Abstract
Context:
Sexual dysfunction (SD) among diabetic women is an important disorder. It has many negative effects on general health.
Aims:
This study aimed to compare SD status between diabetic and non-diabetic women.
Settings and Design:
This study was conducted on 200 women, half of them diabetic and the others as non-diabetic in Tohid Hospital (Sanandaj, Iran).
Materials and Methods:
The non-diabetic group was matched for age (±5 years) and education. Data were collected using an interview-based questionnaire containing demographic characteristics and female sexual function index (FSFI).
Statistical Analysis Used:
Univariate and multivariate analyses were performed to assess and interpret the results.
Results:
Analyses of the data showed that low educational levels, longer duration of diabetes and poor controlled diabetes were associated with the lower FSFI scores. In both groups the prevalence of SDs for all FSFI domains was high. Furthermore, multivariate analysis showed that these three variables were associated with lower FSFI scores.
Conclusions:
Study confirms that Kurdish Iranian diabetic women are at an increased risk of SD. Low educational level, longer duration of diabetes, and poor controlled diabetes were associated with a lower FSFI score.
Keywords: Diabetes mellitus, sexual dysfunction, women health
INTRODUCTION
Sexual dysfunction (SD) is a common disease among Iranian women and most of them never seek treatment and help for this sort of problem.[1] SD among diabetic women is also a frequent disorder; However, previous studies have reported different prevalence rates for it.[2,3,4] It seems SD is associated with different factors including, age, depression, duration of diabetes, emotional, and hormonal disorders.[2,3,5,6,7,8,9,10,11,12,13]
In a study conducted by Ziaei-Rad, et al., they reported the prevalence of 88% for SD among Iranian diabetic women.[14] Most of the previous studies showed that diabetic women have higher SD prevalence as compared to non-diabetic women.[3,14,15,16] However, there were some reports about no significant difference between diabetic and non-diabetic women[8,17] and hence, SD among diabetic women is still a controversial topic. Neuropathy, vascular, and psychological disorders and un-controlled glucose caused by diabetes may affect sexual function and their impact could be observed in various sexual domains.[15,18,19,20]
SDs have many negative effects on general health and are associated with social problems, psychological diseases, and high divorce rate.[4] These impacts are more complicated at the presence of special cares necessary for diabetic patients. Therefore, it is necessary to conduct comprehensive studies among different ethnic groups, especially in Islamic countries where sex is a taboo. Kurdish ethnicity is one of the main Iranian ethnicities living in the western part of Iran. Sex is a taboo subject in this ethnicity and it seems sexual behaviors among this ethnicity suffer from basic problems. There has been little research conducted on SD in Iran.[14,21] Therefore, the present study aims to survey the current status of SD among Kurdish diabetic women and compare the prevalence of this disorder between diabetic and non-diabetic women.
MATERIALS AND METHODS
The present study, conducted on 100 diabetic women selected by simple sampling method among the patients attending Tohid Diabetes Center (Sanandaj, Iran) during 2010-2011. All procedures of the study were approved by ethical committee of Kurdistan Medical University and informed consent was obtained from participants. An inclusion criterion for diabetic group was carrying diabetes more than 1 year and exclusion criteria were limbs amputation, any history of cardiovascular or cerebrovascular attack, dialysis, physical or mental disability, and post-menopause. The non-diabetic group was composed of 100 women selected by systematic sampling method among non-diabetic women attending the general clinic in Tohid hospital (Sanandaj, Iran). For every diabetic participants, there was a non-diabetic matched for age (±5 years) and educational group (educated and non-educated). Exclusion criteria for non-diabetic group were similar to those applied to diabetic group.
The participants were clearly informed about the research objective and all of them signed a written informed consent form prior to participation. Data were collected using an interview-based questionnaire containing demographic items, the disease characteristics, and female sexual function index (FSFI). glycated hemoglobin (HbA1C) was assessed in the diabetic group. The FSFI questionnaire consists of 19 questions in six domains (desire, arousal, lubrication, orgasm, satisfaction and pain).[22] The Persian version of SFSI was used. The validity and reliability of this version were evaluated by Mohammadi, et al.[21] Every domain's score could be calculated by adding the all questions’ scores in the domain and multiplying the sum by the domain factor provided in the FSFI. The minimum and maximum score were 2 and 36, respectively.
The data were entered in Statistical Program for Social Sciences (SPSS 11.5) software. Univariate analysis for paired quantitative and independent data was performed using paired t-test and independent t-test, respectively.
Multiple regression analysis was carried out in the diabetic group. FSFI score was selected as a dependent variable and those variables with (P < 0.25) in univariate analysis were entered the model as independent variables.
RESULTS
All participants accepted to participate in the study and nobody refused. From all participants, 68 persons (68%) in the diabetic group and 70 persons (70%) in non-diabetic group were literate (P = 0.76); 46 persons (46%) in the diabetic group and 72 (72%) in the non-diabetic group were married < 10 years (P < 0.001); 33 people (33%) in the diabetic group were taking insulin; 46 subjects (46%) were carrying diabetes < 5 years; and six persons in the diabetic group were older than 45 years old.
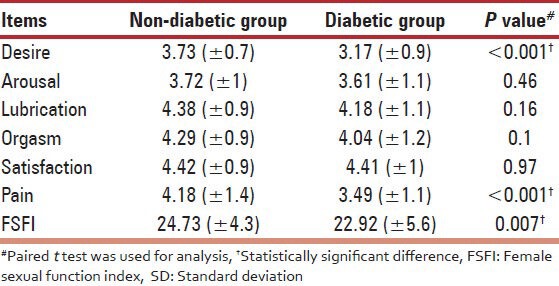
The mean FSFI score for diabetic and non-diabetic group was 22.92 (±5.6) and 24.73 (±4.3), respectively; the difference was statistically significant (P = 0.007). As shown in Table 1, the scores in the domains of desire and pain were also statistically significant (P < 0.001).
Table 1.
Comparison of mean (±SD) female sexual function index domain in case and control groups
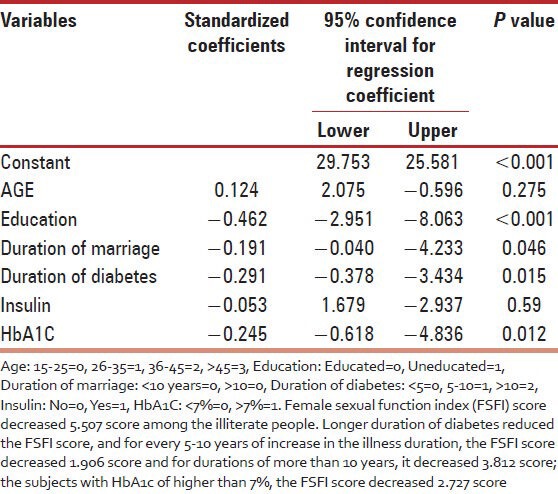
In the univariate analysis as shown in Table 2, FSFI scores in diabetic group were statistically different considering the following factors: HbA1c (P < 0.001), literacy status (P < 0.001), duration of illness and marriage (P < 0.001), taking insulin (P = 0.003), and age group (P < 0.001). In the multivariate analysis the illiteracy level, longer duration of marriage, duration of diabetes and HbA1c > 7% reduced the FSFI score in the diabetic group; age and insulin-injection did not have statistically significant impact (R2 = 0.624). FSFI score decreased 5.507 score among the illiterate people. Longer duration of diabetes reduced the FSFI score, and for every 5-10 years of increase in the illness duration, the FSFI score decreased 1.906 score and for durations of more than 10 years, it decreased 3.812 score; the subjects with HbA1c of higher than 7%, the FSFI score decreased 2.727 score [Table 3].
Table 2.
Comparison of mean (±SD) of female sexual function index domain in the case group
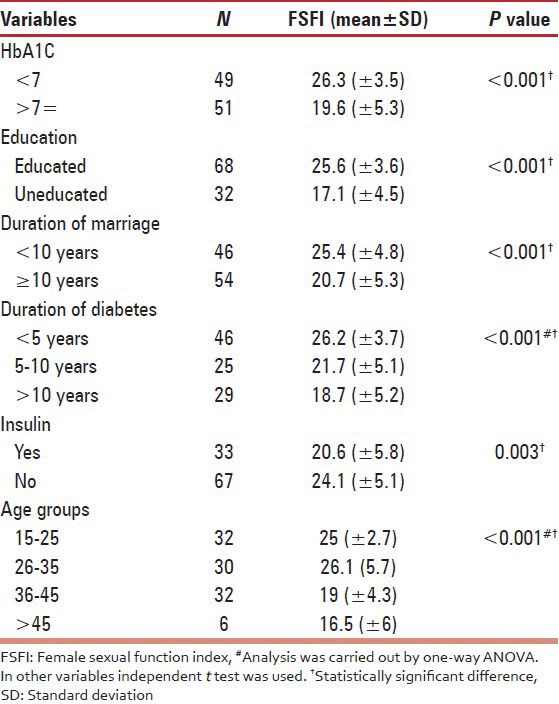
Table 3.
Analysis of multiple regression with female sexual function index score as dependent variables and some variables as independent variables in the case group
DISCUSSION
In this study, we compared the FSFI among the diabetic and non-diabetic Iranian women and the associated factors of FSFI in diabetic women were evaluated. Low educational level, longer duration of diabetes and poor controlled diabetes were associated with a lower FSFI score range in our study. The mean score of FSFI was 22.92.
In Aslan et al.,[23] the mean FSFI score was 24.25 (±9.50). Furthermore, some of this study's scores were lower than those reported by Wallner et al.,[8] and Salonia et al.[6] In Fatemi et al.'s,[15] study, sexual function's scores for the domains of desire, arousal, vaginal lubrication, orgasm, and overall satisfaction were lower among diabetic women as compared to non-diabetic peers. Similar to our findings, they showed that age and duration of diabetes had negative correlation with sexual function. In a study conducted by Abu Ali et al.,[5] they showed that the scores for the domains of arousal, lubrication and satisfaction were lower in the diabetic compared with non-diabetic women. According to their findings, duration of diabetes and age were associated with higher prevalence of SD However, in other study[3] only decreased lubrication was found in women with diabetes. Schreiner-Engel et al.[16] reported the negative impacts of type II diabetes on sexual desire, orgasmic capacity, lubrication, and sexual satisfaction. According to the Enzlin et al.'s,[2] findings, only depression was associated with SD, not diabetes.
There was no correlation between age and FSFI score in this study. In some previous studies, older age was associated with higher prevalence of SD.[4,24,25] However, effects of aging on SD were remained controversial.[26]
Several studies were found that HbA1c level was not associated with sexual function,[3,4,14,15] but in some studies sexual function decreased whenever there was a poor control over blood sugar.[7] The poor control of diabetes and poor care can lead to further complication and then decrease healthy feeling in the patients. Our results demonstrated that FSFI score was negatively correlated with HbA1C. Enzlin et al.,[3] discussed that poor control of patients, older age, and longer diabetes duration do not have a significant association with SD Different studies conducted by Doruk et al.[27] Wallner et al.,[8] and Nowosielski et al.,[28] indicated that there is no special risk-factors related to SD in diabetic women. They concluded that higher prevalence of SD in diabetic women can be related to probable confounder variables. We excluded post-menopausal women and the statistical analysis was conducted under the controlling of the confounders. However, we couldn’t investigate depression level and status among the participants of this study. Furthermore, the present study has another limitation; lack of vaginal and urinary tract evaluation for signs and symptoms of infections.
Discrepancies of results in different studies can be attributed to the prevalence of depression, heterogeneous patient population[6] and cultural situation of the study settings.
Duration of marriage had borderline significance relation with SD there are some studies indicating sexual function may decline with increasing the length of a relationship.[4,9,29,30,31] Partner factors can affect sexual behaviors between couples that they can be affected by duration of marriage. Having good sexual partners can decrease SD, but we didn’t have evaluated participants’ partners.
In our study, similar to some other studies,[24,32] we found that sexual disorder was related to a lower level of education. Maybe higher educational level can be associated with better socioeconomic status and skillful partners. Educated patients express their problem and seeking treatment, so they have lower SD.
CONCLUSION
Study confirms that Kurdish Iranian diabetic women are at an increased risk of SD. Low educational level, longer duration of diabetes and poor controlled diabetes were associated with a lower FSFI score.
ACKNOWLEDGMENTS
This study supported financially by Research deputy of Kurdistan University of Medical Sciences. The authors thank all staffs of the diabetes clinic in Tohid hospital specially Dr. Nadia Shakiba. They also thank Dr. Ebrahim Ghaderi, for his valuable contribution to the preparation of this paper. We would like to thank Syrous Shahsavari (statistical consultant).
Footnotes
Source of Support: This study supported financially by Research deputy of Kurdistan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Vahdaninia M, Montazeri A, Goshtasebi A. Help-seeking behaviors for female sexual dysfunction: A cross sectional study from Iran. BMC Womens Health. 2009;9:3. doi: 10.1186/1472-6874-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Enzlin P, Mathieu C, Van Den Bruel A, Vanderschueren D, Demyttenaere K. Prevalence and predictors of sexual dysfunction in patients with type 1 diabetes. Diabetes Care. 2003;26:409–14. doi: 10.2337/diacare.26.2.409. [DOI] [PubMed] [Google Scholar]
- 3.Enzlin P, Mathieu C, Van den Bruel A, Bosteels J, Vanderschueren D, Demyttenaere K. Sexual dysfunction in women with type 1 diabetes: A controlled study. Diabetes Care. 2002;25:672–7. doi: 10.2337/diacare.25.4.672. [DOI] [PubMed] [Google Scholar]
- 4.Kamaralzaman S, Sidi H, Yau M, Budin SB, Sani A, Mohamed H. Sexual function of Malay women with type 2 diabetes mellitus: A preliminary study. Asian J Psychiatry. 2010;11:64–71. [Google Scholar]
- 5.Abu Ali RM, Al Hajeri RM, Khader YS, Shegem NS, Ajlouni KM. Sexual dysfunction in Jordanian diabetic women. Diabetes Care. 2008;31:1580–1. doi: 10.2337/dc08-0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salonia A, Lanzi R, Scavini M, Pontillo M, Gatti E, Petrella G, et al. Sexual function and endocrine profile in fertile women with type 1 diabetes. Diabetes Care. 2006;29:312–6. doi: 10.2337/diacare.29.02.06.dc05-1067. [DOI] [PubMed] [Google Scholar]
- 7.Guay AT. Sexual dysfunction in the diabetic patient. Int J Impot Res. 2001;13:S47–50. doi: 10.1038/sj.ijir.3900779. [DOI] [PubMed] [Google Scholar]
- 8.Wallner LP, Sarma AV, Kim C. Sexual functioning among women with and without diabetes in the Boston Area Community Health Study. J Sex Med. 2010;7:881–7. doi: 10.1111/j.1743-6109.2009.01510.x. [DOI] [PubMed] [Google Scholar]
- 9.Laurent SM, Simons AD. Sexual dysfunction in depression and anxiety: Conceptualizing sexual dysfunction as part of an internalizing dimension. Clin Psychol Rev. 2009;29:573–85. doi: 10.1016/j.cpr.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 10.Najafabady MT, Salmani Z, Abedi P. Prevalence and related factors for anorgasmia among reproductive aged women in Hesarak, Iran. Clinics (Sao Paulo) 2011;66:83–6. doi: 10.1590/S1807-59322011000100015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Sakka AI, Hassoba HM, Sayed HM, Tayeb KA. Pattern of endocrinal changes in patients with sexual dysfunction. J Sex Med. 2005;2:551–8. doi: 10.1111/j.1743-6109.2005.00082.x. [DOI] [PubMed] [Google Scholar]
- 12.Erol B, Tefekli A, Sanli O, Ziylan O, Armagan A, Kendirci M, et al. Does sexual dysfunction correlate with deterioration of somatic sensory system in diabetic women? Int J Impot Res. 2003;15:198–202. doi: 10.1038/sj.ijir.3900998. [DOI] [PubMed] [Google Scholar]
- 13.Maric C. Sex, diabetes and the kidney. Am J Physiol Renal Physiol. 2009;296:680–8. doi: 10.1152/ajprenal.90505.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ziaei-Rad M, Vahdaninia M, Montazeri A. Sexual dysfunctions in patients with diabetes: A study from Iran. Reprod Biol Endocrinol. 2010;8:50. doi: 10.1186/1477-7827-8-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fatemi SS, Taghavi SM. Evaluation of sexual function in women with type 2 diabetes mellitus. Diab Vasc Dis Res. 2009;6:38–9. doi: 10.3132/dvdr.2009.07. [DOI] [PubMed] [Google Scholar]
- 16.Schreiner-Engel P, Schiavi RC, Vietorisz D, Smith H. The differential impact of diabetes type on female sexuality. J Psychosom Res. 1987;31:23–33. doi: 10.1016/0022-3999(87)90094-8. [DOI] [PubMed] [Google Scholar]
- 17.Jensen SB. Sexual dysfunction in younger insulin-treated diabetic females. A comparative study. Diabete Metab. 1985;11:278–82. [PubMed] [Google Scholar]
- 18.Liu Z, Fu C, Wang W, Xu B. Prevalence of chronic complications of type 2 diabetes mellitus in outpatients: A cross-sectional hospital based survey in urban China. Health Qual Life Outcomes. 2010;8:62. doi: 10.1186/1477-7525-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vinik AI, Maser RE, Mitchell BD, Freeman R. Diabetic autonomic neuropathy. Diabetes Care. 2003;26:1553–79. doi: 10.2337/diacare.26.5.1553. [DOI] [PubMed] [Google Scholar]
- 20.O’Kane MJ, Bunting B, Copeland M, Coates VE ESMON study group. Efficacy of self-monitoring of blood glucose in patients with newly diagnosed type 2 diabetes (ESMON study): Randomised controlled trial. BMJ. 2008;336:1174–7. doi: 10.1136/bmj.39534.571644.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohammadi K, Heydari M, Faghihzadeh S. The female sexual function index (FSFI): Validation of the Iranian version. Payesh. 2008;7:269–78. [Google Scholar]
- 22.Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 23.Aslan E, Beji NK, Gungor I, Kadioglu A, Dikencik BK. Re: Prevalence and risk factors for low sexual function in women: A study of 1,009 women in an outpatient clinic of a university hospital in Istanbul-a response. J Sex Med. 2009;6:1491–2. doi: 10.1111/j.1743-6109.2009.01259.x. [DOI] [PubMed] [Google Scholar]
- 24.Singh JC, Tharyan P, Kekre NS, Singh G, Gopalakrishnan G. Prevalence and risk factors for female sexual dysfunction in women attending a medical clinic in south India. J Postgrad Med. 2009;55:113–20. doi: 10.4103/0022-3859.52842. [DOI] [PubMed] [Google Scholar]
- 25.Valadares AL, Pinto-Neto AM, Osis MJ, Sousa MH, Costa-Paiva L, Conde DM. Prevalence of sexual dysfunction and its associated factors in women aged 40-65 years with 11 years or more of formal education: A population-based household survey. Clinics (Sao Paulo) 2008;63:775–82. doi: 10.1590/S1807-59322008000600012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hayes R, Dennerstein L. The impact of aging on sexual function and sexual dysfunction in women: A review of population-based studies. J Sex Med. 2005;2:317–30. doi: 10.1111/j.1743-6109.2005.20356.x. [DOI] [PubMed] [Google Scholar]
- 27.Doruk H, Akbay E, Cayan S, Akbay E, Bozlu M, Acar D. Effect of diabetes mellitus on female sexual function and risk factors. Arch Androl. 2005;51:1–6. doi: 10.1080/014850190512798. [DOI] [PubMed] [Google Scholar]
- 28.Nowosielski K, Skrzypulec-Plinta V. Mediators of sexual functions in women with diabetes. J Sex Med. 2011;8:2532–45. doi: 10.1111/j.1743-6109.2011.02336.x. [DOI] [PubMed] [Google Scholar]
- 29.Fugl-Meyer K, Fugl-Meyer AR. Sexual disabilities are not singularities. Int J Impot Res. 2002;14:487–93. doi: 10.1038/sj.ijir.3900914. [DOI] [PubMed] [Google Scholar]
- 30.Hawton K, Gath D, Day A. Sexual function in a community sample of middle-aged women with partners: Effects of age, marital, socioeconomic, psychiatric, gynecological, and menopausal factors. Arch Sex Behav. 1994;23:375–95. doi: 10.1007/BF01541404. [DOI] [PubMed] [Google Scholar]
- 31.Enzlin P, Rosen R, Wiegel M, Brown J, Wessells H, Gatcomb P, et al. Sexual dysfunction in women with type 1 diabetes: Long-term findings from the DCCT/EDIC study cohort. Diabetes Care. 2009;32:780–5. doi: 10.2337/dc08-1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Owiredu WK, Amidu N, Alidu H, Sarpong C, Gyasi-Sarpong CK. Determinants of sexual dysfunction among clinically diagnosed diabetic patients. Reprod Biol Endocrinol. 2011;9:70. doi: 10.1186/1477-7827-9-70. [DOI] [PMC free article] [PubMed] [Google Scholar]


