75) |
77.84 (27.26) |
−12.01*** |
| SE physical activity barriersb |
29.32 (21.72) |
51.40 (25.51) |
−8.78*** |
| SE neighborhood barriersb |
50.69 (28.24) |
68.01 (25.04) |
−5.84*** |
| SE gaitb | 71.84 (26.85) |
95.33 (7.46) |
−10.76*** |
| SE balanceb | 75.49 (41.49) |
92.87 (10.32) |
−9.29*** |
| Outcome expectations | 3.73 (.60) | 4.06 (.50) | −5.35*** |
| Neighborhood environment |
|||
| Destinations | 1.80 (.62) | 2.11 (.64) | −4.39*** |
| Designc | 2.64 (.47) | 2.81 (.43) | −3.49** |
| Access to servicesd | 2.02 (.88) | 2.39 (.98) | −3.74*** |
| Neighborhood streetsd |
2.59 (.86) | 2.64 (.82) | ns |
| Neighborhood sidewalksd |
2.72 (1.08) | 3.0 (1.0) | −2.31* |
| Neighborhood surroundingsd |
3.37 (.55) | 3.46 (.50) | ns |
| Crime safetyd | 3.32 (.48) | 3.47 (.37) | −3.14** |
| Pedestrian/Traffic safetyd |
2.73 (.66) | 3.02 (.60) | −4.15*** |
| Comfortd | 1.64 (.70) | 1.67 (.68) | ns |
Note. SE = Self-efficacy
total SE scale;
SE subscale;
total Design scale;
Design subscale
p < .05.
p < .01.
p < .001.
The mean total self-efficacy score for participants with mobility limitations was 52.92% and 77.27% for those without mobility limitations. In particular, mobility-limited participants reported significantly lower confidence than participants without mobility limitations in their ability to walk for increasing durations of time, perform physical activity for 30 minutes a day five times a week despite barriers, walk for ten minutes or more in their neighborhoods despite neighborhood barriers, navigate curbs and other obstacles (gait self-efficacy) or maintain balance under a variety of conditions. Mobility limited older adults had remarkably low confidence in overcoming barriers to perform physical activity (M=29.32, SD = 21.72) and walking for increasing durations of time (M= 36.95, SD = 33.75), and moderate confidence in neighborhood walking given common barriers (M=50.69, SD = 28.24).
Mobility-limited participants were significantly less likely to agree that regular physical activity for 30 minutes five times a week would lead to positive outcomes than participants without mobility limitations. Mobility-limited participants also were more likely to perceive negative outcomes from physical activity, including falling, pain, chest pain and worsening of a chronic condition, than those without mobility limitations.
Although all participants reported pleasant neighborhood surroundings and safety from crime in their neighborhoods, mobility-limited participants perceived their neighborhoods to have significantly fewer destinations within walking distance, less access to services, poorer sidewalk conditions, and less safety from crime and traffic than participants without mobility limitations.
Multiple Linear Regression
In mobility-limited participants, demographic characteristics (Step 1) explained 5.2% of the variance in neighborhood walking (Table 4). The addition of self-efficacy and outcome expectations (Step 2) increased the explained variance by 12.2% (R2 = .174, p < .01), with self-efficacy and gender significantly associated with neighborhood walking. The addition of neighborhood destinations and design (Step 3) increased the explained variance in neighborhood walking by 9.4% to (R2 = .268, p < .01), with neighborhood destinations exerting the most influence (β=.32, p < .001), followed by self-efficacy (β = .29, p < .01), gender (β = .21, p < .01), and outcome expectations (β = .16, p < .05). Neighborhood design did not independently contribute to the variance in neighborhood walking.
Table 4.
Multiple Linear Regression Results for Predicting Neighborhood Walking in Older Adults with and without Mobility Limitations
| Older adults with mobility limitations (n = 163) |
Older adults without mobility limitations (n = 163) |
|||||||
|---|---|---|---|---|---|---|---|---|
| R2 | β1 | β2 | β3 | R2 | β1 | β2 | β3 | |
| Demographic Characteristics | .052 | .100 | ||||||
| Age | -.153 | .029 | .058 | -.038 | .029 | .028 | ||
| Gender | .112 | .168* | .211** | .054 | .189* | .179* | ||
| Race | .092 | .137 | .107 | -.020 | .051 | .052 | ||
| Education | .015 | -.012 | -.026 | -.053 | -.064 | -.092 | ||
| Individual Variables | .174** | .156** | ||||||
| Outcome Expectations | .126 | .156* | -.029 | -.047 | ||||
| Self-Efficacy | .329*** | .298** | .420*** | .403*** | ||||
| Neighborhood Environment | .268** | .212** | ||||||
| Neighborhood Destinations | .318*** | .096 | ||||||
| Neighborhood Design | -.004 | .174** | ||||||
Note. β1= standardized coefficient, first step, β2= standardized coefficient, second step, β3= standardized coefficient, third step
p < .05.
p <.01.
p < .001 (two-tailed test)
In participants without mobility limitations, demographic characteristics (Step 1) explained 10.0% of the variance in neighborhood walking (Table 4). The addition of self-efficacy and outcome expectations (Step 2) increased the explained variance by 5.6% (R2 = .156, p < .01): with self-efficacy and gender significantly associated with neighborhood walking. The addition of neighborhood destinations and design (Step 3) increased the explained variance by 5.6% (R2 = .212, p < .01) with self-efficacy exerting the most influence (β = .40, p < .05), followed by gender and neighborhood design (β = .18, β = .17, p < .05 respectively). Outcome expectations and neighborhood destinations did not independently contribute to the variance in neighborhood walking.
Discussion
The purpose of this study was to examine the influence of individual factors and neighborhood environment on neighborhood walking in older adults with and without mobility limitations. Mobility-limited older adults walked fewer minutes per week, perceived fewer neighborhood destinations to walk to and fewer neighborhood features that promoted walking, and had lower self-efficacy and outcome expectations than older adults without mobility limitations.
Neighborhood environment influenced neighborhood walking duration in both groups, but the strength of the association and salient neighborhood characteristics differed by mobility status. Neighborhood destinations were significantly associated with neighborhood walking duration for mobility-limited participants, while design was influential for those without mobility limitations. These differences may be related to the reasons for walking in these groups. Neighborhood destinations may be more important for walking for transport than walking for exercise in older adults (Pikora et al., 2006; Shigematsu et al., 2009), while attractive neighborhood surroundings may be more important for walking for exercise (Strath et al., 2007). Although mobility-limited older adults are less likely to walk for exercise than older adults without mobility limitations (McAuley et al., 2009; Rasinaho, Hirvensalo, Leinonen, Lintunen & Rantanen, 2006), mobility-limited older adults may continue to walk for transport to nearby destinations, particularly if they do not drive. Interventions that incorporate walking to neighborhood destinations may increase walking in this group and help to prevent further declines in mobility.
Total self-efficacy and each of the five types of self-efficacy were significantly lower for participants with mobility limitations than for those without. Mobility-limited participants had very low confidence in their ability to walk for increasing durations of time and overcome common barriers, as well as moderate gait and balance self-efficacy. In addition, the mobility-limited participants walked significantly less time (< 1 hour/week) than older adults without limitations (> 2 hours/week). These findings are consistent with other studies of the general population of older adults. Higher physical activity levels have been associated with confidence in overcoming barriers (Morris, McAuley & Motl, 2008; Wilbur, Vassalo, Chandler, McDevitt & Miller, 2005), maintaining balance (McAuley et al., 2006; Myers, Fletcher, Myers & Sherk) and walking for increasing durations of time (McAuley, 2007; McAuley et al., 1999), and self-efficacy related to gait has been associated with higher gait speeds in older adults (McAuley & Konopack, 2006; Rosengren, McAuley & Mihalko, 1998; VanSwearingen et al., 2009). Thus, activities that improve functional ability (Gretebeck et al., 2007), coordination (Protas & Tissier, 2009; VanSwearingen et al., 2009), endurance and lower-extremity strength (Protas & Tissier, 2009), and skills for overcoming barriers (Chen, 2010; Resnick, 2002; van Stralen, de Vries, Mudde, Bolman & Lechner, 2011) may be particularly important for increasing self-efficacy and walking duration in mobility-limited older adults.
Interestingly, neighborhood destinations and self-efficacy similarly influenced neighborhood walking in mobility-limited participants. This is in contrast to previous studies of the general older adult population which found that self-efficacy had a stronger influence on walking than neighborhood environment (Hall & McAuley, 2010; Michael & Carlson, 2009; Nagel, Carlson, Bosworth & Michael, 2008). This novel finding requires further examination, particularly for older adults with mobility limitations. Neighborhood destinations (e.g., stores and restaurants) located within walking distance of the home may promote walking in mobility-limited older adults, thereby potentially increasing self-efficacy through performance of the behavior (Bandura, 1997). But, it is unclear how the location and kind of neighborhood destinations as well as type of self-efficacy affect neighborhood walking for older adults with mobility limitations. Given the very low level of walking for mobility-limited older adults in this study, it is crucial to consider factors at both the environmental and individual levels when designing physical activity (such as walking) interventions.
Additionally, mobility-limited participants, while more likely to have experienced a fall, remained moderately confident in their ability to maintain balance or navigate walkways under challenging conditions. This confidence may increase their risk of injury by exposure to situations that increase fall risk (Bandura, 1997; Shumway-Cook et al., 2003). Interventions that include identification of high-risk situations and strategies to avoid injury may be particularly important for this group.
The influence of outcome expectations on physical activity in older adults has been mixed (Conn, 1998; Perkins et al., 2008; Resnick, 2001), and in this study outcome expectations influenced neighborhood walking only in mobility-limited older adults. Mobility-limited participants had lower expectations of positive outcomes and higher expectations of negative outcomes for performing regular physical activity. Older adults with mobility limitations may believe that they are unable to achieve a level of walking adequate to result in positive outcomes or may not initiate walking due to fear of negative outcomes such as pain (Gretebeck et al., 2007) or falling (Murphy, Williams & Gill (2002). Interventions for mobility-limited older adults should emphasize the positive outcomes possible with even modest increases in walking (Simonsick et al., 2005) while assisting them in preventing or overcoming negative outcomes such as injury, or unpleasant symptoms such as pain or fatigue (Resnick, 2001).
Limitations
Limitations should be considered when interpreting the results of this study. The cross-sectional design did not allow determination of causality. The sample included predominantly well-educated white participants from the Midwest, limiting generalizability of the findings. Subjective measures were used for neighborhood characteristics and walking; future studies should include objective measures of each. Since some may consider physical activity a socially desirable behavior, walking may have been over-reported, although this is unlikely since a wide range of neighborhood walking durations were reported. This study was conducted in the upper Midwest in late spring, and the results may reflect seasonal variations in neighborhood walking. Future studies should be of longer duration to capture seasonal differences. In addition, although neighborhood walking is a convenient and important form of moderate physical activity for older adults, future studies should examine other forms of physical activity (i.e. swimming, indoor walking, etc.) that are safe, appropriate and enjoyable for older adults with varying levels of mobility limitations. The length of the survey may have led to participant fatigue; however, the instructions recommended that the participant complete the survey in more than one sitting if desired to reduce fatigue.
Given the low level of walking in the mobility-limited older adults in this study, it is important to examine additional factors at both the individual and neighborhood environment levels that influence neighborhood walking and other forms of physical activity in this group. Cognition was not directly measured in this study and would be valuable to include in future studies. Other factors might include medication use, pain, fatigue, climate and the presence of popular neighborhood destinations as well as parks and walking trails within walking distance.
Conclusion
This study extends previous research in physical activity, aging and theory by using Social Cognitive Theory to examine the association between neighborhood environment, five types of self-efficacy, outcome expectations, and neighborhood walking in older adults with and without mobility limitations. Few studies have examined the influence of both the individual and neighborhood environment factors on walking in older adults and none have specifically examined neighborhood walking in older adults with and without mobility limitations. Results from this study indicated that older adults with mobility limitations walk in their neighborhoods for much shorter durations of time, have lower self-efficacy and fewer perceptions of positive outcomes from physical activity, and are more likely to walk in their neighborhood if stores, friends’ houses and other destinations are present. Interventions for older adults with mobility limitations should focus on 1) incorporating neighborhood destinations, 2) increasing self-efficacy, 3) managing barriers to physical activity, 4) preventing or treating negative outcomes or unpleasant symptoms, and 5) emphasizing positive outcomes that may ensue from even modest increases in activity.
References
- Alexander NA, Goldberg A. Common gait disturbances: A clinical overview. In: Hausdorff JM, Alexander NB, editors. Gait Disorders: Evaluation and Management. Boca Raton, FL: Taylor & Francis Group; 2005. pp. 1–18. [Google Scholar]
- Anderson ES, Wojcik JR, Winett RA, Williams DM. Social-cognitive determinants of physical activity: The influence of social support, self-efficacy, outcome expectations, and self-regulation among participants in a church-based health promotion study. Health Psychology. 2006;25(4):510–520. doi: 10.1037/0278-6133.25.4.510. [DOI] [PubMed] [Google Scholar]
- Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: Evidence from the Alameda County Study. American Journal of Epidemiology. 2002;155:507–515. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W.H. Freeman and Company; 1997. [Google Scholar]
- Bassett DR, Fitzhugh EC, Crespo CJ, King GA, McLaughlin JE. Physical activity and ethnic differences in hypertension prevalence in the United States. Preventive Medicine. 2002;34:179–186. doi: 10.1006/pmed.2001.0969. [DOI] [PubMed] [Google Scholar]
- Bean JF, Bailey A, Kiely DK, Leveille SG. Do attitudes toward exercise vary with differences in mobility and disability status? – A study among low-income seniors. Disability and Rehabilitation. 2007;29(15):1215–1220. doi: 10.1080/09638280600949910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belza B, Walwick J, Shiu-Thornton S, Schwartz S, Taylor M, LoGerfo J. Older adult perspectives on physical activity and exercise: Voices from multiple cultures. Preventing Chronic Disease. 2004;1(4):1–12. [PMC free article] [PubMed] [Google Scholar]
- Cervero R, Knockelman K. Travel demand and the 3Ds: density, diversity, and design. Transportation Research Part D. 1996;78:48–58. [Google Scholar]
- Chen Y-M. Perceived barriers to physical activity among older adults residing in long-term care institutions. Journal of Clinical Nursing. 2010;19:432–439. doi: 10.1111/j.1365-2702.2009.02990.x. [DOI] [PubMed] [Google Scholar]
- Clark DO, Nothwehr F. Exercise self-efficacy and its correlates among socioeconomically disadvantaged older adults. Health Education and Behavior. 1999;26(4):535–546. doi: 10.1177/109019819902600410. [DOI] [PubMed] [Google Scholar]
- Clarke P, Ailshire JA, Bader M, Morenoff JD, House JS. Mobility disability and the urban built environment. American Journal of Epidemiology. 2008;168(5):506–513. doi: 10.1093/aje/kwn185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P, George LK. The role of the built environment in the in the disablement process. American Journal of Public Health. 2005;95(11):1933–1939. doi: 10.2105/AJPH.2004.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conn V. Older adults and exercise: Path analysis of self-efficacy related constructs. Nursing Research. 1998;47(3):180–189. doi: 10.1097/00006199-199805000-00009. [DOI] [PubMed] [Google Scholar]
- Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2nd.ed. New York: John Wiley & Sons, Inc.; 2000. [Google Scholar]
- Faber MJ, Bosscher RJ, Chin A Paw MJ, van Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: A multicenter randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2006;87(7):885–896. doi: 10.1016/j.apmr.2006.04.005. [DOI] [PubMed] [Google Scholar]
- Frank LD, Engelke PO, Schmid TL. Health and Community Design. Washington: Island Press; 2003. [Google Scholar]
- Fuller BG, Stewart Williams JA, Byles JE. Active-living-the perception of older people with chronic conditions. Chronic Illness. 2010;6(4):294–305. doi: 10.1177/1742395310377673. [DOI] [PubMed] [Google Scholar]
- Gallagher NA, Gretebeck KA, Robinson J, Torres E, Murphy SL, Martyn K. Subjective measures of neighborhood environmental determinants of walking in older, urban African American adults. Journal of Aging and Physical Activity. 2010;18(1):99–115. doi: 10.1123/japa.18.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giles-Corti B, Timperio A; Cutt, H; Pikora TJ, Bull FC, Knuiman M, Bulsara M, Van Niel K, et al. Development of a reliable measure of walking within and outside the local neighborhood: RESIDE’s Neighborhood Physical Activity Questionnaire. Preventive Medicine. 2006;42(6):455–459. doi: 10.1016/j.ypmed.2006.01.019. [DOI] [PubMed] [Google Scholar]
- Gómez LF, Parra DC, Buchner D, Brownson RC, Sarmiento OL, Pinzón JD, …Lobelo F. Built environment attributes and walking patterns among the elderly population in Bogotá. American Journal of Preventive Medicine. 2010;38(6):592–599. doi: 10.1016/j.amepre.2010.02.005. [DOI] [PubMed] [Google Scholar]
- Gretebeck KA, Black DR, Blue CL, Glickman LT, Huston SA, Gretebeck RJ. Physical activity and function in older adults: The Theory of Planned Behavior. American Journal of Health Behavior. 2007;31(2):203–214. doi: 10.5555/ajhb.2007.31.2.203. [DOI] [PubMed] [Google Scholar]
- Hall KS, McAuley E. Individual, social environmental and physical environmental barriers to achieving 10,000 steps per day among older women. Health Education Research. 2010;25(3):478–488. doi: 10.1093/her/cyq019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JP, McDowell MA, Brody DJ. Leisure-time physical activity among US adults 60 or more years of age: Results from NHANES 1999–2004. Journal of Physical Activity and Health. 2008;5(3):347–358. doi: 10.1123/jpah.5.3.347. [DOI] [PubMed] [Google Scholar]
- King AC. Interventions to promote physical activity by older adults. Journal of Gerontology, Series A, Biological Sciences and Medical Sciences. 2001;56(2):36–46. doi: 10.1093/gerona/56.suppl_2.36. [DOI] [PubMed] [Google Scholar]
- Le Masurier GC, Bauman AE, Corbin CB, Konopack JF, Umstattd RM, Van Emmerik RE. Assessing walking behaviors of selected subpopulations. Medicine & Science in Sports & Exercise. 2008;40(7):S594–S602. doi: 10.1249/MSS.0b013e31817c68b1. [DOI] [PubMed] [Google Scholar]
- Li F, Fisher KJ, Brownson RC, Bosworth M. Multilevel modelling of built environment characteristics related to neighbourhood walking activity in older adults. Journal of Epidemiology and Community Health. 2005;59(7):558–564. doi: 10.1136/jech.2004.028399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord SE, Weatherall M, Rochester L. Community ambulation in older adults: Which internal characteristics are important? Archives in Physical Medicine and Rehabilitation. 2010;91(3):378–383. doi: 10.1016/j.apmr.2009.11.008. [DOI] [PubMed] [Google Scholar]
- Luukinen H, Lehtola S, Jokelainen J, Väänänen-Sainio R, Lotvonen S, Koistinen P. Prevention of disability by exercise among the elderly: A population-based, randomized, controlled, trial. Scandinavian Journal of Primary Health Care. 2010;24(4):199–205. doi: 10.1080/02813430600958476. [DOI] [PubMed] [Google Scholar]
- McAuley E. The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. Journal of Behavioral Medicine. 1992;15:65–88. doi: 10.1007/BF00848378. [DOI] [PubMed] [Google Scholar]
- McAuley E, Blissmer B, Katula J, Duncan TE. Exercise environment, self-efficacy, and affective responses to acute exercise in older adults. Psychology and Health. 2000;15:341–357. [Google Scholar]
- McAuley E, Hall KS, Motl RW, White SM, Wójcicki TR, Hu L, Doerksen SE. Trajectory of declines in physical activity in community-dwelling older women: Social cognitive influences. Journal of Gerontology, Series B, Psychological Sciences and Social Sciences. 2009;64B(5):543–550. doi: 10.1093/geronb/gbp049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley E, Katula J, Mihalko S, Blissmer B, Duncan TE, Pena M, Dunn E. Mode of physical activity and self-efficacy in older adults: A latent growth curve analysis. Journal of Gerontology, Series B, Psychological Sciences and Social Sciences. 1999;54B(5):282–293. doi: 10.1093/geronb/54b.5.p283. [DOI] [PubMed] [Google Scholar]
- McAuley E, Konopack JF, Morris KS, Motl RW, Hu L, Doerksen SE, Rosengren K. Physical activity and functional limitations in older women: influence of self-efficacy. Journal of Gerontology, Series B, Psychological Sciences & Social Sciences. 2006;61(5):P270–P277. doi: 10.1093/geronb/61.5.p270. [DOI] [PubMed] [Google Scholar]
- McAuley E, Mihalko SL, Rosengren K. Self-Efficacy and Balance Correlates of Fear of Falling in the Elderly. Journal of Aging and Physical Activity. 1997;5:329. [Google Scholar]
- McAuley E, Morris KS, Doerksen SE, Motl RW, Hu L, White SM, Wójcicki TR, Rosengren K. Effects of change in physical activity on physical function limitations in older women: mediating roles of physical function performance and self-efficacy. Journal of the American Geriatric Society. 2007;55(12):1967–1973. doi: 10.1111/j.1532-5415.2007.01469.x. [DOI] [PubMed] [Google Scholar]
- Michael YL, Beard T, Choi D, Farquhar S, Carlson N. Measuring the influence of built neighborhood environments on walking in older adults. Journal of Aging and Activity. 2006;14(3):302–312. doi: 10.1123/japa.14.3.302. [DOI] [PubMed] [Google Scholar]
- Michael YL, Carlson NE. Analysis of individual social-ecological mediators and moderators and their ability to explain effect of a randomized neighborhood walking intervention. International Journal of Behavioral Nutrition and Physical Activity. 2009;6(49):49–55. doi: 10.1186/1479-5868-6-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael YL, Green MK, Farquhar SA. Neighborhood design and active aging. Health and Place. 2005;12(4):734–740. doi: 10.1016/j.healthplace.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris KS, McAuley E, Motl RW. Neighborhood satisfaction, functional limitations, and self-efficacy influences on physical activity in older women. International Journal of Behavioral Nutrition and Physical Activity. 2008;27(5):13–20. doi: 10.1186/1479-5868-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motl RW, McAuley E. Physical activity, disability, and quality of life in older adults. Physical Medicine and Rehabilitation Clinics of North America. 2010;21(2):299–398. doi: 10.1016/j.pmr.2009.12.006. [DOI] [PubMed] [Google Scholar]
- Murphy SL, Williams CS, Gill TM. Characteristics associated with fear of falling and activity restriction in community-living older persons. Journal of the American Geriatrics Society. 2002;50(3):516–520. doi: 10.1046/j.1532-5415.2002.50119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers AM, Fletcher PC, Myers AH, Sherk W. Discrimination and evaluative properties of the Activities-specific Balance Confidence Scale. Journal of Gerontology, Series A, Biological Sciences and Medical Sciences. 1998;53A(4):M287–M294. doi: 10.1093/gerona/53a.4.m287. [DOI] [PubMed] [Google Scholar]
- Nagel CL, Carlson NE, Bosworth M, Michael YL. The relation between neighborhood built environment and walking activity among older adults. American Journal of Epidemiology, 15. 2008;168(4):461–468. doi: 10.1093/aje/kwn158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson PK, Chapman NJ. Urban form and older residents' service use, walking, driving, quality of life, and neighborhood satisfaction. American Journal of Health Promotion. 2003;19(1):45–52. doi: 10.4278/0890-1171-19.1.45. [DOI] [PubMed] [Google Scholar]
- Perkins JM, Multhaup KS, Perkins HW, Barton C. Self-efficacy and participation in physical and social activity among older adults in Spain and the United States. The Gerontologist. 2008;48(1):51–58. doi: 10.1093/geront/48.1.51. [DOI] [PubMed] [Google Scholar]
- Pikora TJ, Giles-Corti B, Knuiman MW, Bull FC, Jamrozik K, Donovan RJ. Neighborhood environmental factors correlated with walking near home: Using SPACES. Medicine & Science in Sports & Exercise. 2006;38(4):708–714. doi: 10.1249/01.mss.0000210189.64458.f3. [DOI] [PubMed] [Google Scholar]
- Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. The Journal of Gerontology A Biological Science & Medical Science. 1995;50A(1):M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- Protas EJ, Tissier S. Strength and speed training for elders with mobility disability. Aging and Physical Activity. 2009;17(3):257–271. doi: 10.1123/japa.17.3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasinaho M, Hirvensalo M, Leinonen R, Lintunen T, Rantanen T. Motives for and barriers to physical activity among older adults with mobility limitations. Journal of Aging and Physical Activity. 2007;15(1):90–102. doi: 10.1123/japa.15.1.90. [DOI] [PubMed] [Google Scholar]
- Rejeski WJ, Ettinger WH, Jr., Schumaker S, Burns R, Elam JT. Assessing performance-related disability in patients with knee osteoarthritis. Osteoarthritis Cartilage. 1995;3(3):157–167. doi: 10.1016/s1063-4584(05)80050-0. [DOI] [PubMed] [Google Scholar]
- Rejeski WJ, Ip EH, Marsh AP, Miller ME, Farmer DF. Measuring disability in older adults: the International Classification System of Functioning, Disability and Health (ICF) framework. Geriatrics & Gerontology International. 2008;8(1):48–54. doi: 10.1111/j.1447-0594.2008.00446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rejeski WJ, Marsh AP, Chmelo E, Prescott AJ, Dobrosielski M, Walkup M, Kritchevsy S. The Lifestyle Interventions and Independence for Elders Pilot (LIFE-P): 2-year follow-up. Journal of Gerontology, Series A, Biologic Sciences and Medical Sciences. 2009;64A(4):462–467. doi: 10.1093/gerona/gln041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick B. A prediction model of aerobic exercise in older adults living in a continuing-care retirement community. Journal of Aging and Health. 2001;13(2):287–310. doi: 10.1177/089826430101300207. [DOI] [PubMed] [Google Scholar]
- Resnick B, Orwig D, Zimmerman S, Hawkes W, Golden J, Werner-Bronzert M, Magaziner J. Testing of the SEE and OEE post hip fracture. Western Journal of Nursing Research. 2006;28:586–601. doi: 10.1177/0193945906287218. [DOI] [PubMed] [Google Scholar]
- Resnick B, Palmer MH, Jenkins LS, Spellbring AM. Path analysis of efficacy expectations and exercise behaviour in older adults. Journal of Advanced Nursing. 2000;31(6):1309–1315. doi: 10.1046/j.1365-2648.2000.01463.x. [DOI] [PubMed] [Google Scholar]
- Rodriguez DA, Evenson KR, Diez Roux AV, Brines SJ. Land use, residential density, and walking: The multi-ethnic study of atherosclerosis. American Journal of Preventive Medicine. 2009;37(5):397–404. doi: 10.1016/j.amepre.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roman CG, Chalfin A. Fear of walking outdoors. A multilevel ecologic analysis of crime and disorder. American Journal of Preventive Medicine. 2008;34(4):306–312. doi: 10.1016/j.amepre.2008.01.017. [DOI] [PubMed] [Google Scholar]
- Rosengren KS, McAuley E, Mihalko SL. Gait adjustments in older adults: activity and efficacy influences. Psychology and Aging. 1998;13(3):375–386. doi: 10.1037//0882-7974.13.3.375. [DOI] [PubMed] [Google Scholar]
- Saelens BE, Sallis JF, Black JB, Chen D. Neighborhood-based differences in physical activity: An environmental scale evaluation. American Journal of Public Health. 2003;93(9):1552–1558. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saelens BE, Sallis JF, Frank LD. Environmental correlates of walking and cycling: findings from the transportation, urban design, and planning literatures. Annals in Behavioral Medicine. 2003;25(2):80–91. doi: 10.1207/S15324796ABM2502_03. [DOI] [PubMed] [Google Scholar]
- Satariano WA, Ivey SL, Kurtovich E, Kealey M, Hubbard AE, Bayles CM, Prohaska TR. Lower-body function, neighborhoods, and walking in an older population. American Journal of Preventive Medicine. 2010;38(4):419–428. doi: 10.1016/j.amepre.2009.12.031. [DOI] [PubMed] [Google Scholar]
- Shaw BA, Spokane LS. Examining the association between education level and physical activity changes during early old age. Journal of Aging and Health. 2008;20(8):767–787. doi: 10.1177/0898264308321081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigematsu R, Sallis JF, Conway TL, Saelens BE, Frank LD, Cain KI, Chapman JE, King AC. Age differences in the relation of perceived neighborhood environment to walking. Medicine & Science in Sports & Exercise. 2009;41(2):314–321. doi: 10.1249/MSS.0b013e318185496c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shumway-Cook A, Patala A, Stewart A, Ferrucci L, Ciol MA, Guralnik JM. Environmental components of mobility disability in community-living older persons. Journal of the American Geriatric Society. 2003;51(3):393–398. doi: 10.1046/j.1532-5415.2003.51114.x. [DOI] [PubMed] [Google Scholar]
- Simonsick EM, Guralnik JM, Volpato S, Balfour J, Fried LP. Just get out the door! Importance of walking outside the home for maintaining mobility: Findings from the Women’s Health and Aging Study. Journal of the American Geriatric Society. 2005;53:198–203. doi: 10.1111/j.1532-5415.2005.53103.x. [DOI] [PubMed] [Google Scholar]
- Strath S, Isaacs R, Greenwald MJ. Operationalizing environmental indicators for physical activity in older adults. Journal of Aging and Physical Activity. 2007;15:412–424. doi: 10.1123/japa.15.4.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau, Office of Management and Budget. Federal Register: Standards for Defining Metropolitan and Micropolitan Statistical Areas. Notice. 2000;65(249) Wed. Dec. 27, 2000. [Google Scholar]
- van Stralen MM, de Vries H, Mudde AN, Bolman C, Lechner L. The long-term efficacy of two computer-tailored physical activity interventions for older adults: Main effects and mediators. Health Psychology. 2011 doi: 10.1037/a0023579. Advance online publication. doi: 10.1037/a0023579. [DOI] [PubMed] [Google Scholar]
- VanSwearingen JM, Perera S, Brach JS, Cham R, Rosano C, Studenski SA. A randomized trial of two forms of therapeutic activity to improve walking: Effect on the energy cost of walking. Journal of Gerontology: Medical Sciences. 2009;64(11):1190–1198. doi: 10.1093/gerona/glp098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Lee C. Site and neighborhood environments for walking among older adults. Health and Place. 2009;16(6):1268–1279. doi: 10.1016/j.healthplace.2010.08.015. [DOI] [PubMed] [Google Scholar]
- Wilbur J, Vassalo A, Chandler P, McDevitt J, Miller AM. Midlife women’s adherence to home-based walking during maintenance. Nursing Research. 2005;54(1):33–40. doi: 10.1097/00006199-200501000-00005. [DOI] [PubMed] [Google Scholar]
- Wilcox S, Bopp M, Oberrecht L, Kammermann SK, McElmurray CT. Psychosocial and perceived environmental correlates of physical activity in rural and older African American and White women. Journal of Gerontology, Series B, Psychological Sciences and Social Sciences. 2003;58B(6):P329–P337. doi: 10.1093/geronb/58.6.p329. [DOI] [PubMed] [Google Scholar]
- Wójcicki TR, White SM, McAuley E. Assessing outcome expectations in older adults: The Multidimensional Outcome Expectations for Exercise Scale (MOEES) Journals of Gerontology, Series B, Psychological Sciences and Social Sciences. 2009;64(1):33–40. doi: 10.1093/geronb/gbn032. [DOI] [PMC free article] [PubMed] [Google Scholar]