Abstract
Background
Obesity is a risk factor for colorectal neoplasia. Bioelectrical impedance analysis (BIA) is a novel and convenient method to measure body fat mass. The correlation between BIA and adenoma risk is unknown.
Aims
To conduct a cross-sectional study to evaluate BIA and other measures of obesity as risk factors for adenomas.
Methods
Participants underwent screening colonoscopy between 2006 and 2008. Waist-hip ratio (WHR) and body mass index (BMI) were measured. Percent body fat was calculated by BIA using a proprietary scale. Physical activity and other risk factors were assessed by telephone interview.
Results
255 patients with adenomas and 679 adenoma-free subjects were included. Increased age, male sex, and decreased physical activity were associated with adenoma prevalence. In multivariate analysis, WHR and BMI were independently associated with adenoma prevalence. Patients in the highest tertile of WHR had an OR of 2.0 (95% CI 1.2–3.2) compared to the lowest tertile. Obese white patients had significantly increased odds of having adenomas (OR 2.0 (95% CI 1.3, 3.2)) compared to whites with a normal BMI. Percent body fat measured by BIA was not associated with adenoma status: patients in the highest tertile of percent body fat had an OR of 1.0 (95% CI 0.7–1.6) compared to patients with the lowest tertile.
Conclusions
Percent body fat calculated by BIA was not associated with adenoma prevalence. Although BIA is a quick and convenient measure of adiposity, it is not predictive of adenoma risk perhaps because it measures the amount of fat but not the distribution.
Keywords: Bioelectrical Impedance analysis, Adipose tissue (MeSH), Colonic Neoplasms (MeSH), body fat distribution (MeSH)
Introduction
Colorectal cancer (CRC) is the third most common malignancy among men and women in the United States.[1] Despite a decrease in incidence in recent decades, it is estimated that there will be 143,460 new CRC cases and 51,690 deaths in 2012[2, 3] Variations in geographical CRC prevalence rates and migration patterns suggest that environmental and lifestyle exposures are important risk factors that influence the risk for colorectal neoplasia. Epidemiologic studies suggest that factors such as increased body mass index (BMI), lack of physical activity, central adiposity and high fat diets are all modifiable, risk factors for colorectal cancer and colorectal adenomas, the precursors to most cancers.[4]
Obese patients consistently exhibit a higher prevalence of colonic adenomas than non-obese controls.[5, 6] Despite the increased risk in obese individuals as a group, there is still considerable unexplained variation in risk between obese individuals. This might be explained by variations in individual body composition. The distribution and the composition of body fat, particularly visceral adiposity, is more predictive of complications from metabolic syndrome than weight alone,[7] and this may be the case for adenomas as well. Indeed, some studies have shown a connection between visceral adiposity and colorectal adenomas.[8, 9]
Unfortunately, visceral adiposity is difficult to measure. BMI measurements remain the standard by which obesity is defined, but BMI poorly correlates with true body composition.[10] Most techniques used to measure body composition such as cross-sectional imaging or plethysmography are limited to clinical trials. Traditional anthropometric measures such as waist-hip ratio (WHR) measurements are feasible to obtain but cumbersome, time-consuming, and may be embarrassing for patients. Recently, electronic scales able to measure both weight and body composition by way of bioelectrical impedance (BIA) have become available. These scales make it possible to obtain a potentially more sensitive measure of adiposity without adding significant cost or time. Of interest is that some studies have shown a link between certain BIA measurements and CRC risk[11, 12], but to our knowledge, percent body fat measured by BIA measures has never before been examined as a predictor of adenoma risk.
The Diet and Health Study V (DHS-V) was a cross-sectional study designed to study environmental and lifestyle factors associated with colorectal adenomas. We hypothesized that percent body-fat measured by BIA might be a better predictor of adiposity and therefore, adenoma risk than other anthropometric measures.
Materials and Methods
Study Overview and Population
The DHS-V was one of a series of cross-sectional studies designed to assess environmental and lifestyle factors associated with the presence of colorectal adenoma. The study methods have been published in detail elsewhere, [13–15] but are summarized here in brief. All patients referred for screening colonoscopy at the University of North Carolina (UNC) Hospitals during the years of 2006–2008 were eligible to participate. UNC Hospitals is an academic medical center with a large catchment area serving a diverse population. Inclusion criteria included all participants between the ages of 30 and 80 with a satisfactory preparation for colonoscopy and a complete exam to the cecum. Exclusion criteria included participants with a history of a prior colonoscopy, any patients with a history of a previous colon resection or a diagnosis of polyposis, colitis, or CRC. Following colonoscopy, additional data was collected via telephone interview (see below).
Eligible participants for this study were those who had a complete colonoscopy with available anthropometric data. From the eligible participants, cases were designated as individuals with one or more adenomatous polyp identified after pathology review. The comparator group consisted of subjects without adenomas, but who could have had hyperplastic polyps (HP) only.
The UNC School of Medicine Institutional Review Board approved the study. The STROBE guidelines for reporting descriptive observational studies were followed.[16]
Data Collection
Patients scheduling a screening colonoscopy were mailed a brochure describing the study and the possibility that they would be selected to participate at the time of their procedure. On the day of the scheduled exam, potential participants were recruited by a study coordinator prior to colonoscopy, at which time the participant’s height, weight, waist and hip circumference and percent body fat were measured. Percent body fat was obtained using a Tanita® model TBF-300WA scale (Arlington Heights, Illinois) (Figure 1). The participant’s gender, age, and height were entered into the scale and while the patient was being weighed, an imperceptible electrical current was passed from one foot to the other foot through the body via electrical contact pads incorporated into the base of the scale. The resulting electrical impedance was measured in ohms, and the scale then used the measured impedance to calculate percent body fat using a proprietary regression algorithm that incorporated age, weight, height and sex. Study patients then underwent screening colonoscopy per standard protocol.
Figure 1.
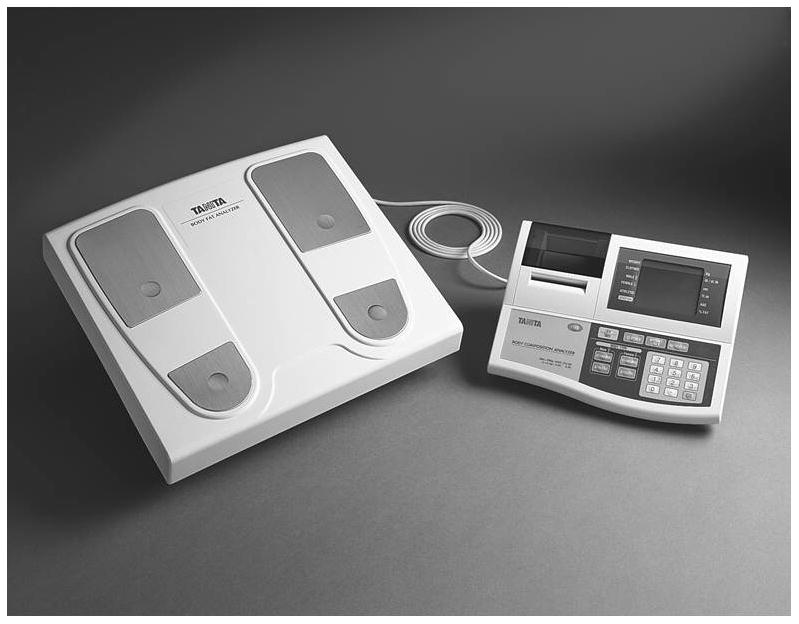
Tanita TBF-300WA scale used for bioelectrical impedance analysis and measurement of percent body fat in this study. Image courtesy of Tanita Corporation.
Within 12 weeks of colonoscopy, each patient received a phone call from a trained interviewer who was blinded to the colonoscopy results. The interviewer collected information on diet, bowel habits, physical activity, age, sex, race, smoking history, alcohol use, nonsteroidal anti-inflammatory drug (NSAID) use, laxative use and other co-morbidities.
BMI was calculated as kg/m2 and further categorized by obesity status per the World Health Organization classification system; normal (BMI < 25 kg/m2), overweight (BMI ≥25 kg/m2 to <30 kg/m2), and obese (BMI ≥ 30 kg/m2). Waist and hip circumference were measured in centimeters and reported as a ratio (‘waist-hip ratio’ or WHR) that was then divided into tertiles for statistical analysis. Percent body fat was reported as the proportion body fat mass to total body mass and divided into tertiles. Physical activity was estimated using the validated International Physical Activity Questionnaire and reported as metabolic equivalents minutes per week (MET-mins/week) and categorized into tertiles of activity.[17]
Statistical Analysis
Bivariate analysis was performed using chi-square or T-tests to assess the association between adenoma status and the following measures: percent body fat, BMI, WHR, weight, physical activity, height, race, sex and age. Multivariable analysis was then performed using logistic regression to explore the relationship of the three main measures of adiposity; percent body fat, BMI and WHR, and their association with adenoma status. These three models controlled for potential confounders including age, sex, race and physical activity. Since the measure of percent body fat by BIA was dependent on age and sex, it was inappropriate to control for these factors in the adjusted model. Therefore, percent body fat was adjusted for only race and physical activity. Effect measure modification was assessed using likelihood ratio tests. If effect measure modification was identified, the analysis was then stratified by the effect measure modifier. A further exploratory analysis was performed using logistic regression to determine which factors were best associated with case status. Factors not meeting the 10% change-in-estimate approach were dropped. All tests of significance were two-tailed and p-values <0.05 were considered significant. All data were entered into and analyzed using Stata 12.0 statistical software (StataCorp, College Station, TX).
Results
Characteristics of Cases and adenoma-free subjects
A total of 934 patients (255 cases and 679 adenoma-free subjects) had a complete colonoscopy and were available for analysis. Cases were older than non-cases, and more likely to be male. (Table 1) On average, cases were 8.6 pounds heavier, 0.7 inches taller, had a higher BMI and a larger WHR compared to non-cases. In addition, cases reported a significantly lower level of physical activity. Percent body fat was not associated with adenoma status in bivariate analysis.
Table 1.
Demographic and Anthropomorphic Characteristics of Study Population
| Characteristics | Adenoma-free subjects (n=679) | Adenoma cases (n=255) |
|---|---|---|
| Mean ±SE or n (%) | Mean ±SE or n (%) | |
| Age | 54.9 ± 0.2 | 56.6 ± 0.5* |
| Male | 241 (39%) | 122 (51%)* |
| Race† | ||
| White | 525 (89%) | 202 (87%) |
| Black | 65 (11%) | 29 (13%) |
| Height (inches) | 67.1 ± 0.2 | 67.8 ± 0.3* |
| Weight (pounds) | 172.3 ± 1.6 | 180.9 ± 2.4* |
| Percent Body Fat‡ | 30.3 ± 0.4 | 30.7 ± 0.7 |
| Waist/Hip Ratio | 0.901 ± 0.003 | 0.929 ± 0.005* |
| BMI (kg/m2) | 26.9 ± 0.2 | 27.8 ± 0.4* |
| Physical Activity (MET-mins/ week) | 2,535 ± 104 | 2,237 ± 152* |
| Tertile 1 | 187 (31%) | 92 (39%) |
| Tertile 2 | 205 (34%) | 74 (32%) |
| Tertile 3 | 211 (35%) | 68 (29%) |
p ≤ 0.05, obtained via Chi-squared tests (categorical variables) or t-tests (continuous variables)
Percentages calculated from subjects with available data on race (missing data excluded)
as measured by bioelectrical impedance analysis
BMI: Body mass index; MET: metabolic equivalent of task
Percent Body Fat, BMI, WHR, Physical Activity and Colorectal Adenomas
Logistic regression was used to calculate unadjusted and adjusted odds ratios for adenoma risk based on demographic and personal characteristics. (Table 2) There was no association between tertiles of percent body fat as measured by BIA and adenoma status. In contrast, there was a significant relationship between case status and WHR, BMI and physical activity. The odds of having an adenoma doubled for patients in the highest tertile of WHR. Patients in the highest tertile of physical activity had almost half the odds of having adenomas compared to patients in the lowest tertile. Significant interaction was found between BMI and race. We therefore, stratified BMI results by race. Using whites with a normal BMI (<25 kg/m2) as the referent for all comparisons, both overweight and obese white patients had significantly increased odds of having adenomas. In contrast, black patients with a normal BMI had 3.8 (95% CI; 1.3–10.6) times the odds of white patients with a normal BMI when adjusted for age, sex and physical activity. When overweight and obese blacks were compared to whites with a normal BMI, the odds of adenoma were increased, but these results were not statistically significant.
Table 2.
Odds Ratios (95% CI) of Adenoma Risk by Demographic, Anthropometric and Lifestyle Factors from Univariate and Multivariate Logistic Regression Models
| Factors | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Age (per 10 year increase) | 1.5 (1.2, 1.9) | |
| Male | 1.6 (1.2, 2.1) | |
| Race | ||
| White | 1.0 | |
| Black | 1.2 (0.7, 1.9) | |
| Height (3 inch increments) | 1.1 (1.0, 1.2) | |
| Weight (per 10 lbs. increments) | 1.05 (1.02, 1.09 | |
| Percent Body Fat by BIA | ||
| Tertile 1 (referent) | 1.0 | 1.0* |
| Tertile 2 | 0.8 (0.5, 1.2) | 0.7 (0.5, 1.1)* |
| Tertile 3 | 1.1 (0.8, 1.6) | 1.0 (0.7, 1.5)* |
| Waist-hip Ratio | ||
| Tertile 1 (referent) | 1.0 | 1.0† |
| Tertile 2 | 1.5 (1.0, 2.2) | 1.5 (1.0, 2.3)† |
| Tertile 3 | 2.2 (1.5, 3.3) | 2.0 (1.3, 3.3)† |
| BMI by Race | ||
| Whites | ||
| BMI < 25 (referent) | 1.0 | 1.0‡ |
| BMI 25 to <30 | 1.9 (1.3, 2.8) | 1.7 (1.2, 2.5)‡ |
| BMI >30 | 1.8 (1.2, 2.9) | 2.0 (1.3, 3.2)‡ |
| Blacks | ||
| BMI < 25 | 3.3 (1.2, 8.9) | 3.8 (1.3, 10.6)‡ |
| BMI 25 to <30 | 1.9 (0.8, 4.5) | 1.8 (0.7, 4.4)‡ |
| BMI >30 | 1.2 (0.6, 2.4) | 1.3 (0.7, 2.6)‡ |
| Physical Activity | ||
| Tertile 1 (referent) | 1.0 | 1.0§ |
| Tertile 2 | 0.7 (0.5, 1.1) | 0.7 (0.5, 1.0)§ |
| Tertile 3 | 0.7 (0.5, 1.0) | 0.6 (0.4, 0.9)§ |
Adjusted for race and physical activity
Adjusted for age sex race and physical activity
Adjusted for age sex and physical activity
Adjusted for age sex and race
BIA: bioelectrical impedance analysis; BMI: Body mass index
Factors Most Strongly Associated with Adenoma Status
Exploratory models were created to determine which factors were most strongly associated with adenoma status. Case status was modeled with a logistic regression model and included the independent variables: age, sex, physical activity, weight, and race and WHR. BMI was excluded because it is a construct of height/weight2 and interacts with race. Percent body fat was excluded because it was calculated using a proprietary equation which incorporated impedance, age, sex, and weight. Using the Wald test, all non-significant terms were dropped from the model. The final model showed that WHR adjusted for age was most strongly associated with adenoma status. For every 0.1 increase in WHR the odds of having an adenoma increased by 1.6 (95% CI; 1.3–2.0)
Discussion
To our knowledge this is the first study to evaluate the relationship between percent body fat as measured with bioelectrical impedance using a commercially-available scale and adenoma status. Contrary to our expectation, percent body fat as measured by leg to leg BIA was not significantly associated to adenoma status. Both the adenoma and adenoma-free groups had equivalent percent body fat. In contrast, other anthropometric measures of adiposity such as weight, WHR, and BMI were statistically associated with adenoma status.
Obesity has been shown to be a risk factor for both colorectal adenomas and cancer. However, not all obese individuals exhibit the same risk. In this study, we hypothesized that percent body fat might be a more sensitive and convenient measure to identify patients at higher risk for adenomatous polyps. The ability to measure body composition using BIA has appeal because of its ease of use and acceptability to patients. Other methods require expensive equipment or are time-consuming. Scales with the capability of measuring body composition using BIA while a patient is being weighed add little extra time.
It is unclear why percent body fat did not correlate with adenoma status in this study. Other measures of adiposity such as weight, BMI and WHR correlated with case status as we had expected. Perhaps the BIA measurements and/or the proprietary equation used resulted in inaccurate estimates of percent body fat. Bipedal devices such as that used in this study may be less accurate than tetrapolar and octapolar BIA instruments, particularly for body fat measurements.[18] However, this and similar devices have demonstrated accuracy for estimating body composition and body fat in validation studies.[19, 20] BIA is a variable measure that can be affected by age, exercise, and fluid shifts.[21–23] It is possible, for example, that BIA measurements were influenced by the polyethylene glycol colon lavage solution ingested by patients in preparation for colonoscopy. It is also possible that the path of the electrical current from one leg to the other does not accurately assess abdominal and visceral adiposity, and it is the fat distribution that is the most important determinant of adenoma risk.[8, 9] We did not adjust for dietary factors, as we were interested in whether % body fat could be a “stand alone” measure of adenoma risk. However, if fat intake (for example) was a confounder of the relationship between % body fat and adenomas, this would be expected to bias away from the null. Since we found a null result, this seems unlikely. Also, since the control group contained some persons with HP, if % body fat is a risk factor for HP, this could have biased our results towards the null. Finally, cross-sectional studies have limitations including inability to definitively establish temporal relationships, but we believe this design was appropriate to answer our research question.
In summary, bioelectrical impedance measures of body composition did not correlate with adenoma status in this study as we had hypothesized. In contrast, BMI, WHR and physical activity did correlate with adenoma status, which is a consistent finding from previous studies. Waist-hip ratio measurements appeared to be most closely correlated with adenoma status and this supports the concept of abdominal and visceral adiposity as a significant modifiable risk factor for adenoma formation. It is important to continue to explore additional ways of measuring abdominal and visceral adiposity and their relationship to colon adenoma status and colorectal cancer. However, our results suggest that percent body fat as measured by bioelectric impedance, as performed in this study, does not correlate with adenoma risk. Therefore, this technique has limited usefulness in colorectal neoplasia research or risk stratification.
Acknowledgments
Financial support: Supported by Grants: P30 DK34987, R01 CA44684, T32 DK07634
Abbreviations
- BIA
Bioelectrical Impedance
- BMI
body mass index
- DHS-V
Diet and Health study V
- MET
Metabolic Equivalent of Task
- NSAID
Nonsteroidal anti-inflammatory drug
- UNC
University of North Carolina
Footnotes
Disclosures/Conflict of interest: None for all authors
Author Contributions:
David Frantz MD, MS: Analysis and interpretation of data, Statistical Analysis, Drafting of the manuscript
Seth Crockett MD, MPH: Analysis and interpretation of data, Critical Revision of Manuscript
Robert Sandler MD MPH: Study Concept and Design, Data Acquisition, Analysis and Interpretation of Data, Critical Revision of Manuscript, and Funding
Joseph Galanko PhD: Statistical Analysis, Critical Revision of Manuscript BIA and Adenoma Status
References
- 1.Society AC, editor. Cancer Facts & Figures 2012. Vol. 58 Atlanta, GA: American Cancer Society; 2012. [Google Scholar]
- 2.Society AC, editor. Cancer Facts & Figures 2011. Vol. 58 Atlanta, GA: American Cancer Society; 2011. [Google Scholar]
- 3.Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA: a cancer journal for clinicians. 2011 Jul-Aug;61(4):212–236. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 4.Giovannucci E. Modifiable risk factors for colon cancer. Gastroenterology clinics of North America. 2002 Dec;31(4):925–943. doi: 10.1016/s0889-8553(02)00057-2. [DOI] [PubMed] [Google Scholar]
- 5.Martin C, Connelly A, Keku TO, Mountcastle SB, Galanko J, Woosley JT, Schliebe B, Lund PK, Sandler RS. Nonsteroidal anti-inflammatory drugs, apoptosis, and colorectal adenomas. Gastroenterology. 2002 Dec;123(6):1770–1777. doi: 10.1053/gast.2002.37053. [DOI] [PubMed] [Google Scholar]
- 6.Keku TO, Lund PK, Galanko J, Simmons JG, Woosley JT, Sandler RS. Insulin resistance, apoptosis, and colorectal adenoma risk. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive. Oncology. 2005 Sep;14(9):2076–2081. doi: 10.1158/1055-9965.EPI-05-0239. [DOI] [PubMed] [Google Scholar]
- 7.Matsuzawa Y. Establishment of a concept of visceral fat syndrome and discovery of adiponectin. Proceedings of the Japan Academy Series B, Physical and biological sciences. 2010;86(2):131–141. doi: 10.2183/pjab.86.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nam SY, Kim BC, Han KS, Ryu KH, Park BJ, Kim HB, Nam BH. Abdominal visceral adipose tissue predicts risk of colorectal adenoma in both sexes. Clin Gastroenterol Hepatol. 2010 May;8(5):443–450. e441–442. doi: 10.1016/j.cgh.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Otake S, Takeda H, Suzuki Y, Fukui T, Watanabe S, Ishihama K, Saito T, Togashi H, Nakamura T, Matsuzawa Y, Kawata S. Association of visceral fat accumulation and plasma adiponectin with colorectal adenoma: evidence for participation of insulin resistance. Clin Cancer Res. 2005 May 15;11(10):3642–3646. doi: 10.1158/1078-0432.CCR-04-1868. [DOI] [PubMed] [Google Scholar]
- 10.Ode JJ, Pivarnik JM, Reeves MJ, Knous JL. Body mass index as a predictor of percent fat in college athletes and nonathletes. Med Sci Sports Exerc. 2007 Mar;39(3):403–409. doi: 10.1249/01.mss.0000247008.19127.3e. [DOI] [PubMed] [Google Scholar]
- 11.MacInnis RJ, English DR, Hopper JL, Haydon AM, Gertig DM, Giles GG. Body size and composition and colon cancer risk in men. Cancer Epidemiol Biomarkers Prev. 2004 Apr;13(4):553–559. [PubMed] [Google Scholar]
- 12.MacInnis RJ, English DR, Haydon AM, Hopper JL, Gertig DM, Giles GG. Body size and composition and risk of rectal cancer (Australia) Cancer Causes Control. 2006 Dec;17(10):1291–1297. doi: 10.1007/s10552-006-0074-y. [DOI] [PubMed] [Google Scholar]
- 13.Guilera M, Connelly-Frost A, Keku TO, Martin CF, Galanko J, Sandler RS. Does physical activity modify the association between body mass index and colorectal adenomas? Nutr Cancer. 2005;51(2):140–145. doi: 10.1207/s15327914nc5102_3. [DOI] [PubMed] [Google Scholar]
- 14.Vinikoor LC, Schroeder JC, Millikan RC, Satia JA, Martin CF, Ibrahim J, Galanko JA, Sandler RS. Consumption of trans-fatty acid and its association with colorectal adenomas. Am J Epidemiol. 2008 Aug 1;168(3):289–297. doi: 10.1093/aje/kwn134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Austin GL, Adair LS, Galanko JA, Martin CF, Satia JA, Sandler RS. A diet high in fruits and low in meats reduces the risk of colorectal adenomas. The Journal of nutrition. 2007 Apr;137(4):999–1004. doi: 10.1093/jn/137.4.999. [DOI] [PubMed] [Google Scholar]
- 16.Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007 Oct 16;147(8):W163–194. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. [DOI] [PubMed] [Google Scholar]
- 17.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003 Aug;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 18.Bosy-Westphal A, Later W, Hitze B, Sato T, Kossel E, Gluer CC, Heller M, Muller MJ. Accuracy of bioelectrical impedance consumer devices for measurement of body composition in comparison to whole body magnetic resonance imaging and dual X-ray absorptiometry. Obes Facts. 2008;1(6):319–324. doi: 10.1159/000176061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang JG, Zhang Y, Chen HE, Li Y, Cheng XG, Xu L, Guo Z, Zhao XS, Sato T, Cao QY, Chen KM, Li B. Comparison of two bioelectrical impedance analysis devices with dual energy X-ray absorptiometry and magnetic resonance imaging in the estimation of body composition. J Strength Cond Res. 2012 Feb 15; doi: 10.1519/JSC.0b013e31824f2040. [DOI] [PubMed] [Google Scholar]
- 20.Ling CH, de Craen AJ, Slagboom PE, Gunn DA, Stokkel MP, Westendorp RG, Maier AB. Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clin Nutr. 2011 Oct;30(5):610–615. doi: 10.1016/j.clnu.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 21.Mally K, Trentmann J, Heller M, Dittmar M. Reliability and accuracy of segmental bioelectrical impedance analysis for assessing muscle and fat mass in older Europeans: a comparison with dual-energy X-ray absorptiometry. Eur J Appl Physiol. 2011 Aug;111(8):1879–1887. doi: 10.1007/s00421-010-1795-x. [DOI] [PubMed] [Google Scholar]
- 22.Knechtle B, Wirth A, Knechtle P, Rosemann T, Rust CA, Bescos R. A comparison of fat mass and skeletal muscle mass estimation in male ultra-endurance athletes using bioelectrical impedance analysis and different anthropometric methods. Nutr Hosp. 2011 Nov-Dec;26(6):1420–1427. doi: 10.1590/S0212-16112011000600032. [DOI] [PubMed] [Google Scholar]
- 23.Dixon CB, Ramos L, Fitzgerald E, Reppert D, Andreacci JL. The effect of acute fluid consumption on measures of impedance and percent body fat estimated using segmental bioelectrical impedance analysis. Eur J Clin Nutr. 2009 Sep;63(9):1115–1122. doi: 10.1038/ejcn.2009.42. [DOI] [PubMed] [Google Scholar]


