Abstract
Objectives
To investigate the 24 h effects of bimatoprost 0.01% monotherapy on intraocular pressure (IOP) and ocular perfusion pressure (OPP).
Design
Prospective, open-label experimental study.
Setting
Single tertiary ophthalmic clinic.
Participants
Sixteen patients with diagnosed primary open-angle glaucoma (POAG) or ocular hypertension (ages, 49–77 years).
Interventions
Baseline data of 24 h IOP in untreated patients were collected in a sleep laboratory. Measurements of IOP were taken using a pneumatonometer every 2 h in the sitting and supine body positions during the 16 h diurnal/wake period and in the supine position during the 8 h nocturnal/sleep period. After baseline measurements were taken, patients were treated with bimatoprost 0.01% one time per day at bedtime for 4 weeks, and then 24 h IOP data were collected under the same laboratory conditions.
Primary and secondary outcome measures
Diurnal and nocturnal IOP and OPP means under bimatoprost 0.01% treatment were compared with baseline.
Results
The diurnal and nocturnal IOP means were significantly lower under the bimatoprost 0.01% treatment than baseline in both the sitting and supine positions. The diurnal and nocturnal OPP means were significantly higher under treatment than baseline in both the sitting and supine positions.
Conclusion
Bimatoprost 0.01% monotherapy significantly lowered IOP and increased OPP during the 24 h period.
Keywords: Ophthalmology, Glaucoma, Clinical Pharmacology, Therapeutics, Clinical trials
Article summary.
Article focus
Diurnal and nocturnal effects of a new bimatoprost formulation.
Key messages
Bimatoprost 0.01% lowers intraocular pressure.
Bimatoprost 0.01% increases ocular perfusion pressure.
Strengths and limitations of this study
Experimental study under strictly controlled conditions.
Small sample size.
Introduction
Glaucoma is a progressive optic neuropathy characterised by pathologic loss of retinal ganglion cells and retinal nerve fibre layer with associated visual field loss. The lowering of intraocular pressure (IOP) is the only proven method to reduce the risk of glaucoma onset and slow disease progression.1 Studies have also shown an association between primary open-angle glaucoma (POAG) and vascular factors, such as systemic hypertension, hypotension, vasospasm, atherosclerosis and ocular blood flow.1 2 While the association between systemic blood pressure and POAG is weak, ocular perfusion pressure (OPP), the difference between ocular arterial blood pressure and IOP, shows a significant correlation to the prevalence, incidence and progression of the disease.2
Peak IOP is related to glaucoma progression, and previous studies have shown that IOP peaks of glaucoma patients frequently occur outside of office hours.3 4 Different classes of glaucoma drugs have variable IOP-lowering efficacies during the nocturnal/sleep period compared with their efficacies during the diurnal/wake period.5–9 Prostaglandin analogues, such as latanoprost and travoprost, have been shown to be effective in lowering IOP during both the diurnal and nocturnal periods.6 7 Bimatoprost (Lumigan, Allergan, Irvine, California, USA) is a prostaglandin F2α analogue that also lowers IOP.10 It appears to mimic the activity of prostaglandins and reduces IOP by enhancing uveoscleral and possibly trabecular outflow via direct effect on ciliary muscle relaxation and remodelling of extracellular matrix.11 Bimatoprost 0.03% has been demonstrated to be safe and highly effective in lowering IOP over the long term in glaucoma and ocular hypertension.12 13 The most common side effect of bimatoprost and other prostaglandin analogues is conjunctival hyperaemia, which can often lead to non-compliance or discontinuation of treatment.14
Bimatoprost 0.01% is a new formulation that was developed to improve the tolerability but maintain the IOP-lowering effectiveness of bimatoprost 0.03% in lowering IOP. A recent study showed that bimatoprost 0.01% is equivalent to bimatoprost 0.03% in lowering IOP during the diurnal/wake period throughout 12 months of treatment with less associated incidence of side effects such as conjunctival hyperaemia.15 However, the nocturnal IOP-lowering effect of bimatoprost 0.01% has not been investigated. In addition, the 24 h effect of bimatoprost 0.01% on OPP is unknown. The present study evaluated the 24 h effects on IOP and OPP of bimatoprost 0.01% monotherapy in a group of patients with POAG or ocular hypertension.
Materials and methods
This prospective study was approved by the University of California, San Diego Institutional Review Board, in accordance with the Health Insurance Portability and Accountability Act, and registered as a clinical trial (http://www.clinicaltrials.gov; NCT01271686). All methods adhered to the Declaration of Helsinki for research involving human subjects. Experimental subjects were recruited consecutively from patients with diagnosed bilateral POAG or ocular hypertension at the Hamilton Glaucoma Center of the University of California, San Diego, a tertiary ophthalmic clinic, with predefined inclusion and exclusion criteria. All subjects enrolled in this study were between 40 and 80 years old with untreated IOP equal to or above 22 mm Hg during office hours. Criteria for the diagnosis of glaucoma and ocular hypertension have been described previously.6 16 In brief, patients with ocular hypertension had untreated IOP over 21 mm Hg during the most recent two or more office visits, but otherwise normal optic discs and visual fields. Patients with POAG had abnormalities in optic discs or visual fields (or both). Subjects were fully informed about this study, and informed consents were obtained.
Subjects who smoked, had previous glaucoma surgery in either eye, had a history of ocular trauma or a sleep disorder, or had an irregular sleep schedule were excluded. All subjects’ medical history was reviewed and each subject had an eye examination, including slit-lamp biomicroscopy, gonioscopy, Goldmann applanation tonometry (Haag-Streit, Mason, Ohio, USA), dilated fundoscopy, and a visual field test. Individuals with ocular inflammation, narrow iridocorneal angle, severe cardiovascular or diabetic condition, or use of a systemic β-blocker for treating high blood pressure were excluded. Routine systemic medications used by the subjects were documented and subjects with a change in the systemic medications during the study period would be excluded.
Subjects were either treatment naïve or washed out from a prior glaucoma medication 4 weeks prior to enrolment at the discretion of the ophthalmologist. Subjects were instructed to maintain a daily 8 h regular sleep schedule for 1 week before the laboratory recording, and this 8 h period was referred to as the nocturnal/sleep period. Individual sleep periods were verified using a wrist monitor for light exposure and arm movements (Actiwatch, Mini Mitter, Sunriver, Oregon, USA) and a wake/sleep log. Subjects were asked to abstain from alcohol for 3 days and coffee for 1 day before the laboratory session beginning at approximately 14:00 hours. Baseline data of 24 h IOP in a sleep laboratory were collected. Subjects were then treated with bimatoprost 0.01% in both eyes one time nightly approximately a half hour before bedtime. The bimatoprost 0.01% treatment lasted for 4 weeks before the second 24 h laboratory recording.
Laboratory conditions and general experimental procedures have been described previously.8 The 8 h nocturnal/sleep period in the laboratory for each subject was adjusted to correspond to the recorded bedtime in the previous week. Clock times for the IOP measurements were also individualised. However, laboratory data were aligned as if each subject had a nocturnal/sleep period from 23:00 to 07:00 hours. The actual length of sleep in the laboratory may be less than 8 h in some subjects. Subjects were encouraged to continue normal indoor activities in the laboratory. Food and water were available, and meal times were not regulated. During the second laboratory recording, subjects self-administered the bimatoprost 0.01% eye drops under supervision at approximately 22:30 hours.
IOP, blood pressure and heart rate were measured every 2 h. Experienced researchers performed the measurements in three random shifts. Their interindividual variations of IOP measurements were confirmed as insignificant (within ±2 mm Hg). IOP was measured using a calibrated pneumatonometer (Reichert, Depew, New York, USA). Topical 0.5% proparacaine was used as the local anaesthetic. Every plot of IOP measurement was evaluated according to commonly accepted standards.17 Blood pressure and heart rate were measured immediately before the IOP measurements using an automated arm monitor (Accutorr Plus, Datascope Inc., Montvale, New Jersey, USA). The cuff was mounted over the brachial artery, level with the heart and removed after the measurement. Before bedtime, measurements were taken at 15:30, 17:30, 19:30 and 21:30 hours. Subjects were instructed to lie in bed for 5 min before the supine measurements and then to sit for 5 min before the sitting measurements. Lights in individual sleep rooms were turned off at 23:00 hours. Measurements were taken supine only at 23:30, 01:30, 03:30 and 05:30 hours. Subjects were awakened, and the measurements were taken immediately. A dim red room light of less than 10 lux was used to assist the measurements. Some sleep disturbance was unavoidable because of the nocturnal measurements, and the levels of blood pressure and IOP may be influenced by the measurement procedure. However, both laboratory sessions are affected, and effects of sleep disturbance and nocturnal measurement procedures on IOP may be insignificant.18 19 Room lighting was restored at 07:00 hours, and subjects were awakened. Measurements were taken at 07:30, 09:30, 11:30 and 13:30 hours. Timings of the measurements were documented using infrared camera recording.
Data of IOP from both eyes were averaged. Mean arterial blood pressure was calculated as the diastolic blood pressure plus one-third of the difference between the systolic and the diastolic blood pressures. Means of IOP, blood pressure and heart rate were calculated for the diurnal period (eight readings between 07:00 and 23:00 hours) and the nocturnal period (four readings between 23:00 and 07:00 hours). Diurnal and nocturnal OPP in different body positions were calculated, using previously described formulae based on the mean blood pressure and IOP, adjusted for the height of the eye over the heart:20
Sitting OPP=95/140×mean blood pressure−IOP
Supine OPP=115/130×mean blood pressure−IOP
Statistical comparisons of study parameters were performed between the bimatoprost 0.01% treatment and the baseline using the paired t-test. Normal distribution of test data was confirmed using the Kolmogorov-Smirnov test. The criterion for statistical significance was p<0.05.
Results
Sixteen subjects were recruited between January and August 2011, and all completed the study. Their demographic data are presented in table 1. Thirteen patients had an ocular hypertension diagnosis and three patients had a POAG diagnosis. Fourteen patients were newly diagnosed and untreated before the enrolment. One patient with ocular hypertension was treated with latanoprost and the other patient with ocular hypertension was treated with dorzolamide. These two patients underwent a 4-week washout before the first laboratory recording. The last office-hour IOP measured using the Goldmann tonometer under no treatment before the laboratory recording was 26.4±3.7 mm Hg (mean±standard deviation; range 22–36 mm Hg).
Table 1.
Demographic characteristics of 16 study participants
| Gender | 10 male, 6 female |
| Ancestry | 11 White, 2 Asian, 2 Black, 1 Hispanic |
| Age (years) | 61.0±8.5 (49–77) |
| Height (in) | 67.3±3.9 (61–74) |
| Weight (lb) | 177.1±35.4 (125–232) |
| Body mass index (lb2) | 27.4±4.5 (19.6–33.8) |
| Central corneal thickness (µm) | 591.0±56.0 (490–695) |
Values represent the mean±standard deviation (range).
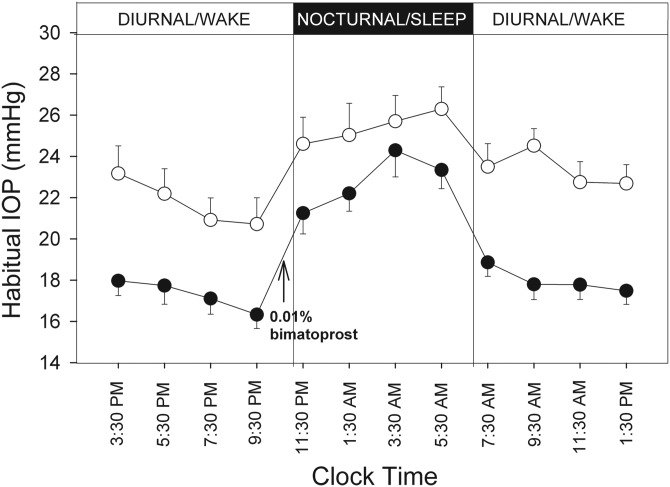
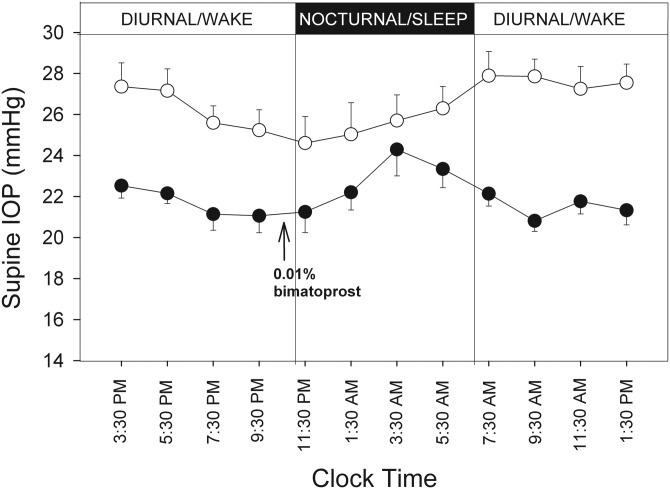
Figure 1 shows the 24 h profiles of habitual IOP (sitting during the day and supine at night) under the two experimental conditions. As shown, IOP increased significantly during the transition from the diurnal period to the nocturnal period when the body position changed from sitting to supine, and IOP decreased significantly during the transition from the nocturnal to the diurnal period. During the 16 h diurnal period, the mean IOP under the bimatoprost 0.01% treatment was consistently lower than the baseline. During the 8 h nocturnal period, mean IOP levels under the bimatoprost 0.01% treatment were also lower than baseline. The IOP reduction was approximately 2 times during the diurnal period than during the nocturnal period. Figure 2 presents the 24 h supine IOP profiles at baseline and under bimatoprost 0.01% treatment. Supine IOP under the bimatoprost 0.01% treatment was lower than the baseline during the diurnal period.
Figure 1.
Profiles of 24 h IOP in the habitual body positions. Measurements were taken from 16 subjects sitting during the diurnal period and supine during the nocturnal period. Open circles represent the baseline, and solid circles represent the bimatoprost 0.01% treatment for 4 weeks. Error bars represent standard error of the mean. IOP, intraocular pressure.
Figure 2.
Profiles of 24 h supine IOP. Open circles represent the baseline, and solid circles represent the bimatoprost 0.01% treatment for 4 weeks. Data were from the same 16 subjects as in figure 1. Error bars represent standard error of the mean. IOP, intraocular pressure.
Table 2 summarises the mean diurnal and nocturnal IOP levels, mean blood pressures and mean OPP under the two experimental conditions. During the diurnal period, sitting and supine IOP under the bimatoprost 0.01% treatment were significantly lower than the baseline IOP in the same body position (p<0.001). During the nocturnal period, the supine IOP under the bimatoprost 0.01% treatment was also significantly lower than the baseline IOP (p<0.01). There was no significant change in systolic, diastolic or mean blood pressure with bimatoprost 0.01% treatment. During the diurnal period, OPP in the sitting or supine position was significantly greater with bimatoprost 0.01% treatment than at baseline (p<0.001). In the nocturnal period, the OPP with treatment was also significantly greater than baseline (p<0.05).
Table 2.
Mean IOP, BP and OPP before and after treatment with bimatoprost 0.01%
| Baseline | Post-treatment | Difference | p Value | |
|---|---|---|---|---|
| Diurnal sitting | ||||
| Mean IOP | 22.6 ± 3.9 | 17.6 ± 2.5 | −4.9 ± 3.5 | <0.001 |
| Mean BP | 91.1 ± 9.4 | 91.6 ± 9.9 | 0.6 ± 5.3 | 0.67 |
| Mean OPP | 39.2 ± 7.4 | 44.5 ± 7.1 | 5.3 ± 3.8 | <0.001 |
| Diurnal supine | ||||
| Mean IOP | 27.0 ± 3.4 | 21.6 ± 2.0 | −5.4 ± 3.1 | <0.001 |
| Mean BP | 87.7 ± 8.9 | 87.4 ± 7.5 | 0.4 ± 5.2 | 0.75 |
| Mean OPP | 49.9 ± 9.0 | 55.7 ± 7.2 | 5.7 ± 4.6 | <0.001 |
| Nocturnal supine | ||||
| Mean IOP | 25.4 ± 4.8 | 22.8 ± 3.7 | −2.6 ± 2.8 | <0.01 |
| Mean BP | 83.6 ± 10.4 | 85.8 ± 7.9 | 2.2 ± 8.6 | 0.31 |
| Mean OPP | 48.5 ± 10.4 | 53.1 ± 6.6 | 4.6 ± 7.5 | <0.05 |
All data in mm Hg unit (mean±standard deviation; N=16).
Diurnal: 07:00 to 23:00 hours, nocturnal: 23:00 to 07:00 hours.
BP, blood pressure; IOP, intraocular pressure; OPP, ocular perfusion pressure; p value performed with paired t-test.
There was no significant change in the heart rate with bimatoprost 0.01% treatment in both body positions during the diurnal/wake period, but the supine heart rate during the nocturnal period was significantly reduced by 6.3±9.2 beats/min under the treatment (p<0.05).
Discussion
Our results showed a significant IOP-lowering effect of bimatoprost 0.01% monotherapy during both the diurnal and nocturnal periods. The nocturnal IOP-lowering efficacy of bimatoprost 0.01% was less than that of the diurnal period, similar to previous studies with latanoprost and travoprost.6 7 Posture was not a factor in the modulated nocturnal IOP-lowering efficacy since IOP measurements under treatment in the supine position demonstrated greater IOP reduction during the wake period than at night. It is possible that the difference in diurnal and nocturnal efficacies is related to the pharmacokinetics of prostaglandin analogues given once a day in the evening.
Reduced OPP could enhance glaucomatous optic nerve damage. POAG patients often have their lowest blood pressures at night, and a reduction in nocturnal blood pressure may lower perfusion pressure to ocular tissues.21 The present study demonstrated that the systolic, diastolic and mean blood pressures did not significantly change over the 24 h period with bimatoprost 0.01% treatment compared to baseline. In contrast, the diurnal and nocturnal OPP significantly increased under bimatoprost 0.01% treatment, reflecting the fact that treatment significantly decreased IOP. This increase in OPP may have favourable implications in the treatment of glaucoma. However, the study population was skewed because we only included those patients with office-hour IOP measurements of 22 mm Hg or greater. Most patients (13 of 16) enrolled in the present study were with ocular hypertension, not with POAG. This selection bias allowed for a potentially greater reduction of IOP. Consequently, there may not be a significant effect of bimatoprost 0.01% on OPP during the diurnal or nocturnal period for glaucoma patients with IOP less than 22 mm Hg.
Bimatoprost 0.01% was formulated with the goal of improving the safety profile and tolerability of the medication while maintaining the IOP-lowering effect of bimatoprost 0.03%. This would be achieved by lowering the concentration of bimatoprost and increasing the concentration of benzalkonium chloride (0.05–0.2%), a commonly used preservative that increases corneal penetration and intraocular bioavailability of topically applied medications.22 Whether or not the formulation used for bimatoprost 0.01% may have modified the time-dependent IOP-lowering profile of bimatoprost 0.03% cannot be answered by the present study.14 23–26
In summary, bimatoprost 0.01% monotherapy results in IOP lowering both during the diurnal/wake and nocturnal/sleep periods, with the IOP-lowering effect being greater in the waking hours. Moreover, bimatoprost 0.01% significantly increases OPP over the 24 h period.
Supplementary Material
Footnotes
Contributors: All authors made a significant contribution in designing the study, performing the experiments, evaluating the results and writing the manuscript. All authors had full access to and can take responsibility for the data and analyses.
Funding: This study was supported by an independent research grant (JHKL) from Allergan and an unrestricted grant from Research to Prevent Blindness (New York, USA). Allergan has no control or influence on this study.
Competing interests: JHKL has received support for research from Alcon and Allergan. RNW is a consultant for Alcon, Allergan, Bausch & Lomb, Merck Research Laboratories and Pfizer, and has received lecture fees from Alcon and Allergan. FAM is a consultant for Alcon, Allergan and Pfizer, and has received lecture fees from Allergan and Pfizer.
Ethics approval: This study was approved by the University of California, San Diego Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data available on request from the corresponding author.
References
- 1.Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet 2004;363:1711–20 [DOI] [PubMed] [Google Scholar]
- 2.Weinreb RN, Harris A. Ocular blood flow in Glaucoma. WGA consensus series 6. Amsterdam, the Netherlands: Kugler Publications, 2009:59–128 [Google Scholar]
- 3.Medeiros FA, Brandt J, Liu J, et al. IOP as a risk factor for glaucoma development and progression. In: Weinreb RN, Brandt JD, Garway-Heath DF, et al. Intraocular pressure: reports and consensus statements of the 4th Global AIGS Consensus meeting on intraocular pressure. The Hague, The Netherlands: Kugler, 2007:59–74 WGA Consensus Series 4 [Google Scholar]
- 4.Bagga H, Liu JH, Weinreb RN. Intraocular pressure measurements throughout the 24 h. Curr Opin Ophthalmol 2009;20:79–83 [DOI] [PubMed] [Google Scholar]
- 5.Orzalesi N, Rossetti L, Invernizzi T, et al. Effect of timolol, latanoprost, and dorzolamide on circadian IOP in glaucoma or ocular hypertension. Invest Ophthalmol Vis Sci 2000;41:2566–73 [PubMed] [Google Scholar]
- 6.Liu JH, Kripke DF, Weinreb RN. Comparison of the nocturnal effects of once-daily timolol and latanoprost on intraocular pressure. Am J Ophthalmol 2004;138:389–95 [DOI] [PubMed] [Google Scholar]
- 7.Sit AJ, Weinreb RN, Crowston JG, et al. Sustained effect of travoprost on diurnal and nocturnal intraocular pressure. Am J Ophthalmol 2006;141:1131–3 [DOI] [PubMed] [Google Scholar]
- 8.Liu JH, Medeiros FA, Slight JR, et al. Comparing diurnal and nocturnal effects of brinzolamide and timolol on intraocular pressure in patients receiving latanoprost monotherapy. Ophthalmology 2009;116:449–54 [DOI] [PubMed] [Google Scholar]
- 9.Liu JH, Medeiros FA, Slight JR, et al. Diurnal and nocturnal effects of brimonidine monotherapy on intraocular pressure. Ophthalmology 2010;117:2075–9 [DOI] [PubMed] [Google Scholar]
- 10.Woodward DF, Phelps RL, Krauss AH, et al. Bimatoprost: a novel antiglaucoma agent. Cardiovasc Drug Rev 2004;22:103–20 [DOI] [PubMed] [Google Scholar]
- 11.Toris CB, Gabelt BT, Kaufman PL. Update on the mechanism of action of topical prostaglandins for intraocular pressure reduction. Surv Ophthalmol 2008;53(Suppl 1):S107–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams RD, Cohen JS, Gross RL, et al. Long-term efficacy and safety of bimatoprost for intraocular pressure lowering in glaucoma and ocular hypertension: year 4. Br J Ophthalmol 2008;92:1387–92 [DOI] [PubMed] [Google Scholar]
- 13.Aptel F, Cucherat M, Denis P. Efficacy and tolerability of prostaglandin analogs: a meta-analysis of randomized controlled clinical trials. J Glaucoma 2008;17:667–73 [DOI] [PubMed] [Google Scholar]
- 14.Konstas AG, Katsimbris JM, Lallos N, et al. Latanoprost 0.005% versus bimatoprost 0.03% in primary open-angle glaucoma patients. Ophthalmology 2005;112:262–6 [DOI] [PubMed] [Google Scholar]
- 15.Katz LJ, Cohen JS, Batoosingh AL, et al. Twelve-month, randomized, controlled trial of bimatoprost 0.01%, 0.0125%, and 0.03% in patients with glaucoma or ocular hypertension. Am J Ophthalmol 2010;149:661–71 e1 [DOI] [PubMed] [Google Scholar]
- 16.Liu JH, Zhang X, Kripke DF, et al. Twenty-four-hour intraocular pressure pattern associated with early glaucomatous changes. Invest Ophthalmol Vis Sci 2003;44:1586–90 [DOI] [PubMed] [Google Scholar]
- 17.Liu JH, Kripke DF, Twa MD, et al. Twenty-four-hour pattern of intraocular pressure in the aging population. Invest Ophthalmol Vis Sci 1999;40:2912–7 [PubMed] [Google Scholar]
- 18.Mansouri K, Shaarawy T. Continuous intraocular pressure monitoring with a wireless ocular telemetry sensor: initial clinical experience in patients with open angle glaucoma. Br J Ophthalmol 2011;95:627–9 [DOI] [PubMed] [Google Scholar]
- 19.Liu JH, Weinreb RN. Monitoring intraocular pressure for 24 h. Br J Ophthalmol 2011;95:599–600 [DOI] [PubMed] [Google Scholar]
- 20.Liu JH, Gokhale PA, Loving RT, et al. Laboratory assessment of diurnal and nocturnal ocular perfusion pressures in humans. J Ocul Pharmacol Ther 2003;19:291–7 [DOI] [PubMed] [Google Scholar]
- 21.Quaranta L, Gandolfo F, Turano R, et al. Effects of topical hypotensive drugs on circadian IOP, blood pressure, and calculated diastolic ocular perfusion pressure in patients with glaucoma. Invest Ophthalmol Vis Sci 2006;47:2917–23 [DOI] [PubMed] [Google Scholar]
- 22.Nakamura T, Yamada M, Teshima M, et al. Electrophysiological characterization of tight junctional pathway of rabbit cornea treated with ophthalmic ingredients. Biol Pharm Bull 2007;30:2360–4 [DOI] [PubMed] [Google Scholar]
- 23.Orzalesi N, Rossetti L, Bottoli A, et al. Comparison of the effects of latanoprost, travoprost, and bimatoprost on circadian intraocular pressure in patients with glaucoma or ocular hypertension. Ophthalmology 2006;113:239–46 [DOI] [PubMed] [Google Scholar]
- 24.Yildirim N, Sahin A, Gultekin S. The effect of latanoprost, bimatoprost, and travoprost on circadian variation of intraocular pressure in patients with open-angle glaucoma. J Glaucoma 2008;17:36–9 [DOI] [PubMed] [Google Scholar]
- 25.Quaranta L, Pizzolante T, Riva I, et al. Twenty-four-hour intraocular pressure and blood pressure levels with bimatoprost versus latanoprost in patients with normal-tension glaucoma. Br J Ophthalmol 2008;92:1227–31 [DOI] [PubMed] [Google Scholar]
- 26.Konstas AG, Hollo G, Mikropoulos D, et al. Twenty-four-hour intraocular pressure control with bimatoprost and the bimatoprost/timolol fixed combination administered in the morning, or evening in exfoliative glaucoma. Br J Ophthalmol 2010;94:209–13 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.