Abstract
Despite the fact that HIV epidemic is mainly driven by injection drug use in Iran, partners of People Who Inject Drugs (PWID) have been seriously neglected in terms of effective preventive interventions. Currently, sexual partners of PWID might have access to some harm reduction services at Voluntary Counselling and Testing (VCT) centers; however, their needs have not been effectively targeted and met. Unfortunately, the current programs implemented by the Ministry of Health have overlooked the importance of this population in the course of the HIV epidemic throughout the country. In this policy brief, we are trying to draw the health policy-makers’ attention to this overlooked population and while reviewing the advantages and disadvantages of some of the readily available options on the table, come up with a recommended action to tackle this problem. Our recommended action that seems to have had promising results elsewhere in Asia would try to implement preventive interventions targeting this particular population through peer prevention programs.
Keywords: Sexual Partners, People Who Inject Drugs (PWID), HIV, Peer Prevention, Iran
Background
What does the HIV epidemic look like in Iran?
Injecting drug use continues to be the dominant mode of HIV transmission in Iran. Iran has the highest proportion of heroin and opium drug dependence in the world and studies suggest that up to 300,000 People Who Inject Drugs (PWID) are living throughout the country (1,2). The prevalence of HIV among the general population in Iran is less than 0.2%, but it stands at 15.07% among injecting drug users (2). Although prevention programs during the last decade have successfully slowed the epidemic down among PWID, they and their sexual partners are still the most affected population in Iran (2,3).
What is a bridging population?
In addition to most at-risk marginalized populations—PWID, Females Sex Workers (FSW), and Men who have Sex with Men (MSM)—bridging/bridge populations are also at a higher risk of HIV infection in compare to general population. These populations usually include clients of FSWs, sexual partners of PWID and MSM. Other groups such as truck drivers, military staffs, sailors, and migrant labor could also fit this category (4). Very few interventions have targeted such bridge populations in Iran and the accessibility, availability and use of such services have not been evaluated; mostly due to the difficulties in verifying and reaching them (particularly for clients of FSW and sexual partners of PWID).
Who are Sexual Partners of PWID and Why Should We Care?
A major overlooked population affected by HIV in Iran are sexual partners of PWID. Worldwide, and in Iran, women are the most vulnerable population due to a number of cultural, political, religious, and biological factors. A considerable part of HIV infected women, are assumed to have acquired the infection through their husbands or sexual partners through unsafe shared injection or sex. Around 8.7% of all detected HIV cases in Iran are women. Moreover, 76% of HIV-infected women in Iran have acquired the infection from their husbands (who are primarily PWID) (2,3). In 2010, majority of new infected cases (6222 Out of 9136) were estimated to belonged to PWID and their sexual partner sub-populations (5). Clearly, sexual partners of PWID in Iran have been underserved regarding HIV preventive programs, given the fact that it is a PWID driven HIV epidemic.
Current situation
A recent cross-sectional study conducted in 2011 in three major cities (Tehran, Mashhad, and Shiraz) estimated an HIV prevalence of 7.7% and 2.8% among injecting and non-injecting sexual partners of PWID, respectively. The high prevalence among those partners who inject drugs themselves could be due to the dual risk of unsafe sex and injection (3). These findings are consistent with the findings of a recent modeling study regarding the modes of HIV transmissions in Iran. It is estimated that more than 1100 new HIV infections occur annually among sexual partners of PWID, putting them as the second-rank HIV affected population in Iran (Figure 1) (5). Currently, sexual partners of PWID like any other women might have access to some harm reduction services at Voluntary Counselling and Testing (VCT) centers or similar clinics; however, none have particularly targeted their needs and tailored interventions (2). Obviously, this high-priority sub-population and their particular needs are overlooked.
Figure 1.
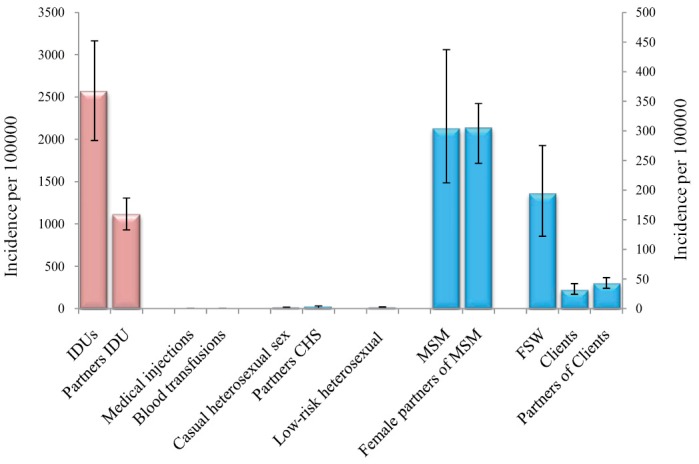
New HIV infections in key populations at highest risk per 100,000 (with 95% CI); the error bars represent the 95% simulation intervals. The incidence in all groups appears on the right hand side of the figure excluding PWID and their sexual partners. Reprinted with permission from Nasirian et al. (5)
Options with pros and cons
a) Providing prevention services through VCTs
As currently sexual partners of PWID are offered some services in VCTs, we may enhance those services. Although access to sexual partners of PWID has improved to a great extent after implementation of “Vulnerable Women Counselling Centers” in large cities, there are still major gaps in access to these services (6). First, these centers are only established in major cities and residents of smaller cities would be deprived of access to these services. Moreover, as these centers provide services for FSWs as well as female PWID, referring to such VCTs is highly stigmatized and seems to have been unacceptable by sexual partners of PWID. VCTs are also mainly established in poor neighborhoods which usually overlap with drug scene areas. Drug scenes are under constant surveillance of the police which could be another drawback for this population in seeking services. All of the above-mentioned concerns somehow are supported by the national annual report stating that only 30.2% of partners had ever sought services and utilized these centers (6).
b) Educational programs for PWID through service providing centers
A possible approach in reducing HIV risk among sexual partners of PWID could be through educating their injecting drug partners. Information and education for PWID are delivered through outreach programs; community based educational centers, prisons, and Drop-in-Centers. This practical approach could improve the knowledge of PWID and promote safe sex and injection among them and in turn, could protect their partners. Nonetheless, based on the 2010 survey among PWID, their knowledge of HIV is already high; a majority of participants had a good knowledge about preventive practices and the effectiveness of condom in preventing HIV transmission (2). Although the awareness on prevention is on the rise among PWID, the effect of such awareness on their behavior seems limited as we continue to see unprotected sexual contact and injection within this population. According to the Bio-Behavioural Surveillance Survey of PWID in 2010, respondents continued to carry out risky sexual and injection behaviours despite their relatively high level of awareness regarding HIV transmission risk factors (2). It seems such knowledge was not translated into safer practices. Targeting PWID and their sexual partners as a couple/family not individual could be a better approach as reported in other studies globally. It could be a particularly useful approach for 50% of PWID who were found to be ever-married and 30% of them who were living with their spouses at the time of the study (2).
Recommended action
Why do we think this intervention could work in the context of Iran?
Iran is a family-oriented society in which gender norms are set in a way that women take care of all family members, their husband in particular. For example, it is the woman who reminds her partner about their medications. This cultural norm although may put an additional burden on women and could be challenged by women activists, but can also be the sweet spot for intervention. We can help improve the adherence and retention to therapy among HIV-positive PWID through educating their partners. In other words, sexual partners of PWID would encourage their partners to take their medications and in fact they would be protecting themselves. A notable profit of such programs would be increasing sexual partners of PWIDs’ access to both healthcare and education along with decreasing their risky behaviour (7,8). In conclusion, we suggest implementing peer counselling and education programs among sexual partners of PWID. Similar projects, elsewhere in Asia, have shown promising results in increasing the level of knowledge and practice of partners (7,8). Findings of studies in Vietnam for example, suggested that sexual partners of PWID could be reached, and their relationships were improved and consistent condom use was increased through peer based HIV prevention interventions (8).
In the case of Iran, access to sexual partners of PWID may be possible through their injecting drug partners who seek services in various centers and are in fact, reachable. Peer educators will provide risk reduction information, materials, supplies, and referrals tailored to their individual and couple related factors. Other services such as regular HIV testing, sexually transmitted infections testing and treatment, reproductive health and family planning services, and harm reduction programs (for sexual partners of PWID who are injecting drug users themselves), could be delivered through family-friendly centers using lessons learned from PWID harm reduction programs.
Challenges and concerns
Unfortunately, the main challenge in front of implementing this approach is the deeply rooted stigma at different social and political levels against HIV and PWID (9). Another major challenge would be the limited knowledge and paucity of research about sexual partners of PWID’s network. We need to get a better understanding of how their network (if there is any) operates and then come up with points of intervention. We know very little about the structure of their network and how it functions; data that is not impossible to gain. We need further qualitative and quantitative researches to provide us with estimations of their network’s strength, PWID’s length of relationship with their sexual partners, and the applicability of this approach in smaller cities. We also need to design appropriate and applicable interventions which are most appropriate for the context and current condition of the country.
Another less challenging concern could be training of the peer educators which could be undertaken based on the WHO guidelines. Having a clear policy and curriculum in training the staff may be helpful in this regard. Due to the nature of this work and the occupational hazards around, some peers may quit working after a while which would waste all those training efforts and their experience of working in the field. Providing the trained peers with adequate salary and other benefits such as health insurance can motivate them to take this task seriously and hold on to their job.
Acknowledgements
Authors would like to express their gratitude to Ali Mirzazadeh for his scientific input and editorial skills.
Ethical issues
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Authors’ Contributions
MK drafted the manuscript and all authors reviewed and approved the final version.
Authors’ affiliations
1School of Population and Public Health, Faculty of Medicine, University of British Columbia, Vancouver, BC, Canada. 2Regional Knowledge Hub, and WHO Collaborating Center for HIV Surveillance, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran. 3Department of Food Hygiene and Public Health, Faculty of Veterinary Medicine, Shahid Bahonar University of Kerman, Kerman, Iran. 4Research Center for Modeling in Health, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran.
Citation: Karamouzian M, Haghdoost AA, Sharifi H. Addressing the needs of sexual partners of people who inject drugs through peer prevention programs in Iran. Int J Health Policy Manag 2014; 2: 81–83. doi: 10.15171/ijhpm.2014.19
References
- 1.Abu-raddad L, Akala FA, Semini I, Riedner G, Wilson D, Tawil O. Characterizing the HIV/AIDS epidemic in the Middle East and North Africa: time for strategic action. Washington, DC: World Bank Publications; 2010. [Google Scholar]
- 2.Khajehkazemi R, Osooli M, Sajadi L, Karamouzian M, Sedaghat A, Fahimfar N. et al. HIV prevalence and risk behaviours among people who inject drugs in Iran: the 2010 National Surveillance Survey. Sex Transm Infect. 2013;89:iii29–32. doi: 10.1136/sextrans-2013-051204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alipour A, Haghdoost AA, Sajadi L, Zolala F. HIV prevalence and related risk behaviours among female partners of male injecting drugs users in Iran: results of a bio-behavioural survey, 2010. Sex Transm Infect. 2013;89:iii41–4. doi: 10.1136/sextrans-2013-051201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UNAIDS. UNAIDS terminology guidelines. Geneva: Joint United Nations Programme on HIV/AIDS; 2011. [Google Scholar]
- 5.Nasirian M, Doroudi F, Gouya MM, Sedaghat A, Haghdoost AA. Modeling of human immunodeficiency virus modes of transmission in iran. J Res Health Sci 2. 012;12:81–7. [PubMed] [Google Scholar]
- 6. National AIDS Committee Secretariat and Ministry of Health and Medical Education (MoHME). Islamic Republic of Iran AَIDS Progress Report [internet]. 2012. Available from: http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/IRIran%20AIDS%20Progress%20Report%202012%20English%20final1_1.pdf
- 7.Go VF, Frangakis C, Le Minh N, Latkin CA, Ha TV, Mo TT. et al. Effects of an HIV peer prevention intervention on sexual and injecting risk behaviors among injecting drug users and their risk partners in Thai Nguyen, Vietnam: A randomized controlled trial. Soc Sci Med. 2013;96:154–64. doi: 10.1016/j.socscimed.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hammett TM, Kling R, Van NT, Son DH, Binh KT, Oanh KT. HIV prevention interventions for female sexual partners of injection drug users in Hanoi, Vietnam: 24-month evaluation results. AIDS Behav. 2012;16:1164–72. doi: 10.1007/s10461-011-0062-4. [DOI] [PubMed] [Google Scholar]
- 9.Haghdoost A, Karamouzian M. Zero New HIV Infections, Zero Discrimination, and Zero AIDS-Related Deaths: Feasible Goals or Ambitious Visions on the Occasion of the World AIDS Day? Int J Prev Med. 2012;3:819–23. doi: 10.4103/2008-7802.104850. [DOI] [PMC free article] [PubMed] [Google Scholar]


