Abstract
Introduction:
Tooth decay (TD) is common in children with significant consequences on systemic well-being, growth and quality of life, as well as increasing the risk of decay in the permanent teeth.
Aim:
The aim of the present study is to define risk factors associated with deciduous TD (DTD) in Iraqi preschool children.
Materials and Methods:
From the 1st June to 31st December 2012, a case-control study was carried out on 684 children under the age of 6 years who attended Al-Aulwyiah pediatric teaching hospital in Baghdad. Clinical examination and World Health Organization caries diagnostic criteria for decayed, missing and filled teeth (DMFT) were applied. Data including gender, residence, socio-economic status (SES), parental education level, parental smoking, tooth brushing frequency, type of feeding during infancy and the presence of any systemic disease in the child were sought.
Results:
The mean DMFT score in the case group was 2.03 ± 1.39, of which decayed teeth formed 1.93. Males had a higher mean DMFT (2.10 ± 1.08) than females (1.96 ± 1.70) but with no statistically significant difference. The study revealed that residence, SES, parental education level and tooth brushing frequency were dependent risk factors significantly associated with DTD. However, gender, parental smoking and pattern of feeding during infancy were not significantly associated with DTD. Only four children with systemic disorders (1.2%), namely asthma and congenital heart diseases, were noticed to have DTD.
Conclusion:
Pediatricians and dentists could provide dental preventive and screening measures. Confronting relevant risk factors associated with DTD and improving access to oral care services are suggested. In addition, promotion of oral health programs through school curricula is needed.
Keywords: Children, deciduous tooth decay, Iraq, risk factors
INTRODUCTION
Tooth decay (TD) represents a tremendous health-affecting challenge and fiscal burden to both developed and developing countries. TD affects three aspects of daily living, namely systemic health, body weight and growth and quality of life.[1] It can also lead to problems with attending to learning because of substantial school absence,[2] increasing the risk of decay in the permanent teeth,[3] and it accounts for the major portion of annual dental expenditures.[4]
In most developing countries, the levels of TD were low until recent years but prevalence rates of TD and TD experience are now tending to increase. This is largely due to the increasing consumption of sugars and inadequate exposure to fluorides. In contrast, a decline in TD has been observed in most industrialized countries over the past 20 years or so. This pattern was the result of a number of public health measures, including effective use of fluorides, together with changing living conditions, life-styles and improved self-care practices.[5]
TD is common in Iraqi children with reported prevalence of 62% in school children and risk factors contributing to TD were addressed.[6] However, no studies are yet present addressing risk factors associated with deciduous TD (DTD) in Iraqi preschool children. Therefore, this work was designed to study risk factors associated with DTD in Iraqi preschool children hoping it would be beneficial to the practicing pediatricians and dentists.
MATERIALS AND METHODS
Over 6 consecutive months (1st June to 31st December) in 2012, a case-control study was carried out on 684 children under the age of 6 years who attended Al-Aulwyiah pediatric teaching hospital in Baghdad. The case group was 342 children with DTD who attended dental consultation out-patient clinic. The control group was 342 caries-free children who attended immunization clinic for filling immunization program. The World Health Organization caries diagnostic criteria for decayed, missing and filled teeth (DMFT) were used to evaluate TD status.[7] Clinical examinations of the studied children were done under artificial light using a sharp sickle explorer, flat-surface mouth mirror, gauze, sponges and compressed air. The studied variables included the following: Gender, residence, socioeconomic status (SES), parental education level, parental smoking, tooth brushing frequency, type of feeding during infancy and the presence of any systemic disease in the child. Statistical analysis of data was performed using Chi-square. The statistical significance was set at P ≤ 0.05. The scientific and ethical committee at Al-Kindy College of Medicine, Baghdad University approved the study.
RESULTS
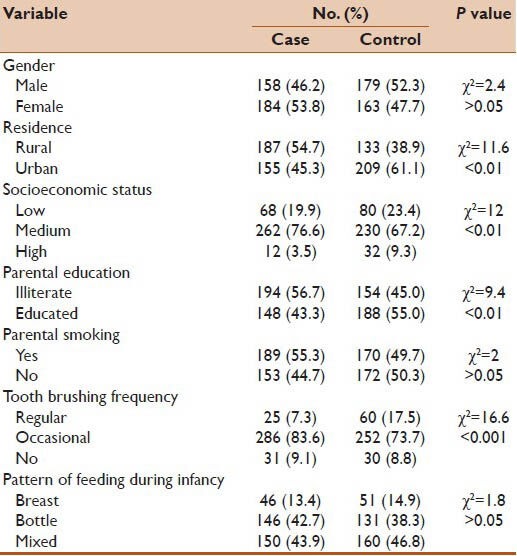
The total number of studied children was 684 (case group: n = 342; control group: n = 342). The case group involved 158 (46.2%) males and 184 (53.8%) females with a male to female ratio of 1:1.2 and a mean age of 3.1 ± 2.2 years. The control group included 179 (52.3%) males and 163 (47.7%) females with a male to female ratio of 1:0.9 and a mean age of 3.6 ± 1.8 years. The mean DMFT score in the studied case group was 2.03 ± 1.39, of which decayed teeth constituted 1.93. Males had a higher mean DMFT (2.10 ± 1.08) than females (1.96 ± 1.70) but with no statistically significant difference. As you can be seen in Table 1, the distribution of the studied variables with their levels of statistical significance. Residence, SES, parental education level and tooth brushing frequency were dependent risk factors significantly associated with DTD. However, gender, parental smoking and pattern of feeding during infancy were not significantly associated with DTD. Four children with systemic diseases (1.2%), namely asthma and congenital heart diseases, were noticed to have DTD.
Table 1.
Statistical significance of various variables in the studied children
DISCUSSION
The study showed that gender was not significantly associated with DTD. However, a set of researchers have addressed that in male children, TD rates are greater than, or equal to, female rates. This gender gap might result from genetic, hormonal and cultural influences.[8]
The study also revealed that residence was significantly associated with DTD (P < 0.01). This could be explained by the fact that children residing in rural areas where infrastructures are deficient have less access to and utilization of dental care compared to children residing in urban areas.
SES was noticed to be significantly associated with DTD (P < 0.01). This supports the notion that poverty and low SES play important roles in TD development.[9] Lower income families absorb disproportionately the effect of dental diseases due to lack of education, food availability and selection and access to early preventive care. Interestingly, a Canadian study has addressed stress-related psychobiological processes that might account for the high, disproportionate rates of TD among children growing up in low SES families. The study showed that the socioeconomic partitioning of childhood TD may involve social and psychobiological pathways through which lower SES is associated with higher numbers of cariogenic bacteria and higher levels of stress-associated salivary cortisol. The study concluded that this convergence of psychosocial, infectious and stress-related biological processes appears to be implicated in the production of greater cariogenic bacterial growth and in the conferral of an increased physical vulnerability of the developing dentition.[10]
Parental education level was found to be a risk factor significantly associated with DTD (P < 0.01). This agrees with the observation that low parental schooling, particularly the mothers made the occurrence of both early and severe TC more likely.[11] Educated parents have better health knowledge and positive attitudes toward oral health, including TD. Hence, they have children's sound dentition. Oral hygiene habits and dietary habits are established during preschool days and parents, particularly the mothers, can function as role models for their children.
Despite the significant association between parental smoking and early TD was identified,[12] no such association was found in the current study. This might be attributed to the observation that smoking is still a prevailing health threat in Iraq that affects all social classes and different age groups.[13]
There was a significantly higher statistical correlation between tooth brushing frequency and DTD (P < 0.001). This augments the notion that low frequency and improper tooth brushing methods are closely associated with early TD.[14] Parents’ characteristics, particularly schooling level and positive attitude towards oral health and dental care were found to be associated with more favorable pattern of tooth brushing in children.[15] Thus, parents need to brush the teeth of the children daily, using fluoridated children toothpaste starting the day of the appearance of the first milk tooth.
Interestingly, no significant association between pattern of feeding during infancy and DTD was noted in the present study. Breast feeding (BF) is almost universal and regarded as the normal way to feed infants and young children. Although the promotion of BF began in Iraq in1993, exclusive BF rate is still not more than 25% in Iraq.[16] Accordingly, bottle and mixed feeding are still the prevailing pattern of feeding infants in Iraq. A lot of debate has been addressed considering the potential protective effect of breast milk against TD. The relationship between BF and TD development is actually complex and could be confounded by many variables, mainly infection with Streptococcus mutans, enamel hypoplasia, sugar intake in its different forms and social conditions represented by parents’ educational level and SES. An interesting Swedish study has confirmed that maternal milk, in addition to not being cariogenic, is a protective factor against the occurrence of TD. Human milk components are able to inhibit adhesion of Streptococcus mutans to hydroxyapatite crystals in vitro.[17] On the other hand, there is a significantly higher percentage of children developed early TD on having prolonged BF, bottle feeding, nocturnal bottle feeding containing sweet drink and milk and higher frequency of consumption of sweets.[18]
Children who have systemic diseases face the burden of a certain disease distinctly greater than their healthy counterparts. Certain systemic diseases were found to be closely linked to TD such as hereditary anomalies, cerebral palsy, juvenile arthritis, developmental delay, congenital heart diseases and chronic respiratory illnesses.[19] In the present study, only four patients with systemic diseases (1.2%), including asthma and congenital heart diseases were identified to have DTD. This low frequency might be attributed to the methodology employed in the study where all the studied children were selected from dental consultation and immunization outpatient clinic.
Few researches were published on risk factors associated with DTD in the preschool children in countries of Jordan,[20] Lebanon[21] and Turkey.[22] Their addressed data looked nearly similar to that in the present study.
Because most children are exposed to general medical care but not dental care at an early age, pediatricians have the opportunity to play an important role in helping children and their families gain access to dental care through screening, referral and provision of dental preventive measures.[23] Parents must actively participate in preserving dental health of their offspring. There is a need to impart them knowledge on TD and periodontal diseases, proper nutrition and the risk of TD from frequent intake of sweet drinks either alone or in addition to sweet treats, regular and proper oral hygiene and proper use of fluoride products as well as the significance of regular check-ups with a dentist. The first dental inspection of children is due at the age of 2 years.
As caries progression or reversal is determined by the balance between protective and pathological factors, comprehensive school-based oral health curricula should be given high priority not only by physicians (general, pediatricians, pediatric dentists) but also by schools faculties and even the governmental authorities. These curricula including oral health knowledge and an evidence-based approach to dental health education within a school setting were found to enable primary school teachers to play a significant part in oral health promotion for young children. They also had positive effects on oral health behavior of children and on oral health knowledge and attitudes of mothers and teachers.[24,25] The three conflicts Iraq has engaged over the past three decades have enormously eroded the healthcare system in Iraq and significantly affected the health of the population, including oral health. Public awareness program adopted by the Ministry of Health and school-based oral health curricula adopted by the Ministry of Education are to be shortly implemented in Iraq. Collaboratively, they are tailored by dentists, pediatricians, school faculties and various public organizations and their beneficial effects are to be evaluated.
The present study has two limitations. The data were collected from a single hospital. Moreover; the study was hospital-based. Therefore, it might not be truly representative of whole Iraqi preschool children. Large multi-center and community-based studies can better determine exact risk factors associated with DTD in Iraqi preschool children.
CONCLUSION
DTD constitutes a significant health problem in Iraqi preschool children. Pediatricians and dentists could play a pivotal role in providing dental preventive and screening measures. Targeting dependent risk factors associated with DTD and improving access to oral care services are suggested. In addition, promotion of oral health programs through school curricula and addressing suitable public preventive measures are of utmost importance.
ACKNOLWLEDGMENTS
Great thanks are due to the staff of dental consultation out-patient clinic and immunization clinic in Al-Aulwyiah pediatric teaching hospital in Baghdad for their kind help in performing this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sheiham A. Dental caries affects body weight, growth and quality of life in pre-school children. Br Dent J. 2006;201:625–6. doi: 10.1038/sj.bdj.4814259. [DOI] [PubMed] [Google Scholar]
- 2.Piovesan C, Antunes JL, Mendes FM, Guedes RS, Ardenghi TM. Influence of children's oral health-related quality of life on school performance and school absenteeism. J Public Health Dent. 2012;72:156–63. doi: 10.1111/j.1752-7325.2011.00301.x. [DOI] [PubMed] [Google Scholar]
- 3.Skeie MS, Raadal M, Strand GV, Espelid I. The relationship between caries in the primary dentition at 5 years of age and permanent dentition at 10 years of age-A longitudinal study. Int J Paediatr Dent. 2006;16:152–60. doi: 10.1111/j.1365-263X.2006.00720.x. [DOI] [PubMed] [Google Scholar]
- 4.Mandel ID. Oral infections: Impact on human health, well-being, and health-care costs. Compend Contin Educ Dent. 2004;25:881–2. 884, 888. [PubMed] [Google Scholar]
- 5.Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83:661–9. [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmed NA, Astrøm AN, Skaug N, Petersen PE. Dental caries prevalence and risk factors among 12-year old schoolchildren from Baghdad, Iraq: A post-war survey. Int Dent J. 2007;57:36–44. doi: 10.1111/j.1875-595x.2007.tb00116.x. [DOI] [PubMed] [Google Scholar]
- 7.Oral Health Surveys: Basic Methods. 4th ed. Geneva: World Health Organization; 1997. World Health Organization: Dentition status and treatment needs; pp. 40–7. [Google Scholar]
- 8.Lukacs JR. Gender differences in oral health in South Asia: Metadata imply multifactorial biological and cultural causes. Am J Hum Biol. 2011;23:398–411. doi: 10.1002/ajhb.21164. [DOI] [PubMed] [Google Scholar]
- 9.Squassi A, Mauro S, Mauro MJ, Sánchez G, Bordoni N. Relationship between oral health in children and poverty related factors. Acta Odontol Latinoam. 2008;21:49–56. [PubMed] [Google Scholar]
- 10.Boyce WT, Den Besten PK, Stamperdahl J, Zhan L, Jiang Y, Adler NE, et al. Social inequalities in childhood dental caries: The convergent roles of stress, bacteria and disadvantage. Soc Sci Med. 2010;71:1644–52. doi: 10.1016/j.socscimed.2010.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Traebert J, Guimarães Ldo A, Durante EZ, Serratine AC. Low maternal schooling and severity of dental caries in Brazilian preschool children. Oral Health Prev Dent. 2009;7:39–45. [PubMed] [Google Scholar]
- 12.Leroy R, Hoppenbrouwers K, Jara A, Declerck D. Parental smoking behavior and caries experience in preschool children. Community Dent Oral Epidemiol. 2008;36:249–57. doi: 10.1111/j.1600-0528.2007.00393.x. [DOI] [PubMed] [Google Scholar]
- 13.Ministry of Health, Directorate of Public Health and Primary Health Care, Ministry of Planning and Development Cooperation, Central Organization for Statistics and Information in Collaboration with World Health Organization. Chronic Non-Communicable Diseases Risk Factors Survey in Iraq 2006, A Step wise Approach. [Last accessed on 2013 Aug 29]. Available from: http://www.who.int/chp/steps/iraqstepsreport2006.pdf .
- 14.Guido JA, Martinez Mier EA, Soto A, Eggertsson H, Sanders BJ, Jones JE, et al. Caries prevalence and its association with brushing habits, water availability, and the intake of sugared beverages. Int J Paediatr Dent. 2011;21:432–40. doi: 10.1111/j.1365-263X.2011.01146.x. [DOI] [PubMed] [Google Scholar]
- 15.Vallejos-Sánchez AA, Medina-Solís CE, Maupomé G, Casanova-Rosado JF, Minaya-Sánchez M, Villalobos-Rodelo JJ, et al. Sociobehavioral factors influencing toothbrushing frequency among schoolchildren. J Am Dent Assoc. 2008;139:743–9. doi: 10.14219/jada.archive.2008.0256. [DOI] [PubMed] [Google Scholar]
- 16.New York: UNICEF; 2007. The State of the World's Children 2008, [Child survival] [Google Scholar]
- 17.Danielsson Niemi L, Hernell O, Johansson I. Human milk compounds inhibiting adhesion of mutans streptococci to host ligand-coated hydroxyapatite in vitro. Caries Res. 2009;43:171–8. doi: 10.1159/000213888. [DOI] [PubMed] [Google Scholar]
- 18.Bahuguna R, Younis Khan S, Jain A. Influence of feeding practices on dental caries. A case-control study. Eur J Paediatr Dent. 2013;14:55–8. [PubMed] [Google Scholar]
- 19.Thikkurissy S, Lal S. Oral health burden in children with systemic diseases. Dent Clin North Am. 2009;53:351–7. doi: 10.1016/j.cden.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Rajab LD, Hamdan MA. Early childhood caries and risk factors in Jordan. Community Dent Health. 2002;19:224–9. [PubMed] [Google Scholar]
- 21.Chedid NR, Bourgeois D, Kaloustian H, Baba NZ, Pilipili C. Caries prevalence and caries risk in a sample of Lebanese preschool children. Odontostomatol Trop. 2011;34:31–45. [PubMed] [Google Scholar]
- 22.Ozer S, Sen Tunc E, Bayrak S, Egilmez T. Evaluation of certain risk factors for early childhood caries in Samsun, Turkey. Eur J Paediatr Dent. 2011;12:103–6. [PubMed] [Google Scholar]
- 23.Krol DM. Children's oral health and the role of the pediatrician. Curr Opin Pediatr. 2010;22:804–8. doi: 10.1097/MOP.0b013e3283402e3b. [DOI] [PubMed] [Google Scholar]
- 24.Petersen PE, Peng B, Tai B, Bian Z, Fan M. Effect of a school-based oral health education programme in Wuhan City, Peoples Republic of China. Int Dent J. 2004;54:33–41. doi: 10.1111/j.1875-595x.2004.tb00250.x. [DOI] [PubMed] [Google Scholar]
- 25.Ramroop V, Wright D, Naidu R. Dental health knowledge and attitudes of primary school teachers toward developing dental health education. West Indian Med J. 2011;60:576–80. [PubMed] [Google Scholar]


