Abstract
Background and Purpose
Human papillomavirus (HPV) vaccine was approved for girls aged 9–24 years in 2006 to prevent HPV infection and cervical cancer. The Parental Human Papillomavirus Survey (PHPVS) was framed on theoretical constructs of the health belief model (HBM) and developed to survey parents regarding their HPV knowledge, attitudes, and intent to vaccinate.
Methods
We evaluated the psychometric properties of the PHPVS using classical item analysis and exploratory factor analysis (EFA) among a sample of 200 parents/caregivers.
Results
The EFA yielded a 4-factor unidimensional model that explained between 62% and 68% of the total variance depending on the extraction method used. The estimated Cronbach’s alpha for the PHPVS was .96.
Conclusions
The PHPVS is a reliable measure of HPV knowledge, attitudes, and intent to vaccinate.
Keywords: HPV vaccines, health surveys, health care disparities, pediatrics, adolescents, Parents
Human papillomavirus (HPV) infection is etiologically linked to cancers of the cervix, anus, oropharynx, penis, vagina, and vulva (Parkin & Bray, 2006). The HPV vaccine is a health care breakthrough and an essential element of health promotion in pediatric and adolescent health care for boys and girls (Chaturvedi, 2010). The Centers for Disease Control and Prevention (CDC) and the Advisory Committee on Immunization Practices (ACIP) recommends vaccinating girls and boys from the age of 9 to 26 years (CDC, 2010). To eliminate HPV-related cancers through HPV vaccination, it is essential to recognize the factors involved in parents’ decision whether to permit their children to get the HPV vaccine (Harper et al., 2006). Indeed, the prevalence of HPV infection and cervical cancer rates continue to increase in African American and Latina women (Kobetz et al., 2010). So, the primary author sought to develop a theory-based survey that was short and simple to use with items that could identify intervention points to address HPV vaccination in populations of children and adolescents with low vaccine rates and those experiencing health disparities.
PURPOSE
The purpose of this article is to describe the development and results of the psychometric evaluation of the Parental HPV Survey (PHPVS). The PHPVS was developed in 2007 in response to the debut of the HPV vaccine and the controversy that followed. During the spring of 2007, nurses and other health care providers discussed with policy makers and public health officials which parents would or would not vaccinate their child or adolescent with the HPV vaccine. The PHPVS was developed and then psychometrically tested so researchers would have an instrument to use in health promotion research. The PHPVS instrument can assist health promotion researchers to explore and describe parental perceptions of HPV infection and vaccination by measuring the perceived severity of HPV infection, parental perceived vulnerability of their child to HPV infection, the perceived benefits of HPV vaccination, and the subsequent barriers to vaccinating their child with the HPV vaccine.
SCOPE OF MEASUREMENT
This survey development was rooted in the construct of primary prevention from Neuman’s Systems Model (NSM) and then developed after further literature review on social psychology theory and the health belief model (HBM; Neuman, 1990, 1996; Rosenstock, 1975; Rosenstock, Strecher, & Becker, 1988). By using this theory, the PHPVS could be used to collect descriptive data to develop primary prevention interventions to reduce HPV-related cancers in populations experiencing health disparities and to begin to use the PHPVS in primary care to elicit parental attitudes and knowledge about HPV and the HPV vaccine.
BACKGROUND AND CONCEPTUAL FRAMEWORK
A Healthcare Breakthrough and a Controversy
Current research findings indicate that parents and caregivers of elementary and middle school children are often misinformed and subsequently filled with anxiety, mistrust, and doubt about reproductive health issues, such as HPV vaccination (Foster, 2007; Moseley, Freed, Bullard, & Goold, 2007; Shafii, Stovel, Davis, & Holmes, 2004). Current research data on parental acceptance of the HPV vaccine are consistent with previous research on acceptability of the herpes simplex virus (HSV) vaccination, reproductive health education, oral contraceptives, and information on sexually transmitted infections (STIs); parents are fearful that these types of health care innovations can lead to promiscuity (Eisenberg, Bearinger, Sieving, Swain, & Resnick, 2004; Hofferth, Kahn, & Baldwin, 1987; Zimet et al., 1997; Zimet, Kee, Winston, Perkins, & Maharry, 2001). The controversy of vaccinating children and adolescents with the HPV vaccine persisted in 2006 because of concerns that it would lead to behavioral disinhibition by encouraging adolescent sexual promiscuity, sexual irresponsibility, or early sexual activity (Hofferth et al., 1987; O’Sullivan, Meyer-Balhburg, & Watkins, 2000). This was supported during 2006 and 2007 by long-standing parental concern that media exposure and discussion of sexually related topics will increase the likelihood that their children will become sexually active (Hofferth et al., 1987).
Initial surveys conducted prior to the introduction of the HPV vaccine with the general public examined general vaccination patterns and only included a single or 2–3 items on HPV vaccination; results implied that parents may not vaccinate against HPV for religious or moral reasons (Dempsey, Zimet, Davis, & Koutsky, 2006). Although religious and moral reasons for not vaccinating children have been an ongoing challenge for nursing and health care professionals, it is important that nursing professionals recognize this possible controversy and give parents balanced and complete information about this vaccine (Thomas, 2008). To this end, the PHPVS was developed to assist the provision of accurate information in the context of what parents or caregivers may or may not understand about HPV-related cancers and the HPV vaccine. The PHPVS differs from earlier surveys because it includes items such as self-reported religious affiliation and specific items framed on theoretical constructs, unlike any survey on HPV vaccination had done previously. Accordingly, the use of the PHPVS could help both researchers and clinicians examine parental attitudes and knowledge. Parental attitudes and knowledge about vaccination is essential to develop culturally specific interventions to address misinformed parents and adolescents who are at increased risk for HPV infection (McKee & Karasz, 2006).
The Theoretical Framework
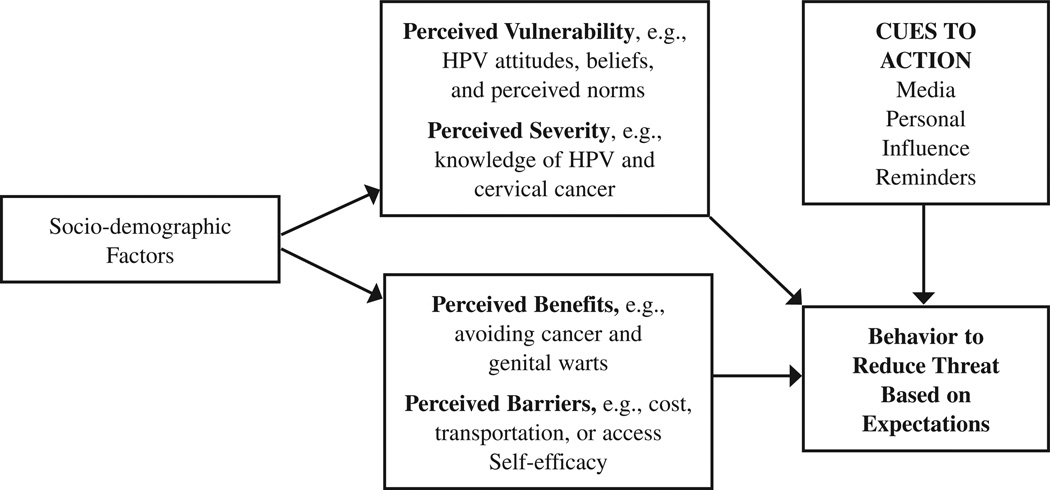
The theoretical framework guiding this work was selected because it was developed to study behaviors related to vaccination and other primary prevention behaviors. The HBM identifies determinants of health-related behavior for a specific health behavior, such as vaccinating a child. In addition, the HBM postulates four factors that account for health-related behavior: perceived vulnerability to a threat (like HPV infection), perceived severity of HPV infection or consequences of not being vaccinated, perceived benefits of being vaccinated, and perceived barriers to being vaccinated (Figure 1; Rosenstock et al., 1988).
Figure 1.
The health belief model constructs with PHPVS item categories.
Psychometric Properties of Health Belief Model Related Measures
The HBM-related measures are prolific throughout the health promotion literature (Harrison, Mullen, & Green, 1992). Some studies have evaluated the psychometric properties of HBM-related measures associated with HPV vaccination and screening (Fernández et al., 2009; Gerend & Shepherd, 2012; Guvenc, Akyuz, & Açikel, 2011; Kahn et al., 2008; Marlow, Waller, Evans, & Wardle, 2009; McRee, Brewer, Reiter, Gottlieb, & Smith, 2010; Zimet et al., 2005). A few of these studies have used either exploratory or confirmatory factor analyses to evaluate the factor structures underlying HBM in this context (Gerend & Shepherd, 2012; Guvenc et al., 2011; Kahn et al., 2008; Marlow et al., 2009; McRee et al., 2010). The subscale reliabilities for these studies vary considerably. Cronbach’s alpha (α) ranged from .55 in Marlow et al. (2009) to .96 in Kahn et al. (2008). Most studies retained between 4 and 5 factors; however, one study (Kahn et al., 2008) yielded a 10 factor structure.
The Need for a Parental Survey
Public debate continues among parents of all backgrounds because of the high cost of the HPV vaccine and fears that the HPV vaccine provides tacit permission for children to engage in sexual activity. The impetus for the PHPVS’ development and use in descriptive research was generated by the disproportionately higher rates of HPV-related cancers, including cervical cancer, and the dearth of information on parental knowledge, attitudes, beliefs, perceived vulnerability, perceived severity, perceived benefits, and perceived barriers for vaccinating their children with the HPV vaccine.
PROCEDURES FOR INSTRUMENT DEVELOPMENT
The development of the parental HPV survey was completed in several steps. In the spring of 2007, an intensive literature search was completed, including review of other types of general vaccine surveys and surveys with items about HPV vaccination. Drafts of the PHPVS were then reviewed and critiqued by parents and providers. Further evaluation and literature review then led to refinement of survey items, and these survey items were revised to reflect the constructs of the HBM. This borrowing of theories proved to be essential to lending clarity to the PHPVS’ development and applicability to nursing research (Villarruel, Bishop, Simpson, Jemmott, & Fawcett, 2001).
The 2008 versions of the PHPVS items were organized by HBM theoretical constructs into subscales: perceived vulnerability, perceived severity, perceived benefits, and perceived barriers with items that addressed knowledge, attitudes, beliefs, and intent to vaccinate. The results of further pilot testing demonstrated that some items were redundant, and several experts encouraged the addition of negative items to test for validity. As a result, some items were deleted, and several false statements were included. This process took more than 10 months. Although at times challenging, this process was important because the process led to the development of an instrument that was (a) theoretically framed; (b) could be used for quantitative research; (c) was simply enough to be translated to other languages as needed; (d) was brief and concise as to be “parent friendly”; and (e) could be implemented in primary care settings to inform health care providers about individual parent knowledge and attitudes about HPV vaccination. In 2009, PHPVS items were then organized into the final survey format described in the following texts.
DESCRIPTION OF THE INSTRUMENT
The PHPVS contains 28 survey items to describe parental beliefs and attitudes about the HPV vaccine and vaccinations in general, parental decision making and intentions, and the acceptability of vaccinating their child for HPV, along with experiential factors such as whether or not the parent knows someone who has been diagnosed with a sexually transmitted disease. All survey items and their correlated theoretical concepts have demonstrated intent to vaccinate in other studies (Zimet et al., 1997). General questions about personal characteristics, such as age and gender, were placed at the beginning of the survey. Questions that were more sensitive—such as household income, educational level, and marital status—were placed at the end of the survey and included a “refuse to answer” option.
ADMINISTRATION OF THE INSTRUMENT
The ethical considerations of all aforementioned research projects were addressed and approved prior to data collection by ethics committees from university and county school boards. After community engagement was initiated, the PHPVS survey in English was used to survey 200 parents or caregivers attending elementary and middle school parent–teacher meetings in the Southeastern United States. At a parent–teacher school meeting, study personnel were introduced and the research study was explained. A letter of explanation was given to parents or caregivers of children aged 9–13 years of age. The content of the letter explained that all results would be reported anonymously and in group format. Parents and caregivers of children aged 9–13 years who spoke and read English (met inclusion criteria) were then invited to complete the anonymous survey. In addition, privacy for each participant was maintained by providing a separate area to complete the survey with returned surveys considered implied consent. As the parent or caregiver turned in the survey, they received a gift certificate from a local grocery store chain.
SCORING OF THE INSTRUMENT
A five-choice Likert scale response was provided for parents. Parents responded by circling 1 = disagree, 2 = slightly disagree, 3 = unsure, 4 = slightly agree, and 5 = agree. Throughout all survey development, scoring was cumulative with higher scores indicating greater knowledge and greater intent to vaccinate their child and complete the HPV vaccination series.
METHODS
Sample
The samples used for developing and initial piloting of the PHPVS were relatively small and, for this statistical evaluation, we chose to evaluate surveys completed by parents with children attending elementary and middle schools in the Southeastern United States (n =200). Participants included any parent or caregiver with a daughter aged 9–13 years of age. The parent/caregiver completing the survey was required to be 18 years of age and able to understand English.
Procedures
We evaluated the psychometric properties of the PHPVS using classical item analysis and exploratory factor analysis (EFA) among a sample of 200 parents/caregivers. Using classical item analysis, we evaluated the item level statistics/functioning including scale reliability (Cronbach’s alpha), interitem correlations, and standard errors. An EFA was conducted to identify general or latent variables. The EFA identifies the factor structure for a given set of variables through determining the number of factors and the pattern of factor loadings (Stapleton, 1997; Yanai & Ichikawa, 2006). This method allows the researcher to identify the minimal number of dimensions necessary to delineate relationships among the variables.
Factor analysis was performed using the principal axis factor extraction method, which focuses on the shared (common) variance within the 28 items. Oblique rotation (δ = 0) was used because it was expected that the resulting factors would be correlated. The Kaiser–Meyer–Olkin (KMO) measure of adequacy was calculated to evaluate sampling adequacy. Bartlett’s test of sphericity was performed to assure that the items included in the factor analysis were related and not independent (i.e., factor analysis was appropriate; Field, 2009; Tabachnick & Fidell, 2007).
The following three methods were used to determine the optimal number of factors to retain: number of eigenvalues greater than 1, Velicer’s minimum average partial (MAP) test, and the parallel analysis approach (O’Connor, 2000). Because each extraction method has inherent limitations, it is prudent to compare results (Zwick & Velicer, 1986).
Approaches to Reliability and Validity Assessments
Item- and subscale-level Cronbach’s alpha and interitem correlations were calculated as measures of reliability. Factor analysis and reliability statistics were performed on the entire instrument of 28 items as well as on each of the four theory-derived subscales. Tests for external validity were precluded by the lack of similar measures. All statistical analyses were performed using SPSS (v19.0.0.1, IBM Company, 2010).
RESULTS
The factor analysis yielded a four-factor model that explained between 62% and 68% of the total variance depending on the extraction method used. The observed factor structure of the 28 items appears to be consistent with that of similar HBM studies in this context (Gerend & Shepherd, 2012; Guvenc et al., 2011; Marlow et al., 2009; McRee et al., 2010). Each extraction method yielded very similar results. As seen in Table 1, MAP analysis indicated three components, parallel analysis indicated four factors, and four of the initial eigenvalues were greater than 1.
Table 1.
Eigenvalues and Sums of Squared Loadings from Factor Analysis of all 28 Items (Principal Axis Factoring, Oblique Rotation, Delta = 0)
| Initial Eigenvalues |
Extraction Sum of Squared Loadings |
Rotation Sums of Squared Loadingsa |
|||||
|---|---|---|---|---|---|---|---|
| Factor | Total | % of Variance |
Cumulative % |
Total | % of Variance |
Cumulative % |
Total |
| 1 | 13.56 | 48.44 | 48.44 | 13.25 | 47.31 | 47.31 | 12.20 |
| 2 | 2.38 | 8.49 | 56.93 | 2.06 | 7.36 | 54.67 | 3.10 |
| 3 | 1.86 | 6.63 | 63.56 | 1.43 | 5.10 | 59.77 | 4.61 |
| 4 | 1.14 | 4.06 | 67.62 | 0.74 | 2.63 | 62.40 | 7.84 |
Note. Eigenvalues for all remaining factors were less than 1. Extraction Method: Principal Axis Factoring, n = 149. Kaiser-Meyer-Olkin Measure of Sampling Adequacy, 0.926. Bartlett’s Test of Sphericity; approximate chi-square 3624.534, df = 378, p < 0.001. Velicer’s MAP test indicated the number of components was 3. Parallel analysis indicated the number of components to be 4.
When factors are correlated, sums of squared loadings cannot be added to obtain a total variance.
Additional analyses suggest the models are a good fit. Sample size was more than adequate (KMO > .9), and the extracted factors are related to each other such that factor analysis was appropriate (Bartlett’s test of sphericity was significant, p < .05; Table 1). Item-level examination (Table 2) indicates that three items had low communality (<.4; Q9, Q12, Q4), and four items, if removed, increased Cronbach’s alpha (Q4, Q7, Q26, Q27). The pattern matrix (factor loadings) from the oblique rotation show that most items load onto Factor 1 or Factor 4 with only some of the items also loading onto Factors 2 and 3. Thus, the extracted factors do not explicitly represent the four subscales caused by their intercorrelations. Factor 1 was highly correlated with Factor 4 and Factor 3 (Table 3). Factor 2 was not highly correlated with any other factors and only had three items which had loadings greater than .4, two of which (Q7 and Q26) had low communality.
Table 2.
Factor Analysis Loadings and Reliability Results for all 28 Items
| Item | Communalities | Pattern Matrix Loadings |
Cronbach’s Alpha if Deleted |
|||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| Factor 1: Perceived Vulnerability | ||||||
| Q8: Human Papillomavirus (HPV) is a sexually transmitted disease. | .47 | .17 | .02 | .06 | .55 | .956 |
| Q9: Using condoms can prevent HPV. | .23 | .24 | .15 | .21 | .07 | .957 |
| Q10: Genital warts are caused by HPV. | .63 | .07 | .09 | .02 | .73 | .956 |
| Q11: People with HPV might not have symptoms. | .72 | .33 | −.02 | .32 | .43 | .954 |
| Q12: HPV makes you unable to have children. | .36 | .32 | .16 | .27 | .09 | .956 |
| Factor 2: Perceived Severity | ||||||
| Q13: I worry that my child may get HPV. | .51 | .41 | .17 | .03 | .32 | .955 |
| Q14: HPV can cause cervical cancer. | .84 | .61 | −.07 | .18 | .34 | .953 |
| Q15: Treatment for HPV is painful. | .29 | .37 | .02 | .15 | .14 | .957 |
| Q18: Required vaccinations protect children from getting disease from unvaccinated children. | .64 | .49 | −.10 | .31 | .23 | .955 |
| Q19: I understand exactly what the HPV vaccine is for. | .60 | .36 | −.15 | .16 | .44 | .955 |
| Q24: Having genital warts makes it very difficult to find a sexual partner. | .48 | .52 | .01 | .18 | .14 | .955 |
| Factor 3: Perceived Benefits | ||||||
| Q4: Children should only get vaccinated for serious diseases. | .33 | −.17 | −.06 | .54 | .19 | .960 |
| Q5: I am more likely to trust vaccinations that have been around awhile. | .73 | .45 | −.03 | .55 | .04 | .955 |
| Q6: Vaccinations are getting better all the time because of research. | .87 | .79 | −.08 | .11 | .18 | .953 |
| Q7: Healthy children do not need vaccinations. | .80 | −.09 | .90 | .04 | .01 | .958 |
| Q20: A vaccine against HPV could prevent future problems for my child. | .83 | .74 | −.13 | .18 | .17 | .954 |
| Q21: Giving my child a new vaccine is like performing an experiment on them. | .53 | .22 | .14 | .57 | .02 | .956 |
| Q22: Most people I know think vaccinating children with the HPV vaccine before they are teenagers is a good idea. | .70 | .95 | .03 | −.11 | −.19 | .955 |
| Q23: A teenager should be able to get a vaccination for HPV without a parent’s consent. | .59 | .09 | .59 | −.16 | .41 | .957 |
| Factor 4: Perceived Barriers | ||||||
| Q16: I would vaccinate my daughter with the HPV vaccine if it were free or at a very low cost. | .84 | .87 | −.02 | −.02 | .08 | .954 |
| Q17: I would vaccinate my daughter with the HPV vaccine if she could get it at school. | .68 | .64 | .27 | −.21 | .20 | .955 |
| Q25: If this new HPV vaccine was available when my daughter was an infant I would have vaccinated my child. | .62 | .68 | .21 | −.16 | .12 | .955 |
| Q26: Shots are very painful for my child so I would rather not vaccinate her. | .67 | −.04 | .79 | .18 | −.09 | .958 |
| Q27: If the new HPV vaccine is not required, I will not vaccinate my daughter. | .55 | .09 | .33 | .64 | −.19 | .958 |
| Q28: I think that even if the vaccine is expensive I will be able to vaccinate my daughter. | .66 | .81 | .03 | .02 | −.01 | .955 |
| Q29: My closest friends are vaccinating their daughters with the HPV vaccine. | .58 | .81 | −.06 | −.07 | −.03 | .956 |
| Q30: Generally I do what my doctor recommends, so I would vaccinate my daughter. | .82 | .89 | .00 | −.02 | .03 | .954 |
| Q34: When I decide to get my daughter vaccinated I believe I will be able to get her vaccinated. In other words, I feel confident I can get my daughter vaccinated. | .91 | .77 | −.11 | .23 | .16 | .953 |
Note. n = 149, Cronbach’s alpha before item deletion = .957. Bold numbers indicate: communalities > .4, loadings > .4, and higher Cronbach’s alphas if item deleted.
Table 3.
Correlations and Cronbach’s Alphas of the Four PHPVS Factors
| Factor | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| (1) Perceived Vulnerability | .80 | |||
| (2) Perceived Severity | .24 | .89 | ||
| (3) Perceived Benefits | .33 | .15 | .85 | |
| (4) Perceived Barriers | .60 | .13 | .34 | .92 |
Note. Cronbach’s alpha for each factor is along the diagonal. PHPVS = Parental Human Papillomavirus Vaccine Survey.
Separate factor analysis and reliability statistics for each of the four theoretical subscales revealed that each had good reliability (Cronbach’s alpha > .8), moderate interitem correlations (average interitem correlation > .4), and mostly consisted of a single underlying factor (Table 4). The last two subscales, perceived benefits and perceived barriers, had up to two additional eigenvalues greater than 1 primarily because of items Q4, Q7 (benefits) and Q26, Q27 (barriers), which have already been described as having low communality and loading onto Factors 2 or 3 separate from most other items in the instrument. Overall, these results support acceptable reliability and internal consistency of the PHPVS for parents of girls.
Table 4.
Convergent Validity: Internal Consistency Statistics for Each of the Four Subscales
| Perceived Vulnerability |
Perceived Severity |
Perceived Benefits |
Perceived Barriers |
|
|---|---|---|---|---|
| Number of Items | 5 | 6 | 8 | 9 |
| Number of Subjects with Complete Data | 167 | 166 | 183 | 169 |
| Reliability | ||||
| Cronbach’s alpha (α) | .80 | .89 | .85 | .92 |
| Average inter-item correlation | .44 | .56 | .41 | .53 |
| Range of inter-item correlations | .27–.63 | .41–.76 | .04–.89 | .14–.91 |
| α increase if item deleted | .80 (Q9) | .89 (Q15) | .88 (Q4) .86 (Q7) |
.93 (Q26) .93 (Q27) |
| Factor Analysis | ||||
| Number of eigenvalues >1 | 1 | 1 | 3 | 2 |
| % variance explained by 1st factor | 45.49% | 57.48% | 47.07% | 58.90% |
| Number of components indicated by MAP test | 1 | 1 | 1 | 1 |
| Number of factors indicated by PA | 1 | 1 | 3 | 2 |
| KMO Measure of Sampling Adequacy | .75 | .88 | .82 | .88 |
| Bartlett’s Test of Sphericity |
x2 = 268.60, df = 10, p < .001 |
x2 = 529.00, df = 1 5, p < .001 |
x2 = 881.84, df = 28, p < .001 |
x2 = 1304.65, df = 36, p < .001 |
DISCUSSION
Data obtained from classical item analysis and EFA provide evidence that the PHPVS is a reliable measure of HPV knowledge, attitudes, and intent to vaccinate in parents of girls. This study also provides evidence that the PHPVS may be a valid measure of four unidimensional constructs (perceived severity, perceived vulnerability, perceived benefits, and perceived barriers) associated with a desired health behavior such as HPV vaccination. The findings from this analysis support the internal consistency, internal validity, and reliability of the PHPVS. Further, the psychometric testing also provides an analysis of the items included in the four subscales. Analysis of survey items is important to intervention development because each subscale correlates with a theoretical construct of the HBM. Findings from an examination of survey responses in each subscale can then guide researchers to specific points of intervention to increase HPV vaccination knowledge for parents and identity barriers to HPV vaccination.
An example of this application would be the use of responses to items assessing perceived barriers from parents experiencing health disparities. These responses would or could be used to address parents’ perceived and actual barriers to HPV vaccination for their children. Once identified, the barriers can be addressed or removed using interventions built on data from a validated instrument that is theoretically based. The identified outcome would hypothetically be the increase in HPV vaccination rates among the children or adolescents of these parents who are experiencing health disparities. The PHPVS’ basis on HBM theoretical constructs allows for the provision of empirical evidence to support health promotion research and subsequent interventions. This contribution of the PHPVS is important because HPV vaccination is essential to maintaining the normal line of defense as a protective buffer against the stressors of chronic disease such as HPV-related cancers, which are increasing in African American and Latina populations (Fawcett & Gigliotti, 2001; Kobetz et al., 2010).
An additional example for the use of PHPVS data would be to understand parents’ perceived severity of HPV-related cancer. Correlational data between item responses on the PHPVS’ Perceived Severity subscale and demographic items can then help identify populations who might benefit from cancer prevention education the most—and more specifically education about prevention of HPV transmission through vaccination. Because there are no similar instruments available, external validity must be addressed in the future with additional studies.
In 2010, the HPV vaccine was approved for boys and the PHPVS was then adapted for use in parents with boys by substituting the word daughter for son. Because this time, the PHPVS has been used in research studies by parents of both girls and boys. It is hoped that the PHPVS—a psychometrically evaluated survey that is theoretically based, concise, and simple to use with parents and caregivers—can also be used to address HPV vaccination in other populations of children and adolescents with low vaccination rates. Nurse researchers, as well as clinicians, now have an instrument for use in health promotion research to provide insights into educational gaps in knowledge, points for intervention development, and future areas for nursing research.
In primary care settings, nurses can use this survey to rapidly evaluate parental knowledge about HPV infection, transmission, and vaccination. When using the PHPVS in a clinical setting, the 5-point Likert scale may be exchanged for a dichotomous Yes–No scale in which Yes = 5 and No = 0. When using either response scale, the nurse should equate a higher score, totaling to 100 or more, to indicate a high level of knowledge and understanding. Likewise, a score lower than 25 would imply little or no understanding, and scores between 26 and 100 would indicate opportunities and areas for further education and guidance. The nurse in a primary care practice can easily identify these specific opportunities for education by noting which section of the PHPVS has the lower scores. The nurse in clinical practice can then modify education or refine specific clinic protocols to increase HPV vaccination. Furthermore, it is possible that the use of the PHPVS in nursing research can inform nursing practice and impact health policy while guiding the development and evaluation of culturally specific interventions, educational programs, and research as other tools have done. Nurse researchers and practicing nurses now have a survey they can use to evaluate parents’ perceived vulnerability, perceived severity, perceived benefits, and perceived barriers to vaccinating their children with the HPV vaccine. In addition, the use of the PHPVS could provide nurses and nurse practitioners in primary care clinics important screening information to educate parents and evaluate parents’ readiness to consent for the initiation of their child’s HPV vaccine series.
LIMITATIONS
There was no external survey to validate against because this was the first survey developed of its kind in 2007, but, using a convergent and discriminate validation approach, we feel the tool is acceptable (Campbell & Fiske, 1959; Waltz, Strickland, & Lenz, 2005). Because of the specific nature of the current descriptive research and use of the survey, test–retest reliability is not applicable at this time.
CONCLUSIONS
Parents with elementary and middle school children are aware of many mandatory vaccines that protect their children from disease, such as the hepatitis B vaccine and polio vaccine, and the HPV vaccine has recently come on the scene as a recommended vaccine for cancer prevention. The PHPVS pilots have yielded information about the understandability, health literacy, and social acceptability of a survey that can be exported for use in larger community-based intervention studies and in health care settings.
Acknowledgments
The authors gratefully acknowledge the cooperation and support of the school officials, community leaders, and parents of Miami-Dade county, Florida, and Burke, Lincoln, and Screven counties, Georgia.
Contributor Information
Tami Lynn Thomas, Emory University.
Ora L. Strickland, Florida International University.
Ralph DiClemente, Emory University.
Melinda Higgins, Emory University.
Bryan Williams, Emory University.
Kathleen Hickey, Columbia University.
REFERENCES
- Campbell DT, Fiske DW. Convergent and discriminant validation by the multivariate-multimethod matrix. Psychological Bulletin. 1959;56(2):81–105. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. FDA licensure of quadrivalent human papillomavirus vaccine (HPV4, Gardasil) for use in males and guidance from the Advisory Committee on Immunization Practices (ACIP) MMWR Morbidity and Mortality Weekly Report. 2010;59(20):630–632. [PubMed] [Google Scholar]
- Chaturvedi AK. Beyond cervical cancer: Burden of other HPV-related cancers among men and women. Journal of Adolescent Health. 2010;46(Suppl. 4):S20–S26. doi: 10.1016/j.jadohealth.2010.01.016. http://dx.doi.org/10.1016/j.jadohealth.2010.01.016. [DOI] [PubMed] [Google Scholar]
- Dempsey AF, Zimet GD, Davis RL, Koutsky L. Factors that are associated with parental acceptance of human papillomavirus vaccines: A randomized intervention study of written information about HPV. Pediatrics. 2006;5(117):1486–1493. doi: 10.1542/peds.2005-1381. [DOI] [PubMed] [Google Scholar]
- Eisenberg ME, Bearinger LH, Sieving RE, Swain C, Resnick MD. Parents’ beliefs about condoms and oral contraceptives: Are they medically accurate? Perspectives on Sexual and Reproductive Health. 2004;36(2):50–57. doi: 10.1363/psrh.36.50.04. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Gigliotti E. Using conceptual models of nursing to guide nursing research: The case of the Neuman systems model. Nursing Science Quarterly. 2001;14(4):339–345. doi: 10.1177/089431840101400411. [DOI] [PubMed] [Google Scholar]
- Fernández ME, Diamond PM, Rakowski W, Gonzales A, Tortolero-Luna G, Williams J, Morales-Campos DY. Development and validation of a cervical cancer screening self-efficacy scale for low-income Mexican American women. Cancer Epidemiology Biomarkers & Prevention. 2009;18(3):866–875. doi: 10.1158/1055-9965.EPI-07-2950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field A. Discovering statistics using SPSS. 3rd ed. London, England: Sage; 2009. [Google Scholar]
- Foster PH. Use of stigma, fear, and denial in development of a framework for prevention of HIV/AIDS in rural African American communities. Family & Community Health. 2007;30(4):318–327. doi: 10.1097/01.FCH.0000290544.48576.01. [DOI] [PubMed] [Google Scholar]
- Gerend M, Shepherd J. Predicting human papillomavirus vaccine uptake in young adult women: Comparing the health belief model and theory of planned behavior. Annals of Behavioral Medicine. 2012:1–10. doi: 10.1007/s12160-012-9366-5. http://dx.doi.org/10.1007/s12160-012-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guvenc G, Akyuz A, Açikel CH. Health belief model scale for cervical cancer and pap smear test: Psychometric testing. Journal of Advanced Nursing. 2011;67(2):428–437. doi: 10.1111/j.1365-2648.2010.05450.x. http://dx.doi.org/10.1111/j.1365-2648.2010.05450.x. [DOI] [PubMed] [Google Scholar]
- Harper DM, Franco EL, Wheeler CM, Moscicki AB, Romanowski B, Roteli-Martins CM, Dubin G. HPV vaccine study group: Sustained efficacy up to 4.5 years of a bivalent L1 virus-like particle vaccine against human papillomavirus types 16 and 18: Follow-up from a randomized controlled trial. Lancet. 2006;367(9518):1247–1255. doi: 10.1016/S0140-6736(06)68439-0. [DOI] [PubMed] [Google Scholar]
- Harrison JA, Mullen PD, Green LW. A meta-analysis of studies of the health belief model with adults. Health Education Research. 1992;7(1):107–116. doi: 10.1093/her/7.1.107. [DOI] [PubMed] [Google Scholar]
- Hofferth SL, Kahn JR, Baldwin W. Premarital sexual activity among U.S. teenage women over the past three decades. Family Planning Perspectives. 1987;19:46–53. [PubMed] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY: Author; 2010. [Google Scholar]
- Kahn JA, Rosenthal SL, Jin Y, Huang B, Namakydoust A, Zimet GD. Rates of human papillomavirus vaccination, attitudes about vaccination, and human papillomavirus prevalence in young women. Obstetrics & Gynecology. 2008;111(5):1103–1110. doi: 10.1097/AOG.0b013e31817051fa. [DOI] [PubMed] [Google Scholar]
- Kobetz E, Dunn Mendoza A, Menard J, Finney Rutten L, Diem J, Barton B, McKenzie N. One size does not fit all: Differences in HPV knowledge between Haitian and African American women. Cancer Epidemiology Biomarkers & Prevention. 2010;19(2):366–370. doi: 10.1158/1055-9965.EPI-09-1180. http://dx.doi.org/10.1158/1055-9965.EPI-09-1180. [DOI] [PubMed] [Google Scholar]
- Marlow LAV, Waller J, Evans REC, Wardle J. Predictors of interest in HPV vaccination: A study of British adolescents. Vaccine. 2009;27(18):2483–2488. doi: 10.1016/j.vaccine.2009.02.057. http://dx.doi.org/10.1016/j.vaccine.2009.02.057. [DOI] [PubMed] [Google Scholar]
- McKee DM, Karasz A. You have to give her that confidence: Conversations about sex in Hispanic mother-daughter dyads. Journal of Adolescent Research. 2006;2(21):158–184. [Google Scholar]
- McRee A-L, Brewer NT, Reiter PL, Gottlieb SL, Smith JS. The Carolina HPV immunization attitudes and beliefs scale (CHIAS): Scale development and associations with intentions to vaccinate. Sexually Transmitted Diseases. 2010;37(4):234–239. doi: 10.1097/OLQ.0b013e3181c37e15. [DOI] [PubMed] [Google Scholar]
- Moseley KL, Freed GL, Bullard CM, Goold SD. Measuring African-American parents’ cultural mistrust while in a healthcare setting: A pilot study. Journal of the National Medical Association. 2007;99(1):15–21. [PMC free article] [PubMed] [Google Scholar]
- Neuman B. Health as a continuum based on the Neuman systems model. Nursing Science Quarterly. 1990;3(3):129–135. doi: 10.1177/089431849000300308. [DOI] [PubMed] [Google Scholar]
- Neuman B. The Neuman systems model in research and practice. Nursing Science Quarterly. 1996;9(2):67–70. doi: 10.1177/089431849600900207. [DOI] [PubMed] [Google Scholar]
- O’Connor B. SPSS and SAS programs for determining the number of components using parallel analysis and Velicer’s MAP test. Behavior Research Methods. 2000;32(3):396–402. doi: 10.3758/bf03200807. http://dx.doi.org/10.3758/bf03200807. [DOI] [PubMed] [Google Scholar]
- O’Sullivan LF, Meyer-Balhburg HF, Watkins BX. Social cognitions associated with pubertal development in a sample of urban, low-income, African-American and Latina girls and mothers. Journal of Adolescent Health. 2000;4(27):227–235. doi: 10.1016/s1054-139x(99)00111-1. [DOI] [PubMed] [Google Scholar]
- Parkin DM, Bray F. Chapter 2: The burden of HPV-related cancers. Vaccine. 2006;24(Suppl. 3):11–25. doi: 10.1016/j.vaccine.2006.05.111. http://dx.doi.org/10.1016/j.vaccine.2006.05.111. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. Patients’ compliance with health regimens. The Journal of the American Medical Association. 1975;234(4):402–403. [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Education Quarterly. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Shafii T, Stovel K, Davis R, Holmes K. Is condom use habit forming? Condom use at sexual debut and subsequent condom use. Sexually Transmitted Disease. 2004;31(6):366–372. doi: 10.1097/00007435-200406000-00010. [DOI] [PubMed] [Google Scholar]
- Stapleton CD. Basic concepts in exploratory factor analysis (efa) as a tool to evaluate score validity: A right-brained approach. Paper presented at The Annual Meeting of the Southeast Educational Research Association; Austin, TX. 1997. [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. London, UK: Pearson Education; 2007. [Google Scholar]
- Thomas TL. The new human papillomavirus (HPV) vaccine: Pros and cons for pediatric and adolescent health. Pediatric Nursing. 2008;34(5):429–431. [PubMed] [Google Scholar]
- Villarruel AM, Bishop TL, Simpson EM, Jemmott LS, Fawcett J. Borrowed theories, shared theories, and the advancement of nursing knowledge. Nursing Science Quarterly. 2001;14(2):158–163. doi: 10.1177/08943180122108210. [DOI] [PubMed] [Google Scholar]
- Waltz FW, Strickland O, Lenz ER. Measurement in nursing and health research. 3rd ed. New York, NY: Springer Publishing; 2005. [Google Scholar]
- Yanai H, Ichikawa M. Factor analysis. In: Rao CR, Sinharay S, editors. Handbook of statistics. Vol. 26. Amsterdam, Netherlands: Elsevier; 2006. pp. 257–296. [Google Scholar]
- Zimet GD, Fortenberry JD, Fife KH, Tyring SK, Herne K, Douglas JM. Acceptability of genital herpes immunization: The role of health beliefs and health behaviors. Sexually Transmitted Diseases. 1997;10(24):555–560. doi: 10.1097/00007435-199711000-00001. [DOI] [PubMed] [Google Scholar]
- Zimet GD, Kee R, Winston Y, Perkins SM, Maharry K. Acceptance of hepatitis B vaccination among adult patients with sexually transmitted diseases. Sexually Transmitted Diseases. 2001;28(11):678–680. doi: 10.1097/00007435-200111000-00011. [DOI] [PubMed] [Google Scholar]
- Zimet GD, Perkins SM, Sturm LA, Bair RM, Juliar BE, Mays RM. Predictors of STI vaccine acceptability among parents and their adolescent children. The Journal of Adolescent Health. 2005;37(3):179–186. doi: 10.1016/j.jadohealth.2005.06.004. [DOI] [PubMed] [Google Scholar]
- Zwick WR, Velicer WF. Comparison of five rules for determining the number of components to retain. Psychological Bulletin. 1986;99(3):432–442. http://dx.doi.org/10.1037/0033-2909.99.3.432. [Google Scholar]