Abstract
Background:
Cross-cultural differences in attitudes and practices related to diabetes are well-known. Similar differences in symptom reporting of endocrine conditions such as menopause are well documented. Minimal literature is available on the cross-cultural variation in reporting of hypoglycemic symptoms.
Aims:
This cross-sectional study aimed to assess the symptoms of hypoglycemia encountered by diabetologists who deal with patients from different language groups from various states of North and West India and Nepal.
Materials and Methods:
Eighty three doctors from six Indian states and Nepal, attending a continuing medical education program were requested to fill a detailed, pre-tested, Likert scale based questionnaire which assessed the frequency and symptoms with which patients presented with hypoglycemia in their clinical practice. Data were analyzed based on geographic location of the diabetologists and language spoken by their patients (Hindi vs. Gujarati).
Results:
Gujarati-speaking patients tended to report to their doctors, a greater inability to work under pressure and a higher frequency of intense hunger during hypoglycemia. They were less likely to report specific adrenergic (inward trembling), neuroglycopenic (feeling down over nothing), and nocturnal (crumpled bedsheets upon waking up) symptoms.
Conclusion:
Significant cross-cultural differences related to the symptomatology of hypoglycemia are noted. Indian diabetologists should be aware of the varying presentation of hypoglycemia based on language and ethnic background.
Keywords: Culture, diabetes, ethnicity, hypoglycemia, India
INTRODUCTION
Cross-cultural differences related to perception of health and diseases are well-known. Attitudes and practices related to causation of illness, health care-seeking behavior, and acceptance of modern health care systems are determined, in part, by culture and society. Examples of the influence of culture on health and medicine abound.[1]
One of the best studied endocrine conditions with cross-cultural differences in symptomatology is menopause. Multiple studies report the variation in symptoms reported by menopausal women belonging to Caucasian, Japanese, Chinese, and Laotian ethnic groups.[2,3,4]
Variations in symptoms and clinical presentation based on culture have also been reported in endocrine diseases as diverse as prolactinoma, disorders of sex differentiation, and obesity.[5,6,7]
One disease in which substantial work has been done to document cultural impact on clinical and therapeutic aspects is diabetes.[8] Parents from different cultures rate the importance of various issues in divergent manners. Caucasian parents, for example, stress on child-centered activities, whereas African-American parents expect more social support and ask for family-oriented interventions to help manage their children with type 1 diabetes.[9]
It is surprising to note, however, that the symptomatology of disease states may also vary across cultures. People from different parts of the world perceive or define health in varying manners.[10] This cultural dichotomy is more obvious with chronic disease or in conditions with non-specific symptoms.
Although ample work has been done on cultural determinants of diabetes, one important aspect that has been neglected is the symptomatology of hypoglycemia.
Hypoglycemia is a frequently occurring, avoidable, potentially fatal, complication in both type 1 and type 2 diabetes.[11] One of the main limiting factors of aggressive titration of treat-to-target therapy, hypoglycemia negatively impacts physical and psychological health, as well as quality of life.[11,12] The symptoms of hypoglycemia are well known and are classified according to pathophysiological mechanisms (neuroglycopenia, autonomic, general), clinical (whether or not requiring external assistance), or biochemical (degree of hypoglycemia) parameters.[13] These classifications, however, do not adequately cover the wide variety of symptoms that a patient may present.
Symptoms of hypoglycemia can vary based upon the degree and rapidity of development of the condition. The presenting symptoms may also be influenced by the autonomic health of the individual and may be masked by hypoglycemia unawareness.[10] On the other hand, an individual who has undergone hypoglycemia awareness training may report subtle symptoms of neuroglucopenia.
As regards to any medical illness, hypoglycemia included, reporting of symptoms, is patient-dependent. On the other hand, the documentation of signs corresponding to the same medical condition is physician-dependent. A trained physician will be able to extract from the history, subtle, unrecognized symptoms of hypoglycemia, which a less experienced colleague may not appreciate. Much of the quality of history-taking depends upon grasp of the language or dialect that the patient and physician are conversing. An in-depth knowledge of the intricacies of word architecture of the language concerned will help the physician ferret important clinical clues. Even a cursory look at Thesaurus will sensitize the physician to the countless possibilities of symptom reporting. For example, the adjective “sick” has 49 synonyms,[14] as reported in the Thesaurus.
Cross-cultural differences in the perception of the hypoglycemia have been studied in a small qualitative – descriptive study[15] that has been recently reported. Authors compared a small cohort (n = 10 each) of Russian-speaking Slavic immigrant American women and non-Hispanic non-immigrant white American women with type 2 diabetes. They observed significant differences in symptomatology of diabetes between the two groups, as well as less awareness of hypoglycemia in the Slavic group. Their study highlighted the need for culturally congruent diabetes care to improve outcomes.
Another study assessed the “meaning” of hypoglycemia for six Singaporean adults with type 2 diabetes. The work highlighted the different impact of hypoglycemia on individuals as well as the varied terminology with which they reported their symptoms.[16]
No such work has been performed in India, a country with numerous cultures and languages. Indian doctors working in most parts of the country are called upon to manage patients from varying ethnic groups. Although almost all Indian doctors are multi-lingual, they may or may not be equally fluent in all the dialects that their patients speak. The authors, for example, are from Haryana, considered a relatively “homogenous” state, but deal with patients speaking in Hindi, Haryanvi, Punjabi, Urdu, and English, in a wide variety of accents.
MATERIALS AND METHODS
This study was designed as a cross-sectional survey of diabetologists and endocrinologsts from six states of North and West India to assess whether symptoms of hypoglycemia exhibit cross-cultural variation. The states covered were Gujarat, Rajasthan, Punjab, New Delhi, Uttarakhand, and Uttar Pradesh. A few study participants from Nepal were also surveyed.
A pre-tested questionnaire was administered, after taking informed verbal consent, to 88 diabetologists attending a regional continuing medical education program in July 2012. This questionnaire listed 47 symptoms of hypoglycemia which were graded by respondents on a 5-point Likert Scale, as per the frequency with which they were reported by patients in their clinical practice. These symptoms included 11 general, 17 neuroglycopenic, and 11 adrenergic manifestations of hypoglycemia, as well as 8 well-characterized symptoms of nocturnal hypoglycemia. The questionnaire also captured data regarding the frequency of hypoglycemia noted in 9 types of clinical situations.
Analysis
Data were analyzed with statistical package for social sciences (SPSS) version. 17.0 (IBM Corporation, New York, USA). Descriptive statistics used included mean and median (with range) scores of different study variables. Parametric test used included ANOVA with post-hoc analysis (using Least Significant Difference (LSD)). Pearson's correlation coefficient statistics was used to ascertain correlation between years in practice and questionnaire items. Non-parametric tests used included Kruskal-Wallis test. The level of statistical significance was kept at P < 0.05 for all the tests.
RESULTS
A total of 88 respondents returned the survey questionnaire. All but two respondents were male. The frequency distribution of the respondents has been described in Table 1. It included endocrinologists and diabetologists from Gujarat (32.5%), Rajasthan (15.7%), Uttarakhand and Uttar Pradesh (21.7%), Delhi, Punjab (25.3%) and Nepal (4.8%).
Table 1.
Mean age and years in practice of study respondents
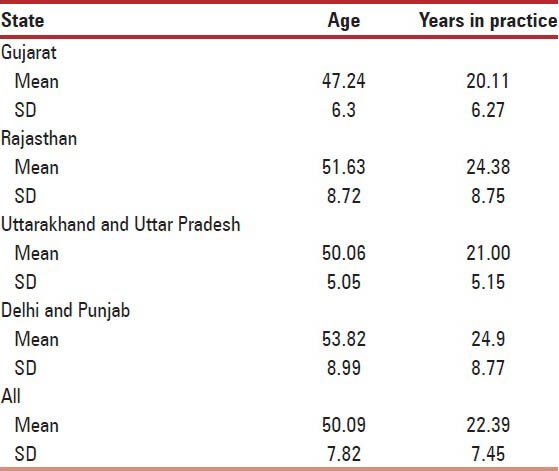
The mean age and years in practice of respondents from different states has been presented in Table 1. There was significant difference in mean age of respondents from different states (F = 2.97, df = 3, P = 0.03). Post-hoc analysis revealed that this difference was due to significant difference in mean age of respondents from Gujarat and Delhi/Punjab (mean difference 6.58 years, SEM-2.27, P = 0.03, 95% CI-0.40-12.76). The difference was not significant for any other pair. The mean years in practice were comparable between different groups (F = 1.07, df = 3, P = 0.36).
Table 2 presents the proportion of total patients (given as median percentage and range) seen by the respondents that presented with hypoglycaemia in various clinical situations. Median values have been reported here because of wide range of standard deviation observed for mean for these variables. No significant differences were observed between the different groups on any of these variables.
Table 2.
Hypoglycaemic episodes observed by clinicians from different states within between-group comparisons
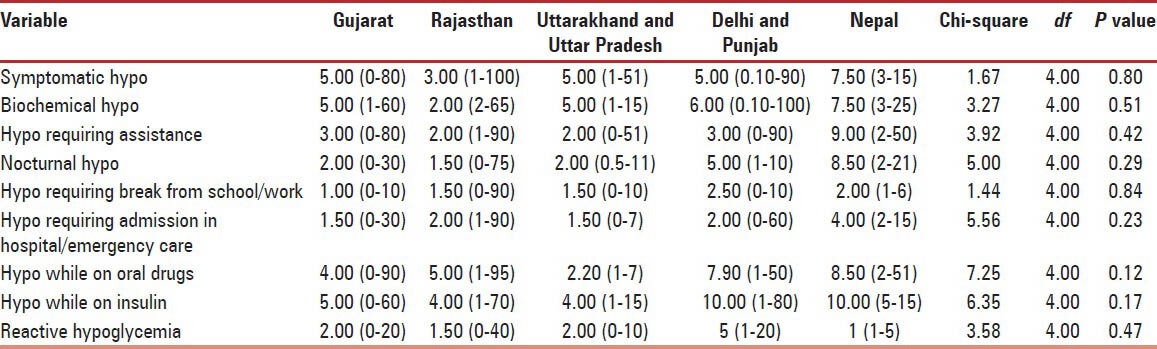
Table 3 presents the proportion of patients (given as mean percentage and SD) presenting with various general and adrenergic features of hypoglycaemia as reported by the respondents from various states. The only variable significantly difference between the groups was “cannot work under pressure” (F = 2.63, P = 0.04). Post-hoc analysis revealed that the difference was significant between the respondents from states of Rajasthan and Gujarat (mean difference = 0.108, P = 0.009, 95% CI-0.27-1.88). The mean score was significantly higher for respondents from Rajasthan (mean-2.92, SD 1.32) when compared with those from Gujarat (mean-1.84, SD 1.03).
Table 3.
General and adrenergic features of hypoglycaemia reported by respondents from different states with in between group comparisons
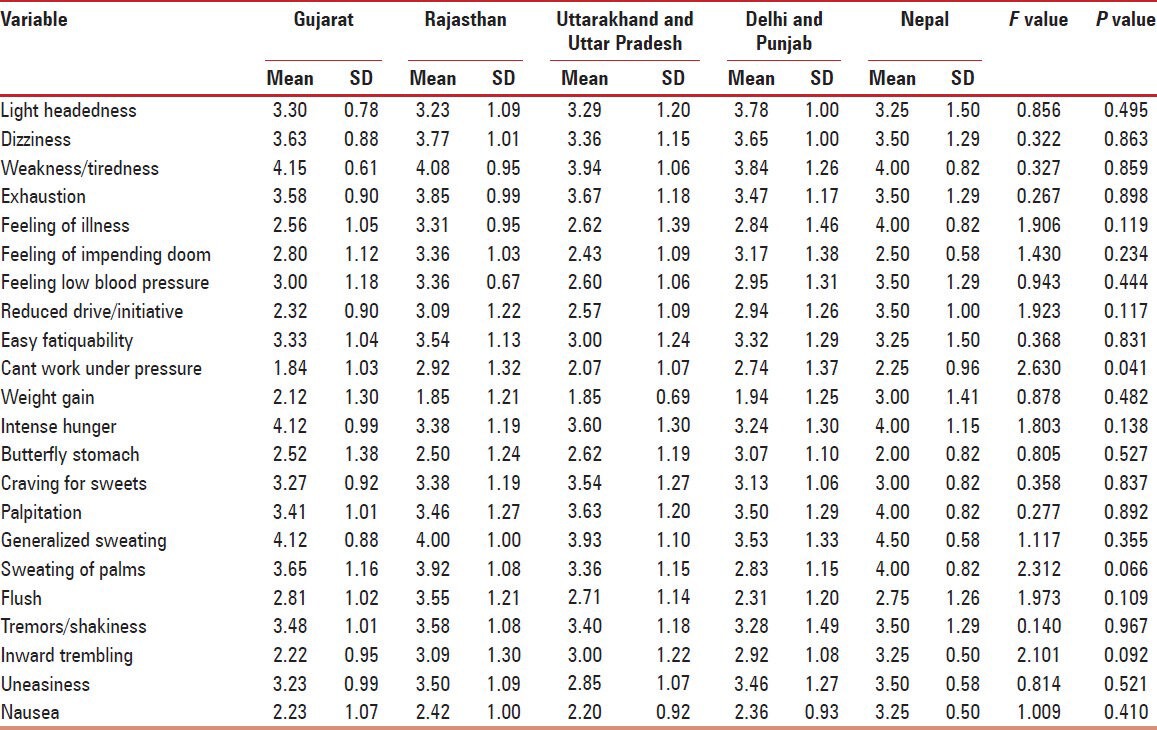
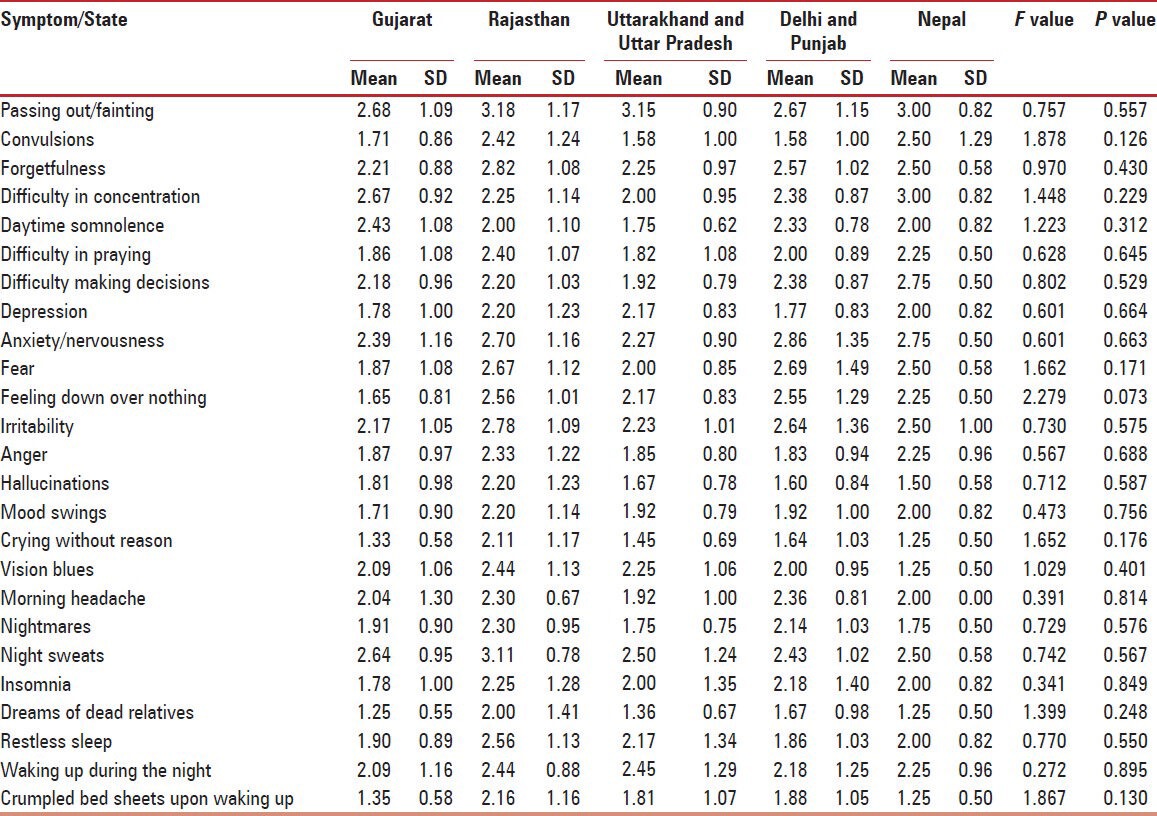
Table 4 presents the proportion of patients among those with hypoglycaemia (given as mean percentage and SD) presenting with various neuroglycopenic and nocturnal symptomatic features. No significant differences were observed between the respondents from different states for any of these psychologic variables.
Table 4.
Neuroglycopenic and nocturnal features of hypoglycemia reported by respondents from different states within between-group comparisons
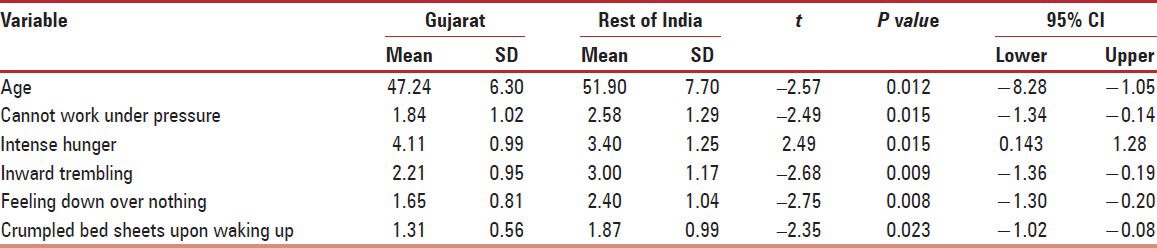
There was no significant correlation between the years in practice and any of the items of the study questionnaire. Between-group comparisons were carried out for respondents from different regions. On comparing the respondents from Gujarat with rest of the country, significant differences were observed on certain variables [Table 5]. The mean age of respondents from Gujarat (47.24 SD 6.30) was lower than respondents from rest of the country (51.90 SD 7.70). The difference was statistically significant (t = 2.57, P = 0.012, 95% CI 1.05-8.28). The clinical features of “inability to work under pressure” (general symptom) was encountered more frequently by the respondents from Gujarat among their Gujarati-speaking patients when compared with respondents from rest of the country, who managed Hindi-speaking patients (t = 2.49, P = 0.015, 95% CI 0.14-1.34). Similarly, clinical features “inward trembling” (hyperadrenergism) (t = 2.68, P = 0.009, 95% CI 0.19-1.36), “feeling down over nothing” (neuroglycopenia) (t = 2.75, P = 0.008, 95% CI.20-1.30), and “crumpled bed sheets upon waking up” (nocturnal hypoglycemia) (t = 2.35, P = 0.023, 95% CI 0.08-1.02) were encountered at a significantly lower frequency by respondents from Gujarat when compared with respondents from rest of the country. However, “intense hunger” (adrenergic symptom) was encountered at a significantly higher frequency by respondents from Gujarat (t = 2.49, P = 0.015, 95% CI 0.14-1.28).
Table 5.
Between-group differences for respondents from Gujarat and rest of India
Data from Nepal were not considered for statistical analysis in view of the small number of study participants (n = 4). However, a descriptive analysis of the same revealed interesting findings. Nepalese doctors were of the same age as their Indian counterparts. They encountered a higher incidence of hypoglycemia of all types related to all clinical situations, except for reactive hypoglycemia. Symptoms which were reported more often in Nepal included feeling of illness, weight gain, palpitations, sweating, and trembling. Some symptoms such as butterfly stomach were reported relatively less frequently by the doctors from Nepal.
DISCUSSION
This is the first study in the world, to the best of our knowledge, to objectively study the potential cross-cultural and cross-linguistic differences in symptom reporting of hypoglycemia in patients with diabetes. This study utilized the responses of 88 experienced diabetologists and endocrinologists, with years of clinical experience. All of them reported encountering patients with hypoglycemia. This helped gather information from a much larger pool of patients than would have otherwise been possible. When asked to report the symptoms with which their patients presented, their responses varied according to language of patients. Gujarati-speaking patients tended to report a greater inability to work under pressure, and a higher frequency of intense hunger, during hypoglycemia, to their doctors. They were less likely to report specific adrenergic (inward trembling), neuroglycopenic (feeling down over nothing), and nocturnal (crumpled bed sheets upon waking up) symptoms as specified above.
These findings highlight the potential cross-cultural and cross-linguistic variations in patient perception of hypoglycemic symptoms. The results are important as they have major diagnostic and therapeutic implications. Diabetes care providers should be aware of the possible differences in reporting of hypoglycemic symptoms by patients belonging to different linguistic and ethnic groups. The ability to elicit a detailed history of hypoglycemia is not only part of general clinical competence, but should be also be highlighted as a domain of cross-cultural competence.
Our study does have a few limitations. The choice of respondents was based on convenience sampling rather than a randomized method. Physicians were asked to rate the frequency of various symptoms reported by their patients rather than asking patients directly. This introduced an added recall bias. Apart from this, the response is based on physicians’ impression, not that of patients. Physicians in their busy practice tend to ask leading questions, and a lot of time our patients just try to be affirmative. The questionnaire was prepared in English rather than in local languages which the patients spoke (Hindi, Gujarati, Punjabi, Nepali). The English translations may not have conveyed the nuances of the patient-reported symptoms. The study which was planned as an all-India exercise had to be limited to North and West India due to unforeseen circumstances. The sample of the physicians in number and distribution is probably not well powered to represent the large community of Indian diabetologists.
In spite of these issues this study has strengths which warrant its publication and dissemination. This is the first study in India, rather in the world, to the best of our knowledge, to objectively study the cross-cultural or cross-linguistic variation in symptomatology of hypoglycemia. It makes use of appropriate statistical tools to quantify the significance of such differences using physician-reported data, based on their clinical experience of treating vast number of patients, it takes advantage of a much greater pool of patients, through their physicians, than would have been possible using a direct face-to-face interview method. The questionnaire itself works as a therapeutic education tool for both physicians and patients, prompting them to elicit and offer relevant medical history and help them improve communication skills related to hypoglycemia.
Measuring diabetes health beliefs in a South Asia population is challenging. A recent review highlights the virtual lack of literature and the difficulties in comparing existing studies in this field, from a part of the world which faces the brunt of the diabetes pandemic.[17] Keeping this in mind, the current work assumes greater importance. It has added significant contribution to world literature on hypoglycemia perception as an aspect of medical anthropology, and should stimulate larger studies on this topic in India and other parts of the globe.
CONCLUSION
Cross-cultural care and multi-linguistic care is a part and parcel of an Indian diabetologist's work. What needs to be emphasized, however, is the need for cultural and linguistic competence as well. This will encompass, among other issues, an understanding of the varied symptoms of hypoglycemia reported by patients from different ethnic and language groups.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hjelm KG, Bard K, Nyberg P, Apelqvist J. Beliefs about health and diabetes in men of different ethnic origin. J Adv Nurs. 2005;50:47–59. doi: 10.1111/j.1365-2648.2004.03348.x. [DOI] [PubMed] [Google Scholar]
- 2.Green R, Santoro N. Menopausal symptoms and ethnicity: The study of women's health across the nation. Womens Health (Lond Engl) 2009;5:127–33. doi: 10.2217/17455057.5.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown DE, Sievert LL, Morrison LA, Reza AM, Mills PS. Do Japanese American women really have fewer hot flashes than European Americans? The hilo women's health study. Menopause. 2009;16:870–6. doi: 10.1097/gme.0b013e31819d88da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sayakhot P, Vincent A, Teede H. Cross-cultural study: Experience, understanding of menopause, and related therapies in Australian and Laotian women. Menopause. 2012;19:1300–8. doi: 10.1097/gme.0b013e31825fd14e. [DOI] [PubMed] [Google Scholar]
- 5.Kann PH, Juratli N, Kabalan Y. Prolactinoma and hyperprolactinaemia: A transcultural comparative study between Germany as a western, liberal, industrialised country and Syria as an oriental society with a strong Islamic tradition. Gynecol Endocrinol. 2010;26:749–54. doi: 10.3109/09513590.2010.487600. [DOI] [PubMed] [Google Scholar]
- 6.Warne GL, Raza J. Disorders of sex development (DSDs), their presentation and management in different cultures. Rev Endocr Metab Disord. 2008;9:227–36. doi: 10.1007/s11154-008-9084-2. [DOI] [PubMed] [Google Scholar]
- 7.Craig P, Halavatau V, Comino E, Caterson I. Perception of body size in the Tongan community: Differences from and similarities to an Australian sample. Int J Obes Relat Metab Disord. 1999;23:1288–94. doi: 10.1038/sj.ijo.0801069. [DOI] [PubMed] [Google Scholar]
- 8.Barko R, Corbett CF, Allen CB, Shultz JA. Perceptions of diabetes symptoms and self-management strategies: A cross-cultural comparison. J Transcult Nurs. 2011;22:274–81. doi: 10.1177/1043659611404428. [DOI] [PubMed] [Google Scholar]
- 9.Lipman TH, Murphy KM, Kumanyika SK, Ratcliffe SJ, Jawad AF, Ginsburg KR. Racial differences in parents’ perceptions of factors important for children to live well with diabetes. Diabetes Educ. 2012;38:58–66. doi: 10.1177/0145721711427454. [DOI] [PubMed] [Google Scholar]
- 10.Wallin AM, Ahlström G. From diagnosis to health: A cross-cultural interview study with immigrants from Somalia. Scand J Caring Sci. 2010;24:357–65. doi: 10.1111/j.1471-6712.2009.00729.x. [DOI] [PubMed] [Google Scholar]
- 11.Amiel SA, Dixon T, Mann R, Jameson K. Hypoglycaemia in type 2 diabetes. Diabet Med. 2008;25:245–54. doi: 10.1111/j.1464-5491.2007.02341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marrett E, Radican L, Davies MJ, Zhang Q. Assessment of severity and frequency of self-reported hypoglycemia on quality of life in patients with type 2 diabetes treated with oral antihyperglycemic agents: A survey study. BMC Res Notes. 2011;4:251. doi: 10.1186/1756-0500-4-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Workgroup on Hypoglycemia, American Diabetes Association. Defining and reporting hypoglycemia in diabetes: A report from the American diabetes association workgroup on hypoglycemia. Diabetes Care. 2005;28:1245–9. doi: 10.2337/diacare.28.5.1245. [DOI] [PubMed] [Google Scholar]
- 14.Sick. [Last accessed 2012 Sep 15]. Available from: http://www.thesaurus.com/browse/sick?s=t .
- 15.Barendse S, Singh H, Frier BM, Speight J. The impact of hypoglycaemia on quality of life and related patient-reported outcomes in Type 2 diabetes: A narrative review. Diabet Med. 2012;29:293–302. doi: 10.1111/j.1464-5491.2011.03416.x. [DOI] [PubMed] [Google Scholar]
- 16.Tan PS, Chen HC, Taylor BJ, Hegney DG. Exploring the meaning of hypoglycaemia to community-dwelling Singaporean Chinese adults living with type 2 diabetes mellitus. Int J Nurs Pract. 2012;18:252–9. doi: 10.1111/j.1440-172X.2012.02031.x. [DOI] [PubMed] [Google Scholar]
- 17.Patel N, Kennedy A, Chew-Graham C, Blickem C, Bower P. Measuring diabetes health beliefs in the South Asian population: A narrative systematic review of feasibility and validity. Diversity and Equality in Health and Care. 2012;9:57. [Google Scholar]


