Abstract
Purpose
To identify predictors of human papillomavirus (HPV) vaccination among rural African American families.
Design
Cross-sectional descriptive study in schools in three rural counties in southeastern United States. The sample consisted of African American parents or caregivers with children 9 to 13 years of age who attended elementary or middle school in 2010–2011.
Methods
Using an anonymous, 26-item survey, we collected descriptive data during parent-teacher events from African American parents with children in elementary or middle school. The main outcome was measured as a response of “yes” to the statement “I have or will vaccinate my child with the HPV vaccine.” In addition, composite scores of knowledge and positive attitudes and beliefs were compared. No interventions were conducted.
Findings
We identified predictors of HPV vaccination and found that religious affiliation had a correlation with vaccinating or planning to vaccinate a child.
Conclusions
Results indicate a need for further research on the role of local culture, including religion and faith, in rural African Americans’ decisions about giving their children the HPV vaccination.
Clinical Relevance
This study emphasizes the importance of understanding rural African American parents’ knowledge, attitudes, and spiritual beliefs when designing health education programs and public health interventions to increase HPV vaccination uptake among African American boys and girls living in rural areas.
Keywords: Human papillomavirus vaccination, African American, parents, consent, health disparities, rural health
The Centers for Disease Control and Prevention (CDC) reports that certain strands of the Human Papillomavirus (HPV) are responsible for nearly 99% of cervical cancer cases and at least 20% of cancers of the head, neck, and anogenital areas (CDC, 2011b). The HPV vaccine can prevent many of these cancers if it is given to children at the recommended age of 11 to 12 years, and its safety and efficacy have been evaluated by both the CDC and the Food and Drug Administration (FDA; Paavonen et al., 2009). In June 2006, the FDA approved the vaccine for girls and then subsequently approved the vaccination for boys in 2010 (FDA, 2006, 2010). The Advisory Committee on Immunization Practices (ACIP) followed in October 2011 with the recommendations to vaccinate both girls and boys starting at age 11 to prevent the ever-increasing prevalence of HPV infection (Elbasha & Dasbach, 2010; Ferris, Horn, & Waller, 2010; Smith, Gilbert, Melendy, Rana, & Pimenta, 2011). Further, the CDC notes that, in rural Georgia, female completion rates for the HPV series are less than 18% and much lower than national rates (CDC, 2011a; Chou, Krill, Horton, Barat, & Trimble, 2011; Dempsey, Cohn, Dalton, & Ruffin, 2011; Jain et al., 2009). Recent research among U.S. men reveals that as few as 2% of males have received a dose of the HPV vaccine, and this number is likely to be even lower in rural areas (Reiter, McRee, Kadis, & Brewer, 2011). The findings imply that, in rural areas, the need for education on HPV transmission and the HPV vaccine is greater than first recognized (Rosenthal et al., 2008; Schluterman, Terplan, Lydecker, & Tracy, 2011).
Early on, when the vaccine was first introduced for girls in 2006, controversies arose regarding the effects HPV vaccination might have on young girls, specifically, that it would cause promiscuity and a financial burden due the cost associated with the three-shot series, approximately $360 in total (Charo, 2007; Thomas, 2008).
Among African American women and Latina immigrants who reside in urban areas, researchers found that African American women were more skeptical about the HPV vaccine than Latinas (Constantine & Jerman, 2007). Similarly, African American men know less about HPV infection and vaccination than Hispanics and non-Hispanic Whites (Daley et al., 2011). A study of African American parents’ and daughters’ acceptance of HPV implied that acceptance was low and related to sexual activity (Read, Joseph, Polishchuk, & Suss, 2010). The same study showed that knowledge of HPV and the HPV vaccine were significantly associated with parents’ interest in having their daughters vaccinated (Read et al., 2010). When parents understood the significance of HPV vaccination (cancer prevention) and that the reason for starting the series early was to elicit the best immune response, then an increased interest in having their child vaccinated occurred. The challenge of vaccine cost has been addressed, and the vaccine is now covered under the Vaccines For Children (VFC) program, with a maximum charge of $14.81 in Georgia, where this study was conducted (CDC, 2011c; Georgia Department of Public Health [GADPH], 2012).
Understanding parental perceptions about the HPV vaccine is key to increasing vaccine rates, which are significantly lower among children from minority groups and children living in rural areas (Bynum et al., 2011). Currently, parental opinions on the HPV vaccine vary from one racial or ethnic group to another in rural areas, but frequently all ethnic groups had little access to HPV-related information (GADPH, 2012; Thomas, Strickland, DiClemente & Higgins, in press). This situation is particularly true for African Americans living in rural areas because the information that is available does not sufficiently describe the benefits of HPV vaccination in a way that overcomes fears and misperceptions (Cates, Brewer, Fazekas, Mitchell, & Smith, 2009). The need to vaccinate African Americans is particularly great because research findings indicate that African American adolescents take sexual risks at much higher rates than their White or Hispanic counterparts (Aral, Adimora, & Fenton, 2008). Moreover, rates of HPV-related cancers in rural areas are rarely researched, and there are limited data on rural populations by which to calculate the incidence of HPV-related cancers and cancer-related mortality (Lengerich et al., 2005). However, what we do know is that poverty and consequent health disparities contribute to higher rates of chronic disease in rural areas (“Management of clusters of sexually transmitted infection,” 2000).
Many studies that focus on HPV vaccination were done in urban areas with participants who receive their medical care at clinics. The few studies that were done in rural areas focused only on young women and their acceptance of HPV vaccination or their decision to take a free vaccine (Brewer & Fazekas, 2007; Dempsey, Zimet, Davis, & Koutsky, 2006; Rosenthal et al., 2008). New findings reveal ethnic disparities in HPV vaccination among women and no association between HPV vaccination and high-risk sexual behavior (Liddon, Leichliter, & Markowitz, 2012). Few, if any, studies focused on parents with children, either boys or girls, 9 to 13 years of age. In addition, the Health Belief Model (HBM), while used in other vaccine research, had not been used as a theoretical framework in early HPV vaccine research, so both the measures and analysis were guided by these constructs to determine perceived vulnerability, perceived severity, perceived benefits, and perceived barriers to HPV vaccination for African American parents residing in rural Georgia (Rosenstock, Strecher, & Becker, 1988).
This study’s objectives were (a) to determine the correlates of HPV vaccination among children of African American parents residing in rural areas and (b) to find culturally specific points of intervention that would increase HPV vaccination rates among children in rural African American communities.
Materials and Methods
Design and Sample
We used a descriptive cross-sectional design and quantitative methods to collect data on predictors of HPV vaccination in three counties of rural Georgia. The study population was parents with children 9 to 13 years of age who attended elementary or middle schools with at least a 50% African American student population during the 2010–2011 school year. The study’s sample size was based on the number of students who were enrolled in the counties’ schools and who came from households with low median incomes. There were no refusals, and the convenience sample of African American parents total N was 400.
Study Procedures
School superintendents in the selected counties understood this study’s importance for their communities and complied with the Family Educational Rights and Privacy Act. Before the study was implemented, the principal investigator (PI) met with the superintendents, each school principal, and school clerical staff to explain the study procedures, and written letters of support were given to the PI. The PI supplied the schools with a letter to be sent to parents. This letter included the study’s purpose, the use of an individual access code to avoid fraud, a description of the incentive for participating (a $50.00 gift card), the PI’s contact information, a description of the study, and information about Emory University’s methods for protecting the privacy of human study subjects. At prearranged school events, parents read the information letter, gave informed consent, and were asked to complete an anonymous survey with the choice of either completing the survey by pen and paper or on a secure laptop computer.
Measures
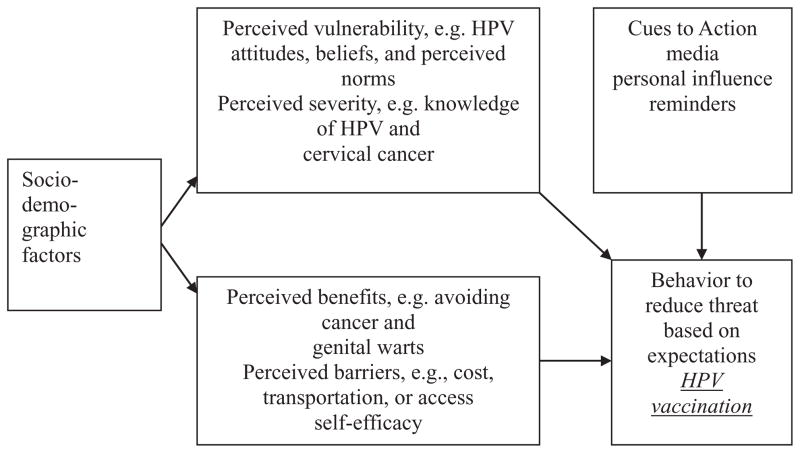
Measurement was guided by the HBM (Figure 1), which identifies correlates of health-related behavior and posits four factors to account for the behavior: perceived vulnerability, perceived severity, perceived benefits, and perceived barriers. The Parental HPV Survey (PHPVS), which contains 26 dichotomous items, was developed by the PI to map onto the HBM survey items specific to a HPV vaccination, and validity testing has confirmed the PHPVS factor structure: perceived vulnerability (five items), perceived severity (six items), perceived benefits (eight items), and perceived barriers (six items) demonstrate reliability, with Cronbach α ranging from .80 to .92 (Thomas, Strickland, DiClemente, Williams, Higgins & Hickey, in press).
Figure 1.
Health Belief Model as applied to human papillomavirus (HPV) vaccination uptake.
The main outcome variable, vaccine uptake, was measured by one survey item, which asked parents and guardians whether they have vaccinated or will vaccinate their child (boys and girls 9–13 years of age). Each of the four HBM factors were examined as potential predictors, and parental knowledge and parental attitude composite scores were computed to determine which constructs correlated with the decision to vaccinate a son or daughter against HPV.
Statistical Analysis
Analyses were performed using SPSS 19 (SPSS Inc., Chicago, IL, USA) and SAS 9.2 (SAS Institute Inc., Cary, NY, USA). Statistical significance was assessed at an alpha level of 0.05. Before being analyzed, all data were reviewed for normality and possible outliers. Summary statistics were generated for each variable of interest across participants and by intention to vaccinate (yes or no). Total scores were calculated for the four scales of the PHPVS, a psychometrically validated instrument (Thomas, Strickland, DiClemente, Williams, Higgins, & Hickey, in press). Each scale was calculated as the percentage of items marked “agree” out of the total number of items in each scale; each scale ranged from 0 to 100%, with higher scores indicating greater perceived vulnerability, severity, benefits, and barriers. Comparison tests between the three counties were performed using chi-square tests and analysis of variance F tests. Logistical regression was used to analyze the aforementioned predictor variables after controlling for potential covariates defined as variables related to intent to vaccinate, with p < .2. Regarding power analysis, after adjusting for parent’s religion, perceived vulnerability and perceived barriers entered the model in block 2 (χ2 [df = 2] = 12.85, p = .002, n = 392, observed power = 90.4%.
Results
Four hundred African American parents were surveyed from three rural Georgia counties: 143 (36%) from Burke, 144 from Screven (36%), and 113 (28%) from Lincoln (Table 1). Most surveyed parents were female (80.0%), Baptist (84.2%), and had at least one female child (76.5%) in their household (Table 2). Slightly more than half of the parents (51.1%) were married or in a long-term relationship. Annual household income was less than $15,000 for 31.7% of the sample, $15,000 to $30,000 for 35.8%, and greater than $30,000 for 32.5%. The mean parental age was 40.7 years (SD = 10.30), with a mean age for their children of 11.39 years (SD = 1.52; Table 3). Parents who intended to vaccinate their children were significantly non-Baptist, χ2 ([df = 1], n = 392) = 34.35, p < .001. Parents who intended to vaccinate their children also had higher levels of education, χ2 ([df = 1], n = 393) = 3.83, p = .050. Rates of the main outcome variable, intention to vaccinate, were significantly different across the three counties (p < .01), with the highest rate of 40.8% in Burke County, which had significantly fewer Baptists (p < .01) and significantly more married parents (p < .05). Counties also had significantly different rates by survey parent’s gender, child’s gender, and parent’s education level when compared with each other, and these same county distinctions were noted in the rates of HPV vaccination. Rates of the main outcome variable, intention to vaccinate, were significantly different across the three counties (p < .01), with the highest rate of 40.8% in Burke County, which had significantly fewer Baptists (p < .01) and significantly more married parents (p < .05; Table 4). Counties also had significantly different rates by survey parent’s gender, child’s gender, and parent’s education level when compared with each other, and these same county distinctions were noted in the rates of HPV vaccination.
Table 1.
Enrollment and Parental Human Papillomavirus Vaccine Survey (PHPVS) Completion
| County | Enrollment | Surveys completed | African Americans (% African Americans of complete surveys) |
|---|---|---|---|
| Burke | 780 | 230 | 143 (62.2%) |
| Screven | 380 | 176 | 144 (81.8%) |
| Lincoln | 307 | 113 | 113 (100%) |
| Totals | 1,467 | 519 | 400 |
Note. This study focuses on the 400 African Americans who completed the PHPVS.
Table 2.
Categorical/Ordinal Demographic Summaries Overall and Differences by Intent to Vaccinate
| Categorical/ordinal data | All participants Summary
|
Intent to vaccinate
|
Test between vaccinate no/yes participants
|
|||||
|---|---|---|---|---|---|---|---|---|
| No
|
Yes
|
Chi-square df = 1, p-value | Odds ratio (reference category) [95% CI] | |||||
| n | % | n | Row% | n | Row% | |||
| Parent gender | 1.69, p = .19 | 1.48 (Female) [0.82, 2.66] | ||||||
| Male | 79 | 20.0% | 62 | 78.5% | 17 | 21.5% | ||
| Female | 316 | 80.0% | 225 | 71.2% | 91 | 28.8% | ||
| Child gender | 0.14 p = .70, | 0.90 (Female) [0.53, 1.53] | ||||||
| Male | 93 | 23.5% | 69 | 74.2% | 24 | 25.8% | ||
| Female | 302 | 76.5% | 218 | 72.2% | 84 | 27.8% | ||
| Religion | 34.35, p < .001 | 0.20 (Baptist) [0.11, 0.36] | ||||||
| Baptist | 330 | 84.2% | 258 | 78.2% | 72 | 21.8% | ||
| Other | 62 | 15.8% | 26 | 41.9% | 36 | 58.1% | ||
| Education level | 3.83, p = .050 | 1.58 (some college+) [0.997, 2.51] | ||||||
| Some high school & high school | 266 | 67.7% | 201 | 75.6% | 65 | 24.4% | ||
| Some college, bachelor’s, master’s degree, and above | 127 | 32.3% | 84 | 66.1% | 43 | 33.9% | ||
| Income level | 0.03, p = .86 (≤$30K vs. >$30K) | 0.96 (>$30K) [0.59, 1.54] | ||||||
| $15,000 or less | 122 | 31.7% | 85 | 69.7% | 37 | 30.3% | ||
| $15,000 to $30,000 | 138 | 35.8% | 102 | 73.9% | 36 | 26.1% | ||
| $30,000 to $45,000 | 67 | 17.4% | 54 | 80.6% | 13 | 19.4% | ||
| $45,000 to $60,000 | 30 | 7.8% | 16 | 53.3% | 14 | 46.7% | ||
| $60,000 and greater | 28 | 7.3% | 21 | 75.0% | 7 | 25.0% | ||
| Marital status | 0.25, p = .61 | 0.89 (married/LTR) [0.57, 1.39] | ||||||
| Married or long-term relationship (LTR) | 202 | 51.1% | 149 | 73.8% | 53 | 26.2% | ||
| Single, divorced, or widowed | 193 | 48.9% | 138 | 71.5% | 55 | 28.5% | ||
| Know someone who has had a sexually transmitted disease | 1.37, p = .24 | 0.75 (Yes) [0.47, 1.21] | ||||||
| Yes | 147 | 44.0% | 107 | 72.8% | 40 | 27.2% | ||
| No | 187 | 56.0% | 125 | 66.8% | 62 | 33.2% | ||
Note. CI = confidence interval.
Table 3.
Continuous Measures Summaries Overall and Differences by Intent to Vaccinate
| Continuous data | All participants Summary
|
Intent to vaccinate
|
Test between vaccinate no/yes participants
|
|||||
|---|---|---|---|---|---|---|---|---|
| No
|
Yes
|
t-test, p-value | Mean difference [95% CI] | |||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |||
| Parent’s age | 379 | 40.7 (10.3) | 269 | 40.9 (10.5) | 105 | 40.4 (9.9) | t = 0.42, p = .68 | 0.49 [−1.84, 2.83] |
| Child’s age | 327 | 11.4 (1.5) | 245 | 11.4 (1.5) | 81 | 11.4 (1.5) | t = 0.19, p = .85 | 0.04 [−0.35, 0.42] |
| Number of female children | 399 | 1.85 (1.0) | 286 | 1.83 (1.0) | 108 | 1.85 (1.1) | t = −0.20, p = .84 | −0.02 [−0.25, 0.21] |
| Number of male childrena | 399 | 1.0 (0.7) | 286 | 0.94 (0.6) | 108 | 1.1 (0.9) | t = −1.42, p = .16 | −0.14 [−0.33, 0.05] |
| Perceived vulnerability | 397 | 39.2 (30.9) | 284 | 42.0 (31.6) | 108 | 32.4 (28.2) | t = 2.77, p = .006 | 9.63 [2.80, 16.47] |
| Perceived severity | 399 | 44.5 (29.3) | 286 | 44.9 (29.7) | 108 | 43.7 (28.8) | t = 0.38, p = .71 | 1.26 [−5.29, 7.80] |
| Perceived benefits | 399 | 43.5 (25.6) | 286 | 44.2 (26.1) | 108 | 42.0 (24.7) | t = 0.76, p = .45 | 2.22 [−3.50, 7.93] |
| Perceived barriersa | 400 | 31.4 (23.9) | 287 | 28.6 (22.8) | 108 | 37.5 (25.3) | t = −3.21, p = .002 | −8.93 [−14.42, −3.44] |
Equal variances not met, unpooled t test performed.
Table 4.
Demographics Characteristics and Vaccination Rates by County
| Lincoln | Screven | Burke | χ2(df=2) | p | |
|---|---|---|---|---|---|
| HPV (% yes) | 8.0% | 29.3% | 40.8% | 34.657 | <.001 |
| Religion (% Baptist) | 100.0% | 79.6% | 76.1% | 30.454 | <.001 |
| Education (% HS or less) | 86.7% | 57.0% | 62.2% | 27.847 | <.001 |
| Income (% <$30K) | 72.1% | 64.7% | 66.4% | 1.608 | .447 |
| Marital status (%married or LTR) | 45.1% | 47.2% | 60.1% | 7.151 | .028 |
Note. HPV = human papillomavirus; HS = high school; LTR = long-term relationship.
The PHPVS yielded four subscores based on four constructs of the HBM: perceived vulnerability (including items on HPV knowledge), perceived severity (including items on HPV attitudes), perceived benefits, and perceived barriers. The average percentage of perceived severity (44.5%, SD = 29.3) and perceived benefits (43.5%, SD = 25.6) were similar, with no significant differences among the intend-to-vaccinate groups (see Table 3). However, parents who intended to vaccinate their children scored significantly lower on perceived vulnerability (p = .006) and higher on perceived barriers (p = .002; see Table 3). We strongly suspect this may be due to very low HPV knowledge about persistent HPV infection and the subsequent HPV-related cancers as cited in a larger study published elsewhere (Thomas, Strickland, DiClemente, & Higgins, in press).
Using logistic regression, potential demographic covariates (parent’s gender, religion, education, and number of male children per household with p < .20 from Tables 2 and 3) were adjusted in block 1, followed by the four PHPVS scales in block 2 as predictors of intention to vaccinate. Then, using forward likelihood ratio variable selection within each block, we found that only parent’s religion was significant (block 1, χ2 [df = 1] = 30.49, p < .001). However, after adjusting for parent’s religion, perceived vulnerability and perceived barriers entered the model in block 2 (χ2 [df = 2] = 12.85, p = .002). Non-Baptists were 3.6 times more likely to vaccinate. For every 1 point decrease in perceived vulnerability scores, the odds of vaccination increased 1.01 times, and for every 1 point increase in perceived barrier scores, the odds of vaccination increased 1.02 times (Table 5). Since religion was the most significant predictor of HPV, it is worth noting that religion was significantly associated with parent’s gender (χ2 [df = 1] = 8.910, p = .003; more women were non-Baptist), education (χ2 [df = 1] = 5.023, p = .003; higher educated parents were non-Baptist), and number of male children (t [df = 68] = 2.35, p = .02; non-Baptists had more male children per household).
Table 5.
Hierarchical Logistic Regression Analysis Predicting Human Papillomavirus
| Step and predictors | Block χ2(df) | p | SE | p | OR | 95% CI |
|---|---|---|---|---|---|---|
| Block 1 | 30.49(1) | <.001 | ||||
| Religion | .290 | <.001 | 4.904 | [2.778, 8.656] | ||
| Block 2 | 12.85(2) | .002 | ||||
| Religion | .304 | <.001 | 3.638 | [2.006, 6.596] | ||
| Perceived vulnerability | .004 | .007 | 0.988 | [0.980, 0.997] | ||
| Perceived barriers | .005 | .002 | 1.016 | [1.006, 1.027] |
Note. Final model χ2(3) = 43.335, p < .001, Nagelkerke R2 = .152, n = 389. SE = standard error; OR = odds ratio; CI = confidence interval.
Limitations
Only about 35% of the parents with children aged 9 to 13 enrolled in school participated in the study. Although results from a sample of 400 may not be generalized to all African American parents with children 9 to 13 years of age enrolled in elementary and middle schools, such a sample is representative of the rural African American parents living in the counties involved in this study.
Discussion
African Americans and the HPV Vaccine
The results from this study emphasize the importance of understanding rural African American parents’ perceived vulnerability, perceived severity, perceived benefits, and perceived barriers to HPV vaccination when designing health education programs and public health interventions to increase HPV vaccination uptake among African American boys and girls living in rural areas. The need to address cancer prevention education in rural areas is clear, but the complexities involved in educating parents must be addressed in the context of the local rural culture with community engagement. Findings imply several points of intervention: culture, religious affiliation, and parent education.
Culture
Findings from our study describe rural communities with low income, geographic challenges to access care, and large numbers of self-reported religious affiliation in a particular group, Baptist. Social demographics directly influence perceived vulnerability and severity as purported in the HBM (see Figure 1), and these sociodemographics comprise the local rural culture, including religious affiliation, in rural African Americans’ decisions about HPV vaccination for their children 9 to 13 years of age. Rural culture may impact not only accessing knowledge about healthcare innovations such as HPV vaccination but also access to care. Local culture shapes people’s perceptions of risk or perceived vulnerability; people assign value (either positive or negative) to an issue on the basis of their experience, and they trust experts who have cultural backgrounds similar to their own (Kahan, Braman, Cohen, Gastil, & Slovic, 2010). Studies in rural areas outside Georgia imply that focusing on norms in an individual’s cultural population may be more effective than other approaches to intervention development (Lechuga, Swain, & Weinhardt, 2011).
Thus, we believe that describing and understanding cultural norms (e.g., level of religiosity and spirituality, parenting views, etc.) is essential in the development of interventions to increase HPV vaccination rates in these rural communities because culture cognition theory implies that people will accept or reject information about risk (perceived vulnerability and perceived severity) in a way that fits their cultural values, beliefs, or spirituality (Kahan, Braman, Slovic, Gastil, & Cohen, 2009). In this manner, perceived vulnerability and perceived severity varies among cultural groups. This was evident in each rural county in Georgia where we conducted our study: each county seemed unique, with a large portion of the variance in results attributed to perceived vulnerability and perceived severity ascribed to membership in cultural subgroups integral to individual identity such as, race, gender, parenting norm, social norms, and religious affiliation (Kahan & Braman, 2006; Slovic, 2000). And, indeed, a large body of research supports that culture has a greater effect on perceived vulnerability (risk perception) than education or socioeconomic status (Drake, 1991; Ellis & Thompson, 1997; Jenkins-Smith, 2001; Kahan, Braman, Gastil, Slovic, & Mertz, 2007; Peters, Burraston, & Mertz, 2004; Teitelman et al., 2011).
Religious Affiliation
Among participants in our study, religious affiliation had a correlation with vaccinating or planning to vaccinate a child 9 to 13 years of age. This is a significant finding, since religion and spirituality are integral components of sociodemographics (rural culture) and influence perceived vulnerability to HPV infection and perceived severity to HPV infection and subsequent HPV-related cancer. In addition, studies of the influence of religion on African Americans’ health-related behaviors found that rural church-going African Americans sometimes perceive illness as a punishment from God and sometimes believe that a person of strong faith can overcome illness (Holt et al., 2009). During our research we found a disconnection between people’s attitudes about faith and healing and their actual choice to vaccinate with the HPV vaccine. Those that designated themselves as “Baptist,” a reportedly conservative religion, reported high rates of HPV vaccination and intent to vaccinate, a finding that is similar to the finding of research conducted in rural areas of the Midwest (Gonnerman, Lutz, Yehieli, & Meisinger, 2008). Studies of African American perceptions about religion and the effect of being religious on health indicate that the following are important tenets of faith: belonging to the church family, giving problems over to God, and recognizing the body as a temple of God. Accepting these tenets results in physical well-being (Holt & McClure, 2006). In contrast, a 2009 study of young African American women attending a historically black university in the rural south found that a high level of spirituality and religiosity were not protective against sexual risk taking (Thomas & Freeman, 2011).
We cannot therefore assume that all African Americans living in rural areas are buffered against health risk behaviors because of the importance of religion and spirituality. Yet we must recognize the importance of the church and faith-based organizations in rural communities and consider their role in rural community life. The effect of pastors and churches on rural African Americans should not be underestimated (Foster, Arnold, Rebchook, & Kegeles, 2011). Parents in our study self-identified predominantly as Baptists, indicating that intervention developers must understand the religious tenets of these rural Baptist churches if they are to be successful in educating the parents there about the risks for HPV and the benefits of vaccination.
Parent Education
Low composite scores on perceived vulnerability and perceived severity from our participants imply that interventions must also function to educate parents by concentrating on HPV knowledge and including the connection between persistent HPV infection and related cancers in order to influence the desired behavior (HPV vaccination). Our findings substantiate results of one pilot study, completed 4 years after the HPV vaccine was approved in 2006, that indicated HPV vaccine acceptability alone does not always predict HPV vaccination among young African American women (Bynum et al., 2011). Results from our study imply that in this population of rural African American parents, both low knowledge of HPV vaccination and low level of perceived barriers could be attributed to the lack of knowledge about the connection between persistent HPV infection and HPV-related cancer (i.e., perceived severity of HPV infection). Increasing parents’ perceived severity of HPV infection, perceived vulnerability to HPV infection, and perceived benefits of HPV vaccination could promote HPV vaccine series initiation and completion. This is critically important in Burke, Screven, and Lincoln Counties, where the series completion rate is barely half the national average (Chou et al., 2011; Dempsey et al., 2011; Jain et al., 2009). The findings from national studies and our study imply that, in rural areas, the need for parent education about HPV, HPV transmission, and the HPV vaccine may be greater than first recognized (Rosenthal et al., 2008; Schluterman et al., 2011; Thomas, Strickland, DiClemente, & Higgins, in press).
Conclusions
The complexity and interaction of culture, economics, and rurality or urbanicity must be part of an integrated strategy to prevent HPV-related cancers. This study reveals several intervention points for future research. The most notable is to educate parents or caregivers about HPV-related cancers, HPV transmission, and HPV vaccination. Although HPV knowledge may be the first step in increasing HPV vaccination rates, other interventions such as increasing access to health care, reducing the cost of vaccination, and implementing school-based vaccine programs are also possibilities. Many rural communities included in this study had no pediatrician, and parents often had to drive more than 60 min to receive primary health care. Health care for children was provided by the local health department, which carried the HPV vaccine but had few or no requests to vaccinate children 9 to 13 years of age, when the HPV vaccine is most effective.
Recommendations based on our results include educating parents on the benefits of HPV vaccination, intervening in ways that respect the culture of rural communities (including religious and spiritual influences on personal health practices), having a policy to maintain vaccine programs in these rural counties, and increasing pediatric health services in these areas. Telemedicine and school-based clinics may serve to promote the latter in these rural counties.
Clinical Resources.
HPV and men – fact sheet: http://www.cdc.gov/std/hpv/stdfact-hpv-and-men.htm
Vaccines and Preventable Diseases: HPV vaccine –questions and answers: http://www.cdc.gov/vaccines/vpd-vac/hpv/vac-faqs.htm
Acknowledgments
This work was funded by the Robert Wood Johnson Foundation, ID # 67983.
References
- Aral SO, Adimora AA, Fenton KA. Understanding and responding to disparities in HIV and other sexually transmitted infections in African Americans. Lancet. 2008;372(9635):337–340. doi: 10.1016/S0140-6736(08)61118-6. [DOI] [PubMed] [Google Scholar]
- Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Preventive Medicine. 2007;45(2–3):107–114. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Bynum SA, Brandt HM, Annang L, Friedman DB, Tanner A, Sharpe PA. Do health beliefs, health care system distrust, and racial pride influence HPV vaccine acceptability among African American college females? Journal of Health Psychology. 2011;17(2):217–226. doi: 10.1177/1359105311412833. [DOI] [PubMed] [Google Scholar]
- Cates JR, Brewer NT, Fazekas KI, Mitchell CE, Smith JS. Racial differences in HPV knowledge, HPV vaccine acceptability, and related beliefs among rural, southern women. Journal of Rural Health. 2009;25(1):93–97. doi: 10.1111/j.1748-0361.2009.00204.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National and state vaccination coverage among adolescents aged 13 through 17 years– United States, 2010. Morbidity and Mortality Weekly Report. 2011a;60(33):1117–1123. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Vaccines for Children Program VFC: Federal Register. Vaccines & immunizations. 2011b Feb 28; Retrieved July 11, 2012, from http://www.cdc.gov/vaccines/programs/vfc/fee-fedreg.htm.
- Centers for Disease Control and Prevention. VFC: Federal Register. 2011c Retrieved July 11, 2012, from http://www.cdc.gov/vaccines/programs/vfc/fee-fedreg.htm.
- Charo RA. Politics, parents, and prophylaxis–Mandating HPV vaccination in the United States. New England Journal of Medicine. 2007;356(19):1905–1908. doi: 10.1056/NEJMp078054. [DOI] [PubMed] [Google Scholar]
- Chou B, Krill LS, Horton BB, Barat CE, Trimble CL. Disparities in human papillomavirus vaccine completion among vaccine initiators. Obstetrics and Gynecology. 2011;118(1):14–20. doi: 10.1097/AOG.0b013e318220ebf300006250-201107000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantine NA, Jerman P. Acceptance of human papillomavirus vaccination among Californian parents of daughters: A representative statewide analysis. Journal of Adolescent Health. 2007;40(2):108–115. doi: 10.1016/j.jadohealth.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Communicable disease report. Management of clusters of sexually transmitted infection. CDR Weekly. 2000;10(46):409–412. [PubMed] [Google Scholar]
- Daley EM, Marhefka S, Buhi E, Hernandez ND, Chandler R, Vamos C, Giuliano AR. Ethnic and racial differences in HPV knowledge and vaccine intentions among men receiving HPV test results. Vaccine. 2011;29(23):4013–4018. doi: 10.1016/j.vaccine.2011.03.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempsey A, Cohn L, Dalton V, Ruffin M. Worsening disparities in HPV vaccine utilization among 19–26 year old women. Vaccine. 2011;29(3):528–534. doi: 10.1016/j.vaccine.2010.10.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempsey AF, Zimet GD, Davis RL, Koutsky L. Factors that are associated with parental acceptance of human papillomavirus vaccines: A randomized intervention study of written information about HPV. Pediatrics. 2006;5(117):1486–1493. doi: 10.1542/peds.2005-1381. [DOI] [PubMed] [Google Scholar]
- Drake K. Orienting dispositions in the perception of risk– Analysis of contemporary worldviews and cultural biases. Journal of Cross-Cultural Psychology. 1991;22(1):61–82. [Google Scholar]
- Elbasha EH, Dasbach EJ. Impact of vaccinating boys and men against HPV in the United States. Vaccine. 2010;28(42):6858–6867. doi: 10.1016/j.vaccine.2010.08.030. [DOI] [PubMed] [Google Scholar]
- Ellis RJ, Thompson F. Culture and the environment in the Pacific Northwest. American Political Science Review. 1997;91(4):885–898. [Google Scholar]
- Ferris D, Horn L, Waller JL. Parental acceptance of a mandatory human papillomavirus (HPV) vaccination program. Journal of the American Board of Family Medicine. 2010;23(2):220–229. doi: 10.3122/jabfm.2010.02.090091. [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration. FDA licenses new vaccine for prevention of cervical cancer and other diseases in females caused by human papilloma virus. 2006 Retrieved from http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2006/ucm108666.htm.
- Food and Drug Administration. FDA licensure of quadrivalent human papilloma virus vaccine (HPV4, Gardasil) for use in males and guidance from the Advisory Committee on Immunization Practices (ACIP) MMWR Morbidity and Mortality Weekly Report. 2010;59(10):630–632. [PubMed] [Google Scholar]
- Foster ML, Arnold E, Rebchook G, Kegeles SM. “It’s my inner strength”: Spirituality, religion and HIV in the lives of young African American men who have sex with men. Culture, Health & Sexuality. 2011;13(9):1103–1117. doi: 10.1080/13691058.2011.600460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgia Department of Public Health. Vaccines for children. 2012 Retrieved July 11, 2012, from http://health.state.ga.us/programs/immunization/vfc/index.asp.
- Gonnerman ME, Jr, Lutz GM, Yehieli M, Meisinger BK. Religion and health connection: A study of African American, Protestant Christians. Journal of Health Care for the Poor and Underserved. 2008;19(1):193–199. doi: 10.1353/hpu.2008.0020. [DOI] [PubMed] [Google Scholar]
- Holt CL, Clark EM, Roth D, Crowther M, Kohler C, Fouad M, Southward PL. Development and validation of instruments to assess potential religion-health mechanisms in an African American population. Journal of Black Psychology. 2009;35(2):271–288. doi: 10.1177/0095798409333593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt CL, McClure SM. Perceptions of the religion-health connection among African American church members. Qualitative Health Research. 2006;16(2):268–281. doi: 10.1177/1049732305275634. [DOI] [PubMed] [Google Scholar]
- Jain N, Euler GL, Shefer A, Lu P, Yankey D, Markowitz L. Human papillomavirus (HPV) awareness and vaccination initiation among women in the United States, National Immunization Survey–Adult 2007. Preventive Medicine. 2009;48(5):426–431. doi: 10.1016/j.ypmed.2008.11.010. [DOI] [PubMed] [Google Scholar]
- Jenkins-Smith H. Modeling stigma: An empirical analysis of nuclear waste image of Nevada. In: Flynn J, Slovic P, Kunreuther H, editors. Risk, media and stigma: Understanding public challenges to modern science and technology. Sterling, VA: Earthscan; 2001. pp. 107–132. [Google Scholar]
- Kahan DM, Braman D. Cultural cognition and public policy. Law working paper No. 87. Yale Law & Policy Review. 2006;24:147. [Google Scholar]
- Kahan DM, Braman D, Cohen GL, Gastil J, Slovic P. Who fears the HPV vaccine, who doesn’t, and why? An experimental study of the mechanism of cultural cognition. Law and Human Behavior. 2010;34:501–516. doi: 10.1007/s10979-009-9201-0. [DOI] [PubMed] [Google Scholar]
- Kahan DM, Braman D, Gastil J, Slovic P, Mertz CK. Culture and identity-protective cognition: Explaining the white-male effect in risk perception. Journal of Empirical Legal Studies. 2007;4(3):465–505. [Google Scholar]
- Kahan DM, Braman D, Slovic P, Gastil J, Cohen GM. Cultural cognition of the risks and benefits of nanotechnology. Nature Nanotechnology. 2009;4(2):87–91. doi: 10.1038/nnano.2008.341. [DOI] [PubMed] [Google Scholar]
- Lechuga J, Swain GR, Weinhardt LS. The cross-cultural variation of predictors of human papillomavirus vaccination intentions. Journal of Women’s Health. 2011;20(2):225–230. doi: 10.1089/jwh.2010.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengerich EJ, Tucker TC, Powell RK, Colsher P, Lehman E, Ward AJ, Wyatt SW. Cancer incidence in Kentucky, Pennsylvania, and West Virginia: Disparities in Appalachia. Journal of Rural Health. 2005;21(1):39–47. doi: 10.1111/j.1748-0361.2005.tb00060.x. [DOI] [PubMed] [Google Scholar]
- Liddon NC, Leichliter JS, Markowitz LE. Human papillomavirus vaccine and sexual behavior among adolescent and young women. American Journal of Preventive Medicine. 2012;42(1):44–52. doi: 10.1016/j.amepre.2011.09.024. 10.1016/j.amepre. 2011.09.024. [DOI] [PubMed] [Google Scholar]
- Paavonen J, Naud P, Salmeron J, Wheeler CM, Chow SN, Apter D, Dubin G. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): Final analysis of a double-blind, randomised study in young women. Lancet. 2009;374(9686):301–314. doi: 10.1016/S0140-6736(09)61248-4. [DOI] [PubMed] [Google Scholar]
- Peters EM, Burraston B, Mertz CK. An emotion-based model of risk perception and stigma susceptibility: Cognitive appraisals of emotion, affective reactivity, worldviews, and risk perceptions in the generation of technology stigma. Risk Analysis. 2004;24(5):1349–1367. doi: 10.1111/j.0272-4332.2004.00531.x. [DOI] [PubMed] [Google Scholar]
- Read DS, Joseph MA, Polishchuk V, Suss AL. Attitudes and perceptions of the HPV vaccine in Caribbean and African-American adolescent girls and their parents. Journal of Pediatric and Adolescent Gynecology. 2010;23(4):242–245. doi: 10.1016/j.jpag.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Reiter PL, McRee AL, Kadis JA, Brewer NT. HPV vaccine and adolescent males. Vaccine. 2011;29(34):5595–5602. doi: 10.1016/j.vaccine.2011.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Education Quarterly. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Rosenthal SL, Rupp R, Zimet GD, Meza HM, Loza ML, Short MB. Uptake of HPV vaccine: Demographics, sexual history and values, parenting styles and vaccine attitudes. Journal of Adolescent Health. 2008;43(3):239–245. doi: 10.1016/j.jadohealth.2008.06.009. [DOI] [PubMed] [Google Scholar]
- Schluterman NH, Terplan M, Lydecker AD, Tracy JK. Human papillomavirus (HPV) vaccine uptake and completion at an urban hospital. Vaccine. 2011;29(21):3767–3772. doi: 10.1016/j.vaccine.2011.03.032. [DOI] [PubMed] [Google Scholar]
- Slovic P. The perception of risk. Sterling, VA: Earthscan; 2000. [Google Scholar]
- Smith JS, Gilbert PA, Melendy A, Rana RK, Pimenta JM. Age-specific prevalence of human papillomavirus infection in males: A global review. Journal of Adolescent Health. 2011;48(6):540–552. doi: 10.1016/j.jadohealth.2011.03.010. [DOI] [PubMed] [Google Scholar]
- Teitelman AM, Stringer M, Nguyen GT, Hanlon AL, Averbuch T, Stimpfel AW. Social cognitive and clinical factors associated with HPV vaccine initiation among urban, economically disadvantaged women. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2011;40(6):691–701. doi: 10.1111/j.1552-6909.2011.01297.x. [DOI] [PubMed] [Google Scholar]
- Thomas TL. The new human papillomavirus (HPV) vaccine: Pros and cons for pediatric and adolescent health. Pediatric Nursing. 2008;34(5):429–431. [PubMed] [Google Scholar]
- Thomas TL, Freeman A. Project genesis: Self-reported religiosity and spirituality and sexual risk-taking in young African-American women attending a historically African-American college. Journal of National Black Nurses Association. 2011;22(1):27–35. [PubMed] [Google Scholar]
- Thomas T, Strickland O, DiClemente R, Higgins M. Identifying opportunities for cancer prevention during preadolescence and adolescence: Stopping HPV related cancer through HPV vaccination. Journal of Adolescent Health. doi: 10.1016/j.jadohealth.2012.08.011. in press. (Special Suppl) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas TL, Strickland O, DiClemente R, Williams B, Higgins M, Hickey K. Parental Human Papillomavirus Vaccine Survey (PHPVS): Nurse led instrument development and psychometric testing for use in research and primary care screening. Journal of Nursing Measurement. doi: 10.1891/1061-3749.21.1.96. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]